GENERAL
At the moment, there are isolated cases of polio, whereas in the past, before mass vaccination, there were epidemics of this disease.
Even at the beginning of the twentieth century in Europe and Africa, due to the increasing incidence of polio, it had the character of a national disaster. In the 1950s, after the rapid introduction of the polio vaccine, the rate of diagnosed outbreaks decreased by 99%, but endemic regions of the disease are still observed in Nigeria and South Asia.
Poliomyelitis is seasonal, with an increase in incidence occurring in the summer and autumn. Children from six months of age to 5 years are especially susceptible to the disease, but cases of infection have also been recorded among adults.
The causative agent of poliomyelitis is poliovirus from the group of intestinal enteroviruses of the picornavirus family (Picornaviridae). There are 3 types of this pathogen. In 85% of cases of paralysis, type 1 poliovirus is diagnosed.
The virus is highly resistant in the external environment: it persists in water for 100 days, and in feces for six months. Exposure to digestive tract juices, freezing and drying does not affect its vital functions. The death of poliovirus occurs during prolonged boiling, under the influence of ultraviolet radiation and low concentrations of disinfectant solutions (chlorhexidine, bleach, furatsilin, hydrogen peroxide).
CAUSES
The source of infection is an infected person, both with signs of the disease, and a carrier whose pathology is asymptomatic.
The pathogen enters the human body through the mucous membranes of the upper respiratory tract and intestines. The main route of transmission of infection is through contaminated food, water, and hands. The spread of the disease by airborne droplets occurs much less frequently. There have also been cases of infection while swimming in a polluted pond.
Development phases:
- Enteral. Primary replication of the virus in the tonsils during airborne infection or in the lymphoid follicles of the intestine during fecal-oral infection.
- Lymphogenic. From localization sites, viral particles spread into the lymphoid tissue, then into the mesenteric and cervical lymph nodes, where the replication process continues.
- Viremia. The poliovirus exits the lymphatic system into the bloodstream and spreads throughout the body. Secondary replication of viral particles occurs from internal organs.
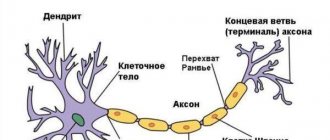
- Neural. This phase of development is possible only in the absence of neutralization of viruses by mononuclear phagocytes. The pathogen migrates from the blood to the neurons of the anterior horns of the spinal cord and motor nuclei of the brain. Damage and death of neurocytes provokes the development of inflammation, in this place the nervous tissue is replaced by connective tissue.
People with mild or mild symptoms of polio pose a particular danger to others. They continue to lead their normal lives and spread the virus to others, becoming a source of infection. In addition, 3-4 days before the development of the first symptoms of polio in the form of an increase in body temperature, a person is already contagious.
Despite the severity of the disease, only 1% of people, after penetration of the poliovirus through the mucous membranes and viremia, develop a severe form of poliomyelitis, which is accompanied by flaccid paralysis.
How does infection occur and who is at risk?
The routes of infection with polio mainly come down to the penetration of the virus through the digestive tract - if water, food or hands have previously come into contact with contaminated substances. For example, feces of a sick person get into a pond, and then when swimming, the patient gets the virus along with the contaminated water. The causative agent of the disease is poliovirus.
You can become infected through water, food, dirty clothes, etc. At risk are:
- children under 7 years old. Poliomyelitis occurs much more often in children than in adults;
- Pregnant women;
- people with very weakened immune systems. This can be facilitated by various diseases, as well as disorders at the endocrine level, periods after operations, etc.;
- people suffering from immunodeficiencies.
The risk of infection is higher during the warm season: summer or autumn. The virus is very tenacious; in a humid environment it can live up to 4 months.
CLASSIFICATION
Poliomyelitis is classified by the severity of damage to the central nervous system, by external manifestations, and by the nature of its course.
Forms of the disease depending on the symptoms:
- Poliomyelitis, which occurs without damage to the cells of the nervous system, is an inapparent (virus carrier) and visceral (abortive) form.
- Poliomyelitis occurring with neuronal damage, or typical - meningeal, paralytic and non-paralytic forms.
According to the severity of damage to the nervous system by poliovirus:
- Spinal – paralysis of the muscles of the trunk, diaphragm, limbs and neck.
- Bulbar - suppression of swallowing function, breathing, changes in speech and decreased cardiac activity.
- Pontine is accompanied by a partial change in facial expressions with distortion of the corner of the mouth on one side of the face and incomplete closure of the eyelids.
- Encephalitic – signs of focal brain damage.
- Mixed
According to the nature of the flow:
- smooth course - without complications; •
- unsmooth course - with the development of complications in the form of a secondary infection or with an exacerbation of sluggish pathological processes).
SYMPTOMS of polio in adults
The latent period of polio lasts from 2 to 35 days, but generally lasts 1–2 weeks. In 95–99% of adult patients, the disease proceeds without paralysis.
Symptoms depending on the form of the disease:
- Inapparent. In other words, it means carrying the virus. There are no external manifestations of infection; the presence of the pathogen in the body can only be confirmed through laboratory tests.
- Visceral (abortive). Occurs when diagnosing 80% of cases of poliovirus infection. Most often, clinical manifestations occur in the form of fever, headache, intoxication, catarrhal phenomena, abdominal pain, nausea, vomiting and diarrhea are not excluded. Sometimes muscle weakness and lameness may occur. Symptoms are nonspecific, the disease ends after 3–7 days with complete recovery.
- Meningeal. There are two waves of fever over 2–5 days, followed by headache, muscle weakness, nausea and vomiting after 1–3 days. The course of the disease resembles serous meningitis. Recovery occurs after 3–4 days.
- Paralytic (spinal). This form of polio is characterized by the most severe course and unpredictable outcome. First, the patient experiences symptoms of meningeal and abortive forms. When body temperature rises again, pain in the spine and muscles, confusion and convulsions are noted. The paralytic phase in adults manifests itself 3–6 days after the first symptoms appear. It is characterized by the sudden development of paralysis of the limbs (usually legs) without loss of sensitivity. Less commonly, the disease is of an ascending nature, in which paresis of the arms, face and torso occurs, often with impaired function of defecation and urination. Damage to the cervicothoracic spinal cord is accompanied by paralysis of the diaphragm and respiratory muscles, which can cause the death of the patient from acute respiratory failure. The severity of paralysis increases over the course of a week, then in half of the patients there is a gradual restoration of normal motor ability. A quarter of patients with paralytic polio later become disabled.
How to prepare your child for testing
2-3 days before the test, it is advisable to eliminate physical and emotional stress. It is also recommended not to carry out physical therapy procedures the day before blood sampling.
A small child needs to be prepared mentally, given that taking a blood test from a vein is not the most pleasant procedure. If blood from a vein is donated for the first time, the baby may experience fear. Parents should try to adjust the child accordingly. Maybe even include some game moment, maybe persuade you to be patient if a needle pricks - there can be many options. But, in any case, the child’s panic will only prevent the nurse from performing manipulations.
DIAGNOSTICS
Identification of the causative agent of the disease is of great practical importance, since similar symptoms can be caused by other types of enteroviruses and herpeviruses. Differential diagnosis is carried out to exclude or confirm tick-borne encephalitis, Guillain-Barré syndrome, myelitis, serous meningitis and other enteroviral infections.
Detection of poliomyelitis in the non-paralytic form or in the pre-paralytic stage, occurring without damage to the nervous system, is difficult. Often during this period, acute respiratory viral diseases, intestinal infections or serous meningitis are mistakenly diagnosed. Therefore, the clinical picture at this stage is not decisive. The main role is given to laboratory diagnostics.
Diagnostic methods:
- Polymerase chain reaction (PCR) can detect the virus in the patient's feces and cerebrospinal fluid.
- An enzyme-linked immunosorbent assay (ELISA) helps isolate poliovirus RNA.
- Serological analysis of blood plasma determines antibodies to poliovirus.
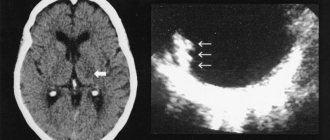
- Clinical analysis of cerebrospinal fluid, electroencephalogram, CT, MRI - as additional methods for identifying changes in the structure of the motor centers of the spinal cord and brain.
When a lumbar puncture of cerebrospinal fluid is taken, increased pressure is noted. The content of leukocytes and protein in it exceeds the norm.
What should you do if an unvaccinated child came into contact with someone vaccinated against polio?
You need to understand that only virulent viruses pose a danger, and in order to become such, they must undergo a mutation in the intestines of the vaccinated person. This is possible if a person has a serious immunodeficiency, which in itself is a rare case.
Therefore, usually a vaccinated baby releases unchanged (non-dangerous) viruses in much smaller quantities (passive immunization) than they were injected with during immunization. That is, those around you who have received such a small dose simply maintain the tension of the immune system in the team.
This is the purpose of OPV vaccination. But even if we assume that an unvaccinated baby still managed to catch a virulent virus (that is, he also has severe immunodeficiency), the probability of contracting polio is only 5% (or less).
But, even if included in these statistics (which is absolutely incredible), the child is unlikely to get paralytic (which is what everyone is afraid of). The disease will go unnoticed or will be similar to ARVI or an intestinal infection.
And only 2% of children have a chance of getting vaccine-associated paralysis. But do not forget that such a baby has severe immunodeficiency. In addition, the contact must be long and close.
In a kindergarten setting, all of the above points are unlikely to coincide. Therefore, such cases were not recorded.
TREATMENT
Patients with suspected polio and identified cases of infection are treated in the hospital infectious diseases department. Therapy involves isolation, strict bed rest with limited active movements and proper nutrition.
There is no specific treatment for polio; effective antiviral drugs do not currently exist. All measures are limited to symptomatic therapy.
To treat the disease the following is prescribed:
- analgesics;
- antipyretics;
- sedatives;
- anti-inflammatory;
- antihistamines;
- intravenous infusions for the purpose of detoxification.
In addition, it is possible to prescribe diuretics, antibiotics, immunoglobulins, antihypoxants and drugs to improve neuromuscular conduction.
It is important to monitor the correct position of the patient's body. When paralysis develops, he is placed on a hard bed without a pillow. The legs, slightly bent at the knees and hip joints, are placed parallel, the feet are fixed with a splint in a normal physiological position. The arms are spread to the sides and bent at the elbows at a right angle.
Resuscitation measures are carried out in case of breathing disorders. For this purpose, a forced ventilation device is used with simultaneous suction of mucus from the respiratory tract.
The recovery period begins in the hospital immediately after treatment and continues in an outpatient setting.
The recovery period includes:
- water procedures;
- physical therapy;
- physiotherapy (electrical stimulation, UHF, hot compresses on affected muscles).
COMPLICATIONS
With polio, paralysis of the respiratory muscles is likely to develop, which provokes an attack of acute cardiac and respiratory failure. These severe conditions can cause death, so patients should be monitored in a hospital.
Other complications of polio may include interstitial myocarditis, pneumonia, and pulmonary atelectasis. Bulbar forms of the disease sometimes lead to the development of severe gastrointestinal disorders, which are accompanied by ulcers, bleeding and perforations.
One of the rather rare complications of vaccination with live polio vaccine is the development of vaccine-associated poliomyelitis.
PREVENTION
The only effective measure to prevent polio is vaccination. It provides active lifelong immunity against the disease. Routine vaccination of children is usually carried out with an inactivated and then a live vaccine. The inactivated vaccine is administered intramuscularly by injection, and the live vaccine is available in the form of drops for oral use. Polio vaccine administration schedules differ in different countries in terms of timing of vaccination and revaccination.
Another measure to prevent the spread of the disease is the isolation of patients in specialized hospitals until complete recovery and compliance with hygiene standards.
In what cases is a study prescribed?
Sometimes doctors encounter patients whose medical records do not contain information about vaccinations for some reason. Someone may fall behind the vaccination schedule and miss important stages of immunization. In such cases, it is necessary to find out whether a person’s blood contains antibodies to pathogens of dangerous diseases. This determines whether the patient needs additional vaccinations and when it is appropriate to vaccinate.
Parents are often worried that their child may become infected in a child care facility (kindergarten, nursery, school) from other children vaccinated against polio with a live vaccine. They want to find out whether their child has immunity against this disease and, accordingly, how high the risk of infection is. In recent years, there has been a growing trend among some "advanced" parents to avoid vaccinating their children. For some reason, this category of parents is convinced that vaccinations are harmful, not always correctly comparing possible complications with the risk of contracting a dangerous disease. However, in the future they put not only their children in danger, but also the children with whom their children communicate.
The danger of polio, meanwhile, has not been disputed by anyone for a long time. This disease kills about 5% of those affected and makes 25-30% disabled for life.
An antibody test may be prescribed for diagnostic purposes when a disease is suspected. If the disease has already been detected and the patient is prescribed treatment, an immunoglobulin test helps control this process.