Description of residual organic damage to the central nervous system
As you know, the central nervous system is a coherent system in which each of the links performs an important function.
As a result, damage to even a small area of the brain can lead to disruption in the functioning of the body. In recent years, damage to nervous tissue has been increasingly observed in pediatric patients. To a greater extent, this applies only to born babies. In such situations, a diagnosis of “residual organic damage to the central nervous system in children” is made. What is it and is this disease treatable? The answers to these questions worry every parent. It is worth keeping in mind that such a diagnosis is a collective concept that can include many different pathologies.
The selection of therapeutic measures and their effectiveness depend on the extent of the damage and the general condition of the patient. Sometimes residual organic damage to the central nervous system occurs in adults. Often, pathology occurs as a result of previous injuries, inflammatory diseases, and intoxication. The concept of “residual organic damage to the central nervous system” implies any residual effects after damage to nerve structures.
Reasons ↑
Despite the fact that the diagnosis of schizophrenia has existed for quite a long time, scientists have not fully identified the exact causes that influence the development of the disease. A number of theories have been put forward, which are confirmed by certain facts, but nothing more. The most common theories are:
- neurotransmitter, lies in the fact that representatives of this theory believe that the onset of the disease is provoked by an excess of the substance dopamine. Based on this theory, some treatment principles have been built that block the production of dopamine;
- The serotonin theory suggests that serotonin is produced in excess and leads to insufficient transmission of nerve impulses. New generation neuroleptics are developed taking this factor into account;
- the noradrenergic theory suggests the participation of adrenaline, dopamine and norepinephrine in the development of pathology;
- predisposition is both hereditary and constitutional. Many facts suggest that pathology can be transmitted from parents to children, as well as from other relatives. The greatest risk occurs when both parents have schizophrenia. Constitutional predisposition lies in the characteristics of a person’s character, his resistance to stress and temperament.
In addition to the described theories, there are also: psychoanalytic, dysontogenetic, autointoxication and cognitive theories.
What is residual encephalopathy
Residual organic damage to the central nervous system in children is diagnosed quite often. The causes of nervous disorders can occur both after the birth of a child and during pregnancy. In some cases, damage to the central nervous system occurs due to complications of childbirth. The main mechanisms for the development of residual organic damage are trauma and hypoxia. There are many factors that provoke nervous system disorders in a child. Among them:
- Genetic predisposition. If parents have any psycho-emotional disorders, then the risk of their development in the baby increases. Examples include pathologies such as schizophrenia, neuroses, and epilepsy.
- Chromosomal abnormalities. The cause of their occurrence is unknown. Incorrect DNA construction is associated with unfavorable environmental factors and stress. Due to chromosomal abnormalities, pathologies such as Down's disease, Shershevsky-Turner syndrome, Patau, etc. occur.
- The impact of physical and chemical factors on the fetus. This refers to unfavorable environmental conditions, ionizing radiation, and the use of drugs and medications.
- Infectious and inflammatory diseases during the formation of the nervous tissue of the embryo.
- Toxicoses of pregnancy. Late gestosis (pre- and eclampsia) is especially dangerous for the condition of the fetus.
- Impaired placental circulation, iron deficiency anemia. These conditions lead to fetal ischemia.
- Complicated childbirth (weakness of uterine contractions, narrow pelvis, placental abruption).
Residual organic damage to the central nervous system in children can develop not only during the perinatal period, but also after it. The most common cause is head trauma at an early age. Risk factors also include taking drugs that have a teratogenic effect and narcotic substances during breastfeeding.
The word “residual” is translated from Latin as residual. Residual encephalopathy indicates that pathological processes in the brain remaining after treatment of other diseases have led to the development of a serious complication. In some cases, several years pass after a previous illness before a person is diagnosed with encephalopathy.
ICD-10 code
According to the international classification of diseases ICD-10, residual encephalopathy has the code G93.4. If the complication arose after a head injury, then use the coding T90.5 or T90.8. When a doctor makes a diagnosis and indicates the disease code, it is necessary to specify in parentheses the reason for the disease, the degree of brain damage and the symptoms that bother the patient.
Difficulties in diagnosis
It is not always possible to easily diagnose this disease , since its initial symptoms are very similar to the behavioral changes characteristic of adolescence.
The transitional age is one of the most important and difficult for a person, since the child is looking for his place in the world, although he often lacks the knowledge to fully understand and understand what is happening around him.
Also, hormonal changes in the body affect the child’s behavior, and he cannot always control his emotions and correctly express his own thoughts. Because of these characteristics, many adults do not always react to the behavior of a teenager, associating it with hormones in the body, considering his actions normal.
But it is very important to diagnose the disorder as quickly as possible, since schizophrenia in the early stages is more treatable . Many psychiatrists, when diagnosing the early stage, describe such symptoms.
Previously kind, well-mannered, purposeful children become aggressive and their attitude towards relatives and close people changes for the worse. For no particular reason, rudeness, anger, or unexpected coldness may appear in their behavior. Sometimes the child moves away from the people around him, becomes cold and spends more and more time alone.
Tests for schizophrenia online
This is very noticeable, especially if before this the patient was positive, kind and had warm relationships with others. There may also be a decrease in school performance and shirking from household duties, apathy towards any mental or physical activity.
Sometimes children even neglect their own hygiene.
The adults around the child need to be very attentive in order to be able to distinguish the fine line between a child who has changed his behavior due to adolescence and a child with schizophrenia. Otherwise, the development of schizophrenia can lead to personality disintegration.
At the second stage, you can observe signs that clearly indicate the presence of mental disorders.
In this case you will see:
- reduced social activity and apathy;
- reduction of facial diversity;
- thinking disorders;
- decrease in vocabulary.
The patient’s speech becomes poorer, emotional intensity is reduced, a tendency to vagrancy and a break in social ties may appear due to social maladjustment. Very often, patients can experience eating disorders, which can be expressed, for example, by gluttony or anorexia nervosa.
All people with schizophrenia are alike. They lack initiative and are also unemotional. All actions of patients are repeated monotonously day after day, the person performs them automatically. Over time, the patient loses the ability to learn and absorb new material.
Also, a sign characteristic of the second stage of the disease is unfinished sentences. The patient does not bring his phrases to their logical conclusion. A quick transition in conversation from one topic to another, not related to the original one, is another characteristic feature of this stage.
Sometimes, in advanced cases, a person’s speech can be composed only of unrelated fragments of phrases that cannot be logically connected to each other. Some words lose their familiar sound or are replaced by new words.
Although this disease is not characterized by persistent delusions and the occurrence of visual or auditory hallucinations, sometimes you can observe how the patient seems to be listening carefully to something.
When diagnosing, psychiatrists do not rely on individual symptoms, but on all clinical signs in total. This includes information about cases of illness in the family and the development of a person throughout his life.
How is psychosis different from schizophrenia?
Causes of residual organic brain damage in children
It is customary to divide the reasons that caused the residual nature of changes in the brain into acquired and congenital. This is due to the fact that the factors and characteristics of brain damage received in childhood or in adulthood are different. Among the reasons that can lead to residual encephalopathy, doctors name:
- injury leading to concussion and death of brain cells;
- undergone surgery to remove a malignant brain tumor;
- meningitis;
- tick-borne encephalitis;
- stroke;
- bad habits – consumption of alcohol, psychotropic substances, narcotic substances;
- exposure to ionizing radiation;
- diabetes;
- difficult pregnancy and childbirth.
The occurrence of residual encephalopathy can be influenced by disturbances in the functioning of the kidneys and liver, which contribute to an increase in the level of urea in the blood. The substance has a destructive effect on brain cells. Another common cause of the development of residual encephalopathy is vascular atherosclerosis, leading to a cessation of oxygen supply.
Signs of perinatal encephalopathy in children are caused by the consequences of intrauterine disorders that are congenital in nature. The reason may be:
- fetal hypoxia;
- intrauterine infection;
- negative heredity;
- birth injuries;
- the lifestyle that the mother led when she was pregnant.
With timely diagnosis of encephalopathy, it is possible to cure the child without consequences. The acquired form in children can cause:
- head injury;
- viral infection;
- exposure to radiation.
A child, unlike an adult, cannot talk about his problems, so you need to carefully monitor his behavior in order to prevent the consequences of perinatal encephalopathy before they become irreversible. If this is not done on time, the disease threatens to develop into hydrocephalus, mental retardation or cerebral palsy. Frequent, causeless crying, irritability, and lack of normal sleep in the child may be a cause for concern for parents.
In adulthood, signs of residual organic damage are observed less frequently, however, they are present in some patients. Often the cause of such episodes is trauma received in early childhood. At the same time, neuropsychic abnormalities are long-term consequences. Residual organic brain damage occurs for the following reasons:
- Post-traumatic illness. Regardless of when the damage to the central nervous system occurs, residual symptoms remain. These often include headaches, seizures, and mental disorders.
- Condition after surgery. This is especially true for brain tumors, which are removed using nearby nerve tissue.
- Taking drugs. Depending on the type of substance, the symptoms of residual organic damage may differ. Most often, serious disorders are observed with long-term use of opiates, cannabinoids, and synthetic drugs.
- Chronic alcoholism.
In some cases, residual organic damage to the central nervous system is observed after inflammatory diseases. These include meningitis and various types of encephalitis (bacterial, tick-borne, post-vaccination).
The residual type of encephalopathy according to the ICD has code G93.4. If changes in the brain are caused by a head injury, then the doctor may indicate the code T90.5 or T90.8. The disease is considered dangerous because can lead to serious complications. It is divided into degrees that correspond to the severity of the disease: mild, moderate and severe.
The main classification involves division into 2 types: perinatal and acquired. They determine the genesis of the disease and occur with special symptoms, which is important to consider when making a diagnosis.
Perinatal type
Congenital residual encephalopathy manifests itself in childhood and increases the risk that the child will become disabled. It occurs when the child’s brain is damaged during pregnancy or during childbirth, as well as in the first days after birth.
An increased likelihood of this disease occurring is present in those whose mother experienced severe symptoms of toxicosis or experienced premature birth. The main reasons for the development of the disease are as follows:
- Birth injury;
- Fetal hypoxia;
- Genetic brain mutations;
- Fetal asphyxia;
- Intrauterine infection;
- Rhesus conflict.
If an illness associated with pregnancy occurs, special attention should be paid to the affected baby in order to reduce the risk of complications.
Acquired type
The residual genesis of the acquired type is secondary. As a rule, the disease is detected in adults from 18 to 50 years old. At risk are people who have suffered spinal or head injuries, brain damage or infections.
Main reasons:
- Congenital cerebral pathologies;
- Brain injuries;
- Stroke;
- Toxic effects on the brain;
- Inflammation of nerve tissue in the brain due to infections or endocrine diseases;
- Vascular damage due to atherosclerosis;
- Abuse of psychotropic drugs or antipsychotics;
- Hypertension combined with manifestations of hypertensive crisis;
- Pathologies of the liver or kidneys.
In adults, the disease occurs with less consequences, but in some cases dangerous complications can still occur.
Residual mental disorders
Read:- F65.8 - Other disorders of sexual preference
- Nutritional disorders
- AUTOIMMUNE DISORDERS
- Affective disorders
- Affective disorders (F3)
- WHITE MATTER OF THE SPINAL CORD (CONDUCTING APPARATUS); CONDUCTION DISORDERS
- WHITE MATTER OF THE SPINAL CORD (CONDUCTING APPARATUS); CONDUCTION DISORDERS
- Painful memory disorders.
- Delusional (paranoid) disorders
- As a result of a closed spinal cord injury, the patient experienced acute urinary and fecal retention. Which pathways are affected by these disorders?
The heading “Residual mental disorder and mental disorder with late (delayed) onset” is highlighted in ICD-10 to designate disorders caused by psychoactive drugs that continue beyond the period of direct action of the substance and are characterized by disturbances in cognitive functions, personality or behavior. Changes in mental activity that occur as a result of chronic drug use can be included in this category and coded as F18.7. According to diagnostic guidelines, the occurrence of a disorder must be directly related to the use of the drug and be a change or a pronounced increase in the previous and normal state.
Residual mental disorders in this type of addiction are represented by three groups. The first includes persons with personality and behavior disorders (category F18.71 according to ICD-10). In the second group, along with personality and behavioral disorders, cognitive impairments are observed (headings F 18.71 and F 18.74). In patients of the third group, dementia is diagnosed (F18.73).
Personality and behavior disorder meets the criteria for organic personality disorder (F07.0), dementia - the general criteria for dementia (introduction to section F00-F09 of ICD-10). For the code “Other persistent cognitive impairment” in ICD-10 there are no clear diagnostic guidelines, only that it does not meet the criteria for amnestic syndrome or dementia. Therefore, it seems appropriate to correlate it with category F06.7 - “Mild cognitive impairment” (section F00-F09 “Organic, including symptomatic, mental disorders”) and be guided by its diagnostic guidelines.
When studying the dependence of the type of residual mental disorder on the length of drug abuse, it was found that within 2 years of their active use, personality and behavior disorders and persistent cognitive impairment are predominantly formed. In the 3rd year, the risk of developing dementia increases (Kozyreva, 2002).
In patients of the 1st group (personality or behavior disorder), the ability for purposeful activity is significantly reduced, emotional lability appears: causeless fun is easily replaced by hypothymia, anxiety, and irritability. Emotions become superficial and uncontrolled. Euphoria is devoid of true fun; against its background, a tendency to flat, inadequate jokes is revealed. Periodically, unreasonable outbursts of anger and aggression arise. Character
Residual mental disorders 365
The turn is a lack of higher personality traits: lack of intellectual interests, weakness of moral principles, disinhibition of instincts. Generally accepted norms of behavior are not observed, which often causes conflicts with the law. The inability to foresee the consequences of one's actions is typical. Patients are not aware of the problems created by their behavior to others, or neglect them. These disorders persist for at least 6 months, which is one of the diagnostic criteria.
With a certain degree of convention, patients in this group can be distinguished into two types of personality and behavior disorders - explosive and unstable. The explosive type is characterized by increased affective excitability, explosiveness, a tendency to wander, increased sexuality, and a desire for new experiences - “sensory thirst.” In the company of peers, these children and adolescents more often occupy a leading position, proving their superiority through physical violence and rudeness. An unstable type of personality and behavior disorder is characterized by weakness of the volitional sphere, instability of attachments, carelessness, lack of pride and determination, unmotivated euphoria, and a weak reaction to reproach and punishment. The leading motive for behavior is to obtain momentary pleasure. Children and teenagers easily fall under the influence of others and find themselves “on the sidelines” in companies. They commit offenses out of a desire to establish themselves in a reference group and earn the respect of stronger peers.
In patients of group 2 (where personality and behavioral disorders were combined with cognitive impairment), clinical expressions of personality disorders and behavior generally correspond to those in patients of group 1. In addition to the explosive and unstable types, an apathetic type of personality and behavior disorder is identified here, indicated by passivity, lethargy, reluctance to do anything, and indifference to the environment. In patients in this group, personality and behavioral disorders are accompanied by cognitive impairment, which indicates the next stage in the formation of residual mental disorders as a result of drug use. The clinical picture of cognitive impairment includes deterioration of memory, intelligence, and concentration. Patients experience difficulty in solving problem situations. Spatial and abstract thinking suffers. An indispensable criterion for diagnosis is a decrease in the results of experimental psychological studies of intellectual functions. Firstly, this is one of the ICD-10 diagnostic requirements for the category “Mild cognitive impairment”. Secondly, this approach allows us to differentiate the subjectively perceived difficulties of comprehension and memorization, which almost all patients complained about, from true impairments of cognitive functions, recorded only through experimental psychological research.
Patients of the 3rd group, who are diagnosed with dementia, have such a pronounced decrease in intellectual functions that this leads to disruption of their adaptation to everyday life. They lose self-care skills, discover previously uncharacteristic sloppiness, and lose interest in their surroundings. Memory impairments are combined with pathology of mental operations. The ability to abstract, generalize, highlight similarities and differences, and form problem-solving behavior suffers. The ability to reason, understand, and learn decreases. Speech becomes slow, vocabulary becomes poor, and patients have difficulty verbalizing their thoughts. Switching of attention suffers, which is manifested by difficulties in conversation when moving from one topic to another. From emotional disturbances to
Dependence on volatile solvents
In some cases, the apathetic manifestations that predominate here come to the fore, in others - extreme irritability, impulsiveness, brutality (explosive type), in others - an elevated mood background with a touch of euphoria and complacency, carelessness (unstable type).
Data regarding the reversibility of cognitive impairment and their functional nature are worthy of attention. All children and adolescents note that during the period of active drug use, they studied “disgustingly” at school; their memory and intelligence sharply deteriorated. They forgot the multiplication tables, could not remember what they read, could not memorize a short poem, and found it difficult to perform simple arithmetic operations. From pedagogical and medical documentation it became known that during the experimental psychological study of intellectual functions at that time, patients demonstrated low and sometimes extremely unsatisfactory test results. However, at the time of examination, cognitive impairment is not detected in all patients, which may indicate that it is reversible in children and adolescents. Since some patients are examined outside the period of active drug use, their intellectual functions could significantly improve during abstinence. In addition, often the subjective complaints of patients in the first group about poor memory, intelligence, and inability to concentrate do not find objective confirmation when performing tests. Probably, the cause of these disorders is not a real decrease in intellectual functions in itself, but personality changes that arise as a result of the use of drugs: restlessness, weakness of will, lack of determination, rapid exhaustion, fatigue. This does not allow patients to cope with school normally, creating the impression of true intellectual decline.
The presented variants of residual mental disorders due to drug use are, in fact, stages of the formation of a psychoorganic syndrome based on toxic encephalopathy caused by chronic intoxication with inhalants. Manifestations of the initial stage include personality and behavioral disorders (group 1, “Personality and behavior disorder”), occurring in the explosive and unstable types. With increasing experience of inhalant abuse, they are joined by subjective complaints from patients about rapid fatigue, difficulties in assimilating new information, deterioration of memory and intelligence, which does not find objective confirmation in experimental psychological studies of intellectual functions. For this reason, this period in the development of the disease can be designated as the stage of functional cognitive impairment. At the same time, based on the test results, these patients adequately assess their intellectual abilities (subjectively aware of the problems in this area, they assess their own mental abilities as low). However, this does not prevent them from being carefree, self-satisfied, self-sufficient, and independent. They are prone to rapid mood changes, variability of interests, and instability in stressful situations. They are often irritable, unrestrained, hot-tempered, and incapable of self-control in emotionally significant situations. Their self-assessments of character, health, and success in life also seem somewhat inflated, especially in connection with existing behavioral and personality disorders, which allows us to conclude that there is a slight decrease in critical resources.
The results obtained by experimental psychological methods in the study of the intellectual-mnestic activity of subjects in dynamics allow us to qualify the next stage of the formation of psychoorganic syn-
Treatment
Roma - stage of persistent cognitive impairment (group 2, “Personality and behavior disorder. Persistent cognitive impairment”). Here, the intellectual indicators obtained by the Wechsler test are at a borderline level. The functions of working memory, attention (activity, switchability, concentration), general understanding, and the ability to form conclusions based on common sense are especially reduced. In an initially normal state, nonverbal intellectual functions may remain relatively intact. As for the verbal functions of intelligence, then, regardless of the initial premorbid state, as a result of using LR, they decrease to a borderline level. Personality and behavior disorders in this group are more pronounced. They fit mainly into the framework of the explosive type, although during this period the apathetic type of these personality disorders and behavior appears. The results of psychological testing indicate that there is a worsening of the features characteristic of patients of the first group. Impulsivity, emotional imbalance, and tension increase. Behavior is characterized by inappropriately strong reactions in relation to the stimuli that cause them. At the same time, self-confidence and satisfaction with one’s own behavior increase. Despite the decline in intellectual indicators and the worsening of behavioral and personality disorders, self-esteem of intelligence, character, health, and success in life remains at the same level. These results indicate a further decrease in critical resources, however, in a number of patients there is an awareness of the causes of existing disorders and a desire to be cured.
As the disease progresses, there is a further decrease in intellectual indicators (group 3, “Dementia”). They descend to the level of mild mental retardation, mainly due to the verbal functions of the intellect. A sharp narrowing of the range of interests, lack of activity and initiative, passivity and inactivity come to the fore, which is reflected in the results of psychological testing. Against this background, short-term reactions of irritation and anger easily arise. Self-service skills are lost. The predominant types of personality disorders here are apathetic and explosive. Critical abilities are sharply reduced, patients are not able to adequately assess their existing impairments, which manifests itself in inflated self-esteem of mental abilities, character, success in life, and excessive self-satisfaction. There is a complete lack of focus on healing and stopping drug use. Ultimately, the disease leads to personal degradation and social maladaptation of children and adolescents, making them virtually helpless.
Date added: 2015-09-03 | Views: 354 | Copyright infringement
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | 100 | 101 | 102 | 103 | 104 | 105 | 106 | 107 | 108 | 109 | 110 | 111 | 112 | 113 | 114 | 115 | 116 | 117 | 118 | 119 | 120 | 121 | 122 | 123 | 124 | 125 | 126 | 127 | 128 | 129 | 130 | 131 | 132 | 133 | 134 | 135 | 136 | 137 | 138 | 139 | 140 | 141 | 142 | 143 | 144 | 145 | 146 | 147 | 148 | 149 | 150 | 151 | 152 | 153 | 154 | 155 | 156 | 157 | 158 | 159 | 160 | 161 | 162 | 163 | 164 | 165 | 166 | 167 | 168 | 169 | 170 | 171 | 172 | 173 | 174 | 175 | 176 | 177 | 178 | 179 | 180 | 181 | 182 | 183 | 184 | 185 | 186 | 187 | 188 | 189 | 190 | 191 | 192 | 193 | 194 | 195 | 196 | 197 | 198 | 199 | 200 | 201 | 202 | 203 | 204 | 205 | 206 | 207 | 208 | 209 | 210 |
Symptoms
Signs of residual encephalopathy appear slightly at the initial stage. The nature of the violations can be varied. With encephalopathy, the nervous and cardiovascular systems suffer, weakening of memory, attention, and coordination disorders occur. A person should see a doctor if the following symptoms are present:
- insomnia;
- frequent headache;
- weakness;
- dizziness;
- increased excitability;
- constant fatigue;
- anxiety.
With complications, the patient quickly gets tired, convulsions, partial or complete paralysis occur. There are often cases when, with residual encephalopathy, the victim falls into a coma. A decrease in mental abilities is directly related to impaired blood circulation in the brain. If residual phenomena are left unattended, the process may become irreversible.
Signs of residual encephalopathy depend on its type. This greatly complicates diagnosis and accurate diagnosis. Nevertheless, with the help of knowledge of the symptoms characteristic of the disease, it is possible to preliminarily assess whether a person really has signs of developing such encephalopathy.
Often, the appearance of the first symptoms indicating residual encephalopathy leads to the idea that the baby has developed degenerative diseases. Therefore, doctors begin to look for a completely different disease.
How residual encephalopathy manifests itself in children:
- Increased excitability, sleep problems;
- Vivid negative reaction to sounds, light;
- Neurotic disorders (irritability, nervousness);
- Increased intracranial pressure;
- Sucking reflex disorders;
- Protrusion of the eyeballs;
- Pyramidal insufficiency syndrome (left-sided or right-sided);
- Lethargy, lack of desire to play, bad mood;
- Disturbances in motor functions;
- Nausea, vomiting;
- Episodic cephalgia;
- Problems remembering information;
- Decreased mental abilities;
- Jaundice.
The manifestation of the disease depends on the location of the lesion. However, some symptoms may be absent.
Acquired residual encephalopathy is characterized by a gradual development of the disease and symptoms, which increases the likelihood of a later detection of the problem. The symptoms are similar to the perinatal type of the disease, but most of its manifestations are special.
Symptoms of acquired residual encephalopathy:
- Severe headaches;
- Problems with concentration and memory;
- Decreased brain activity;
- Fatigue, daytime sleepiness, severe weakness;
- Mood instability;
- Mental disorders;
- Insomnia;
- Hyperreflexia, muscle hypertonicity;
- Paralysis;
- Parkinson's disease;
- Convulsive syndrome;
- Deterioration of hearing, vision;
- Numbness of the tongue and lips;
- Retardation of movements, loss of coordination.
Sometimes patients may lose consciousness, but this manifestation of the disease is very rare. However, if it occurs, there is an increased risk of complications.
What is a simple form of schizophrenia?
Simple schizophrenia is a relatively rare variant of schizophrenia , the onset of which is most often observed in childhood and adolescence.
This disease manifests itself as apathy, decreased initiative, an indifferent attitude towards the world around us, a lack of interest in establishing relationships with people, as well as a noticeable decrease in the level of productivity in educational or professional activities.
It is important to note that this form of schizophrenia is characterized by slow progressive development, sometimes it can appear only a couple of years after the onset of the disease .
Delusions and hallucinations almost do not appear in the early stages of such schizophrenia; they are more characteristic of the onset of the disease, so the patient looks like an ordinary person who does not suffer from clouding of reason.
However, as the disorder progresses, more characteristic symptoms will appear.
Mechanism of development of central nervous system lesions
Residual damage to the central nervous system is always caused by unfavorable factors that preceded it. In most cases, the basis for the pathogenesis of such symptoms is cerebral ischemia. In children, it develops during the period of intrauterine development. Due to insufficient blood supply to the placenta, the fetus receives little oxygen.
As a result, the full development of nervous tissue is disrupted, and fetopathy occurs. Significant ischemia leads to intrauterine growth retardation and the birth of a child before the gestational age. Symptoms of cerebral hypoxia can appear already in the first days and months of life. Residual organic damage to the central nervous system in adults often develops due to traumatic and infectious causes. Sometimes the pathogenesis of nervous disorders is associated with metabolic (hormonal) disorders.
PROGNOSIS FOR SCHIZOPHRENIA
It is possible to predict more or less favorable clinical dynamics of schizophrenia, taking into account the factors listed below.
| Prognosis factors | P R O G N O Z | |
| Relatively Favorable | Relatively Unfavorable | |
| Floor | Female | Male |
| Constitution | Picnic | Asthenic |
| Morphodysplasia | None | More than three |
| Birth season | ? | Cold season |
| Upbringing | Symmetrical family | Asymmetrical and single-parent family |
| Premorbid | Norm | Schizoid |
| Initial period | About a month | More than a year |
| Manifest period | Polymorphic and acute with productive disorders, up to 14 days | Monomorphic, prolonged, negative disorders, more than 2 months |
| Intelligence | High | Short |
| First remission | Full, more than 3 years | Partial, less than a year |
| Family | Full | Divorced |
Diagnostics
Making a diagnosis of residual encephalopathy is a difficult task. This is due to the fact that the disease very often occurs with symptoms that may indicate several pathologies at once. Also complicating the process of finding an accurate diagnosis is the long period of time that has passed since the event when the brain tissue was damaged. Sometimes the result is an incorrect diagnosis, which is why the patient begins to take pills that do not help him at all.
The conversation between the patient and the doctor is of great importance in diagnosis. A detailed description of symptoms, personal observations, features of the manifestation of certain sensations - all this is of great importance in identifying the disease.
For diagnosis, the patient is prescribed many procedures:
- EEG;
- EchoEG;
- CT;
- MRI;
- NMR;
- UZDS;
- Doppler ultrasound;
- REG.
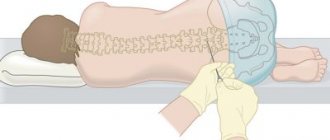
Additionally, you will need to take classic blood and urine tests, as well as conduct a cerebrospinal fluid test. After a complete examination, the doctor will be able to make a final diagnosis.
The main task of the doctor is to establish the relationship between the symptoms of encephalopathy and brain damage. If several months have passed since the injury, this is more difficult to do. An initial survey of the patient and assessment of his complaints will help to draw the right conclusion. However, the most accurate diagnostic method is considered to be a complete examination for encephalopathy, including:
- Electroencephalography. The procedure is carried out to study the functioning of brain cells. Helps determine the extent of the disease.
- MRI is necessary for a detailed study of processes in the body that occur at the cellular level.
- Computed tomography serves as an additional method to confirm the diagnosis. CT scan is prescribed when there is doubt after previous examinations.
- X-ray of the skull, craniography.
A biochemical blood test clarifies the clinical picture. It is an additional method for diagnosing encephalopathy, like a urine test. Carrying out all the studies helps to exclude other diseases whose symptoms are similar to those of residual encephalopathy. The future successful treatment strategy prescribed by the doctor depends on the accuracy of the diagnosis.
Syndromes with residual organic damage to the central nervous system
In neurology and psychiatry, several main syndromes are distinguished, which can occur either independently (against the background of a brain disease) or be regarded as a residual lesion of the central nervous system. In some cases, a combination of these is observed. The following signs of residual organic damage are distinguished:
- Cerebrasthenic syndrome. Its manifestations are considered to be increased fatigue, unsatisfactory mastery of the school curriculum, general weakness, tearfulness, and mood changes.
- Neurosis-like syndrome. It is characterized by the development of phobias, enuresis (uncontrollable urination at night), and motor agitation (tics).
- Hyperactivity and attention deficit disorder. It is observed in children of primary and secondary school age.
- Encephalopathy. The main manifestations are sleep disturbance, loss of memory, and perseverance. In severe cases, focal neurological symptoms and seizures are observed.
- Psychopathy. Characterized by disobedience and aggressiveness. In adulthood – mood lability, hysterical reactions, antisocial behavior.
Most often, cerebral hypoxia leads to diffuse symptoms, when the listed syndromes are combined with each other and are not very pronounced. The predominance of focal symptoms is rarely observed.
Treatment
It is quite difficult to make a prognosis in advance when treating a disease. This is due to the fact that residual encephalopathy in an adult or child is resistant in nature, i.e. resists medications. Therefore, the recovery process becomes unpredictable and difficult.
Once the final diagnosis has been made, treatment can begin. The main goal is to restore blood circulation in the brain tissues, as well as the general condition and relieve all unpleasant symptoms.
To begin with, the patient is prescribed therapeutic procedures, which sometimes successfully cope with the disease without taking any medications. These include:
- Manual therapy (massage);
- Acupuncture;
- Physiotherapy;
- Osteopathy;
- Phytotherapy;
- Reflexology;
- Contrast morning shower;
- Conversations with a psychotherapist;
- Sanitary resort treatment.
After repeated procedures, the patient will feel much better. If such methods are not effective enough, the doctor prescribes medication. Some are given intravenously, but most are taken in pill form. The following groups of drugs are prescribed:
- Neuroprotectors;
- Nootropics;
- Antioxidants;
- Cerebral circulation normalizers;
- CNS stimulants;
- Hormonal;
- Sedatives;
- Immunomodulators;
- Anticonvulsants;
- Nonsteroidal anti-inflammatory drugs;
- Vitamin complexes.
The exact treatment can only be prescribed by a doctor. Self-administration of random medications can lead to severe side effects and dangerous complications, which can only be dealt with in a hospital setting.
Residual changes in the brain are very dangerous. If you delay, there is a high risk of encountering serious complications. It will be difficult to cure them, and recovery from the underlying illness will take a long time. Therefore, it is important to consult a doctor immediately after the first symptoms appear.

Treatment of residual organic damage is aimed at strengthening the nervous system and rehabilitating a person in society. It is important to understand that the patient’s loved ones must be patient. With the right approach, treatment can significantly improve the prognosis of the disease. Nootropic, sedatives, antipsychotics, tranquilizers and psychostimulants are used as drug therapy.
After the examination, the patient is sent to the clinic where he will be observed. The main goal of treatment procedures for encephalopathy is to restore blood circulation in the brain tissue. If it is not possible to return to full activity, then treatment should be aimed at alleviating the patient’s condition and relieving unpleasant symptoms. To begin with, therapeutic methods are used that do not require the use of medications:
- Manual therapy. Massage of the neck, head, and upper back helps improve blood microcirculation.
- Acupuncture and acupressure. The reflexology technique helps to restore lost functions by influencing the necessary points.
- Physiotherapy. Special gymnastics recommended by a doctor increases the overall tone of the body and restores blood flow to the affected areas.
If these types of therapy do not cure the encephalopathy, then the use of medications is required. The most effective medications include tablets and injections:
- neuroprotectors - Gromecin, Cerebrolysin, Glycine, Ceraxon, Actovegin;
- antioxidants – Thioctic acid, Mexidol, Synergin;
- vitamins for restoring thought processes - Vitrum Memory, Gerimax Energy, Supradin, Griffonia;
- drugs for dizziness - Tagista, Vestibo, Betaserc.
The most effective treatments
The drugs used in treatment are antipsychotics , antidepressants , psychostimulants and other medications that normalize metabolism and brain activity. The use of traditional antipsychotics is undesirable , as this can only aggravate negative symptoms.
Treatment of a simple type most often does not require hospitalization and occurs on an outpatient basis, but if the patient is hungry, has thoughts of suicide, or shows strong aggression towards others, then hospitalization is necessary. This is necessary so that the patient does not harm himself or the people around him.
It is important for the patient to take the medications prescribed to him on time, and also to be constantly under the supervision of a doctor, regularly visiting him to adjust the dosage and list of medications. It is advisable for the patient to adhere to proper nutrition so that his body receives all the necessary microelements.
Treatment should consist not only of medication, but also psychotherapy, which involves psychotherapy for the patient and his family. Such sessions are aimed primarily at rehabilitating the patient for life in society.
Only comprehensive treatment will help to get good results and speed up recovery. But patients do not always believe that they need medical care and deviate from interacting with a doctor.
Even despite remission, the patient will still need maintenance therapy, as well as a course of adaptation to society. Of course, cases of complete recovery from schizophrenia have occurred very rarely, but high-quality and timely treatment will help reduce the rate of progression of the disease, reduce the manifestation of symptoms, and also speed up the onset of remission.
The development of modern medicine allows a patient with schizophrenia to live normally to one degree or another. Since this form mainly affects adolescents, it is very important to predict the disease as early as possible in order to save the child from irreversible consequences.
Clinical picture of CNS damage
Most often, symptoms of residual organic damage to the central nervous system appear some time after exposure to an unfavorable factor. With perinatal fetal hypoxia, disturbances can be noticeable already in the first month of life. Depending on the extent of the damage, the following symptoms may be observed:
- Minor damage to nervous tissue: tearfulness, poor sleep, memory loss. At school age, a child may experience attention deficit hyperactivity disorder, a tendency to hysterical states, and phobias.
- Damage to the central nervous system of moderate severity has such manifestations as constant crying, breast refusal, convulsive syndrome, and enuresis.
- In severe cases, focal neurological symptoms are observed. This includes muscle weakness, paresis and paralysis of the limbs, delayed physical and mental development, generalized convulsions, etc.
Predictions and consequences
The consequences of residual organic damage to the central nervous system depend on the degree of the disease and the approach to treatment. For mild disorders, complete recovery can be achieved. Severe damage to the central nervous system is dangerous due to the development of conditions such as cerebral edema, spasm of the respiratory muscles, and damage to the cardiovascular center. To avoid such complications, constant monitoring of the patient is necessary.
The subsequent prognosis after diagnosis depends on the severity of brain damage and the time that has passed since the discovery of encephalopathy. When the right treatment is chosen, a person has a chance of recovery. For perinatal encephalopathy diagnosed in a child after birth, modern methods of therapy will help to recover in infancy.
When patients do not seek medical help, consequences may occur:
- cerebral paralysis;
- hydrocephalic syndrome;
- vegetative-vascular dystonia;
- residual brain dysfunction;
- Parkinson's disease;
- cerebral hypertension;
- epilepsy.
Concept and code according to ICD-10
- Residual encephalopathy is a type of brain pathology in which the death of a certain group of nerve cells occurs without the possibility of their subsequent restoration.
- This disease is not an independent disease.
- The development of pathology occurs when the underlying disease is treated incorrectly or incompletely, which has a negative effect on the brain.
- Residual encephalopathy can develop at a rapid pace and provoke serious deviations in the performance of vital body systems.
- Features of the disease:
- symptoms of residual encephalopathy may appear several years after treatment of the underlying disease;
- According to ICD-10, the pathology is assigned the number G93.4 - “unspecified encephalopathy.”
Residual encephalopathy of perinatal origin is a separate type of pathology that develops during gestation or during childbirth.
The diagnosis is made when the disease occurs from the 28th week of pregnancy until the end of the first week of life of the newborn child. The provoking factor is negative influences and brain damage.
https://www.youtube.com/watch?v=ytcopyrightru
The risk of developing residual encephalopathy of perinatal origin increases with the following factors:
- multiple pregnancy;
- premature or late birth;
- mother's age is over 40 or under 20 years;
- placental abruption during pregnancy;
- taking potent medications during pregnancy;
- other types of complications of a woman’s condition during pregnancy.
Residual encephalopathy develops against the background of death of nerve cells in the brain. This condition can be provoked by numerous external and internal factors affecting the child in the prenatal period or after birth.
Identifying the exact cause of the pathology is difficult in some cases. To determine the provoking factor, a special set of examinations of the small patient is carried out.
The following factors can provoke the development of residual encephalopathy:

Hereditary predisposition.- Consequences of traumatic brain injuries (regardless of the child’s age).
- Atherosclerotic lesion of cerebral vessels.
- Increased levels of bilirubin and urea.
- Fetal hypoxia during intrauterine development.
- Negative effects of toxins on the fetus or the child’s body after birth.
- Inflammatory processes of the nervous tissue of the brain.
- Consequences of fetal infection.
- Cerebrovascular accident.
- Instability of blood pressure.
- Complications of vegetative-vascular dystonia.
- Complications of viral and infectious diseases.
Residual encephalopathy can be congenital or acquired. In the first case, the pathology develops during the period of intrauterine formation of the fetus, in the second it arises due to certain negative factors affecting the child’s body after his birth.
Based on severity, residual encephalopathy is divided into three categories. At the initial stage of pathology development, brain tissue is affected. With moderate severity, clinical symptoms become more pronounced. The severe form is accompanied by persistent neurological disorders.
Congenital residual encephalopathy is divided into the following types:
- anoxic;
- radial;
- diabetic;
- metabolic;
- bilirubin.
Symptoms and signs
The symptoms of residual encephalopathy have some features that distinguish it from other forms of this pathology.
Over a long period of time, the disease can develop in a latent form.
For example, if a child received a head injury, as a result of which the nerve cells of the brain began to die, then encephalopathy may appear several years after the incident. The intensity of the signs of the disease depends on the degree of progression of the pathological process.
Signs of the development of residual encephalopathy may include the following conditions:
- Sleep disturbance and moodiness.
- Inappropriate reaction to various stimuli.
- Impaired memory and intellectual abilities.
- Regular attacks of vomiting and nausea.
- Lack of sucking reflex in infancy.

Muscle hypertonicity.- Movement disorders.
- Bulging eyes.
- Emotional lability.
- Heartbeat disturbance.
- Weak or late cry at birth.
- General weakness of the body and apathy.
- Excessive fatigue.
Residual encephalopathy can have an extremely negative impact on all systems of the child’s body. The disease provokes dysfunction of certain parts of the brain, which cause the progression of irreversible pathological processes.
Children who suffered from this disease in childhood are lagging behind in physical, mental and speech development. Additionally, complex diseases develop that change the quality of life and shorten the life cycle.
Complications of residual encephalopathy can be the following pathologies:
- cerebral paralysis;
- progressive dementia;
- Parkinson's disease;
- vegetative-vascular dystonia;
- epilepsy;
- developmental delay.
Diagnostics
- Diagnosis of residual encephalopathy is a complex process that includes many laboratory and instrumental techniques for examining a small patient.
- In the early stages of the development of pathology, its symptoms can develop in a latent form.
- The only way to detect the disease is a comprehensive examination of the child’s brain.
- The following procedures are used for diagnosis:
- electroencephalography;
- MRI of the brain;
- CT scan of the brain and internal organs;
- general blood and urine analysis;
- nuclear magnetic resonance;
- Doppler ultrasound;
- biochemical analysis of blood and urine;
- cerebrospinal fluid puncture.
Several treatment methods are used in the treatment of residual encephalopathy. To normalize brain function, the child is prescribed special medications.
At the second stage of therapy, procedures are used that consolidate the results of medications (physiotherapy, physical therapy, therapeutic massage, etc.). If there are complications, a small patient may need surgery.
Treatment of residual encephalopathy uses the following drugs:
- vitamin complexes appropriate for the child’s age;
- anticonvulsants;
- medications to improve cerebral circulation;
- non-steroidal anti-inflammatory drugs;
- hormonal drugs;
- means to accelerate the regeneration of brain tissue.
Favorable prognosis for residual encephalopathy is possible only with timely diagnosis of the pathology and its full treatment. An important role is played by the general health of the child and the reasons that provoked the disease.
Residual encephalopathy is not included in the list of diseases exempt from military service, but a ban on conscription may be due to complications of the disease.
For example, if a diagnosis of “dyscirculatory encephalopathy” is established, then exclusion from the ranks of conscripts automatically occurs.
Prevention
Preventive measures to prevent residual encephalopathy include basic rules of child care and careful attention to the state of his health, starting from the stage of intrauterine development.
Recommendations for the prevention of residual encephalopathy in children:
- Regular examinations of women during pregnancy (scheduled and unscheduled if alarming symptoms occur).
- Timely and complete treatment of diseases of any etiology in a child (especially viral and infectious diseases).
- Prevention of traumatic brain injuries in a child (including birth injuries).
- Prevention of stressful situations and any negative impact on the child’s psyche.
- From an early age, a child should eat right, spend enough time in the fresh air, and play sports.
- Maintaining sleep and wakefulness (excluding the child’s regular lack of sleep, excessive physical activity, etc.).
- The baby’s immune system must be strengthened from an early age (if necessary, the supply of vitamins in the body must be replenished with special preparations).
https://www.youtube.com/watch?v=https:accounts.google.comServiceLogin
Residual encephalopathy is one of the dangerous and intractable diseases. Favorable prognosis is possible only with early diagnosis of the pathology and timely treatment. Otherwise, it will be impossible to eliminate developing pathological processes.

We kindly ask you not to self-medicate. Make an appointment with a doctor!
Complications, prevention
In order to prevent relapses of residual encephalopathy, the patient must follow preventive measures:
- Conduct an annual examination.
- Treat concomitant diseases in a timely manner.
- Lead a healthy lifestyle.
- Eliminate or reduce the likelihood of stressful situations.
To prevent congenital encephalopathy, doctors talk with pregnant women about the dangers of alcoholism, smoking, and antisocial behavior during this period. An important role is played by timely registration, screening and examinations, observation by a gynecologist until birth, and proper care of the baby in the first weeks and months of life.
To avoid residual organic damage to the central nervous system, it is necessary to be observed by a doctor during pregnancy. If there are any deviations, you should seek medical help. You should also refrain from taking medications and bad habits.
In the absence of proper treatment, the patient will inevitably develop complications. This can only be avoided by working with an experienced doctor and taking preventive measures that are effective both in improving the patient’s condition and in preventing the onset of the disease.
Many people face the unpleasant consequences of the disease. Only a serious approach to treatment and the help of an experienced doctor help reduce the risk of complications. And with severe residual encephalopathy, it is extremely difficult to avoid the consequences of the disease, and the treatment itself in such cases can last for years.
What complications may the patient experience:
- Episyndrome and epileptic seizures;
- Brain dysfunction;
- Cerebral paralysis;
- Vegetovascular dystonia;
- Hydrocephalus;
- Autism (Asperger's syndrome);
- Cerebrasthenic syndrome;
- Retardation in intellectual development;
- Brain gliosis;
- Psychospeech deviations.
Young children or teenagers may suffer the most from complications. For adults, the consequences are less dangerous. In special cases, the patient may even fall into a coma.
Prevention
You can protect yourself from the onset of the disease or its complications with simple preventive measures. Because they are applicable for healthy people and those who have already developed residual organic encephalopathy; some recommendations will be relevant only for the first category. Regular adherence to the rules and advice will eliminate all risks associated with this disease.
Preventive measures include recommendations:
- Visit your doctor at the first sign of health problems.
- Follow all directions and treat illnesses as soon as possible.
- Spend time outdoors regularly.
- Be more physically active and play sports
- Make the right diet with plenty of vitamins and minerals.
- Do special gymnastics that activates blood circulation in the brain.
- Avoid dangerous places and head injuries.
- Monitor the health of the fetus during pregnancy.
- To refuse from bad habits.
- Normalize the quality of sleep, eliminate stress from life.
This is enough to protect the body from many diseases. Every person should include such prevention in their life.
Residual encephalopathy: classification, symptoms and treatment methods
Residual encephalopathy of the brain in a child or adult is a process that occurs in the membranes and in the brain itself and leads to the irreversible death of cells of the central nervous system.
Pathology in ICD-10
The International Classification of Diseases, Tenth Revision (ICD-10) treats residual encephalopathy controversially. Pathology is considered under the code G93.4. He equates it to encephalopathy of unspecified pathogenesis. But the presence of additional factors forces us to assign other codes to the disease.
- G93.8 – destruction of CNS cells caused by exposure to radiation;
- T90.5, T90.8 – cell death due to injury.
Classification of the disease
By its nature, residual encephalopathy is divided into acquired and congenital. In the latter case, the provoking factors are disturbances during pregnancy or the birth process.
When a residual phenomenon arose due to organic brain damage and manifestations were noticed only many years later, the pathology is called residual organic encephalopathy (acquired).
There is also encephalopathy:
- diabetic (caused by diabetes mellitus);
- anaxic (caused by hypoxia);
- bilirubin (due to an excess of secreted bilirubin);
- radiation (caused by ionizing radiation);
- metabolic (caused by pathologies of other organs).
Reasons for appearance
Ischemic-hypoxic disorders can lead to residual encephalopathy in children. PPCNS (perinatal pathologies of the central nervous system) can develop from the seventh month of pregnancy to the seventh day after birth. This:
- infection of the embryo with infections;
- intrauterine oxygen starvation (fetal hypoxia);
- birth injuries or other abnormalities.
The lifestyle of the woman carrying the child, age, and heredity also influence.
The development of residual changes in the brain in adulthood can result from:
- head injuries, particularly repetitive ones;
- abuse of alcohol, psychotropic and narcotic substances;
- radiation exposure;
- critical increase in blood pressure, micro-strokes, micro-infarctions;
- defects in the development of nerve roots in the head area;
- the presence of cholesterol plaques in the arteries of the brain;
- intracerebral hemorrhage, heart attacks;
- disruption of the endocrine system (presence of diabetes);
- atherosclerosis;
- inflammatory processes that affect the head area;
- surgical intervention;
- poisoning with poisons or insecticides.
It is often quite difficult to establish the cause of the pathology, since its symptoms appear several years later, and several factors can simultaneously influence a person at this time.
Symptoms
Manifestations of pathology in childhood differ slightly from those presented, but usually there are delays in psychomotor development and disturbances in the emotional sphere, and they can be noticed immediately after childbirth.
Infants born with this diagnosis have a late or weak cry immediately after birth, absence or weakness of the sucking reflex, bulging eyes, muscle hypertonicity, convulsive twitching (after three months), constant restlessness, and poor sleep.
The subsequent consequences of congenital encephalopathy may include:
- attacks of uncontrollable aggression, causeless irritability;
- nausea, vomiting, fainting, migraines;
- poor performance at school due to memory problems and decreased attention;
- various disorders of the autonomic system (deterioration of sleep, rapid heartbeat, excessive sweating, etc.).
In adulthood, the manifestations of pathology are somewhat different. When residual encephalopathy was caused by inflammatory processes and injuries, increased ICP occurs quite often.
It is characterized by intense headache (especially in the morning), vomiting, nausea, blurred vision (double vision, blurred vision or “spots” before the eyes), a feeling of throbbing or pressing pain in the eye area.
General weakness, a constant feeling of fatigue, causeless irritability, and nervousness also occur. Many patients report dizziness, rapid heartbeat, and problems with balance while walking.
Doctors divided the symptoms of the disease into separate neurological syndromes:
- Cephalgic, which is characterized by severe migraines.
- Vestibular-coordinative, in which problems arise with motor skills, coordination, and feelings of dizziness appear.
- Astheno-neurotic, the main manifestations of which are fatigue, weakness, depressive states, emotional lability, hypochondria.
- Intellectual-mnestic disorders, which include memory problems, decreased attention and intelligence.
Methods of therapy
Treatment for residual encephalopathy is aimed at eliminating the symptoms of the pathology, improving the patient’s standard of living, and restoring normal functions. For migraines, anti-migraine medications such as Amigrenin and Sumatriptan are prescribed. To get rid of insomnia and stabilize the psycho-emotional state, adaptogens and antidepressants are indicated.
To improve brain activity, neurometabolic stimulants and drugs that increase the metabolism of carbohydrates in brain tissue (Glycine, Mildronate, Phezam, etc.) are prescribed. Diuretics for increased ICP, and for dizziness - Betaserc or its analogues. Hormonal, anticonvulsant drugs, and vitamin complexes may also be prescribed.
Clinical picture of hepatic encephalopathy, methods of treatment and prevention
To increase muscle tone, improve blood circulation, and restore coordination of movements, doctors prescribe physical therapy and massages. You will also need additional consultation with a psychotherapist and physiotherapeutic procedures. Osteopathy and herbal medicine are prescribed as additional treatment.
In especially severe cases, surgery is used. The main indication is the development of tumors in the brain.
Traditional medicine
During therapy, traditional methods are also used. Herbal balm is considered especially effective. It helps get rid of dizziness, cleanse brain vessels, and improve blood circulation.
To prepare such a remedy, you will need three different tinctures: red clover flowers, propolis, and Caucasian dioskerea rhizomes.
Equal parts of the resulting tinctures are mixed. Take the prepared balm three times a day after meals, 5 ml, after diluting with 50 grams of water. The course of such treatment is 60 days. After which a 14-day break is taken.
You should not self-medicate or take medications without first consulting a specialist. Any mistake, even the smallest one, can damage your health even more and lead to serious consequences, including disability.
Prevention
Prevention of pathology involves identifying and eliminating factors that can provoke it. It is worth starting preventive measures during pregnancy and in preparation for it. This will prevent the development of congenital encephalopathy and other serious pathologies. Disease prevention is:
- regular examinations, tests, fulfillment of all doctor’s prescriptions during pregnancy;
- timely, complete treatment of viral and infectious diseases;
- preventing head injuries;
- prevention of stress and other negative effects on the psyche;
- strengthening the immune system.
Don’t forget about an active, healthy lifestyle, exercise, and proper nutrition.
With timely diagnosis, the prognosis for patients is often positive. Every fourth person experiences complete relief from the symptoms of the pathology.
Conclusion
To summarize, we can say that residual encephalopathy is a residual phenomenon that occurs as a result of previous disorders.
There is always a threat that the disease will relapse.
If you do not pay attention to the manifestations in time and start the course of the disease, epilepsy, mental retardation, dementia, cerebral palsy, Parkinson’s disease and other dangerous conditions may develop.
Source: //neuromed.online/rezidualnaya-entsefalopatiya/