Subarachnoid hemorrhage (SAH) is a pathology that is accompanied by the accumulation of blood in the space between the two membranes of the brain: the arachnoid and the pia mater. This pathology is a type of stroke and is observed in 1-10% of cases of acute cerebrovascular accidents.
Blood entering the subarachnoid cavity is accompanied by characteristic neurological symptoms and often leads to death.
Causes
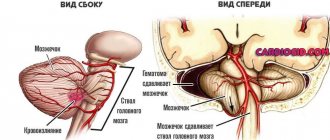
Hemorrhage into the subarachnoid space is a separate subtype of hemorrhagic stroke. The pathogenesis of the disorder consists in an increase in the volume of fluid in the subarachnoid space due to blood flowing from the ruptured vessel. This leads to severe irritation of the pia mater. In response to blood loss, vasospasm occurs, which provokes ischemia of other parts of the brain and can cause a transient ischemic attack or ischemic stroke.
The causes of subarachnoid cerebral hemorrhage are the following:
- Cerebral aneurysms. The presence of an aneurysm (protrusion of the wall) of large cerebral vessels is the etiological factor of SAH in 70-85% of cases. The most common cause of hemorrhage is rupture of a saccular aneurysm. Strokes of aneurysmal origin have a less favorable prognosis than spontaneous nonaneurysmal bleeding.
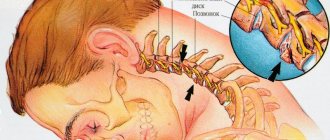
- Dissection of large arteries (vertebral, carotid). In most cases, blood enters the space between the membranes of the brain due to dissection of the wall of the vertebral artery in the cervical region. A more rare etiological factor is dissection of the internal carotid artery. The most common causes of vessel dissection are considered to be severe displacement of the cervical vertebrae, whiplash injury, osteopathic and surgical manipulations.
- Traumatic brain injury. Skull fractures, open head injuries, contusions and compression of the brain cause damage to large cerebral vessels, which leads to blood spilling between the membranes of the brain. A subtype of this factor is birth trauma of the newborn, which can occur with a narrow pelvis of the woman in labor, developmental anomalies and large size of the fetus, as well as pregnancy pathologies (intrauterine infections, postmaturity, rapid and early labor). Less than 15% of clinical cases of SAH have a traumatic etiology.
- Other causes (occur in less than 5% of cases). These include cerebral and spinal neoplasms, secondary foci of malignant tumors (for example, cardiac myxomas), vasculitis, angiopathy of amyloid origin, disorders of blood composition and hemodynamics (coagulopathy, sickle cell anemia), pituitary hemorrhage, rupture of the circumferential artery in the brain stem, etc.
Important information: Where to place leeches after a stroke (hirudotherapy)
In approximately 10% of patients, hemorrhage into the subarachnoid space has an unclear etiology. This pathology, which is called non-aneurysmal perimesencephalic hemorrhage, is characterized by the absence of an exact source of bleeding, mild stroke symptoms and a favorable prognosis. It is assumed that such hemorrhages can be caused by rupture of the walls of small vessels, which makes it possible to close the rupture site using the body's resources.
In rare cases, hemorrhage may occur due to vascular pathologies (arteriovenous malformations and fistulas). With this etiology of the disease, predominantly mixed (subarachnoid and parenchymal) hemorrhage is observed.
Concomitant diseases of the main cause of hemorrhage (saccular aneurysm) are the following pathologies:
- genetic disorders that lead to disruption of the formation of connective tissue, skin and blood vessels (Ehlers-Danlos, Grönblad-Strandberg and Marfan syndromes, alpha-antitrypsin deficiency, etc.);
- hereditary predisposition;
- developmental anomalies of the arteries of the circle of Willis;
- neurofibromatosis;
- renal polycystic disease;
- dilatation of small vessels (telangiectasia);
- arterial-venous malformations;
- coarctation of the aorta;
- Moyamoya disease.
Risk factors for developing SAH are:
- arterial hypertension;
- alcohol abuse;
- taking drugs (most often cocaine and other stimulants);
- atherosclerosis and high concentration of low-density lipoproteins in the blood;
- obesity;
- smoking;
- hormone replacement therapy and COC use;
- pregnancy and childbirth.
What can cause it?
Subarachnoid hemorrhage is a type of hemorrhagic stroke in which blood is released into the subarachnodal space of the brain (the area between its cavities that is filled with cerebrospinal fluid).
The release can occur as a result of the development of vascular pathologies, head injuries, and blood clotting disorders. In this case, the patient experiences a severe headache. The frequent absence of other symptoms can make diagnosis difficult.
This condition also occurs as a result of damage to the brain parenchyma. In this case, specific neurological signs will be observed: disruption of the facial muscles (hemiparesis).
| Traumatic | Spontaneous (non-traumatic) |
| Severe injury (TBI)/closed injury (CTBI). Brain contusion. | The most common reasons:
More rare causes:
|
The pathogenesis of hemorrhage can be described as the collection of fluid in the subarachnoid cavity - the space between the pia mater and the arachnoid membrane. This cavity contains cerebrospinal fluid, which rises from the spinal cord, wraps around both hemispheres of the brain and descends back.
When bleeding begins, blood flows to the basal cisterns (located at the base of the brain). And it begins to enter the cerebrospinal fluid, which leads to spasms of the arteries, death of neurons and swelling of the brain. The amount of cerebrospinal fluid increases due to the blood, which leads to an increase in pressure in the brain cavity and can contribute to its displacement.
Symptoms
Symptoms of subarachnoid hemorrhage include the following:
- severe headache (most often due to severe stress or tension);
- pain in the neck (only with dissection of the vertebral artery in the cervical region);
- depression or loss of consciousness (depending on the volume of blood in the subarachnoid space and the location of the lesion, this symptom can vary from mild stupor to a rapid fall into a coma);
- meningeal syndrome (vomiting, neck tension, increased sensitivity, intolerance to sounds and light);
- epileptic seizures (in 10% of cases);
- psychomotor agitation, predominance of the tone of the sympathetic nervous system;
- ophthalmological disorders (decreased visual acuity, ophthalmoplegia, retinal hemorrhage, nystagmus, etc.);
- respiratory disorders (with aneurysms of the lower segment of the cerebral artery).
The nature, combination and severity of symptoms depend on the location of the source of bleeding. Signs that distinguish SAH from cerebral hemorrhage are the nature and time of development of the pain syndrome: when blood enters the subarachnoid space, neurological symptoms develop within a few minutes.
Important information: Symptoms and first signs of an ischemic microstroke suffered on the legs in elderly women (men)
In aneurysmal subarachnoid hemorrhage, symptoms of neurological pathology may be observed for several weeks before the weak section of the vessel ruptures. This phenomenon is typical for large aneurysms.
Every third patient with SAH has an atypical course of pathology: signs of hemorrhage may resemble the clinical picture of acute psychosis, inflammation of the meninges, hypertensive crisis, cervical radiculitis and migraine.
Classification
The disease subarachnoid hemorrhage has its own classification. It is determined using basic data obtained from CT or MRI. The calculations take into account the massiveness of the hemorrhage, combination with parenchymal, venticular hemorrhages in the cranial cavity. Based on the results of the diagnosis, it is determined what kind of subarachnoid bleeding it is: isolated, parenchymal, venticular or parenchymal-venticular hemorrhage.
Hunt Hess scale
There are three specific grading scales for assessing SAH in neurology. They show the patient’s condition, the amount of blood in the ventricles of the brain (ventricular hemorrhage), and the outcome of the hemorrhage. Each level reflects the severity of the condition, survival or focal neurological deficit.
- Level 1: There is a slight headache, slight stiffness in the neck. At this level, up to 70% of patients survive;
- Level 2: There is moderate to severe headache, moderate neck stiffness, and neurological deficits. Survival rate is 60% of patients;
- Level 3: Obtundation and minimal neurological deficits are present. At this level, up to 50% of patients survive;
- Level 4: there is severe depression of consciousness, incomplete paralysis, increased tone of all muscles and autonomic disorders. Survival rate is up to 20% of patients;
- Level 5: agony, increased tone of all muscles, deep coma. Only 10% of patients survive.
In neurology, three classifications of disease severity are used.
The Hunt-Hess scale, according to which the degree of severity is determined by the symptoms that appear:
- 1st: mild headache and increased tone of the neck muscles;
- 2nd: headache gets worse. At this stage, neurological symptoms begin to appear (eye pain, strabismus, paresis (partial impairment of motor function));
- 3rd: a slight neurological deficit appears, characterized by drowsiness and a decrease in reaction speed;
- 4th: serious neurological deficit - stunning, loss of reaction, partial paralysis of one side of the body, lack of response to external stimuli;
- 5th: deep coma, sharp increase in muscle tone.
The Fisher scale classifies the patient's condition according to the amount of hemorrhage that appears on the results of computed tomography or MRI:
- hemorrhage is not detected;
- lesion size 1 mm;
- lesion more than 1 mm;
- intraventricular hemorrhage or damage to the brain parenchyma (the magnitude does not matter).
The Glasgow Coma Scale (GCS) determines the severity of the disease by neurological deficit (the condition is assessed by points, where 15 is clear consciousness and 3 is deep coma):
- GCS 15—no neurological deficit;
- 13-14 GCS - moderate or deep stunning;
- 8-10 GCS - stupor (numbness, lethargy);
- 6-7 GCS - moderate coma;
- 4-5 GCS - thermal coma;
- GCS 3 - deep coma.
There is also a classification that combines some factors from the above methods of assessing the patient’s condition. The Ogilvy and Carter scale takes into account the age of the patient, the severity of the patient according to the Hunt-Hess and Fisher scales and the size of the aneurysm. Severity is assessed by the number of signs present and absent.
How is it diagnosed?
A neurologist can suspect the presence of SAH in a patient based on the characteristic clinical picture of the pathology. However, to make an accurate diagnosis, there is not enough information about what subarachnoid hemorrhage is and how it manifests depending on the location of the lesion. In addition to external signs, the doctor must have the results of laboratory and instrumental tests.
The most informative diagnostic methods include:
- CT scan. Brain CT is the most accurate examination method for suspected SAH. Tomography makes it possible to detect cerebral edema, bleeding into the ventricles and subarachnoid membrane, foci of ischemia, etc. On days 1-2 after a stroke, the sensitivity of the method is more than 95%, on days 2-3 - 80-85%, and 6 days after hemorrhage - less than 30%. For delayed diagnosis of SAH, magnetic resonance imaging of the brain is a more informative method.
- Transcranial ultrasound and duplex examination of cerebral vessels. Catheter diagnostics of cerebral vessels makes it possible to establish the source of bleeding, diagnose vasospasm and determine the need for urgent surgical intervention. If the source could not be detected during the first examination, a repeat vascular ultrasound is recommended 20-28 days after SAH.
- MRI angiography. If there are contraindications to intravascular examination of the cerebral arteries, non-invasive angiography is performed using computed tomography or magnetic resonance imaging. In case of severe pathology, the study is carried out after stabilization of the patient's condition.
- Puncture of cerebrospinal fluid (CSF). Characteristic signs of SAH are a reddish or xanthochromic color of the cerebrospinal fluid, a high concentration of red blood cells (more than 100,000 units/ml), increased levels of protein and white blood cells (neutrophils). A cerebrospinal fluid sample is necessary in cases where it is not possible to perform a CT scan or tomography does not show cerebral changes against the background of a characteristic neurological picture. If there is a high risk of brain dislocation (displacement), this manipulation is prohibited.
Important information: What is the danger of pneumonia after a stroke in bedridden patients and survival prognosis
Differential diagnosis
But everything may not be so dangerous and serious if you go to see a doctor in time and conduct a series of examinations, and then the cause will be eliminated in time.
The course of examinations includes lumbar function, when leached red blood cells are found in the blood, or computed tomography, performed in several modes. Then it will be possible to identify the aneurysm, its location, and vascular pathology.
Based on this information, the doctor will choose the most appropriate treatment method.
The most effective method is computed tomography (CT).
It is used to determine:
- site of hemorrhage;
- data on the liquor system;
- presence of cerebral edema.
| Diagnostic method | Detectable symptoms |
| Neurological examination | If a patient exhibits several symptoms, hemorrhage is often detected during examination. |
| Blood analysis | Detects abnormalities in coagulation; is prescribed as an additional diagnostic method. |
| Lumbar puncture | A puncture is made at the lumbar level to collect cerebrospinal fluid from the spinal cord. A puncture is performed if a computed tomography scan does not show changes in the brain or it is not possible to carry out it. |
| Echo-encephalography (ECHO-EG) | SAH increases pressure inside the skull. This can cause the brain to become misaligned. This is exactly what ECHO-CG reveals. |
| Magnetic resonance imaging (MRI) | A more accurate method that can replace CT. But due to less availability, it is used much less frequently. |
| Transcranial Dopplerography (TCDG) | Ultrasound diagnostics of the brain. With its help, you can identify narrowing of blood vessels and impaired blood flow. |
| Magnetic resonance angiography (MRA) | This method allows you to obtain an image of the blood vessels and arteries of the brain and determine their integrity. |
Treatment methods
Treatment of pathology is divided into first aid, conservative therapy, surgery and rehabilitation. All stages of therapy are aimed at normalizing brain function, correcting biochemical parameters and preventing complications of hemorrhage.
First aid
First aid and treatment of subarachnoid hemorrhage should be carried out in a medical hospital. If symptoms of SAH occur (severe headache, loss of consciousness, etc.) in a person nearby, you must immediately call an ambulance and monitor the victim until doctors arrive to prevent blockage of the airways.
The medical team provides the patient with emergency care to relieve epileptic seizures and other symptoms, and then transports him to the intensive care unit or neurological hospital.
Medicines
Treatment of subarachnoid hemorrhage involves the use of drugs such as:
- Nimodipine;
- epsilon-aminocaproic acid;
- antiplatelet agents;
- antiemetics (Cerucal);
- laxatives and diuretics (Mannitol, Furosemide);
- anticonvulsants (Diazepam, valproic acid);
- cerebral circulation correctors (Cavinton, Actovegin);
- sedatives (Droperidol), etc.
Conservative therapy is intended only to eliminate the consequences of hemorrhage: reducing cerebral edema, preventing vasospasm, ischemia and thrombosis of blood vessels, as well as relieving the symptoms of the pathology.
During treatment, bed rest is mandatory.
Operation
In the first 3 days after the development of SAH, surgical elimination of the pathology is possible. It is performed by clipping the neck of the aneurysm or filling the vessel using a balloon catheter (endovascular occlusion). Both methods are aimed at excluding the area with the aneurysm from the cerebral blood flow.
The purpose of the operation may also be to reduce brain swelling and prevent its dislocation. In these cases, ventricular drainage or craniotomy is performed.