Why does the pulse become fast?
When the heartbeat increases, it can be assumed that there are abnormalities in the activity of the cardiovascular system.
Especially if the pulse becomes frequent for no apparent reason. Sometimes a rapid heart rate is normal, but if external circumstances cannot provoke such a symptom, you should be wary. If everything else can be neutralized, then the presence of undetected diseases is difficult to overcome. Only a doctor can carry out the necessary diagnostics and you should turn to him for help. He will prescribe the necessary treatment. It is dangerous to start taking any medications without special instructions.
The causes of rapid heart contractions can be different. External stimuli often cause changes in the rhythm of the heart, but when their influence stops, the pulse returns to normal.
Causes of palpitations:
- fright,
- experiences,
- emotions,
- abuse of coffee and energy drinks,
- side effects of drugs,
- allergic reaction,
- increase in body temperature,
- anemia,
- problems with the thyroid gland,
- small amount of oxygen,
- heart diseases.
Some of these reasons cause temporary changes in heart rhythm. But there are also reasons that pose a threat, so anyone should pay attention to the condition of their body and promptly consult a doctor if something worries them. Because many diseases are cured faster if detected on time.
At night, the heart rate can increase for various reasons. Those who go to the doctor with this symptom often find diseases of the endocrine and nervous system, problems with the psycho-emotional state, anemia, poisoning, and internal bleeding. Also, strong heartbeat at night and in the morning can be a sign of heart failure.
With infectious and cold diseases with an increase in body temperature, the pulse can also increase at night, or rather, at any time of the day. In some cases, the cause may be dehydration or a lack of certain substances.
Excessive heart palpitations at night can lead to insomnia, as it is difficult to fall asleep with your heart beating rapidly. This phenomenon can be caused by constant nervous tension, an abundance of conflicts in everyday life, excessive physical fatigue, insufficient or irregular rest, and abuse of harmful substances and medications.
It contains 8 useful medicinal plants that are extremely effective in the treatment and prevention of arrhythmia, heart failure, atherosclerosis, ischemic heart disease, myocardial infarction, and many other diseases. Only natural ingredients are used, no chemicals or hormones!
Example: “I recently noticed that I was waking up at night with terrible heart palpitations. The pulse is so fast that it is impossible to count. The cardiologist checked and said it was sinus tachycardia. During the examination, the pulse was 120. But at night it was clearly even higher. Why does this happen, because I’m sleeping and don’t worry about anything?!”
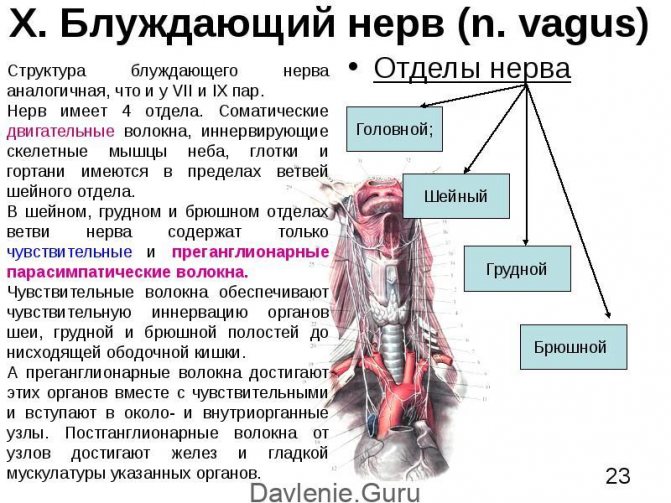
Decreased vagal tone
Tachycardia at night during sleep may be due to decreased activity of the vagus nerve, or vagus, which is part of the parasympathetic nervous system. It is activated at night and helps to slightly reduce heart rate and blood pressure.
When the activity of the vagus nerve decreases at night, the sympathetic department is activated, which provokes:
- Increased heart rate;
- Increased contractility of the heart;
- Increased blood pressure;
- Increased breathing;
- Increased skeletal muscle tone.
Genetic mutations, inflammatory damage to its fibers, and emotional stress lead to a decrease in the tone of the vagus nerve during sleep.
What is the danger of increased heart rate combined with difficulty breathing?
Palpitations are often accompanied by additional symptoms that worsen a person’s condition.
One of the common complaints in this case is that there is not enough air with a rapid pulse. In other words, it is difficult for a person to breathe.
These symptoms can occur even in people who feel healthy. But a rapid heartbeat and lack of air indicate that not everything is ideal in the body. Sometimes this condition is a sign of serious illness.
The cardiologist carries out some of the diagnostic procedures with the help of other specialists: an endocrinologist, a neurologist, etc. Because the causes of unpleasant symptoms can be associated not only with heart disease. Carrying out general and special tests will allow you to get the most correct idea about the disease.
Methods for relieving the condition at home
When general weakness is combined with rapid heartbeat and dizziness, methods to alleviate the condition should be used:
- You need to calm down and lie down on the bed in a well-ventilated area. To make breathing easier, you should remove clothes that tighten the neck and chest area.
- Coughing and holding your breath while trying to expel air through your closed mouth will help lower your heart rate. The pressure in the chest will increase, which will reduce the severity of tachycardia.
- You can alleviate the condition by stimulating reflex zones (eyeballs, carotid artery) for several minutes and washing your face with cold water.
- After taking a deep breath, you need to hold your breath for 10-15 seconds, and then exhale at a slow pace. To relieve the symptoms that arise, you need to perform the breathing exercise several times.
- The severity of tachycardia decreases with massage of active points on the hands and feet. Circular movements are performed counterclockwise.
- Medicines should only be taken with the approval of your doctor. As a last resort, taking a beta-blocker is allowed, but provided that the patient has already been prescribed it before. If blood pressure drops to 100/60 mm Hg. Art. and below, then taking medications from this group is prohibited.
- If you spend a long time under the sun and have the corresponding symptoms (“heavy” head, excessive sweating, decreased visual acuity), you need to go to a dark place. It is advisable for the patient to drink cool water and wash. You can apply something cold to the head and heart area.
Sleep apnea syndrome
Often, an increased heart rate at night provokes sleep apnea - a disorder of respiratory function in which it stops during sleep. The causes of this pathology are:
- Obesity;
- Endocrine system disorders;
- Frequent stressful situations;
- Anatomical features (enlarged tonsils or uvula, narrow nasal passages).
Periodic episodes of apnea at night cause hypoxia and hypercapnia, which signal the brain to wake up. After waking up, breathing usually returns to normal.
Lack of oxygen at night provokes an acceleration of the heartbeat and an increase in cardiac output - tachycardia occurs at night. In addition, people experience snoring and daytime sleepiness.
How are pathologies detected during research?
Each diagnostic method demonstrates the characteristics of the functioning of the heart.
A general blood test can determine how much hemoglobin is contained in blood cells. Its deficiency can cause weakness and create a feeling of difficulty breathing. Therefore, the patient may feel that he does not have enough air.
The level of hormones produced by the endocrine system often causes the development of heart and cardiovascular diseases. There is a huge difference in the treatment of such diseases in the case of thyroid problems and in the case of other complications. Therefore, any detected anomalies have an impact on the chosen treatment method.
The absence or deficiency of nutrients can also cause rapid heart rate and difficulty breathing. Therefore, a blood test is needed that reports on the characteristics of its biochemical composition.
Any abnormalities detected in this case serve as a reason for further research and require treatment. Typically, an ECG should be performed if a patient with heart disease complains of worsening of the condition, or if there are plans to change activities (you need to find out whether this will cause problems). Diseases of the endocrine system also require an ECG.
Human endocrine system
Anxiety during Holster monitoring can be caused by short-term disruptions in the pulse rhythm, not detected by a regular cardiogram. During this study, it is possible to compare the characteristics of cardiac activity with situations in the patient’s life and detect those reactions that deviate from the norm. This will help in making a diagnosis.
Features of the structure of cardiac tissues and their work can be identified through echocardiography. This way you can detect a heart attack, angina pectoris, postoperative complications, etc. This method also provides the opportunity to evaluate the effectiveness of treatment and its timely correction.
Difficulty breathing and rapid heart rate are considered normal in some situations. But sometimes they indicate the development or exacerbation of many diseases of the heart and cardiovascular system. A timely visit to a cardiologist will allow you to detect the problem at an early stage and begin its treatment.
Do you still think that it is impossible to get rid of HEART DISEASES!?
- Do you often experience discomfort in the heart area (pain, tingling, squeezing)?
- You may suddenly feel weak and tired...
- I constantly feel high blood pressure...
- There is nothing to say about shortness of breath after the slightest physical exertion...
- And you have been taking a bunch of medications for a long time, going on a diet and watching your weight...
Thyrotoxicosis is a disease of the thyroid gland characterized by excessive production of thyroid hormones. Increased levels of T3 and T4 in the body disrupt metabolic processes, leading to the development of tachycardia at rest (including at night).
Other symptoms of thyrotoxicosis are irritability, weight loss, hand tremors, and excessive sweating. The progression of the disease often leads to the development of thyrotoxic heart - dystrophy, myocardial hypertrophy, cardiosclerosis and heart failure.
Pheochromocytoma is one of the forms of adrenal tumor, characterized by pathological proliferation of their tissue. The enlargement of these organs leads to excess production of adrenaline, which increases heart rate. In this case, a feeling of fear, tremors of the limbs, and nausea arise.
Treatment methods
A neurological disorder can be diagnosed based on the patient's complaints and medical history. All necessary measures are taken to exclude diseases of the cardiac system. Cardiophobia is treated in an outpatient clinic. If the symptoms of neurosis are too pronounced, the patient may be hospitalized in the neurological department.
For symptoms such as depression, insomnia and other disorders, herbal sedatives or antidepressants are prescribed. An important therapeutic measure is psychological assistance from a specialist. Work is being done to adapt the patient to the stressor and suppress fear.

Anxiety is a symptom of Cadiophobia
It is quite difficult for a person to get rid of cardiophobia on his own.
Psychological impact includes searching for the cause. The first action of the patient, which helps to overcome the pathological fear that his heart will stop beating, is an examination by a cardiologist. Then the psychologist works.
The patient must find something to do for the soul in order to be able to escape from bad thoughts.
Psychological work also involves the patient’s adaptation to communication.
Manifestations of diseases during diagnosis
The most common cause of tachycardia at night is nocturnal hypertension. In this case, the increase in heart rate during sleep is compensatory in nature - in order for the heart to transport blood entering it with increased force, it needs to work faster.
The main cause of hypertension at night is insufficient dosage of antihypertensive drugs taken the night before bedtime. However, there are cases of idiopathic nocturnal hypertension.
The next reason that can cause nocturnal tachycardia is Brugada syndrome, a genetic pathology characterized by a disorder of the conduction system of the heart. In this case, a rapid heartbeat at rest provokes sleep or daytime rest.
Cardiosclerosis is the replacement of the heart myocardium with connective tissue due to myocardial infarction. Areas that have succumbed to scarring disrupt the normal contraction of cardiomyocytes and impair the conduction of impulses through them.
Such pathological processes lead to rhythm disturbances, including at night.
Myocarditis is an inflammatory lesion of the myocardium, most often having an infectious etiology. Less commonly, the cause is rheumatic damage to the heart muscle. Inflammatory processes disrupt the innervation of cells and the conduction of electrical impulses through them, leading to tachycardia.
Any of the diagnostic methods reveals the peculiarities of the functioning of the heart. If pathologies are identified, additional studies may be prescribed to obtain the most complete picture of the disease.
It establishes the source of the heart rhythm, pulse frequency and characteristics of its beating. With its help, you can notice changes in the myocardium, assess the rate of impulses, and discern the parts of the heart. Any of the deviations identified in this may serve as a reason for further research.
An ECG is performed if the condition of a heart patient worsens, to assess the risk to the cardiovascular system when performing a particular type of activity. A planned operation is also a reason to perform an ECG, as it will eliminate possible complications.
Diseases of the nervous and endocrine systems can affect the heart, so if they are present, an ECG is also performed.
Since such monitoring allows you to track the work of the heart in any situation, its further analysis will make it possible to detect abnormal reactions. In this way, you can identify a more accurate diagnosis and understand the causes of the disease.
Echocardiography studies the structure and function of cardiac tissue. Most often, this method is used for heart attack, complications after any illness or surgery. If deviations are observed, this becomes a serious cause for concern. This method can also be used to assess whether the chosen treatment is effective.
When performing magnetic resonance imaging, it is possible to obtain the most accurate information about the condition of the heart. It identifies pathologies of any part of the heart, blood vessels, valves and tissues. In addition, it is possible to assess the blood supply and condition of the coronary artery. Deviations in all this require treatment and caution.
Strong heartbeat during sleep can be considered normal only when it happens very rarely and goes away quickly. But even in this case, an examination by a cardiologist will not be superfluous. If such cases are observed very often, but there are no objective reasons, it is necessary to undergo a thorough examination.
Palpitation is a feeling of accelerated rhythmic contraction of the heart muscle. These sensations are strictly individual.
One person feels the heart beating at 100 beats per minute, and another only at 120 - 130 beats per minute. Increased heart rate has 2 causes.
An attack of rapid heartbeat with low blood pressure
Patients typically describe palpitations as follows: the heart pounding loudly and forcefully in the chest, twitching, jumping out of the chest, or fluttering. Palpitations at night may be accompanied by a sensation of pulsation in the temples, neck, fingertips or pit of the stomach.
It may also be accompanied by tinnitus, pain in the heart, difficulty breathing, or a feeling of tightness in the chest. These symptoms may indicate heart disease. But such complaints in most cases do not lead to the identification of serious disturbances in the functioning of the heart.
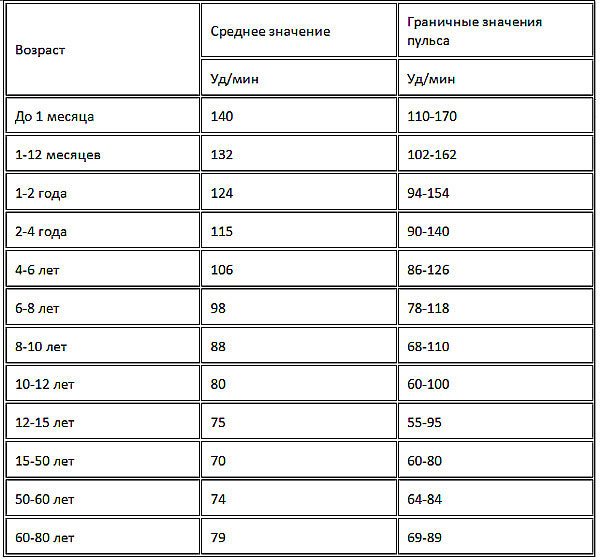
It is important to distinguish palpitations from tachycardia, which is a significant increase in heart rate. The pulse of an adult is 60-80 beats per minute at rest. Tachycardia is diagnosed if more than 90 beats per minute are recorded. But a person may not feel a rapid heartbeat.
A person’s actions in such a situation depend on what causes such symptoms. If you have already had to consult a doctor with this problem, he will definitely provide recommendations in case of repeated cases.
Taking a deep, slow breath followed by a sharp exhalation also reduces your heart rate. Coughing has the same effect. If your doctor has recommended any medications for such cases, they can also be used.
But if the cause is unknown, or the attack is very severe, then you should call an ambulance, not expecting that the alarming symptom will disappear on its own. Sometimes, a strong heartbeat at night can be a sign of an impending heart attack or stroke.
It is best to undergo annual examinations with a cardiologist. Then any heart problems will be noticed immediately. You should see a doctor as soon as possible if increased heart rate at night has become a common occurrence. Additional symptoms should cause even more anxiety: pain in the heart and chest, weakness, lack of air, shortness of breath, etc.
The most dangerous signs:
- excessive force and intensity of heart rate;
- frequent pulse over a long period of time;
- increase in rhythm with small external influences;
- increased heartbeat for no reason;
- uneven heart rate.
These symptoms most often indicate the presence or development of a serious disease, which must be detected and treated.
The first reason is tachycardia, when pulsation is felt not only in the heart, but also in the neck, head and fingers and toes. In a state of tachycardia, the pulse is higher than 90 beats per minute. With normal functioning of the heart muscle, the heartbeat should not be felt.
Very often, with audible beatings in the heart, there is pain in the chest, lack of air in the lungs and noise in the head and ears. These symptoms are temporary in their development and are not a consequence of heart disease. If symptoms recur regularly, this means that there is a pathology in the heart and you should consult a doctor - a cardiologist.
In people who suffer from hypotension, attacks of tachycardia occur quite often. In case of very low blood pressure and an attack of tachycardia, you need to drink at least 100 ml to provide first aid. cold water and wash your face and neck with cold water.
Symptoms of tachycardia occur due to pathologies in the body:
- State of traumatic and anaphylactic shock;
- Dystonia;
- Large loss of blood during bleeding.
What should you do if you have sudden heart palpitations?
However, this is not surprising. We only recently learned how to measure blood pressure. And that’s not all. Many people begin to associate their “abnormal” condition with increased blood pressure only when the doctor notices.
It's time to change the situation, because tachycardia is very serious. If the heart begins to beat too quickly, it does not have time to fill with blood, a full release of blood is not possible, and as a result, oxygen starvation occurs in the cells of the body, including the heart itself. The consequences are not difficult to guess.
If tachycardia occurs frequently and over a long period of time, pathological changes occur in the heart - its contractility is impaired, and the organ itself increases in size. Therefore, in frequent cases of tachycardia, you need to run to a cardiologist. Treating pathological tachycardia is his prerogative.
However, even in normal everyday life, every person can experience temporary heart palpitations.
The causes of physiological tachycardia are very diverse:
1. Physical activity . Any: physical labor, sports and even gymnastics, tension (including during bowel movements, loud screaming during scandals, lifting weights, etc.).
2. Emotional experience . Again, any: grief, fear, joy, hatred, irritation...
3. Harmful environment . And again, any: polluted air, lack of oxygen (in a stuffy room or at altitude), ground-level ozone after a thunderstorm...
4. Increased body temperature . Pay special attention to this point. Think about chills and withdrawal symptoms during a cold. It is possible that the “shaking” is precisely because of the tachycardia that has arisen, because with an increase in body temperature by 1 degree, the heartbeat increases by 10 beats! And then it will be enough to reduce the frequency of heartbeats for relief to occur.
5. Gluttony . Tachycardia occurs quite often when overeating.
6. Allergies . Experienced allergy sufferers should know about this.
7. Hot flashes during menopause . Every woman must keep this in mind!
8. Drinking energy drinks . However, the pulse may increase with frequent consumption of strong coffee or tea.
4. Increased body temperature . Pay special attention to this point. Think about chills and withdrawal symptoms during a cold. It is possible that the “shaking” is precisely because of the tachycardia that has arisen, because with an increase in body temperature by 1 degree, the heartbeat increases by 10 beats! And then it will be enough to reduce the frequency of heartbeats for relief to occur.
How not to cause harm?
During an attack, you should not perform certain actions that can increase your heart rate. For example, taking a hot bath or drinking strong drinks. These recommendations apply to all patients prone to tachycardia, even if they are not currently having an attack. General recommendations include:
- frequent drinking of coffee and cocoa, and it is not even recommended to eat chocolate;
- It is not recommended to take medications containing caffeine;
- eat spicy and salty foods;
- engage in active sports;
- if you want to take any dietary supplements, consult your doctor first;
- If you are prone to tachycardia, it is forbidden to smoke, overeat, or overexert yourself mentally and physically.
- pulse readings at the beginning of the attack and how much it increased over a certain time;
- indicate the factors that provoked the attack;
- whether medications were taken during the attack, which ones and in what quantities.
When is a high heart rate normal?
Normally, the heartbeat increases for the following reasons:
- exercise stress;
- waking up after sleep;
- change in body position (when you suddenly stand up);
- strong emotions (both negative and positive);
- eating (if you have eaten heavily, your heart rate may increase).
Usually such a rapid heartbeat is not even felt. Or you may notice it, but it will not be accompanied by other unpleasant symptoms (discomfort, chest pain, a feeling of your heart “jumping out” of your chest, severe shortness of breath, etc.)
In this case, you don't need to do anything. This condition is not dangerous unless you have heart disease.
The heart beats faster in childhood and adolescence. If you notice that your baby's pulse is faster than yours, this is normal. If nothing bothers the child himself, you can rest assured.
The so-called idiopathic tachycardia also occurs. A condition where a high heart rate is associated with the individual characteristics of the body. Typically, in this case, the heart rate deviates from the norm by 10–15 beats per minute. In this case, there is no reason that provokes a rapid pulse, and no health problems. In this case, you also don’t need to do anything, no treatment is needed.
During the day, your heart rate can vary significantly. And if you notice that your heart is beating a little faster than usual, don’t worry right away.
Prevention, useful tips
Many patients with paroxysmal tachycardia continue to live with this difficulty for a long period of time. Treatment for this disease is dangerous and has unforeseen consequences. It is recommended to follow preventive measures to reduce the frequency of tachycardia attacks.
Prevention measures include:
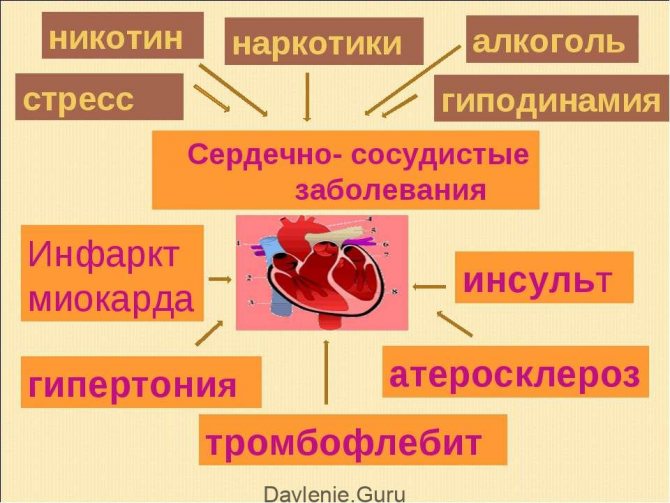
- Follow the menu . There is no special diet for tachycardia, but certain nutritional requirements will help improve the quality of life of patients. It is necessary to limit the use of alcohol, strong tea and coffee, as they provoke an attack. Limit animal fats , as they provoke the development of atherosclerosis and increase the likelihood of a heart attack during tachycardia. Limiting the caloric content of food and consulting with a nutritionist is advised only to those patients who are overweight.
- Stop smoking. Nicotine provokes tachycardia. When a patient suffers from heart pathologies that are accompanied by tachycardia, the likelihood of consequences is especially high. In addition, smoking increases the likelihood of myocardial infarction during an attack.
- Limit physical activity. Lead to an increase in heart rate. In people with constant disruptions of the cardiac conduction system, the arrhythmia drags on for several days, which increases the risk of thrombosis. The likelihood of engaging in physical therapy for preventive purposes should be clarified by a specialist.
- Age;
- Activity level;
- Measurement time;
- Temperature;
- Season;
- Environment.
Clinical picture
During attacks of tachycardia at night, a person usually wakes up abruptly. The following symptoms appear:
- Increased heart rate is the most common symptom of tachycardia during sleep. The sensation of heartbeat occurs due to uneven blood flow and abnormal functioning of the heart muscle. In another way, this sign is called palpitation.
- Increased peripheral pulse rate - Pulse rate in the periphery is most often checked at the radial artery. During night attacks of tachycardia, the pulse number fluctuates between 90-150 beats/min.
- Pulsation of the carotid arteries - visual pulsation of the carotid arteries occurs due to an increase in their tone and an increase in the release of blood into the aorta. You can palpate a high pulse on these vessels on the neck line formed between the chin and earlobe.
- Shortness of breath - a feeling of lack of air and increased breathing during sleep are a consequence of hypoxia, which develops during an attack of tachycardia. For the same reason, dizziness occurs.
- Discomfort in the cardiac region rarely occurs in clinically healthy people and is a consequence of ischemia due to lack of oxygen to the heart muscle.
In the presence of heart pathologies against the background of tachycardia, angina attacks, syncope, increased blood pressure, and cough may occur.
In some cases, tachycardia is associated with autonomic disorders. These include:
- Feelings of fear, anxiety;
- Increased sweating;
- Hand tremors;
- Pale skin;
- Tingling in fingers.
Reasons for development
Fear of death is a natural feeling for any person. A pathological disorder that interferes with life is observed in people who are insecure, withdrawn, and lonely. This can be called a cry for help; the person seems to be trying to say: “pay attention to me, I’m lonely.” The disease often accompanies sanguine people who tend to exaggerate their goals and who cannot be distracted from their activities even on weekends.
The impetus for the manifestation of a phobia is an open or hidden stressful situation.
In most cases, the fear of dying from cardiac arrest occurs after:
- determination of the presence of a heart disease in a relative or close friend;
- long-term communication with the patient;
- death of a loved one from a stroke;
- stories of instantaneous heart failure in young people.
Sometimes cardiophobia begins to develop after an annual medical examination and harmless tachycardia or bradycardia is interpreted as imminent death from a terrible disease. Sometimes patients with symptoms of cardiophobia suffer from cardiovascular disease, but in reality the situation is not as dire as their imagination depicts.
Diagnostic procedures when visiting a doctor
Repeated attacks of palpitations in the morning and at night require contacting a cardiologist. It is he who will carry out the diagnosis and refer you to the necessary consultations with other doctors.
He will identify heart diseases himself using an ECG or stress tests (this is an ECG using exercise equipment, which allows you to track changes in the work of the heart during physical exercise). Very often, heart disease occurs due to malfunctions of the autonomic nervous system.
Review from our reader Victoria Mirnova
I’m not used to trusting any information, but I decided to check and ordered a bag. I noticed changes within a week: the constant pain and tingling in my heart that had tormented me before receded, and after 2 weeks disappeared completely. Try it too, and if anyone is interested, below is the link to the article.
In addition to the cardiogram, the patient will need to answer the doctors’ questions about how he feels his own pulse (whether he notices an increase or decrease in frequency), whether heartbeats skip, and in what situations the heart contracts faster. It will also be necessary to characterize other oddities, if any.
If the ECG shows abnormalities, additional studies are prescribed. It can be:
- Holter monitoring.
In this case, an ECG is recorded throughout the day, when the patient leads a normal life and performs daily activities. This makes it possible to better understand the nature of the disease, the causes of its occurrence, and also choose the right method of treatment.
Echocardiography.
This method allows you to study the valvular apparatus of the heart and its functional changes using ultrasound.
Electrophysiological study.
During such diagnostics, it is possible to study the electrophysiological properties of the conduction system and cardiac sections. The study is performed using catheter electrodes and special equipment. Thanks to this method, it is possible to better understand the characteristics of the disease and its causes.
Coronary angiography.
This diagnostic method allows you to reliably identify coronary heart disease. Such a study shows where, how and how narrowed the coronary artery is.
If necessary, the cardiologist seeks help from other specialists: a neurologist, endocrinologist, psychotherapist, etc. This is done if problems in the heart are caused by diseases of other systems. Together they choose the most appropriate method of treatment. In addition, tests may be prescribed - both general and special.
Development mechanism
Weakness, dizziness and rapid heartbeat have a common development mechanism. Due to certain irritating factors, tachycardia occurs. As the heart rate increases, hemodynamic disruptions occur, which impair the nutrition of the brain and other tissues. The severity of manifestations depends on individual tolerance, the condition of the blood vessels, the degree of maintaining the constancy of cerebral (brain) blood flow and the contractility of the heart.
If there is a sudden interruption in cerebral blood supply, the patient will feel dizzy. If the failure lasts a couple of minutes, loss of consciousness is possible. The feeling of weakness occurs due to frequently recurring attacks of tachycardia, against the background of which oxygen starvation of the tissues manifests itself.
Prevention
To prevent nocturnal tachycardia, it is necessary to reduce the physical and emotional stress on the body and lead an active lifestyle, which helps to strengthen the body’s compensatory capabilities and normalize the heartbeat. It is necessary to control the amount of time spent in a stationary state (working at a computer), and give up bad habits (coffee, nicotine).
It is recommended to streamline your diet, avoid heavy fatty foods at night, and limit the amount of fast carbohydrates. Take the main daily dose of calories in the first half of the day.
It is necessary to give up physical activity in the run-up to bedtime, make walking, a relaxing shower or bath a habit.
Before going to bed, you should do breathing exercises, conduct an auto-training session, and take a sedative (valerian, motherwort).
To prevent the development of tachycardia or reduce the frequency of its night attacks, the following rules must be followed:
- Limit physical activity in the evening;
- Avoid stressful situations during the day;
- Reduce evening time spent watching TV or computer;
- Avoid consumption of caffeine-containing and alcoholic beverages;
- Avoid heavy dinners and snacks before bed.
Along with excluding the above factors, it is necessary:
- Control body weight;
- Eat rationally (exclude fatty, fried foods, eat little and often);
- Engage in active activities (swimming, skiing, table tennis), if available
- Contraindications to sports: walking daily, doing Nordic walking;
- When increasing emotional lability, train the nervous system with yoga and meditation.
Possible complications of tachycardia during sleep
Heart rhythm disturbances can signal cardiac pathologies. In such cases, you should immediately consult a doctor and undergo the necessary examination. In addition to cardiac pathologies, the syndrome can occur for the following reasons:
- disturbances in the functioning of the endocrine system;
- psychogenic diseases;
- intoxication from toxic substances;
- closed injuries;
- cardiosclerosis;
- hypoxia;
- vegetative-vascular dystonia;
- myocardial dystrophy;
- heart defects;
- low hemoglobin.
Any of the above reasons can cause palpitations at night during sleep. To determine the main factor, you need to undergo a comprehensive examination. Now we need to consider the reasons that most often cause nighttime palpitations syndrome.
High blood pressure
An increase in blood pressure during night sleep may well trigger an increase in heart rate. Hypertension, which manifests itself at night, can be either a separate pathology or be the result of an incorrect selection of medications for the treatment of hypertension.
In such cases, it is usually necessary to adjust the dose of medications so that the effect is prolonged (long-lasting) and the effect of taking them lasts even at night. Since increased blood pressure during sleep is the most common cause of rapid heartbeat, it is important to know what to do during another nighttime attack:
- drink cool water - when it enters the esophagus, it normalizes the heart rate;
- take a comfortable position, preferably half-sitting, to reduce blood flow to the veins of the heart;
- wash with cool water;
- take a drug prescribed by a doctor that lowers blood pressure;
- ensure a free flow of fresh air into the room.
It is important not to panic, to calm down, and to breathe deeply and evenly.
Low pressure

Nocturnal tachycardia in hypotensive patients is quite common. The low blood pressure itself in this case does not provoke an increase in heart rate. This happens when hypotension is accompanied by concomitant pathology, for example:
- vegetative-vascular dystonia;
- Iron-deficiency anemia;
- increased anxiety;
- pain from an injury received the day before.
In the presence of such pathologies in a hypotensive person, night awakenings from attacks of tachycardia are not uncommon. Rapid heartbeat with low blood pressure is accompanied by:
- nausea, even vomiting;
- dizziness and pain in the temples;
- pale and bluish skin;
- feeling of fear, panic;
- soreness in the sternum.
If the symptoms are pronounced, it is recommended to call an ambulance, and before it arrives, drink water, or take a sedative, such as valerian infusion.
While carrying a child, a woman’s body undergoes significant changes in organs and systems.
Heartbeat at night during sleep bothers many pregnant women, and in most cases it does not signal any serious pathology.

You need to take action and consult a doctor for examination when the following symptoms are added to nocturnal tachycardia:
- pain in the temples and behind the sternum;
- fainting;
- dizziness, nausea.
To avoid increased heart rate at night, expectant mothers are advised to get proper rest, proper nutrition, and avoid nervous overload and stress.
Panic attacks
This name is given to attacks of severe, causeless anxiety that occur more often at night. A panic attack is accompanied by the following symptoms:
- sudden awakening from a strong heartbeat;
- increased sweating;
- lack of air;
- numbness of the limbs.
When this condition develops, the patient may not realize that he has a psychological problem and may not see a doctor for a long time, regularly experiencing attacks of nighttime palpitations and panic. To eliminate these manifestations, the help of a psychologist is required to eliminate the root cause of nocturnal tachycardia - depressive disorders and neuroses.
Rare attacks of tachycardia, accompanied by a dull clinical picture, have virtually no effect on the functioning of the body. However, a frequently occurring rhythm disturbance is fraught with the development of hypoxia, ischemia, or circulatory disorders in individual organs.
Often recurrent tachycardia during sleep can lead to the following consequences:
- Ischemia of the heart muscle, which is reversible (angina attack) or irreversible (myocardial infarction) in nature;
- Acute cerebrovascular accident (stroke or transient ischemic attack);
- Acute heart failure (cardiac asthma or pulmonary edema);
- With ventricular tachycardia - ventricular fibrillation followed by asystole.
Treatment
If the examination reveals a heart pathology, then therapy is aimed at the underlying disease. The main goal of treating patients with a diseased heart is to reduce the number and intensity of attacks of nocturnal tachycardia, since in cardiac pathology arrhythmia is initially a symptom of the disease, and subsequently becomes a factor that aggravates its course.
If the cause of nocturnal tachycardia is hypertension, then the doctor selects an individual drug and dosage. Usually the evening dose is increased.
The implementation of a set of measures aimed at treating sleep apnea causes great difficulties. Patients are advised to fall asleep on their side, but patients are unable to follow the usual recommendations for controlling sleep posture.
In such cases, the only effective treatment for sleep apnea is the use of CPAP (special ventilator machines), which pump oxygen into the lungs through a mask at a certain pressure during sleep.
To reduce the ability of the windpipe to collapse during sleep, you need to lose weight and consult an ENT doctor. A specialist can select a device for the patient that secures the lower jaw during night sleep.
Important! You can get rid of tachycardia situationally by straining, changing your body position, or taking a contrast shower.
If the cause of nighttime palpitations was mental trauma, after which the patient often woke up for a long time due to panic attacks, then the problem can be solved with the help of a psychotherapist. In such situations, sedatives and beta blockers will help you achieve healthy sleep and improve your general condition.
Treatment for palpitations is impossible without identifying its underlying cause. It is necessary to cure the disease that causes this condition and get rid of bad habits (smoking and drinking alcohol).
The following measures will help you forget about this unpleasant phenomenon:
- avoidance of drinks containing large amounts of caffeine (strong tea, coffee, Coca-Cola, energy drinks);
- reduction in the daily diet of spicy foods and chocolate;
- avoiding mental overload and stress;
- transition to fractional meals 4-6 times a day;
- limiting fats in the menu to 40-50 grams per day;
- You need to spend at least 8 hours sleeping.
Rapid night heartbeat is treated depending on the cause that provoked it. To rid a person of unpleasant symptoms, medications and folk remedies are used.
Sinus tachycardia cannot be ignored. Delaying treatment can lead to stroke, angina pectoris, and heart attack.
Depending on what is the cause of tachycardia during sleep, doctors treat the factor that causes it: dilate blood vessels, relieve anemia, get rid of poisons and toxins. With any method of treatment among women and men, an important circumstance is the cessation of drinking alcoholic beverages and smoking.
In this case, a diet is prescribed that does not contain fatty, spicy and unhealthy foods. Food is consumed in small portions about 5 times a day.
It is recommended to exclude caffeinated drinks and dark chocolate. The work and rest schedule is adjusted (sleep should be at least 8 hours).
What to do if your heart beat is higher than normal? First aid
To quickly relieve symptoms of heartbeat, use Valerian tincture: 20 drops of tincture per 50 ml of water. Valerian will help not only lower the heart rate, but also calm the nerves, especially when an attack occurs at night and a person panics.
You can simply cough and the attack of tachycardia will pass.
The massage must be done for at least 5 - 7 minutes:
- Press the phalanges of your fingers on your closed eyes;
- Apply compression for 10 - 15 seconds;
- Pause between pressure techniques 10 - 15 seconds;
- You need to repeat until the attack goes away.
With normal blood pressure, attacks of increased heart rate very rarely occur, unless the cause is a high load on the body or rapid movement.
If your heart rate increases due to high blood pressure, the following actions are recommended:
- Lie on the bed and relax your body;
- Take a small amount of cold water;
- Wash your face, neck and heart area with cold water;
- If the cause of this attack is a stressful situation, then you need to take sedatives;
- Take the drug - anaprilin;
- To prevent tachycardia, eat foods high in omega-3 (seafood and sea fish);
- If there is a lack of potassium in the body, take vitamins and medications that contain potassium.
At the time of pregnancy, the expectant mother’s body undergoes hormonal changes and big changes in order for the body to better adapt to the state of pregnancy. During this period, a rapid heartbeat is the normal state of a pregnant woman during this period (100 beats in 60 seconds or more).
But there are cases when tachycardia is accompanied by unpleasant and dangerous symptoms:
- Nausea leading to vomiting;
- Dizziness;
- Severe headache;
- Cramps in the stomach;
- Pain and spasms in the chest and heart muscle;
- Fainting;
- Attacks of groundless fear and causeless feelings of anxiety.
A positive mood, walks in the fresh air, relaxing with family and drinking enough clean water for the body will help get rid of the cause of such symptoms.
Hypoxia may be the cause of high heart rate. And this is a consequence of the expectant mother spending a long period of time in a stuffy room. Also due to the increased activity of the pregnant woman. A long period of hypoxia leads to underdevelopment of the nervous system and pathology in the endocrine system.
Attacks of strong heartbeat in women during pregnancy very often arise from a deficiency of iron in the body of the expectant mother, and the cause of a high pulse can be the disease anemia.
An attack of tachycardia in the first trimester of pregnancy is associated with hormonal changes and emotional stress. Also a factor in the rapid beating of the heart is an insufficient amount of potassium in the body of a pregnant woman.
In the second trimester, a woman gains weight, which increases the load on the heart muscle and vascular system.
With cardiac pathologies, a paroxysmal type of tachycardia may develop, which is accompanied by severe headache, dizziness and nausea. With a severe attack of rapid heartbeat, chest pain, convulsions and fainting may occur.
Treatment of high heart rate begins with diagnosis and identification of the causes of tachycardia. And the cardiologist, based on a diagnostic examination, prescribes a course of drug therapy. It is very important to eliminate the cause of the disease and relieve the patient of the symptoms that tachycardia causes: an attack of nausea, headaches, an attack of shortness of breath and fainting.
Two methods are used for treatment: therapy with medications and therapy with drugs based on medicinal plants and medicinal herbs.
| group of drugs | Name | dosage | course of therapy |
| cardiac glycosides | Digoxin | maximum daily dosage 1.5 mg, divided into 2 - 3 doses | course of treatment up to 7 calendar days |
| beta blockers | Atenolol | maximum dosage for an adult patient - 200 mg per day | the course of therapy is individual and established by a cardiologist |
| sedatives | Sedasen | 1 tablet, 2 times a day or 2 tablets once a day | admission course 14 calendar days |
| antioxidants | Preductal | 35 mg of the drug 2 times a day with meals | admission course up to 90 calendar days |
Treatment of tachycardia during panic attacks
Tachycardia during panic attacks can be cured by the following methods:
- working with a psychologist - this includes the use of special relaxation techniques based on systematic breathing controls;
- the practice of yoga, meditation, an example can be seen here;
- systematic exercise (walking, jogging in the fresh air, swimming);
- art therapy, mastering new skills;
- a healthy lifestyle, including proper nutrition, good sleep, maintaining the required level of vitamins and minerals in the body, and the absence of bad habits (abuse of alcohol, cigarettes).
Important! Treatment of tachycardia during a panic attack using tranquilizers and antidepressants should only be selected by the attending physician.
A panic attack without the occurrence of tachycardia indicates that the patient has vegetative-vascular dystonia of the hypotonic type.
What does an increased heart rate mean when you wake up in the morning?
Nocturnal tachycardia can occur as one of the symptoms of cardiovascular disease or as a result of the influence of other factors.
Cardiovascular diseases that can cause increased heart rate include:
- heart defects;
- myocardial infarction;
- bacterial endocarditis;
- cardiosclerosis;
- myocarditis of various origins;
- heart failure (usually left ventricular);
- severe angina;
- cardiac ischemia;
- cardiomyopathy;
- adhesive and exudative pericarditis.
Typically, heart problems cause tachycardia in older people.
In young people and children, rapid heart rate at night occurs as a result of the following factors:
- decreased adrenal function;
- bronchial asthma;
- obstructive pulmonary diseases;
- pneumothorax (accumulation of air in the pleural cavity surrounding the lung);
- acute allergic reactions;
- rheumatism;
- anemia;
- hypoxia (lack of oxygen);
- disturbances in the functioning of the endocrine or autonomic system;
- decreased blood glucose or sodium levels;
- hormonally active tumors
- thyrotoxicosis (thyroid disease).
Also, rapid heartbeat at night often occurs in adolescents during the period of hormonal changes.











