Meningitis: types and differences
Meningitis causes inflammation of the lining of the spinal cord or brain. It proceeds rapidly, without external signs. Meningococcal infection enters the body through blood and Haemophilus influenzae. In newborns, E. coli and enterococci can cause the disease.
The insidiousness of the disease lies in the impossibility of detecting it clinically. A person may not be aware of a dormant infection until the pathogen becomes active. The patient can become deaf and lose vision within a day. In most cases, these changes are irreversible.
A potential victim can only be identified by taking swabs from the nasopharynx during a medical examination or during mass testing due to a surge in incidence.
In 60% of cases, meningococcus is viral in nature. However, its early diagnosis is complicated by the similarity of symptoms to the common cold. Nausea, vomiting, and fever are extremely rare. Even less common is a hemorrhagic skin rash.
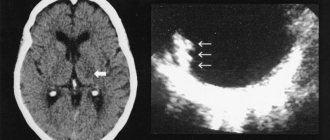
The main danger of the disease is infection of brain tissue by secondary encephalitis and cerebral edema. As a result, disturbances in the functioning of the nervous system appear.
The patient faces long-term disability. In severe cases, swelling develops into an abscess, supported by diseases of the nasopharynx.
All this together will inevitably lead to urgent surgical intervention. In addition to meningitis, meningococcus causes an even more terrible disease - meningococcal sepsis, or meningococcemia.
The infection leads to inflammation of the blood vessels and bleeding of internal organs. Bacteria kill a person within a few hours unless immediate intensive care is taken.
The first sign of an inflammatory attack is the appearance of red and purple lumps. Their pattern corresponds to the sites of internal bleeding. Unlike allergic rashes, the rashes fade when pressed.
Using these signs, it is easy to find out whether meningococcemia has appeared in children or adults. At the slightest suspicion, you should immediately call an ambulance.
Possible complications of meningitis include dementia, increased risk of Alzheimer's disease, and respiratory paralysis. Children are susceptible to delayed physical and mental development.
RESEARCH RESULTS
The ability of the Menactra vaccine to induce the development of immunological memory after primary vaccination is documented by data from clinical studies in both children and adults.
Results of 3 clinical studies conducted in children 9 to 18 months of age with single or double doses of Menactra vaccine alone or concomitantly with other pediatric vaccines (pneumococcal conjugate vaccine SPCV) or measles, mumps, rubella, and varicella (MMRV) vaccine). confirmed that most participants in the two-dose Menactra vaccine groups, alone or concomitantly with other pediatric vaccines, had an increase in the proportion of individuals with SBA titres of ~1:8 across all vaccine serogroups. In 91% and 86% of participants in the group with a separate two-dose administration of the Menactra vaccine, an increase in SBA titer>1:8 to serogroups A, C, Y, and to serogroup W-135, respectively, was observed. When a second dose of Menactra was administered concomitantly with PCV or with MRCV (or MRCV + Haemophilus influenzae vaccine), most study participants experienced an increase in SBA titer of ~1:8 (> 90 study participants in serogroups A, C and Y, and >81% of participants were classified as serogroup W-135). The SBA GT values turned out to be higher than the initial ones for all four serogroups of meningococci included in the vaccine.
Results from studies conducted in participants aged 11 to 18 years confirmed a significant immune response to a single dose of Menactra vaccine. The GTS values of SBA on the 28th day after vaccination turned out to be significantly higher than the initial ones. In addition, in 98-100 adolescents in whom the antibody titer was not initially determined to be “1:8”, by the 28th day there was a 4-fold (or more) increase in the SBA titer to all vaccine serogroups. The results obtained indicate the high immunogenicity of the vaccine in adolescents. When analyzing by sero group, it was revealed that in 93-100 adult participants in clinical trials with initially undetectable antibody titers of “1:8”, by day 28 there was a 4-fold (or more) increase in the SBA titer to all sero groups of the pathogen included in the vaccine . In each of the 3 studies, the immunological response induced by Menactra vaccine was similar when assessed by sex, age and race.
Kinetics of the immune response:
There are no data on the kinetics of the initial response to the Menactra vaccine, however, as with other polysaccharide and conjugate vaccines, immune protection can be observed 7-10 days after vaccination.
Duration of protection
The ability of the Menactra vaccine to induce the formation of immune memory after primary vaccination has been proven in clinical studies. One study demonstrated that the persistence of bactericidal antibodies in the blood three years after a single administration of the Menactra vaccine was higher compared to a group of vaccinated individuals who received a single immunization with a 4-valent polysaccharide meningococcal vaccine against serogroups A, C, Y and W-135. In the group vaccinated with the Menactra vaccine, a higher concentration of serum bactericidal antibodies was observed, as well as a higher proportion of individuals who had specific high-avidity antibodies, which indicates the formation of immune memory.
Indications for vaccination
Vaccination against meningitis is not yet included in the mandatory vaccination schedule. Therefore, for the most part, it is carried out voluntarily and at the expense of the parents.
It is done forcibly or on recommendation:
- Children attending preschool institutions;
- When traveling to areas with an unfavorable epidemiological situation;
- All children who live or have contact with the patient;
- Massively when a surge in infection is detected (20 people per 1000 population) or more.
Restrictions on swimming after vaccines
Among the basic rules that should be followed when washing after vaccinations, so as not to harm the baby, are:
- if daily washing has become a habit, it can be done if the baby is in normal condition, but the child should not stay in the water for too long;
- it is permissible to limit yourself to a warm shower, and not to bathe in the bathroom after vaccination;
- it is desirable to minimize the risk of temperature contrast between atmospheric temperature and water temperature - the water should be warm, not hot, so that children can bathe in it after injections;
- as antiseptics and sedatives, you can add chamomile decoctions, a couple of drops of lavender essential oil or an infusion of valerian herb to the bath;
- Do not bathe with a rough sponge or roughly rub the pricked area of skin with a pumice stone.
If the baby's temperature is elevated, in hot weather you can wipe the baby with a damp cloth without touching the injection site: this will help avoid overheating. In such a situation, it is better not to bathe the baby.
It is always necessary to get vaccinated on time, regardless of the possible inconvenience that may arise from the injection. Water procedures after vaccination are often not a contraindication: when it is possible to bathe a child after vaccination in a particular situation and after how long it is permissible to lift all restrictions on being in swimming pools, the doctor and the parent determine. The decision can be made based on the current state of the baby and his well-being. If there are no reactions to the vaccine or side effects, water procedures are possible at any time and approved by specialists - swim when necessary. An exception may be the Mantoux test, which cannot be wet at all - you can only wash it with it.
Watch a video about how long you should not bathe your child, go to the pool or get the vaccine wet
Share an interesting article with your friends on social networks.
source
Vaccination against meningitis
Due to the variety of pathogens that cause this disease, one vaccination against meningococcal infection is not enough. It is also necessary to protect yourself from pneumococci and Haemophilus influenzae. That is, a preventive course is required. Let's consider each of the vaccinations separately.
Vaccination against meningococci
Vaccinations against meningococcal infection are an effective means of fighting in epidemically disadvantaged areas. These vaccines are combined with protection against other diseases, such as tetanus. Depending on the composition of the vaccine, they are divided into groups, each of which defeats a specific pathogen.
In the Russian Federation, polysaccharide meningococcal vaccines of domestic and imported production are used. They are safe and well tolerated by children over two years of age. However, some manufacturers have achieved success and reduced the minimum age for using the vaccine to six months.
Among Russian drugs, one can note the bivalent meningococcal vaccine A+C. It is recommended to use it from one and a half years. However, in areas of infection, the age limit has been lowered to 6 months.
Belgian ACWY and American Menactra are popular among foreign drugs. They are used to vaccinate children over 2 years of age and adults. During periods of surge in incidence, the threshold for use is reduced to 9 months.
All of the above medications are supplied to pharmacies in dry form. Immediately before vaccination, the nurse dilutes it and administers it to the patient intramuscularly or subcutaneously.
Vaccination against Haemophilus influenzae
Defeating meningococcal infection is only part of preventing meningitis. This disease is also caused by Haemophilus influenzae. There aren't many vaccine options here.
The most commonly used is ACT – ZIB. The drug is available in the form of a dry powder, which is also diluted with a solution or other vaccine preparation immediately before vaccination.
It is a common practice to combine hemophilus serum with Tetracoccus-based DTP. Thanks to the compatibility of the two vaccines, a comprehensive vaccination is obtained against all pathogens of severe blood diseases at once.
Pneumococcal vaccine
And the final frontier is the pneumococcal vaccine. The most effective is the French Pneumo-23.
The lower limit of its use is 2 years, the maximum period of immunization is 10 years. Although it is administered once.
Another drug, Prevenar 13, is used to vaccinate infants. Four injections are enough to develop lifelong immunity. Two of them are done at intervals of 1.5 months, starting at 3 or 6 months.
The decision to send for vaccination is made by the attending pediatrician, based on the duration of breastfeeding. Revaccination is carried out 12 months after the last vaccination. You can check the recommended dates in the calendar.
Protein whey
Prevention of meningococcal infection using polysaccharide vaccines has a significant disadvantage - they do not cover group B meningococci. Its creation was prompted by the epidemic of meningitis in Cuba, which was caused by these viruses.
The first vaccine, VA-Mengor-BC, stopped the spread of infection, proving its effectiveness. A similar drug based on the outer membrane protein was created in Norway, where there was also an outbreak of group B meningitis.
Its use had to be abandoned in the future - its effectiveness was only 50%. For almost two decades, developers in many countries have been trying to develop a similar vaccine against meningococci, covered by group B virus. It was only in the 2010s that the MenB vaccine appeared.
Initially it was used in New Zealand, but in 2013 it was approved in Europe, and a little later here. In response, the Swiss company Novartis released the drug Bexsero. The effectiveness of the product is 88%.
Bexsero is marketed as a childhood vaccine because it is more suitable for injection into infants.
In Irkutsk, due to the threat of the spread of serous meningitis, vaccination of children has begun
Over the past month and a half, cases of infectious diseases have sharply increased in the city. Compared to last year's figures, the number of people infected has quadrupled.
Three hundred children were hospitalized. According to doctors, the increase in incidence is caused by sudden changes in temperature and high humidity. It rained continuously in the city for half of August. To stop the spread of infection, the vaccine was delivered to all clinics in the city. In schools and kindergartens, premises are being sanitized.
Contraindications and side effects
Vaccination is unacceptable for infectious diseases accompanied by fever or exacerbation of chronic pathologies. Also a serious obstacle is acute allergic intolerance to the components of the drug.
In some cases, side effects are possible. This is general weakness, exacerbation of diseases. Fever is rare. The symptoms go away on their own within a couple of days. If there is a large amount of redness or the post-vaccination period is severe, you should consult a doctor.
Everyone is up for vaccination
The first to go to the vaccination office are pensioners and mothers with children - those who are at risk. Pensioners know for sure that concomitant diseases - diabetes or hypertension - will only aggravate the course of the disease. Like any other chronic disease - kidney, lung, liver and others. Therefore, their presence is an indication for vaccination, just like pregnancy. To be vaccinated or not is, of course, voluntary. You can often hear: “Oh, I got vaccinated once and I was so sick!” I will never do it again!” But there are official statistics. And here's what she says: since 2011, the share of Muscovites who get flu shots has increased from 22 to 59 percent. Thanks to this, the incidence of influenza has decreased by 23 times! The health department plans to vaccinate at least 60 percent of the population this year.
Muscovites themselves choose where it is best for them to get vaccinated. Don't have time to get to the clinic? On your way to work, you can stop by a mobile vaccination site. The only documents required are a passport and written consent, which is issued on the spot.
There are enough free vaccines for everyone - now there are already more than a million doses of the domestic drug Sovigripp and Grippol+ in Moscow warehouses. The drugs are equally effective. As for side effects, they were recorded in only three percent of cases, with the vast majority being local redness and a slight increase in temperature.
Infographics "RG" / Leonid Kuleshov / Angelina Zhukova
Prevention and features of vaccination against meningitis
An unscheduled dose of vaccine is administered once. The maximum period between contact with the patient and the injection should not exceed 5 days. In areas of infection, prophylaxis is provided free of charge. Precautionary measures will help increase your chance of staying healthy, including:
- Maintaining personal hygiene - washing hands with soap, disinfecting personal belongings;
- Swimming only in designated places with lifeguard posts - the water is regularly checked there for the presence of infections;
- Regular wet cleaning of premises;
- Careful processing of products;
- Filtration and consumption of high-quality drinking water.
SPECIAL INSTRUCTIONS
Menactra vaccine should not be administered intravenously, subcutaneously, or intradermally because there is no data on the safety and effectiveness of the vaccine when administered subcutaneously, intravenously, or intradermally.
Do not mix Menactra vaccine in the same syringe with other vaccines or medications.
The vaccine has not been studied in persons with thrombocytopenia or bleeding disorders. As with other vaccines administered intramuscularly, the benefit versus risk of using the vaccine should be assessed in individuals at increased risk of bleeding from intramuscular injection.
The risk of developing Guillain-Barré syndrome (GBS) after vaccination with Menactra was assessed in a post-marketing retrospective cohort study. Cases of the development of GBS have been described, characterized by a temporal connection with the administration of the Menactra vaccine. Individuals who have previously been diagnosed with GBS may be at increased risk of developing this condition after receiving the Menactra vaccine. The decision to use Menactra vaccine in this situation should be made after assessing the potential benefits and risks.
The vaccine is not intended for the prevention of meningitis caused by other microorganisms or for the prevention of invasive meningococcal infection caused by meningococcal serogroup B in persons with an impaired immune status, as well as against the background of immunosuppressive therapy, a reduced immune response to the administration of the Menactra vaccine may be observed.
As with any vaccination, protective immunity may not develop in all 100 vaccinated people.
Before administering a vaccine, the health care provider or prescriber should inform the patient, parent, guardian, or other responsible adult of the potential benefits and risks associated with receiving the vaccine.
INFLUENCE ON THE ABILITY TO DRIVE VEHICLES AND OPERATE MACHINES
No studies have been conducted to study the effect of the vaccine on the ability to drive a car or use other machinery.
Controversy surrounding meningitis vaccinations
Meningococcal vaccinations cause heated debate among parents. Many people are concerned that infants are stuffed with vaccines every month. The first doses for hepatitis are administered already in the first hours of life.
Supporters of breastfeeding note that mother's milk reliably protects the growing body from infections, and unnecessary intervention only causes anxiety for the newborn.
Another group of opponents expresses concern about numerous scandals. Over the past few years, the country has been rocked by several major waves of discontent. Immunoglobulins purchased by healthcare institutions had the opposite effect.
Instead of protecting against serious diseases, including meningitis, they contributed to mass infection, and even drove some to the grave.
But we must take into account that the gradual deterioration of the environment directly affects the health of mothers and children. Babies are allergic even to breast milk. Vaccinations against meningitis and other serious diseases are the only way to improve the health of such children.
When and what vaccinations are given?
The vaccines that are most often used contain polysaccharides. They are administered to children from 2 years of age. Such vaccines can protect a child for 3 years. But most often (more than 50% of cases) meningitis occurs in children under two years of age. They are vaccinated with a weak immune response. The vaccine against meningococcal infection of group A is used only for children over one year old, group C - only up to the age of two. The vaccination is done only once.