| Paroxetine | |
| Chemical compound | |
| IUPAC | (3S-trans)-3-((1,3-Benzodioxol-5-yloxy)methyl)-4-(4-fluorophenyl)-piperidine |
| Gross formula | C19H20FNO3 |
| Molar mass | 374,8 |
| CAS | 61869-08-7 |
| PubChem | 43815 |
| DrugBank | APRD00364 |
| Classification | |
| Pharmacol. group | antidepressants |
| ATX | N06AB05 |
| Pharmacokinetics | |
| Bioavailable | completely absorbed in the gastrointestinal tract. The time to reach Cmax in the blood is 5.2 hours. |
| Metabolism | in the liver with the formation of inactive metabolites. It is an inhibitor of the CYP2D6 isoenzyme. |
| Half-life | 24 hours (from 3 to 65 hours) |
| Excretion | 66% with urine, 37% - through the gastrointestinal tract (unchanged - 2% and 1%, respectively) |
| Dosage forms | |
| film-coated tablets. | |
| Methods of administration | |
| orally | |
| Other names | |
| Paroxetine, Rexetine, Paxil, Paroxin, Seroxat, Adepress, Actaparoxetine, Plizil, Paroxetine hydrochloride hemihydrate, Sirestill | |
| Media files on Wikimedia Commons | |
Paroxetine
is an antidepressant with a strong anti-anxiety effect, a selective serotonin reuptake inhibitor (SSRI).
Developed and patented by the Danish company A/S Ferrosan (in the UK - in 1973, in the USA - in 1977, base and maleate), currently, due to the expiration of patent protection, it has moved into the category of generics[1], included in WHO VED list[2].
The antidepressant sertraline has a similar but less potent anti-anxiety effect to paroxetine.
Mechanism of action
It is the most potent serotonin reuptake inhibitor of all SSRIs[4][5]. It has weak, although much greater than other SSRI antidepressants, agonism to norepinephrine receptors; also has low affinity for dopaminergic and histamine (H1) receptors and some similarities with tricyclic antidepressants with a significantly lower ability to cause their characteristic side effects on the central nervous system and the autonomic nervous system. Shows affinity for muscarinic acetylcholine receptors, although to a significantly lesser extent than tricyclic antidepressants[5], as well as low affinity for α1-, α2- and β-adrenergic receptors.[6]
Binding constants:[7][8]
- SERT (Ki = 0.08 nM)
- NET (Ki = 56.7 nM)
- DAT (Ki = 573.7 nM)
The presence of a cholinolytic effect in paroxetine leads to the fact that when taken, a rapid reduction of anxiety and insomnia occurs, while the initial activating effect characteristic of the SSRI group is less pronounced, and side effects such as vomiting or diarrhea are less pronounced. Accordingly, this antidepressant may be preferable in the treatment of anxiety-phobic disorders and anxious depression, but will be less tolerated if the structure of the depressive disorder includes severe mental and motor inhibition [9].
The ability of paroxetine in high doses to inhibit dopamine reuptake makes it similar to sertraline. However, while the beneficial effect of sertraline on cognitive function is associated with the effect on dopamine reuptake, paroxetine, on the contrary, can cause cognitive impairment. Apparently, this is due to its rather pronounced anticholinergic properties and weaker effect on dopamine receptors compared to sertraline [10].
Overdose
Symptoms: nausea, vomiting, severe dry mouth, severe drowsiness, irritability, sinus tachycardia, tremor, dilated pupils.
Treatment: symptomatic. To remove the unabsorbed part of the drug from the stomach, it is necessary to induce vomiting or perform gastric lavage. No specific antidote has been found. Forced diuresis, hemodialysis, hemoperfusion and exchange transfusion are ineffective (due to the large volume of distribution and high degree of binding to plasma proteins).
The maximum dosage of paroxetine is 60 mg per day, which is equivalent to three tablets of the drug. If this dose is exceeded, an overdose may develop. The latter is accompanied by a decrease in blood pressure, dry mouth, nausea, palpitations, tachycardia, and aggressiveness. The patient's pupils dilate and an irresistible desire to sleep arises. Impaired consciousness may develop, leading to coma*.
https://www.youtube.com/watch?v=ytabout
There is no specific treatment for paroxetine overdose. To relieve an acute condition, general methods of treatment are used: gastric lavage, enema, ingestion of sorbents, detoxification infusion therapy. If symptoms of overdose are detected, you must call an ambulance.
Side effects
Side effects of paroxetine include:
From the side of the central nervous system:
headache, nervousness, paresthesia[11], sleep disturbances[12], insomnia[13], agitation, unusual dreams, anxiety, asthenia, stimulation, depersonalization, depression, myoclonus, drowsiness, emotional lability, tremor, convulsions, memory impairment and concentration, dizziness, rarely - thinking disorders, akinesia, hyperkinesia, ataxia, convulsions, grand mal seizures, paranoid reactions, delirium, euphoria, aggressiveness, nystagmus, stupor, autism[14], extrapyramidal disorders, in particular akathisia[15] and orofacial dystonia[16], in extremely rare cases, hallucinations[6].
From the autonomic nervous system:
increased sweating, dry mouth[6].
From the senses:
disturbances of accommodation, dilated pupils, pain in the eyes, noise and pain in the ears, rarely - decreased visual acuity, cataracts, conjunctivitis, glaucoma, exophthalmos[14].
From the cardiovascular and lymphatic system:
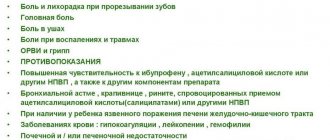
in rare cases, hypertension, tachycardia, bradycardia, hematomas, hypotension, orthostatic hypotension, anemia, leukopenia, lymphadenopathy, purpura; increased risk of bleeding, especially when taking aspirin, non-steroidal anti-inflammatory drugs, warfarin and other anticoagulants simultaneously with paroxetine [6].
From the endocrine system:
hyperprolactinemia[17].
From the reproductive and urinary system:
decreased libido[11], urinary disorders, sexual disorders (including ejaculation disorders and impotence)[6].
From the digestive system:
nausea, decreased appetite, vomiting, constipation, diarrhea[6], clinically significant weight gain[18], dyspepsia[12]; in rare cases, hepatotoxic effect: increased transaminase levels, cholestatic and hepatocellular lesions[19][20].
From the respiratory system:
respiratory disorders, rhinitis, sinusitis.
Other:
allergic reactions, chills, facial swelling, malaise, neck pain, migraine, fainting[6].
When using paroxetine, in rare cases even at a therapeutic dose and most often with the concomitant use of tryptophan, tramadol, triptan, lithium, irreversible MAO inhibitors or other drugs that affect serotonin metabolism, the risk of a potentially fatal side effect - serotonin syndrome - cannot be excluded.
In rare cases, paroxetine can induce mania or hypomania in both patients suffering from unipolar depressive disorder and patients with bipolar affective disorder.
It is possible, especially in the first stage of treatment or when adjusting the dose down or up, anxiety, agitation, panic attacks, irritability, hostility, impulsivity, other unusual changes in mental state, increased depression or suicidal thoughts [6]. Paroxetine is associated with an increased risk of suicide in different age groups[21][22]: youth[23][22], adolescents[24] and adults[21][25][22].
Taking fluoxetine and paroxetine (but not other SSRIs) in the first trimester of pregnancy increases the risk of fetal heart problems[26].
Addiction and withdrawal symptoms
Systematic studies of paroxetine in animals and humans regarding its abuse potential, tolerance, and potential for physical dependence have not been conducted. Although clinical studies have not identified trends in drug dependence, these observations have not been systematic, and it is not possible to draw conclusions from such limited results as to the extent to which a CNS-active drug will be abused, misused, or marketed. Therefore, patients should be carefully assessed for a history of drug dependence, and if identified, patients should be closely monitored for off-label use or abuse of Paxil (eg, development of tolerance, dosage escalation, drug dependence)[6].
Paroxetine therapy should be discontinued gradually due to the risk of withdrawal syndrome, which is more common than with other SSRIs[27][28] and is characterized by dizziness, headache, nausea, vomiting, diarrhea, fatigue, unsteadiness of gait, flu-like symptoms, anxiety, irritability, insomnia, lethargy, emotional lability, hypomania, tremor, fever and chills, in rare cases, paresthesia and visual disturbances [6][28][29][30].
Overdose
The most common symptoms of paroxetine overdose include drowsiness, coma, nausea, tremors, tachycardia, confusion, vomiting, and dizziness; in addition, dilated pupils, convulsions (including status epilepticus), ventricular dysrhythmia, hypertension, aggressive reactions, fainting, hypotension, stupor, bradycardia, dystonia, rhabdomyolysis, liver dysfunction (including liver failure, hepatic necrosis, jaundice, hepatitis, hepatic steatosis), serotonin syndrome, manic reactions, myoclonus, acute renal failure and urinary retention.
Treatment:
gastric lavage and use of activated carbon; ensuring the conductivity of the respiratory tract, oxygenation and ventilation of the lungs; tracking heart rate and other vital signs; supportive and symptomatic measures[6].
Directions for use and dosage
Paxil is intended for oral use, the recommended starting dose is 20 mg once in the morning with food. The tablet is drunk whole, without chewing.
During treatment with Paxil, the dosage is selected individually for each individual patient based on clinical symptoms. The correct dose is established during the first 2-3 weeks of therapy by a qualified specialist.
Therapeutic treatment, as a rule, is long-term, this is necessary to relieve mental disorders. When treating depression, the course of therapy can last several months continuously, obsessive-compulsive and panic disorders are treated even longer.
It is not recommended to suddenly stop taking antidepressants, as this may lead to drug withdrawal syndrome.
To relieve depressive disorders, the optimal initial dosage is 20 mg/day, which must be increased (adding 10 mg each) until a lasting therapeutic effect is obtained. The maximum daily dose is 50 mg.
Panic disorders: the recommended initial dosage is 10 mg, with a gradual increase weekly (by 10 mg) until the desired effect is obtained. The optimal dosage is 40 mg per day. Maximum - 50 mg/day. Improvement in the condition of such patients is only possible when taken at the maximum dosage (50 mg). To relieve symptoms in the early stages, the minimum dosage is used.
Obsessive-compulsive disorders - initial dose - 20 mg, then gradually increase (10 mg more weekly) to 40 mg / day in two doses. The maximum permissible dosage is 60 mg. In some patients, a stable therapeutic effect can be achieved using the maximum dosage per day.
In the presence of post-traumatic, generalized disorders and social phobias, the dosage is selected individually, initially 10 mg/day. with a weekly increase to 50 mg/day, the dose may be lower if a positive effect occurs when using lower doses.
The treatment regimen and duration of treatment can be prescribed by the treating specialist for each patient individually. Paxil can be used long-term, as well as for prophylactic purposes. Before use, please read the attached leaflet.
Contraindications
Concomitant treatment with MAO inhibitors[14], manic states[31], poisoning with alcohol, psychotropic drugs and other drugs[32], renal, liver failure, breastfeeding period, hypersensitivity to the drug, attack of glaucoma, age less than 15 years[12] .
It is not recommended for use in pediatric practice due to the high risk of undesirable clinical outcomes, including self-aggressive behavior[33][34], the occurrence of severe aggressiveness and increased depression[35], as well as for use during pregnancy and conception due to the risk of congenital malformations[36].
Paxil: Analogs
Structural analogues of the active substance:
Paroxetine hydrochloride hemihydrate, Adepress, Plesil, Rexetine, Sirestill.
These drugs have the same composition; for more detailed information, you can study patient reviews.
Currently, there are medications similar to the drug Paxil in their action.
In the pharmacy chain, you can separately purchase medications with a similar composition, for example, analogues in the pharmacological group (thymoanaleptics): Amitriptyline, Oprah, Clominal, Duloxetine, Miracitol, Fevarin, Deprenon, Amizol, Pyrazidol, Efevelon, Amixid, Clomipram, Negrustin, Velaxin, Venlafaxine, Lenuxin, Fluoxetine, Triptisol; ;Fluoracisin, Heptral, Deprex, Doxepin, Zoloft, Neuroplant, Clomipramine, Coaxil, Lerivon, Prodep, Miansan, Tsipralex, Mirzaten, Prozac, Citalopram Tsipramil, Mirtalan, Stimuloton, Framex, Sedopram, Profluzac, Remeron, Noxibel, Elivel
It is highly not recommended to independently replace Paxil with other medications that are similar in action; this requires consultation with a treating psychiatrist.
Drug interactions
Paroxetine is not combined with irreversible and reversible MAO inhibitors, tryptophan, warfarin; It is also not recommended to combine with nortriptyline, imipramine, desipramine, trazodone, bupropion[12]. The interval after stopping taking MAO inhibitors before starting paroxetine (as well as the interval after stopping taking paroxetine before starting MAO inhibitors) should be at least 14 days [14].
In combination with mirtazapine, it may enhance the effect of both drugs. Such combinations of several antidepressants are used for difficult-to-treat depression.
Increases the concentration (with the risk of increased side effects[37]) of tricyclic antidepressants, anticonvulsants, barbiturates[12], indirect anticoagulants, phenothiazine neuroleptics, 1C antiarrhythmic drugs, metoprolol[37]. When paroxetine is used in combination with atypical antipsychotics, phenothiazine antipsychotics, tricyclic antidepressants, NSAIDs (including acetylsalicylic acid), a blood clotting disorder is possible [37].
The simultaneous use of paroxetine and serotonergic drugs (tramadol, sumatriptan) may lead to increased serotonergic effect. Mutual enhancement of the effects of paroxetine, lithium and tryptophan was also noted [37].
Sodium valproate slows down the metabolism of paroxetine and increases its concentration in the blood[38].
Concomitant use of paroxetine with antipsychotics may increase the risk of extrapyramidal symptoms[39] and neuroleptic malignant syndrome[37].
Paroxetine may increase the severity of psychomotor impairment if it is used in conjunction with benzodiazepine tranquilizers[39].
Increases bleeding when taken simultaneously with indirect anticoagulants [3].
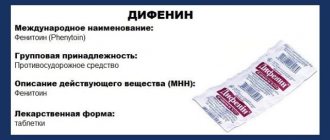
Inducers of microsomal oxidation (barbiturates, diphenine) reduce, and inhibitors (cimetidine) increase the concentration of paroxetine in the blood [3].
Compound
The drug contains the main active ingredient and a number of excipients.
The first has the main therapeutic effect. The active ingredient of the drug is paroxetine. In this case, the drug is named after the active substance, like most original medicines. Excipients do not have an effect on the body, but facilitate the entry of paroxetine into the body. Auxiliary ingredients include the following: cellulose, calcium, magnesium, sodium compounds and silicon dioxide. All of them are contained in negligible concentrations.
Alternative drugs
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on May 12, 2011 . |
The antidepressant sertraline, which also belongs to the SSRI group, has a similar but less pronounced effect with less side effects.
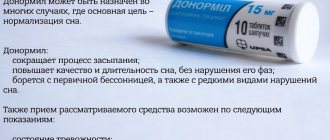
An alternative to paroxetine for treating anxiety may be tranquilizers such as Grandaxin. Tranquilizers do not have significant side effects and are suitable for a one-time fight against anxiety: at your own wedding, exams, public speaking. Paroxetine and sertraline are used for long-term severe anxiety disorders such as panic attacks.
For depression without the anxiety component, paroxetine is preferred over newer antidepressants such as duloxetine (Cymbalta) and milnacipran (Ixel) because they act simultaneously on serotonin and norepinephrine and cause fewer side effects.
Criticism
Main article: Selective serotonin reuptake inhibitors § Criticism
In 2006, GlaxoSmithKline, the company that makes the drug, reported that taking paroxetine was associated with an increased risk of suicide. Several dozen lawsuits were brought against the company by victims and their family members. Lawyers for the injured parties managed to gain access to the company’s internal documentation and, based on its study, concluded that GlaxoSmithKline back in 1989 had information about an eightfold increase in the risk of suicide when taking its drugs[40]; however, the company kept this data silent for a long time[41].
The 1,374 letters from viewers (mostly patients) received by the BBC following its 2002 program on paroxetine involved acts of violence or self-harm occurring at the start of treatment with the drug or immediately after increasing its dosage. As noted by D. Healy, A. Herxheimer, DB Menkes (2006), these data cannot be considered just individual reports, since the analysis clearly indicates the connection of these actions with dosage; in addition, self-reports of acts of violence were provided by patients who were not previously prone to violent acts.[42]
According to some reports, paroxetine withdrawal symptoms can be so persistent that in these cases patients have to reduce their dosage very slowly. It was found that, according to the results of GlaxoSmithKline's own studies, withdrawal symptoms occurred in the majority of healthy volunteers taking paroxetine[43]. According to WHO, patients taking paroxetine have the most severe withdrawal problems compared to patients taking other antidepressants. GlaxoSmithKline for a long time denied the problem of addiction to paroxetine. In 2002, the FDA issued a warning and the International Federation of Pharmaceutical Manufacturers' Associations announced on US television that GlaxoSmithKline was guilty of misleading the public about paroxetine. In 2003, Glaxo, in fine print, rewrote previous estimates of the risk of withdrawal reactions in the labels from 0.2% to 25%[41].
A systematic review of 29 published and 11 unpublished clinical studies (reviewed by C. Barbui, T. Furukawa, A. Cipriani, 2008) found that paroxetine was not superior to placebo in terms of overall treatment efficacy and tolerability. These results were not biased by selective selection of published studies.[25]
Another review, conducted by the famous American psychologist Irving Kirsch and including data from 42 clinical trials of 6 antidepressants, including paroxetine (some of these studies were previously unpublished and were ignored), showed that the difference between drugs and placebo on average was only 1 .8 points on the Hamilton scale - the difference, although statistically significant, has no clinical significance.[44] According to another study conducted by Kirsch et al (a meta-analysis of 35 clinical trials of 4 antidepressants, including paroxetine), the difference between antidepressants and placebo reached clinical significance only in very severe depression [45]. The results of Kirsch's research caused widespread resonance and were discussed both in scientific journals and in the popular media[46].
Data regarding the effectiveness of paroxetine in children and adolescents are also questionable. Thus, in 2001, GlaxoSmithKline published the results of Study 329, which purported to show that Paxil (Seroxat) was an effective drug when used in this age group. The study became widely known and cited, having been cited no less than 184 times by 2010. GlaxoSmithKline even told its own sales representatives that the 329 trial "showed remarkable efficacy." In fact, the company’s internal documents admitted that the drug’s effectiveness had not been proven. In fact, Study 329 was negative for effectiveness on all eight outcomes and positive for demonstrating harm, but these facts were distorted by manipulation of the data, and the published paper of shadow authorship (with as many as 22 “authors”) ended up reporting positive effects . The New York State Attorney General sued GlaxoSmithKline in 2004 for deceiving consumers about the harms caused by paroxetine, leading to the disclosure of company records as part of the settlement. In addition to the findings that paroxetine was ineffective, it was found that at least eight children became suicidal while taking the drug, compared with only one in the placebo group. However, in an article published on the results of Study 329, five cases of suicidal ideation and behavior were defined as “emotional lability”, and three additional cases of suicidal ideation and self-harm were called “hospitalization”[41].
Four of GlaxoSmithKline's five studies of paroxetine in children and adolescents, which did not show paroxetine to be effective and demonstrated a possible increased risk of suicidal ideation and behavior, were not published.[47] Due to the suppression of data on paroxetine, which showed that the drug caused severe side effects in children, an unprecedented four-year investigation was launched in the UK in 2004. This investigation into the circumstances surrounding the marketing of paroxetine was the largest ever conducted by the UK Medicines and Healthcare Products Regulatory Agency in connection with a drug safety review[48].
Arthrocin (ointment, gel, cream, tablets): instructions, reviews of use
Have you been trying to heal your JOINTS for many years?
Head of the Institute for Joint Treatment: “You will be amazed at how easy it is to heal your joints by taking every day...
Read more "
Arthrocin is a dietary supplement whose main active ingredient is chondroitin sulfate. The chondroprotector slows down the progression of pathologies of the musculoskeletal system and has a beneficial effect on the condition of bone tissue, which is possible due to the additional enrichment of the body with vitamins.
The action of the drug is to normalize the process of producing synovial fluid inside the joint. This allows you to significantly increase your mobility and reduce the harmful effects of heavy physical activity.
Arthrocin will be most effective in getting rid of radiculitis, osteochondrosis, arthrosis and manifestations of rheumatic joint pathologies.
Release form and features of the drug
The manufacturer offers patients to purchase Arthrocin in several release forms. The composition and amount of active ingredient in each version of the product are different. So, it could be:
- gel (50 ml tube). It consists of bee honey, vitamin P, essential oils of rosemary, lavender, wormwood, natural extracts of laurel, hop cones, bergenia root;
- cream (50 ml tube). Made from petroleum jelly and olive oil, honey, beeswax, vitamins D, PP, B, arnica extracts, white willow bark, fir, coriander, wild rosemary, St. John's wort, hellebore, immortelle, knotweed, nettle, bearberry, lavender essential oil;
- tablets (12 pieces in a blister, 1.6 g each). They consist of chondroitin sulfate, ascorbic acid, calcium carbonate, glucosamine, vitamin E, dihydroquercetin. Additionally, the tablets are enriched with extracts of medicinal herbs: horsetail, white willow bark, dandelion;
- capsules (12 pieces in a blister, 0.5 g each) have a composition similar to tablets.
How to use?
The drug Arthrocin is not a means of independent action, but only one of the components of an integrated approach to the treatment of pathologies of bones and joints. Depending on the form of release, the methods of its use will be differentiated.
Tablets and capsules are indicated for adults and children over 12 years of age. In this form, the drug should be consumed strictly with meals twice a day. If the patient is recommended to take a medicine with a stronger composition (Forte), then a single dose per day will be sufficient.
Every patient who is treated with Arthrocin should know that it is important, even in the absence of visible results, not to stop treatment. Only after completing the entire course can you achieve:
- returning the elasticity of cartilage tissue;
- improving joint mobility;
- relieving swelling;
- reducing the manifestations of the inflammatory process.
Arthrocin gel and Arthrocin cream are applied directly to the affected joint. The number of such applications per day should not be more than 3. The course of therapy will be from 3 to 6 months, after which it is recommended to take a break and repeat the treatment.
Due to the fact that this drug is a dietary supplement, it, like other chondroprotectors, acts slowly and requires long-term use.
Contraindications, adverse reactions, cases of overdose
Despite the fact that the drug has a natural composition, it may not be indicated for all patients. So, it should not be used in the following cases:
- pregnancy and breastfeeding (due to lack of experience in using the product in this group);
- children under 12 years of age;
- individual intolerance to the components of the drug.
As for adverse reactions, according to the latest medical studies, regardless of the form of release, the drug is well tolerated by patients. Thanks to the natural ingredients, Arthrocin gel, Arthrocin cream, capsules and tablets are not capable of causing irritation.
With oral and external use, no side effects on the body were noted. An exception is situations in which the patient has a predisposition to allergic reactions and is particularly sensitive to bee products.
If there has been excessive ingestion of the drug, attacks of nausea and vomiting may develop. No specific treatment is provided in this case.
special instructions
Tablets, capsules and other forms of Arthrocin combine well with other medications. However, despite the fact that you can buy it without a prescription, self-medication is not recommended.
Do not allow the ointment or gel to come into contact with mucous membranes, eyes or open wounds.
The same banned issue for which Ernst fired Malakhov!
Joints and cartilage will be cured in 14 days with the help of ordinary...
Store the drug at a temperature not exceeding 15 degrees. From the date of manufacture it is suitable for use for 2 years.
At the moment, the chondroprotector Arthrocin has no direct analogues. There are only medications that are similar in their mechanism of action on the musculoskeletal system.
Depending on the region and the trade markup, a 50 ml cream and ointment will cost the patient between 130-180 rubles; for 35 tablets and capsules you will have to pay from 200 to 250 rubles.
Notes
- Trends in Drug Patenting - Case Studies: THE CASES: 1. PAROXETINE // WHO, 2001. Retrieved March 16, 2012. Archived June 24, 2012.
- WHO | Paroxetine hydrochloride (Inclusion). Essential medicines selection, 17th Expert Committee on the Selection and Use of Essential Medicines (2009). Retrieved March 16, 2012. Archived June 24, 2012.
- ↑ 12345
Paroxetine // Medicines / M. D. Mashkovsky. — Mashkovsky’s directory on-line. - Marks DM, Park MH, Ham BJ, Han C, Patkar AA, Masand PS, Pae CU. (November 2008). "Paroxetine: safety and tolerance issues." Expert Opin Drug Saf 7
(6):783–94. PMID 18983224. - ↑ 1 2
Bourin M, Chue P, Guillon Y. (Spring 2001).
"Paroxetine: a review." CNS Drug Rev 7
(1):25–47. PMID 11420571. - ↑ 1234567891011
PAXIL (paroxetine hydrochloride) Tablets and Oral Suspension: PRESCRIBING INFORMATION (PDF). Research Triangle Park, NC: GlaxoSmithKline (August 2007). Retrieved August 14, 2007. Archived August 25, 2011. - Roth, B.L.;
Driscol, J. PDSP Ki Database.
Psychoactive Drug Screening Program (PDSP)
. University of North Carolina at Chapel Hill and the United States National Institute of Mental Health (January 12, 2011). Retrieved November 22, 2013. - Brunton, L;
Chabner, B; Knollman, B. Goodman and Gilman's The Pharmacological Basis of Therapeutics. — 12th. - New York: McGraw-Hill Professional, 2010. - ISBN 978-0-07-162442-8. - Drobizhev M.Yu., Mukhin A.A.
Selective serotonin reuptake inhibitors: options for choice (comments on the works of Thase et al.) // Psychiatry and psychopharmacotherapy. - 2004. - T. 6, No. 1. - Ushkalova E.A., Ushkalova A.V.
Pharmacotherapy of depression in cardiac patients // Difficult Patient. - 2006. - No. 1. - ↑ 1 2
Aursnes I, Gjertsen MK.
(July 2008). "Common adverse events associated with an SSRI: meta-analysis of early paroxetine data." Pharmacoepidemiol Drug Saf 17
(7):707–13. PMID 18383561. - ↑ 1 2 3 4 5 Podkorytov V. S., Chaika Yu. Yu.
Depression. Modern therapy. - Kharkov: Tornado, 2003. - 352 p. — ISBN 966-635-495-0. - Grimsley SR, Jann MW. (November 1992). "Paroxetine, sertraline, and fluvoxamine: new selective serotonin reuptake inhibitors." Clin Pharm 11
(11):930–57. PMID 1464219. - ↑ 1 2 3 4 5 Gubsky Yu. I., Shapovalova V. A., Kutko I. I., Shapovalov V. V.
Medicines in psychopharmacology. - Kyiv - Kharkov: Health - Torsing, 1997. - 288 p. — 20,000 copies. — ISBN 5-311-00922-5, 966-7300-04-8. - Baldassano CF, Truman CJ, Nierenberg A, Ghaemi SN, Sachs GS (March-April 1996). "Akathisia: a review and case report following paroxetine treatment." Compr Psychiatry 37
(2):122–4. PMID 8654061. - Ener RA, Meglathery SB, Van Decker WA, Gallagher RM
Serotonin syndrome and other serotonergic disorders. (English) // Pain medicine (Malden, Mass.). - 2003. - Vol. 4, no. 1. - P. 63-74. - PMID 12873279. [correct] - Torre D, Falorni A.
Pharmacological causes of hyperprolactinemia // Ther Clin Risk Manag. - Oct 2007. - T. 3, No. 5. - P. 929-951. - Papakostas GI. (2008). "Tolerance of modern antidepressants". J Clin Psychiatry 69
(E1):8–13. PMID 18494538. - Colakoglu O, Tankurt E, Unsal B, Ugur F, Kupelioglu A, Buyrac Z, Akpinar Z (July 2005). "Toxic hepatitis associated with paroxetine." Int J Clin Pract 59
(7):861–2. PMID 15963219. - Guzmán Ruiz O, Ramírez Martín del Campo M, Fernandez López I, Romero Gómez M (March 2005). "Hepatotoxicity induced by paroxetine." Med Clin (Barc) 19
(124(10)): 399. PMID 15766517. - ↑ 1 2 Aursnes I., Tvete IF, Gaasemyr J., Natvig B.
Even more suicide attempts in clinical trials with paroxetine randomized against placebo. (English) // BMC psychiatry. - 2006. - Vol. 6. - P. 55. - DOI:10.1186/1471-244X-6-55. - PMID 17129393. [correct] - ↑ 123
Paxil (paroxetine hydrochloride) Tablets and Oral Suspension. FDA (05/12/2006). - Tang SW, Helmeste D. (April 2008). "Paroxetine". Expert Opin Pharmacother 9
(5):787–94. PMID 18345955. - Bauer MS, Wisniewski SR, Kogan JN, Marangell LB, Thase ME, Sachs G. (2006). "Brief report: paroxetine in younger and adult individuals at high risk for suicide." Psychopharmacol Bull 39
(1):31–7. PMID 17065973. - ↑ 1 2
Barbui C, Furukawa TA, Cipriani A (January 2008).
"Effectiveness of paroxetine in the treatment of acute major depression in adults: a systematic re-examination of published and unpublished data from randomized trials." CMAJ 178
(3):296–305. DOI:10.1503/cmaj.070693. PMID 18227449. - Paroxetine (Paxil) and fluoxetine (Prozac) can cause fetal development disorders // Moscow Regional Psychiatric Newspaper. — January — February 2009 — No. 1 (45).
- Rosenbaum JF, Fava M, Hoog SL, Ascroft RC, Krebs WB (July 1998). "Selective serotonin reuptake inhibitor discontinuation syndrome: a randomized clinical trial." Biol. Psychiatry 44
(2):77–87. PMID 9646889. - ↑ 1 2
Black K, Shea C, Dursun S, Kutcher S (May 2000).
"Selective serotonin reuptake inhibitor discontinuation syndrome: proposed diagnostic criteria." J Psychiatry Neurosci 25
(3):255–61. PMID 10863885. - Belloeuf L, Le Jeunne C, Hugues FC (April 2000). "Paroxetine withdrawal syndrome". Ann Med Interne (Paris) 151
(124(10)): 399. PMID 10855379. - Renoir T.
Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. (English) // Frontiers in pharmacology. — 2013. — Vol. 4. - P. 45. - DOI:10.3389/fphar.2013.00045. - PMID 23596418. [correct] - ↑ 12
Reference Guide to Psychopharmacological and Antiepileptic Drugs Approved for Use in Russia / Ed. S. N. Mosolova. — Ed. 2nd, revised - M.: BINOM Publishing House, 2004. - P. 139-140. — 304 p. — 7000 copies. — ISBN 5-9518-0093-5. - Puzhinsky S.
Pharmacotherapy of depressive states // Depression and comorbid disorders / Ed. Smulevich A.B. - M., 1997. - Hammad TA, Laughren T, Racoosin J (March 2006). "Suicidality in pediatric patients treated with antidepressant drugs." Arch. Gen. Psychiatry 63
(3):332–9. DOI:10.1001/archpsyc.63.3.332. PMID 16520440. - Report of the CSM expert working group on the safety of selective serotonin reuptake inhibitor antidepressants (PDF). MHRA (December 2004). Retrieved February 17, 2009. Archived August 25, 2011.
- Glaxo releases classified materials
- Thormahlen GM (October 2006). "Paroxetine use during pregnancy: is it safe?". Ann Pharmacother 40
(10):1834–7. PMID 16926304. - ↑ 12345
Rational pharmacotherapy in psychiatric practice: a guide for practitioners / Ed. ed. Yu. A. Alexandrovsky, N. G. Neznanov. - Moscow: Litterra, 2014. - 1080 p. — (Rational pharmacotherapy). — ISBN 978-5-4235-0134-1. - Malin D.I.
Drug interactions of psychotropic drugs (Part II) // Psychiatry and psychopharmacotherapy. - 2000. - ↑ 1 2 Minutko V.L.
Depression. - Moscow: GEOTAR-Media, 2006. - 320 p. — 2000 copies. — ISBN 5-9704-0205-2. - For 15 years, a large pharmaceutical company hid data on the relationship between an increased risk of suicide and the use of its antidepressant (February 13, 2008). Source: New Scientist magazine, 06 February 2008, page 12.
- ↑ 1 2 3 Goetsche P.
Deadly drugs and organized crime: How Big Pharma corrupted healthcare / [Trans. from English L. E. Ziganshina]. - Moscow: Publishing House "E", 2020. - 464 p. — (Evidence-based medicine). — 3000 copies. — ISBN 978-5-699-83580-5. - Healy D, Herxheimer A, Menkes DB.
Antidepressants and Violence: Problems at the Interface of Medicine and Law // PLoS Med. - 2006. - T. 3, No. 9. - DOI:10.1371/journal.pmed.0030372. - The secrets of seroxat // BBC News / Programs / Panorama. See more details: https://news.bbc.co.uk/2/shared/spl/hi/programmes/panorama/transcripts/seroxat.txt
- Angell M.
The Epidemic of Mental Illness: Why?. The New York Review of Books (June 23, 2011). Archived from the original on September 21, 2012. - Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT (February 2008). "Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration." PLoS Medicine 5
(2):e45. DOI:10.1371/journal.pmed.0050045. PMID 18303940. - Horder J, Matthews P, Waldmann R (June 2010). "Placebo, Prozac and PLoS: significant lessons for psychopharmacology." Journal of Psychopharmacology 25
(10): 1277–88. DOI:10.1177/0269881110372544. PMID 20571143. - McGauran N, Wieseler B, Kreis J, Schüler YB, Kölsch H, Kaiser T. (2010 Apr 13). “Reporting bias in medical research - a narrative review.” Trials 11
: 37. DOI:10.1186/1745-6215-11-37. PMID 20388211. - Goldacre B.
The whole truth about drugs: The global conspiracy of pharmaceutical companies / Translation: Poroshina T.I., Cherepanov V.V. — RIPOL Classic, 2020. — 630 p. — (New way of life).