The compatibility of Quetiapine and alcohol can lead to exacerbation of schizophrenia and the development of psychosis. Both substances penetrate the blood-brain barrier, causing an effect on the central nervous system.
But alcohol has a great toxic effect, so it completely eliminates the therapeutic effect.
Zincteral and alcohol
Coldrex and alcohol
Z-Factor and alcohol
Macropen and alcohol
Use search
Are you having any problem? Need more information? Type in the form and press Enter!
Compatibility of Quetiapine and alcohol
The medicine belongs to antipsychotic drugs. It penetrates the brain, interacting with dopamine receptors, improving the patient's well-being. If a person drinks alcohol at the same time, it interferes with the therapeutic effect, causing damage to nerve cells.
To remove ethyl alcohol from the body, the kidneys increase diuresis. Not only ethanol is eliminated, but also the drug. Therefore, the antipsychotic effect is reduced even more.
Take the Attention Test! Find 10 differences! (click right here!)
Comparison of the effectiveness of Ketilept and Quetiapine
The effectiveness of Ketilept is quite similar to Quetiapine - this means that the ability of the drug substance to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Ketilept is more pronounced, then using Quetiapine even in large doses will not achieve this effect.
Also, the speed of therapy - an indicator of the speed of therapeutic action - is approximately the same for Ketilept and Quetiapine. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Brief characteristics of the drug
This medicine is based on the active substance of the same name, which is produced in the form of tablets.
The drug is characterized by the following pharmacological actions:
- interaction between serotonin and dopamine receptors, forming catalepsy;
- decreased activity of dopamine neurons;
- does not cause an increase in prolactin.
When taking a dose of the medicine, the effect lasts for 12 hours. The medicine is absorbed through the mucous membrane of the digestive tract and binds to blood plasma proteins in a high percentage. Excretion is carried out through the kidneys and intestines.
The drug is indicated for use in psychosis and schizophrenia. The dosage depends on the patient’s condition, his age, and the presence of liver and kidney diseases.
Side effects:
- dizziness, headache, sleep disturbance;
- decreased or increased blood pressure, increased heart rate;
- dyspepsia, increased liver enzymes with the development of an inflammatory reaction of the organ, abdominal pain, dry mouth;
- decrease in immune blood cells;
- inflammation of muscle tissue, mucous membrane of the nasal passages;
- skin allergic reactions;
- penetration of infection into the genitourinary system;
- a decrease in the amount of thyroid hormones, which is reversible after completion of treatment;
- weight gain;
- rise in body temperature.
The product is contraindicated in case of individual intolerance to one of the components. The medicine can be used by pregnant and lactating women as prescribed by a doctor if the effect outweighs the risk of side effects. Prescribed with caution for elderly people and patients with cardiovascular disorders.
The medicine causes drowsiness, inhibits the functioning of the nervous system, and can lead to lethargy, therefore it is forbidden to drive a vehicle or operate machinery during treatment.
https://myweak.ru/alkogolizm/lekarstva/kvetiapin-sovmestimost.html
Kvetiron: composition and release form of the drug
Kvetiron is available in the form of film-coated tablets.
The active ingredient is quetiapine. 1 tablet contains quetiapine fumarate in terms of 100% dry matter quetiapine 25 mg, 100 mg or 200 mg.
Excipients – lactose monohydrate, calcium hydrogen phosphate dihydrate, microcrystalline cellulose, sodium starch glycolate, povidone, magnesium stearate; shell: OpadryIIWhite (Kvetiron 25, Kvetiron 200) (polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide (E 171)), OpadryIIYellow (Kvetiron 100) (polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide (E 171), quinoline yellow (E 104), iron oxide red (E 172), iron oxide yellow (E 172)).
Use of the drug for alcoholism
If a person has chronic alcoholism, ethanol is concentrated in large quantities in his brain. This causes neurological disorders, psychoses, neuroses, delirium, hallucinations, and delirium tremens.
If the patient starts taking the medicine, there will be no therapeutic effect. The condition will continue to improve until you quit your addiction.
In humans, the function of many internal organs is impaired. Alcoholic hepatitis, cirrhosis, and renal failure occur. The instructions for use say that the product is used with caution in these conditions. If a person continues to consume ethanol, the condition of the organs becomes worse. Therefore, there is a contraindication for taking the medicine.
Consequences of drinking alcohol
If the ban on the simultaneous use of substances is violated, the following consequences occur in the body:
- strengthening of the effect of psychosis, the person becomes inadequate, capable of any actions;
- if schizophrenia is treated, the disease worsens;
- the incidence of delusions, hallucinations and delirium tremens increases;
- inflammation of the liver and kidneys with prolonged use of both substances;
- when the liver is inflamed, the patient’s skin becomes yellow, itching and spider veins occur;
- muscle pain;
- skin allergic reactions;
- decreased body resistance to bacteria, genitourinary infections often occur, for example, pyelonephritis, cystitis;
- body temperature rises;
- the patient constantly feels sick and vomits periodically;
- stool changes, diarrhea or constipation may occur.
Negative consequences occur even with a single use of ethanol and the drug.
Kvetiron: how to take the drug
There are different dosages for each indication. The dose of the drug and the duration of treatment are determined by the doctor individually for each patient, depending on the indications and severity of the disease.
For oral use.
Quetiapine can be taken with or without food.
Adults
Course treatment of schizophrenia. Quetiapine should be taken twice daily. In the first 4 days of therapy, the daily dose is: 1st day - 50 mg, 2nd day - 100 mg, 3rd day - 200 mg, 4th day - 300 mg. Starting from the 4th day, increase the dose until the required clinical effect is achieved (ranging from 300 to 450 mg/day). Depending on the clinical effectiveness and tolerability of the drug, the daily dose of Kvetiron can range from 150 mg to 750 mg. The maximum daily dose of Kvetiron for the treatment of schizophrenia is 750 mg.
Course treatment of manic episodes associated with bipolar disorders. Quetiapine should be taken twice daily. The daily dose in the first 4 days of treatment is: 1st day – 100 mg, 2nd day – 200 mg, 3rd day – 300 mg, 4th day – 400 mg. Subsequently, increase the dose (but not more than 200 mg daily) to 800 mg/day, starting from the 6th day of treatment. Depending on the clinical effectiveness and tolerability of the drug, the dose can range from 200 to 800 mg/day. The usual effective dose ranges from 400 to 800 mg per day. The maximum daily dose of Kvetiron for the treatment of manic episodes is 800 mg.
Treatment of depressive episodes associated with bipolar disorders. Quetiapine should be used once a day before bedtime. The daily dose in the first 4 days of treatment is: 1st day - 50 mg, 2nd day - 100 mg, 3rd day - 200 mg, 4th day - 300 mg. The recommended daily dose is 300 mg. It is known that during clinical studies there was no additional benefit in the 600 mg group compared to the 300 mg group. A dose of 600 mg may be effective for some patients. Clinical studies show that for individual patients, if problems associated with intolerance to the drug arise, a dose reduction to a minimum of 200 mg may be considered. Treatment for depressive episodes associated with bipolar disorder should be prescribed by a physician experienced in treating bipolar disorder.
Relapse prevention in patients with bipolar disorders. To prevent subsequent manic, depressive or mixed episodes in bipolar disorder, patients who have responded to quetiapine in the acute treatment of bipolar disorder should continue treatment at the same dose. The dose may be adjusted based on the clinical response and tolerability of the individual patient within a daily dosage range of 300 mg to 800 mg given twice daily. It is important that the lowest effective dose is used for maintenance therapy.
Elderly patients
In elderly patients, quetiapine, like other antipsychotics, should be prescribed with caution, especially at the beginning of treatment. A slower dose titration of quetiapine may be necessary and the daily therapeutic dose should be lower than that used in younger patients, depending on the clinical response and tolerability of treatment in the individual patient. The mean plasma clearance of quetiapine was reduced by 30-50% in elderly patients compared to younger patients.
Efficacy and safety were assessed in patients over 65 years of age with depressive episodes as part of bipolar disorder.
Liver and kidney dysfunction
Dose adjustment is not necessary in patients with renal impairment.
Quetiapine is actively metabolized in the liver, so patients with liver failure should use Quetirone with caution, especially during the initial period of treatment.
Patients with impaired liver function should start with a dose of 25 mg/day. The dose is increased daily by 25-50 mg/day until an effective dose is achieved, depending on the clinical response and tolerability of the drug by the patient.
Children. There is insufficient data on the safety and effectiveness of quetiapine to support the use of the drug in children, therefore quetiapine should not be used in pediatric practice.
When can I take the drug, after how long?
Doctors warn against the simultaneous use of antipsychotic substances and alcohol. Therefore, there should be no alcohol in any concentration in the human body.
How soon can you start therapy?
- single use of alcohol – at least 2 days;
- frequent consumption of alcoholic beverages – 1 week;
- alcoholism - treatment in a drug treatment clinic or at home under the supervision of a doctor, at least 5 weeks must pass from the moment the last dose was taken.
If the patient remains in treatment for addiction and is using an antipsychotic, the doctor may periodically order toxicology tests to screen for alcohol.
Comparison of ease of use of Ketilept and Quetiapine
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Ketilept is approximately the same as Quetiapine. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2019-09-19 06:00:34
Quetiapine and beer
Quetiapine and beer are incompatible. The blocking of serotonin, dopamine, and histamine receptors is reduced. Psychosis, schizophrenia worsens, the person will become dangerous to people. An increase in the dose of the drug and plasmapheresis will be required.
Drinking any alcoholic beverages, including beer, is prohibited during therapy with an antipsychotic substance. This will lead to an exacerbation of the underlying disease, new outbreaks of psychosis.
Dyspeptic disorders, abdominal pain, flatulence, and impaired stool formation will appear. The load on the liver increases; alcoholics develop hepatitis, fibrosis, and cirrhosis more quickly.
Organs affected by the toxin
The combined use of pharmacological agents and alcohol has a toxic effect on the internal organs and environments of the body. Alcohol, entering into a chemical reaction with a medicine, leads to poisoning, disrupts physiological processes, enhances or weakens the healing properties of drugs.
The liver suffers more than other organs. She gets hit twice. Many medications have a side effect - hepatotoxicity, destroy cells, and disrupt the physiology of the organ. In the liver, alcohol breaks down to ethanal, a substance 20-30 times more toxic than ethanol, which causes the death of hepatocytes.
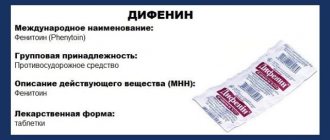
Dangerous groups of drugs for the organ in combination with alcohol:
- anti-inflammatory;
- hormonal;
- antibacterial;
- antifungal;
- glucose control agents for diabetes mellitus;
- anti-tuberculosis;
- cytostatics (chemotherapy drugs);
- tranquilizers (anti-epileptic, psychotropic).
In second place among the internal organs exposed to the harmful effects of alcohol together with medications are the heart and vascular system. Strong drinks during drug therapy constrict blood vessels and increase blood pressure. The simultaneous intake of alcohol and chemical substances leads to failure of the myocardium and increases the risk of developing an attack of angina pectoris and a heart attack.
A mixture of ethanol and pharmaceuticals disrupts the quality of the blood and reduces clotting. This is dangerous due to internal bleeding and strokes.
Comparison of safety of Ketilept and Quetiapine
The safety of a drug includes many factors.
At the same time, in Ketilept it is quite similar to Quetiapine. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing metabolism in Ketilept, as well as in Quetiapine, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Ketilept does not have any risks when used, just like Quetiapine.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of using Ketilept and Quetiapine.
Rules for taking medications and alcohol
Drinking alcohol during treatment minimizes the clinical effect of therapy and creates a risk of developing complications of the disease.
If this cannot be avoided, follow the rules of behavior that will reduce the occurrence of negative consequences:
- Do not drink strong drinks (vodka, cognac, whiskey), choose dry wine (100-150 ml), beer (no more than 300 ml). Don't drink alcohol on an empty stomach.
- The interval between taking the medicine and alcohol should be at least 2 hours.
- To reduce the toxic effect, take medications that protect the liver (hepatoprotectors), pancreas (pancreatin), and stomach (antacids ─ Rennie, Almagel).
If a person takes antiviral medications for colds, anti-inflammatory drugs, alcohol in moderation does not pose a threat to the body.
Alcoholic drinks during treatment are strictly contraindicated in cases of liver cirrhosis, severe infectious diseases, and during a course of chemotherapy.
Comparison of side effects of Ketilept and Quetiapine
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Ketilept's side effects are almost the same as Quetiapine's. They both have few side effects. This implies that the frequency of their occurrence is low, that is, the indicator of how many cases of an undesirable effect of treatment are possible and registered is low. The undesirable effect on the body, the strength of influence and the toxic effect of Ketilept are similar to Quetiapine: how quickly the body recovers after taking it and whether it recovers at all.
Medicines, alcohol and chronic diseases
If a person has chronic diseases, simultaneous use of alcohol and medications is potentially dangerous for the functioning of vital organs. Since patients systematically take prescribed medications, the influence of alcohol can lead to negative consequences.
People with chronic heart disease (angina pectoris, heart defects) develop arrhythmias of varying severity. Heart attacks with severe pain syndrome develop, which is not relieved by Nitroglycerin, and the risk of developing myocardial infarction increases significantly.
In case of chronic liver diseases (viral hepatitis, hepatosis), alcohol during treatment can become a trigger in the development of cirrhosis and hepatocellular carcinoma (cancer).
Drinking alcohol during cirrhosis leads to the following consequences:
- bleeding into the abdominal cavity;
- liver decomposition, infection, peritonitis;
- hepatic coma;
- death.
If a person is on long-term treatment with sedatives, psychotropic drugs, tranquilizers, he is contraindicated in drinking alcohol. This leads to severe depression and the appearance of obsessive states (hallucinations, phobias). Suicidal feelings develop. Such a patient needs constant monitoring and assistance from a psychiatrist.
The most dangerous combinations and consequences
The combination of alcohol and chemical-based drugs can lead to serious disorders in the body, and in some cases to fatal consequences.
List of medications and their side effects in combination with alcohol:
| Name of group, drug | Negative results of interaction |
| Neuroleptics (tranquilizers, anticonvulsants, hypnotics) | Severe intoxication, up to cerebral coma |
| CNS stimulants (Theophedrine, Ephedrine, Caffeine) | Rapid increase in blood pressure, hypertensive crisis |
| Antihypertensives (Captofrin, Enalapril, Enap-N), diuretics (Indapamide, Furosemide) | Sudden drop in pressure, collapse |
| Analgesics, anti-inflammatory | Increased toxic substances in the blood, general poisoning of the body |
| Acetylsalicylic acid (Aspirin) | Acute gastritis, perforation of gastric ulcer and 12-PC |
| Paracetamol | Toxic liver damage |
| Hypoglycemic (Glibenclamide, Glipizide, Metformin, Phenformin), insulin | A sharp decrease in blood sugar levels, hypoglycemic coma |