Difenin (international name Phenytoin) is a drug that was derived from glycolyl urea. The product is used to relax skeletal muscle tissue, reduce its tone, eliminate heart rhythm disturbances, and reduce the occurrence of pain attacks.
The drug also has a pronounced anticonvulsant effect without a hypnotic effect, which distinguishes it from other similar drugs. Reduces the duration of convulsive seizures.
Belongs to the group of antiepileptic drugs.
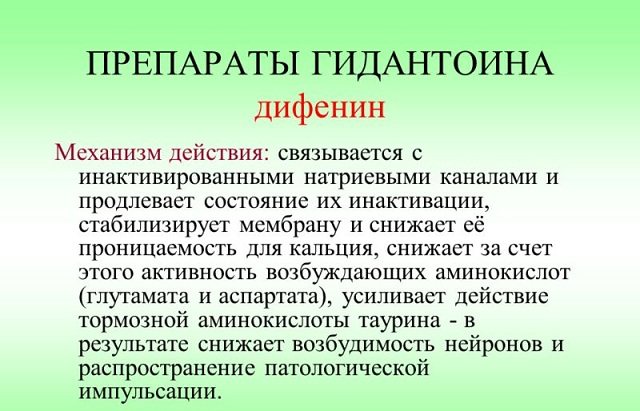
pharmachologic effect
The main disease for which Difenin is used is epilepsy. During attacks of this disease, in the motor cortex of the brain
Phenytoin formula
changes occur, which the main elements of the drug come into play to combat.
Due to the presence of phenytoin, the main component of the drug, the limits of excitability are compensated, resulting in a decrease in sodium, which is located in membrane cells. It is also characterized by a decrease in neural communication potential (NCP).
It is this fact that leads to the fact that in adjacent areas of the cerebral cortex the process of inhibition of epilepsy foci is started. In addition, the main element of the drug has a positive effect on the brain stem, which suppresses the activity of its centers.
This effect has an impact on grand mal seizures, and in particular on their tonic stage.
Pharmacokinetics of the drug
Depending on the regimen of the drug and its dosage, the time of maximum concentration of the active substance in the blood is determined. It ranges from 3-12 hours.
The distribution of medicinal elements of the drug occurs throughout the central nervous system. It also settles in tissues and enters seminal ejaculate, cerebrospinal fluid, bile, saliva, breast milk and digestive juice. Binds to protein in the blood by 70–95%.
The drug is broken down by the liver and forms passive metabolic products. In this case, it is 5-(p-hydroxeryl)-5-phenylhydantoin.
The applied dosage characterizes the elimination time; with a standard dose, this occurs around the clock (+-1 hour). If the medicine has been used for a long time, complete elimination of the substances occurs within 72 hours.
Side effects
When using the drug Difenin, side effects are possible:
CNS and peripheral nervous system:
- mood changes;
- confusion;
- ataxia;
- nystagmus;
- dizziness;
- hand trembling;
- stuttering or slurred speech;
- sleep disorders;
- movement coordination disorder;
- muscle weakness;
- transient nervousness;
- peripheral neuropathy.
Digestive system:
- constipation;
- feeling of nausea;
- toxic hepatitis;
- vomit;
- liver injuries;
- gum hyperplasia - usually occurs within six months of treatment and, as a rule, begins with gingivitis, most often before the age of 23 years.
Hematopoietic systems:
In rare cases:
- granulocytopenia;
- leukopenia;
- megaloblastic anemia;
- agranulocytosis;
- thrombocytopenia;
- pancytopenia.
Endocrine system:
- expansion of the tip of the nose;
- enlargement of facial features;
- hypertrichosis;
- protrusion of the lower jaw;
- thickening of lips
Metabolism:
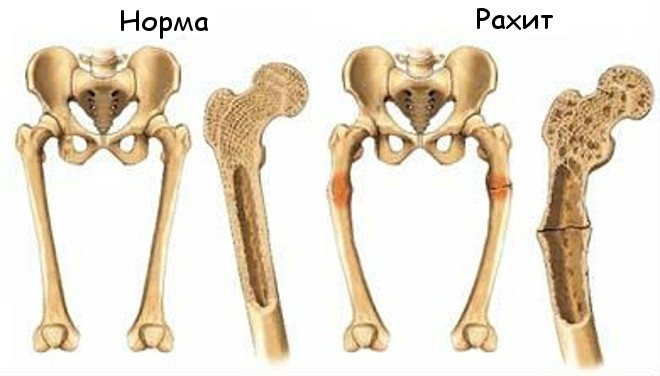
- hypocalcemia;
- vitamin D metabolism disorder;
- due to inhibition of insulin release - impaired glucose absorption.
Musculoskeletal system:
- Dupuytren's contracture;
- peripheral polyarthropathy;
- rickets and osteomalacia - when using the drug for a long period of time in the absence of sufficient solar radiation and a diet that covers the need for vitamin D.
Allergic reactions:
- drug-induced lymphadenopathy;
- fever;
- eosinophilia;
- skin rash due to severe skin reactions (Lyell and Stevens-Johnson syndromes).
Other:
- Peyronie's disease.
Mechanism of action
The active substance of the tablet penetrates into the swollen cells of Purkinje fibers and stabilizes their membrane, which in turn leads to an antiarrhythmic effect. The likelihood of calcium ions entering cells also decreases and transmembrane currents are blocked.
The membrane-stabilizing effect prevents seizures by protecting nerve and muscle cells from prolonged nerve impulses during activation of the body.
Thanks to the hydantoin base, the product serves to enhance the effect of drugs that are used in parallel.
Indications for use
The use of Phenytoin is recommended during the manifestation of diseases with convulsive syndrome:
- major attacks of epilepsy;
- temporal lobe epilepsy;
- epileptic seizures with loss of consciousness or aura;
- deviations of the central nervous system with cardiac dysfunction;
- in case of overdose of cardiotonics;
- trigeminal neuralgia (auxiliary drug);
- Meniere's syndrome.
Article on the topic: Which brewer's yeast is best for weight gain?
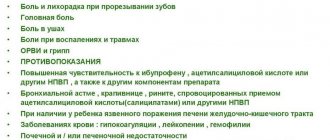
When taking the drug is unacceptable
The drug is not recommended for use in case of hypersensitivity to the component composition, as well as:
- Morgagni syndrome;
- atrioventricular block 2 and 3 degrees;
- sinoatrial heart block;
- bradycardia with decreased heart rate;
- liver and kidney failure;
- chronic alcohol intoxication.
Also, due to the possible loss of NRTI effectiveness, it is not recommended to mix Phenytoin with Delavirdine.
special instructions
If Diphenin is hypersensitive to one of the hydantoin anticonvulsants, hypersensitivity to other drugs in this group is likely.
In epilepsy, sudden cessation of taking Diphenin leads in some cases to the development of withdrawal syndrome; in such cases, anticonvulsants that are not hydantoin derivatives are usually used.
Phenytoin is intensively metabolized in the liver, therefore, patients with functional liver disorders and the elderly should adjust the dosage regimen.
During drug therapy, especially long-term therapy, a diet is necessary that fully satisfies the need for vitamin D directly; exposure to UV radiation is also important.
In relation to children, the use of Diphenin during their growth leads to disorders of the connective tissue.

In acute alcohol intoxication, the plasma concentration of phenytoin may increase, and in chronic alcoholism, it may decrease.
During therapy with Difenin, caution should be exercised when it is necessary to drive vehicles and complex machinery, as well as when performing hazardous types of work, since side effects and decreased reactions are likely when taking the drug.
Instructions for use: regimens and doses
Depending on the degree of manifestation of epilepsy symptoms, take 0.5-1 tablet of Phenytoin 3 times a day. To optimize the patient's condition, the dosage is increased over time to 4 tablets per day. The maximum allowed dose is no more than 8 units in 24 hours and no more than 3 at a time.
Children's dosage (5-9 years) should not exceed 0.5 tablets at a time, no more than 2 times a day. For children over 9 years old, the dosage is determined at the rate of 5-8 mg per 1 kg of body.
For arrhythmia, it is recommended to use no more than 4 tablets per day, taking into account the fact that the first result appears after 4 days of use. After achieving the first effect, the dosage is reduced to 3 tablets.
Also, to achieve quick results when the disease is advanced, there is a developed application regimen:
- 1 day – 2 tablets 4 times a day;
- Day 2 – 1 unit of the drug 5 times a day;
- Day 3 – 1 tablet in 5 doses per day;
- from day 4 until the end of the course - 1 unit of the drug 3 times a day.
To reduce the possibility of an allergic reaction of the mucous membrane to the drug, it must be taken either before or after meals.
Instructions for use of Diphenin
Difenin is available in the form of tablets intended for oral administration. Diphenine is recommended to be taken after meals.
The anticonvulsant and sedative effect is ensured by taking 0.1-0.3 g of the drug 1-3 times a day.
The antiarrhythmic properties of Difenin appear on days 3-5, provided that 0.1 g of the drug is taken 4 times a day . After achieving a therapeutic effect, the daily dose of Diphenin can be reduced to 0.3 g.
For a faster effect (by the end of 1-2 days), the instructions recommend taking Difenin according to the following regimen: on the first day 5 times 0.2 g, on days 2-3 the dose should be reduced to 0.1 g, leaving the same frequency of doses , and from day 4 the number of doses is reduced to 2-3 times a day.
The recommended daily dose of Diphenin for children is 2-4 mg/kg, a subsequent increase in the daily amount of the drug is possible, but not more than 300 mg.
Renal failure is an indication to reduce the daily dose of Diphenin by half.
Overdose and actions for it
An overdose of Diphenin is accompanied by the main symptoms:
- nausea with vomiting;
- trembling in hands;
- visual disturbances;
- toxic hepatitis;
- pendulum involuntary eye movements;
- violation of movement coordination;
- dysarthria;
- loss of consciousness;
- coma, stupor;
- decreased blood pressure;
- respiratory failure;
- sleep apnea;
- appetite suppression;
- constipation;
- lymphadenopathy.
If such symptoms occur, it is necessary to provide the patient with first aid. When a person is in a conscious state, one can limit oneself to gastric lavage and taking sorbents.
Respiratory failure or depression of the cardiovascular system can be eliminated with the help of artificial air carriers. Treatment is based on symptoms only. A universal antidote has not yet been found.
Overdose can occur if the dosage regimen is violated and the permitted dosage is increased. This factor also depends on the amount of phenytoin contained in the blood plasma. For example, involuntary eye movements may occur at a dosage of more than 20 mg, and impaired muscle movement above 30 mg.
Difenin
When used simultaneously with drugs that have a depressant effect on the central nervous system, the depressant effect on the central nervous system may be enhanced.
With the simultaneous use of amiodarone, antifungals (including amphotericin B, fluconazole, ketoconazole, miconazole, itraconazole), metronidazole, chloramphenicol, chlordiazepoxide, diazepam, dicumarol, histamine H1 receptor blockers, halothane, isoniazid, methylphenidate, omeprazole, fluoxet ina , estrogens, salicylates, succinimides, sulfinpyrazone, sulfonamides, tolbutamide, trazodone, it is possible to increase the concentration of phenytoin in the blood plasma, which leads to an increase in its therapeutic effect and increases the risk of side effects.
The therapeutic effect of antifungals, clozapine, GCS, dicumarol, digitoxin, doxycycline, furosemide, estrogens, oral contraceptives, quinidine, rifampicin, vitamin D changes with the simultaneous use of phenytoin.
When used simultaneously with phenothiazine derivatives (including chlorpromazine, prochlorperazine, thioridazine), phenobarbital, and antitumor agents, an increase or decrease in the concentration of phenytoin in the blood plasma is possible. The effect of phenytoin on plasma concentrations of phenobarbital is unpredictable.
When used simultaneously with acetazolamide, osteomalacia and rickets are possible.
When used simultaneously with acyclovir, it is possible to reduce the concentration of phenytoin in the blood plasma and reduce its effectiveness.
With simultaneous use of valproic acid during the first few weeks, the total concentration of phenytoin in the blood plasma may decrease due to its displacement from sites of binding to plasma proteins by sodium valproate, induction of microsomal liver enzymes and acceleration of phenytoin metabolism. Next, the metabolism of phenytoin is inhibited by valproate and, as a result, the concentration of phenytoin in the blood plasma increases. Phenytoin reduces plasma concentrations of valproate, probably by increasing its metabolism in the liver. It is believed that phenytoin, as an inducer of liver enzymes, also increases the formation of a minor but hepatotoxic metabolite of valproic acid.
With simultaneous use, the plasma concentrations of verapamil, nimodipine, and felodipine decrease.
A case has been described of an increase in the concentration of phenytoin in the blood plasma and the development of toxic effects when used simultaneously with gabapentin.
With simultaneous use, a decrease in the concentration of desipramine in the blood plasma is possible.
When used simultaneously with diltiazem and nifedipine, it is possible to increase the concentration of phenytoin in the blood plasma and create a risk of developing toxic effects.
When used simultaneously with disulfiram, it is possible to increase the concentration of phenytoin in the blood plasma with the development of toxic reactions; with imipramine, clarithromycin - it is possible to increase the concentration of phenytoin in the blood plasma.
When used simultaneously with carbamazepine, folic acid, reserpine, sucralfate, vigabatrin, the concentration of phenytoin in the blood plasma may decrease and its therapeutic effect may decrease.
In patients receiving phenytoin, the effectiveness of paracetamol may be reduced.
When taking pyridoxine at a dose of 200 mg/day, a decrease in the concentration of phenytoin in the blood plasma is possible.
When used simultaneously with ritonavir, there are reports of increased plasma concentrations of phenytoin. It is believed that interaction is possible, but its nature has not been definitively established.
When used simultaneously with sucralfate, the absorption of phenytoin is reduced.
When used simultaneously with theophylline, it is possible to reduce the plasma concentrations of phenytoin and theophylline and reduce their effectiveness.
When used simultaneously with felbamate, it is possible to increase the concentration of phenytoin in the blood plasma.
When used simultaneously with phenylbutazone, cases of increased concentrations of phenytoin in the blood plasma with the development of toxic reactions have been described.
When treating folic acid deficiency, the use of folic acid preparations reduces the effectiveness of phenytoin.
When used simultaneously with cimetidine, the concentration of phenytoin in the blood plasma increases, and there is a risk of developing toxic effects.
When used simultaneously with ciprofloxacin, a decrease or increase in the concentration of phenytoin in the blood plasma is possible. The interaction is ambiguous.
Special conditions and instructions
During the course of using the drug, it is recommended to refrain from drinking alcoholic beverages. But if you use Diphenin with alcohol once, the concentration of phenytoin in the blood will increase.
If the functionality of the liver and kidneys fails, consultation with a doctor regarding dosage is necessary.
The drug is prescribed by doctors during pregnancy only when the issue of the mother’s health is higher than the risk to the pregnant child. After childbirth, blood clotting may be impaired.
Use during lactation is prohibited, due to the fact that Diphenin passes into breast milk. This may cause an adverse reaction in the child.
Article on the topic: Very heavy periods - causes and dangerous symptoms, diagnosis, treatment methods and prevention
Interaction with other drugs and substances
Diphenin when taken in parallel with other medications:
- Prolongs the work of Paracetamol.
- Increases the toxicity of Aminazine and other drugs that are based on phenytoazine, sulfanilamide or reserpine.
- St. John's wort reduces the accumulation of phenytoin in plasma. This effect can last for 10-14 days after stopping taking medications with this herb. Sucralfate, vitamin B9, Theophylline, Nelfinavir and Vigabatrin can also affect the decrease in the substance in the blood.
- The cardiodepressive effect is enhanced by the combination of the drug with lidocaine and a β-adrenergic receptor blocker.
- An increase in the amount of phenytoin in the blood is increased by: Dicumarol, Omeprazone, Viloxazine, succinimides, Isoniazid, Diazepam, Golotam, Tolbutamide, Nifedipine, Amiodarone and any antifungal agents.
- The drug reduces the effectiveness of antifungal and antitumor agents. The action of: Methadone, Furosemide, Digitoxin, Clozapine, Paroxetine, estrogens and oral contraceptives is blocked.
- In addition, the drug can affect test results and increase the content of calcium and vitamin B9.
Difenin, 10 pcs., 0.117 g, tablets
During treatment, careful selection of doses is necessary (for epilepsy, the concentration in the blood is determined on the 7-10th day of treatment) since an increase in dose may be accompanied by a disproportionate increase in plasma concentration in the blood.
Most patients maintain stable serum phenytoin concentrations when taking stable doses. However, significant variations in phenytoin serum concentrations may occur in individual patients when equivalent doses are used. A patient with large fluctuations in plasma phenytoin levels despite the use of standard doses presents a challenging clinical problem. Determination of serum levels in such patients is critical. In some cases, the development of an epileptic seizure can be prevented with a serum phenytoin concentration of 6-9 mcg/ml (24-36 μmol/l). Although the relationship between drug concentrations, clinical efficacy and tolerability varies among patients, treatment effectiveness should be assessed by clinical signs of the disease and serum drug concentrations, especially in cases where there is a change in the frequency of attacks, in the treatment of children and adolescents, when the development of toxic reactions and in cases of combined anticonvulsant therapy.
The use of Diphenin in the monotherapy of absence seizures and the prescription of combination therapy in case of joint development of tonic-clonic seizures and absence seizures are not recommended.
Use in patients with porphyria is not recommended, as Difenin can provoke an exacerbation of the disease.
During the treatment period, it is necessary to monitor the content of calcium and phosphorus in the blood serum. With long-term treatment, the development of osteopenia, osteoporosis, osteomalacia is possible due to a decrease in bone mineral density, bone fractures due to the development of hypovitaminosis D, hypocalcemia and hypophosphatemia. The exact mechanism of phenytoin's effect on bone metabolism is unknown; Long-term therapy with phenytoin requires concomitant use of vitamin D supplements.
When using Diphenin in children during the growth period, the risk of developing side effects from connective tissue increases.
When treating with Difenin, at the beginning of therapy monthly, and subsequently every six months, it is necessary to conduct a clinical blood test, liver enzymes, alkaline phosphatase, and also monitor thyroid function. Patients should be informed of the importance of strictly adhering to the prescribed dosage regimen; sudden discontinuation of the drug is unacceptable and may provoke an epileptic attack.
Diphenine should be immediately discontinued if hypersensitivity reactions or symptoms suspected of
indicating the possible development of Stevens-Johnson syndrome or Lyell's syndrome. Drug-induced hypersensitivity syndrome (systemic idiosyncrasy reaction) is a rare but potentially dangerous complication of antiepileptic therapy. Clinical manifestations include fever, maculopapular rash, lymphadenopathy, leukocytosis combined with eosinophilia and/or lymphocytosis. Various organ systems can be involved in the pathological process with the development of hepatitis, nephritis, pneumopathy and others. The syndrome has been described when taking phenytoin, carbamazepine, phenobarbital, valproate (extremely rare).
The etiology and pathogenesis of the development of the syndrome are unknown. The development of the syndrome is most often observed in the period from 2 to 4 weeks from the start of phenytoin therapy, with possible development in the period of 3 or more months from the start of therapy. If the syndrome develops, phenytoin should be discontinued and appropriate therapy prescribed. A higher risk of developing the syndrome is observed in patients with decreased immunity and a history of systemic allergic reactions.
Patients with impaired liver function and the elderly require adjustment of the dosage regimen.
In acute alcohol intoxication, the concentration of phenytoin in the blood increases, and in chronic intoxication it decreases. It is necessary to warn the patient about the need to avoid drinking alcohol-containing drinks during treatment with Diphenin.
When treated with Difenin, toxic effects from the central nervous system may develop if the permissible therapeutic concentration of phenytoin in plasma is exceeded: delirium, psychosis, encephalopathy or, in rare cases, cerebellar dysfunction.
In some cases, treatment with antiepileptic drugs, including Diphenin, was accompanied by the occurrence of suicidal thoughts/attempts. This was also confirmed in a meta-analysis of randomized clinical trials. Epilepsy can also trigger suicidal thoughts. Patients and those around them must be warned about the possibility of suicidal thoughts and, if they occur, they must immediately seek medical help.
Phenytoin may decrease serum T4 concentrations. Phenytoin may lead to increases in serum glucose, alkaline phosphatase and gamma glutamyl transpeptidase (GGT).
Difenin affects glucose metabolism and insulin production; hyperglycemia may develop with toxic concentrations of phenytoin in plasma, so it is impossible to use Difenin in the treatment of seizures against the background of hypoglycemia or seizures caused by metabolic disorders. When treated with antiepileptic drugs, including Diphenin, cases of the development of severe exfoliative dermatitis, accompanied by fever, eosinophilia and systemic manifestations (DRESS syndrome), with the development of life-threatening conditions and death, have been described. Drug-induced hypersensitivity syndrome with eosinophilia (DRESS) is characterized as a life-threatening systemic multiorgan reaction manifested by rashes, fever, lymphadenopathy, leukocytosis with eosinophilia, hepatitis, as well as involvement of other organs, with the development of nephritis, hematological disorders, myocarditis, myositis, etc. . When the first signs appear, it is necessary to immediately conduct a full examination of the patient and stop treatment with Diphenin.
There have been cases of acute hepatotoxicity with the use of phenytoin, manifestations of which may include jaundice, hepatomegaly, high levels of transaminases, leukocytosis and eosinophilia. This can be either one of the manifestations of DRESS syndrome or an isolated syndrome. In such patients, it is necessary to immediately stop therapy with Diphenin.
When using Difenin, changes in the hematopoietic system may occur, including thrombocytopenia, leukopenia, granulocytopenia, agranulocytosis and pancytopenia, sometimes with fatal outcomes. Cases of lymphadenopathy, benign lymph node hyperplasia, pseudolymphomas and Hodgkin's disease have been reported. It is necessary to carefully monitor patients if these reactions develop during phenytoin therapy, and timely correction of therapy. Macrocytosis and megaloblastic anemia are successfully treated with folic acid. If the lymph nodes are affected, fever, rash, and liver damage may occur, but these symptoms may not be present. For any lymphadenopathy, a long period of monitoring the patient's condition is required, with consideration of the possibility of using antiepileptic drugs of other groups.
Influence on the ability to drive vehicles and machinery.
During the treatment period, it is necessary to refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reaction.
Practical application experience
Reviews from patients and doctors who use Difenin in practice.
I have been suffering from epilepsy for several years now, and after seeing a doctor, he prescribed me Difenin. For a long time I was afraid to drink it, because I had heard a lot about its effects and side effects.
The doctor personally prescribed the dosage and regimen for use with other tablets. I was positively surprised by the effect. The attacks began to appear less frequently. Tell me, what else can this drug be combined with in order to achieve complete elimination of epilepsy?
Polina Selezneva
I have epileptic seizures. I didn’t go to the doctor, but when I heard Phenytoin I decided to try taking it. I went to the pharmacy and it was only available with a prescription. After another attack (2 times a month), I decided to go to the hospital. The doctor also suggested taking Difenin with Finlepsin (400 mg). After a month of use, the attacks subsided. But they didn't disappear.
Nikita Sergeev
I prescribe the drug to epileptics as the main drug. But to be honest, I don’t risk prescribing it to children. Once prescribed it to a 9-year-old boy in a minimal dose (half a tablet per day), after two days of use he developed side effects (respiratory suppression and vomiting). Although the adult body always perceives it with a bang. Here you can safely bet 4+.
It is also not recommended to take the drug for people with periodontal disease and stomatitis. Diphenin can aggravate these diseases.
I don’t recommend driving after taking it, the side effects appear suddenly.
Teplov Alexander Sergeevich, neurologist
I consider Diphenin a good product that corresponds to trends in price and quality. Basically, such products are very expensive. The same drug costs between 200-250 rubles, which makes it affordable for people. Of course, there are stronger drugs. I always prescribe them in pairs.
Nevbiraka Sergei Ilyich