A cyst in the brain is a pathological process that is considered quite dangerous. If a diagnosis is made, the patient undertakes to follow all the doctor’s instructions. This will avoid the negative consequences of the disease. If there is a deterioration in the condition, the doctor makes a decision on surgical treatment.
Description
A brain cyst is a large intracranial formation, which is a fluid-filled cavity. Often has a hidden subclinical course without increasing in size. It manifests itself mainly as symptoms of intracranial hypertension and epileptic paroxysms. Focal symptoms are possible, corresponding to the location of the cyst. It is diagnosed based on the results of MRI and CT scan of the brain, in infants - according to neurosonography. Treatment is carried out with progressive growth of the cyst and the development of complications, consisting of surgical removal or aspiration of the cyst.
In children
In children, this neoplasm is diagnosed based on symptomatic manifestations and the child’s medical history.
The specialist will find out whether the child has had injuries or operations in the brain, whether he or she also suffered from meningitis, or whether there have been hemorrhages.
After this, a neurological examination is performed, and a CT or MRI is also prescribed.
It must be said that this pathology is dangerous for the child. It consists in provoking persistent neurological disorders and epileptic seizures.
Under no circumstances should parents independently treat their child, much less let the disease take its course. The baby urgently needs to be shown to a doctor who will prescribe the correct treatment regimen. If the clinical picture is pronounced, surgical intervention may be required.
Clinical picture in a newborn baby:
- strong pulsation in the fontanel region;
- limbs are flaccid;
- unoriented look.
One of the clearest signs of a cyst in a newborn is severe regurgitation during or after feeding.
Useful video on the topic:
Additional facts
A brain cyst is a local accumulation of fluid in the membranes or substance of the brain. A small cyst, as a rule, has a subclinical course and is detected accidentally during a neuroimaging examination of the brain. A large volume cyst due to the limited intracranial (intracranial) space leads to intracranial hypertension and compression of the surrounding brain structures. The clinically significant size of cysts varies significantly depending on their location and compensatory capabilities. Thus, in young children, due to the flexibility of the skull bones, a long latent course of cysts is often observed without signs of severe liquor hypertension. A brain cyst can be detected at different age periods: from newborns to old age. It should be noted that congenital cysts more often appear in middle age (usually 30-50 years) than in childhood. According to generally accepted practice in clinical neurology, watchful and expectant management tactics are used for frozen or slowly progressing small-volume cysts.
Brain cyst
Classification
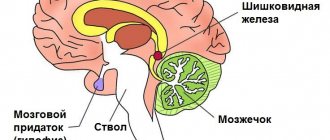
Depending on the location, arachnoid and intracerebral (cerebral) cysts are distinguished. The first is localized in the meninges and is formed due to the accumulation of cerebrospinal fluid in places of their congenital duplication or adhesions formed as a result of various inflammatory processes. The second is located in the internal structures of the brain and is formed in the area of brain tissue that has died as a result of various pathological processes. Separately, there are also pineal gland cysts, choroid plexus cysts, colloid and dermoid cysts. All brain cysts according to their genesis are classified into congenital and acquired. Exclusively congenital cysts include dermoid and colloid cysts of the brain. In accordance with the etiology, acquired cysts are divided into post-traumatic, post-infectious, echinococcal, and post-stroke.
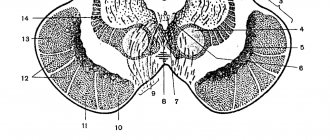
Retrocerebellar type formation
This is a fairly rare pathology, which is diagnosed in 5% of the population.
This neoplasm combines several types of neoplasms that differ in location:
- arachnoid,
- intracerebral - can form in any part,
- inferior retrocerebellar.
This cyst is spoken of when the tumor is localized only in the cerebellum. In this case we observe:
- migraine;
- vomit;
- paralysis and paresis;
- problems with balance;
- the image before your eyes becomes unclear;
- decreased concentration;
- deterioration of character;
- loss of consciousness;
- twitching of the eyeballs;
- deterioration of thinking;
- violation of orientation in space and time;
- decreased muscle tone.
Causes
Factors that provoke the formation of a congenital brain cyst are any adverse effects on the fetus in the antenatal period. These include fetoplacental insufficiency, intrauterine infections, pregnant women taking medications with a teratogenic effect, Rh conflict, fetal hypoxia. Congenital cysts and other anomalies of brain development can occur if the development of the fetus occurs under conditions of intrauterine intoxication due to drug addiction, alcoholism, nicotine addiction of the expectant mother, as well as if she has chronic decompensated diseases. An acquired cyst is formed as a result of traumatic brain injury, birth trauma of a newborn, inflammatory diseases (meningitis, arachnoiditis, brain abscess, encephalitis), acute cerebrovascular accidents (ischemic and hemorrhagic stroke, subarachnoid hemorrhage). It may have a parasitic etiology, for example, with echinococcosis, cerebral form of taeniasis, paragonimiasis. A cyst of iatrogenic origin can form as a complication of brain surgery. In some cases, various dystrophic and degenerative processes in the brain are also accompanied by the replacement of cerebral tissue with a cyst. A separate group consists of factors that can provoke an increase in the size of an existing intracranial cystic formation. Similar triggers can be head injuries, neuroinfections, inflammatory intracranial processes, vascular disorders (stroke, obstruction of venous outflow from the cranial cavity), hydrocephalus.
Development options
Most often, the cyst does not interfere with brain activity. In case of an increase in the volume of the tumor and the appearance of neurological abnormalities, the options for the development of the cyst will depend on the timeliness of diagnosis and correct treatment.
When pressure increases in the head, serious problems with speech, hearing, vision and memory can occur. Persistent neurological disorders may occur. A sharp increase in the size of the tumor can provoke its rupture and death of the patient. If diagnosis and therapy are carried out on time, the prognosis is quite optimistic and after treatment the patient recovers 100%.
Source
Symptoms
The most typical manifestation of a cerebral cyst is with symptoms of intracranial hypertension. Patients complain of almost constant cephalalgia, a feeling of nausea not associated with food, a feeling of pressure on the eyeballs, and decreased performance. There may be sleep disturbances, noise or a sensation of pulsation in the head, visual disturbances (decrease in visual acuity, double vision, narrowing of visual fields, the appearance of photopsia or visual hallucinations), mild hearing loss, ataxia (dizziness, unsteadiness, incoordination of movements), small-scale tremor, fainting. With high intracranial hypertension, repeated vomiting is observed. In some cases, a brain cyst debuts with a first-time epileptic paroxysm, followed by repeated epileptic attacks. Paroxysms can be of a primary generalized nature, in the form of absence seizures or focal Jacksonian epilepsy. Focal symptoms are observed much less frequently than general cerebral manifestations. In accordance with the localization of the cystic formation, it includes hemi- and monoparesis, sensory disorders, cerebellar ataxia, brainstem symptoms (oculomotor disorders, swallowing disorders, dysarthria, etc.). Complications of the cyst may include its rupture, occlusive hydrocephalus, compression of the brain, rupture of a vessel with hemorrhage into the cyst, and the formation of a persistent epileptogenic focus. In children, cysts accompanied by severe intracranial hypertension or episyndrome can cause mental retardation with the formation of oligophrenia. Colloid cyst accounts for about 15.20% of intraventricular formations. In most cases, it is located in the anterior region of the third ventricle, above the foramen of Monroe; in some cases - in the IV ventricle and in the area of the transparent septum. The filling of a colloid cyst is highly viscous. The basis of the clinical manifestations are the symptoms of hydrocephalus with a paroxysmal increase in cephalgia in certain positions of the head. Behavioral disorders and memory loss are possible. Cases of weakness in the limbs have been described. A choroid plexus cyst is formed when cerebrospinal fluid fills the space between the individual plexus vessels. Diagnosed at different ages. Clinically manifested rarely, in some cases it can give symptoms of intracranial hypertension or epilepsy. Often, choroid plexus cysts are detected by obstetric ultrasound at the 20th week of pregnancy, then they resolve on their own and by approximately the 28th week of intrauterine development they are no longer detected on ultrasound.
Characteristics by location
The cyst in question may be located:
- in the temporal lobes;
- in the parietal part;
- in the frontal region;
- in the region of the cerebellum;
- in the spinal canal;
- in the spinal column;
- in the lumbar region.
In the posterior cranial fossa
This cyst in the posterior cranial fossa (posterior cranial fossa) is accompanied by symptoms:
- persistent headaches;
- vomit;
- failure to coordinate movements;
- intermittent paralysis of body parts;
- convulsive syndrome;
- mental disorders;
- hallucinations.
Diagnostics
Clinical symptoms and neurological status data allow the neurologist to suspect the presence of an intracranial space-occupying lesion. To check hearing and vision, the patient is referred to a consultation with an otolaryngologist and ophthalmologist; Audiometry, viziometry, perimetry and ophthalmoscopy are performed, in which congestive optic discs are noted in cases of severe hydrocephalus. Increased intracranial pressure can be diagnosed using echo-encephalography. The presence of epileptic paroxysms is an indication for electroencephalography. However, relying only on clinical data, it is impossible to verify a cyst from a hematoma, abscess or brain tumor. Therefore, if a brain mass is suspected, it is necessary to use neuroimaging diagnostic methods. The use of ultrasound makes it possible to identify some congenital cysts during the period of intrauterine development; after the birth of a child and before the closure of its large fontanel, diagnosis is possible using neurosonography. In the future, the cyst can be visualized using CT or MRI of the brain. To differentiate a cystic formation from a brain tumor, these studies are carried out with contrast, since, unlike a tumor, a cyst does not accumulate a contrast agent. For better visualization of the cystic cavity, it is possible to introduce contrast into it by puncture of the cyst. Unlike MRI, CT of the brain makes it possible to judge the viscosity of the cyst contents by the density of its image, which is taken into account when planning surgical treatment. Of fundamental importance is not only establishing a diagnosis, but also continuous monitoring of the cystic formation to assess changes in its volume over time. In case of post-stroke genesis of cysts, additional vascular examinations are used: duplex scanning, Doppler ultrasound, CT or MRI of cerebral vessels.
Treatment
Conservative therapy is ineffective. Treatment is only possible through surgery. However, most cysts do not require active treatment because they are small and do not progress in size. They are subject to regular follow-up with MRI or CT monitoring. Cysts that are clinically manifested by symptoms of hydrocephalus, progressively increasing in size, complicated by rupture, bleeding, and compression of the brain are subject to neurosurgical treatment. The choice of surgical method and surgical approach is made during a consultation with a neurosurgeon. In cases of a severe condition of a patient with a disorder of consciousness (stupor, coma), external ventricular drainage is urgently indicated to reduce intracranial pressure and compression of the brain. If complications develop in the form of cyst rupture or hemorrhage, as well as with a parasitic etiology of the cyst, surgical intervention is performed with the aim of radical excision of the cystic formation; The surgical approach is craniotomy. In other cases, the operation is planned and is carried out primarily endoscopically. The advantage of the latter is low trauma and a short recovery period. To carry it out, you only need a burr hole in the skull, through which the contents of the cyst are aspirated. In order to prevent re-accumulation of fluid in the cystic cavity, a series of holes are made, connecting it with the cerebrospinal fluid spaces of the brain, or cystoperitoneal shunting is performed. The latter involves the implantation of a special shunt through which fluid from the cyst enters the abdominal cavity. In the postoperative period, comprehensive rehabilitation therapy is carried out, in which, if necessary, a neuropsychologist, exercise therapy doctor, massage therapist, and reflexologist take part. The medicinal component includes absorbable agents, drugs that improve blood circulation and brain metabolism, decongestants and symptomatic medications. In parallel, in order to restore muscle strength and sensory function, and adapt the patient to physical activity, physiotherapy, exercise therapy, massage, and reflexology are carried out.
Additional facts
A brain cyst is a local accumulation of fluid in the membranes or substance of the brain. A small cyst, as a rule, has a subclinical course and is detected accidentally during a neuroimaging examination of the brain. A large volume cyst due to the limited intracranial (intracranial) space leads to intracranial hypertension and compression of the surrounding brain structures.
from newborns to old age. It should be noted that congenital cysts more often appear in middle age (usually 30-50 years) than in childhood. According to generally accepted practice in clinical neurology, watchful and expectant management tactics are used for frozen or slowly progressing small-volume cysts.
Dimensions and norm
Patients are often interested in the question of the normal size of the cyst and the volume at which surgical intervention is necessary.
It must be said that we can speak of normality only in the absence of a cystic neoplasm; if there is a cyst, then this is already an anomaly, and its size essentially does not matter much.
This type can have different sizes, but the cyst still cannot grow very much. Brain fluid resists its growth. If the size of the cyst is 1-2 mm, it is considered small; if the neoplasm grows to 1 cm, it is considered medium; cysts larger than 1 cm are considered large.
When diagnosing small cysts, doctors, as a rule, do not prescribe treatment, but choose a wait-and-see approach and simply monitor changes in the volume of the tumor. Large cysts are treated surgically; surgery is also indicated for medium-sized tumors when symptoms appear.
Classification
Depending on the location, arachnoid and intracerebral (cerebral) cysts are distinguished. The first is localized in the meninges and is formed due to the accumulation of cerebrospinal fluid in places of their congenital duplication or adhesions formed as a result of various inflammatory processes.
The second is located in the internal structures of the brain and is formed in the area of brain tissue that has died as a result of various pathological processes. Separately, there are also pineal gland cysts, choroid plexus cysts, colloid and dermoid cysts. All brain cysts according to their genesis are classified into congenital and acquired.
Causes
Factors that provoke the formation of a congenital brain cyst are any adverse effects on the fetus in the antenatal period. These include fetoplacental insufficiency, intrauterine infections, pregnant women taking medications with a teratogenic effect, Rh conflict, and fetal hypoxia.
Congenital cysts and other abnormalities of brain development can occur if the fetus develops under conditions of intrauterine intoxication due to drug addiction, alcoholism, nicotine addiction of the expectant mother, as well as if she has chronic decompensated diseases. An acquired cyst is formed as a result of traumatic brain injury, birth trauma of a newborn, inflammatory diseases (meningitis, arachnoiditis, brain abscess, encephalitis), acute cerebrovascular accidents (ischemic and hemorrhagic stroke, subarachnoid hemorrhage).
It may have a parasitic etiology, for example, with echinococcosis, cerebral form of taeniasis, paragonimiasis. A cyst of iatrogenic origin can form as a complication of brain surgery. In some cases, various dystrophic and degenerative processes in the brain are also accompanied by the replacement of cerebral tissue with a cyst.
A separate group consists of factors that can provoke an increase in the size of an existing intracranial cystic formation. Similar triggers can be head injuries, neuroinfections, inflammatory intracranial processes, vascular disorders (stroke, obstruction of venous outflow from the cranial cavity), hydrocephalus.
Consequences
Unfortunately, the consequences of cerebral edema can sometimes be extremely sad (even fatal), and it is sometimes simply impossible to make an accurate forecast of what kind of traces the disorder will leave in the body. The occurrence of this disorder can begin irreversible processes in the body, as well as damage too significant amounts of tissue and brain cells.
Without a doubt, cerebral edema is an unpredictable disease, the results of which are extremely difficult to predict. In order for the consequences of the illness to be minimal, it is necessary to immediately consult a doctor after detecting the first signs of the disease. Of course, recovery from an illness takes a long time, but if it is followed correctly, all consequences can be minimized.
Symptoms
The most typical manifestation of a cerebral cyst is with symptoms of intracranial hypertension. Patients complain of almost constant cephalalgia, a feeling of nausea not associated with food, a feeling of pressure on the eyeballs, and decreased performance. There may be sleep disturbances, noise or a sensation of pulsation in the head, visual disturbances (decrease in visual acuity, double vision, narrowing of visual fields, the appearance of photopsia or visual hallucinations), mild hearing loss, ataxia (dizziness, unsteadiness, incoordination of movements), small-scale tremor, fainting.
With high intracranial hypertension, repeated vomiting is observed. In some cases, a brain cyst debuts with a first-time epileptic paroxysm, followed by repeated epileptic attacks. Paroxysms can be of a primary generalized nature, in the form of absence seizures or focal Jacksonian epilepsy.
Focal symptoms are observed much less frequently than general cerebral manifestations. In accordance with the localization of the cystic formation, it includes hemi- and monoparesis, sensory disorders, cerebellar ataxia, brainstem symptoms (oculomotor disorders, swallowing disorders, dysarthria, etc.). Complications of the cyst may include its rupture, occlusive hydrocephalus, compression of the brain, rupture of a vessel with hemorrhage into the cyst, and the formation of a persistent epileptogenic focus.
In children, cysts accompanied by severe intracranial hypertension or episyndrome can cause mental retardation with the formation of oligophrenia. Colloid cyst accounts for about 15.20% of intraventricular formations. In most cases, it is located in the anterior region of the third ventricle, above the foramen of Monroe;
in some cases - in the IV ventricle and in the area of the transparent septum. The filling of a colloid cyst is highly viscous. The basis of the clinical manifestations are the symptoms of hydrocephalus with a paroxysmal increase in cephalgia in certain positions of the head. Behavioral disorders and memory loss are possible.
Cases of weakness in the limbs have been described. A choroid plexus cyst is formed when cerebrospinal fluid fills the space between the individual plexus vessels. Diagnosed at different ages. Clinically manifested rarely, in some cases it can give symptoms of intracranial hypertension or epilepsy.
Symptomatic manifestations
This cystic neoplasm is characterized by an asymptomatic course .
Most often, such neoplasms are detected during a patient examination for neurological pathologies with similar symptoms.
The clinical signs of the cyst are nonspecific; their severity depends on the size of the tumor and its location. Patients may complain of general cerebral symptoms, which are associated with compression of brain areas. A focal clinical picture is observed in rare cases, and is most often caused by the presence of hygroma or rupture of the cystic cavity.
The main features are:
- dizziness , which are not associated with pregnancy, taking certain medications, severe fatigue, iron deficiency, and so on;
- vomiting , which is also not associated with gastrointestinal poisoning, taking medications, and so on;
- mental disorders, hallucinations ;
- convulsive syndrome;
- loss of consciousness;
- hemiparesis , decreased sensitivity in the limbs;
- failure to coordinate the activity of the body muscles;
- headaches that are not relieved by painkillers;
- a feeling of fullness , pressure, compression and increased pulsation in the affected area;
- visual and hearing problems;
- extraneous sounds in the ears;
- heaviness in the skull;
- painful or uncomfortable sensations when turning the head.
Reference! Secondary arachnoid cystic neoplasms may be accompanied by symptoms of injury or primary disease, which served as an impetus for the development of the disease.
Diagnostics
Clinical symptoms and neurological status data allow the neurologist to suspect the presence of an intracranial space-occupying lesion. To check hearing and vision, the patient is referred to a consultation with an otolaryngologist and ophthalmologist; Audiometry, viziometry, perimetry and ophthalmoscopy are performed, in which congestive optic discs are noted in cases of severe hydrocephalus.
Increased intracranial pressure can be diagnosed using echo-encephalography. The presence of epileptic paroxysms is an indication for electroencephalography. However, relying only on clinical data, it is impossible to verify a cyst from a hematoma, abscess or brain tumor.
Therefore, if a brain mass is suspected, it is necessary to use neuroimaging diagnostic methods. The use of ultrasound makes it possible to identify some congenital cysts during the period of intrauterine development; after the birth of a child and before the closure of its large fontanel, diagnosis is possible using neurosonography.
In the future, the cyst can be visualized using CT or MRI of the brain. To differentiate a cystic formation from a brain tumor, these studies are carried out with contrast, since, unlike a tumor, a cyst does not accumulate a contrast agent. For better visualization of the cystic cavity, it is possible to introduce contrast into it by puncture of the cyst.
Unlike MRI, CT of the brain makes it possible to judge the viscosity of the cyst contents by the density of its image, which is taken into account when planning surgical treatment. Of fundamental importance is not only establishing a diagnosis, but also continuous monitoring of the cystic formation to assess changes in its volume over time.
Brain tumor: stages
The stages of cancer are usually distinguished by clinical signs and there are only 4 of them. At the first stage, the most common symptoms appear, for example, headaches, weakness and dizziness. Since these symptoms cannot directly indicate the presence of cancer, even doctors cannot detect cancer at an early stage. However, there is still a small chance of detection; cases of cancer being detected during computer diagnostics are not uncommon.
Tumor of the temporal lobe of the brain
In the second stage, the symptoms are more pronounced, in addition, patients experience impaired vision and coordination of movements. The most effective way to detect a brain tumor is an MRI. At this stage, in 75% of cases, a positive outcome is possible as a result of surgery.
The third stage is characterized by impaired vision, hearing and motor function, increased body temperature, and rapid fatigue. At this stage, the disease penetrates deeper and begins to destroy lymph nodes and tissues, and then spreads to other organs.
The fourth stage of brain cancer is glioblastoma, which is the most aggressive and dangerous form of the disease, it is diagnosed in 50% of cases. Glioblastoma of the brain has an ICD 10 code —
C71.9 is characterized as a multiforme disease. This brain tumor belongs to the astrocytic subgroup. It usually develops as a result of the transformation of a benign tumor into a malignant one.