Wallenberg-Zakharchenko syndrome is named after the scientists who almost simultaneously and independently described this brain lesion. It belongs to the group of alternating syndromes associated with impaired blood supply to the brain.
The cause of Wallenberg syndrome is stroke-like thrombosis of the posterior artery supplying blood to the cerebellum.
As a rule, loss of consciousness does not occur, but there is severe dizziness, lack of balance, there may be hiccups or vomiting and slight stupor.
The factor causing thrombosis is vascular atherosclerosis, as well as endarteritis of the spinal artery of the syphilitic type or the posterior inferior cerebellar line lagging behind it, or rheumovasculitis.
Damage of a thrombotic or non-thrombotic nature generally occurs slowly. The most common lesions are the areas of the vertebral and basilar arteries. In this case, the signs of the syndrome alternate with periods of improvement and deterioration, however, the disease itself gradually progresses.
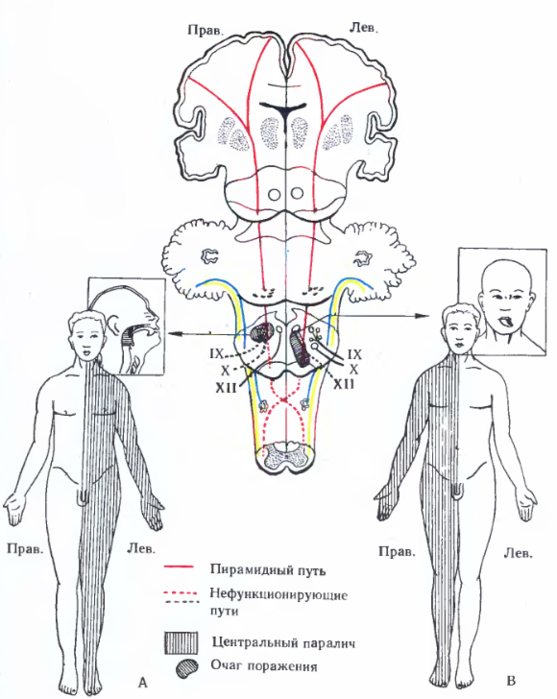
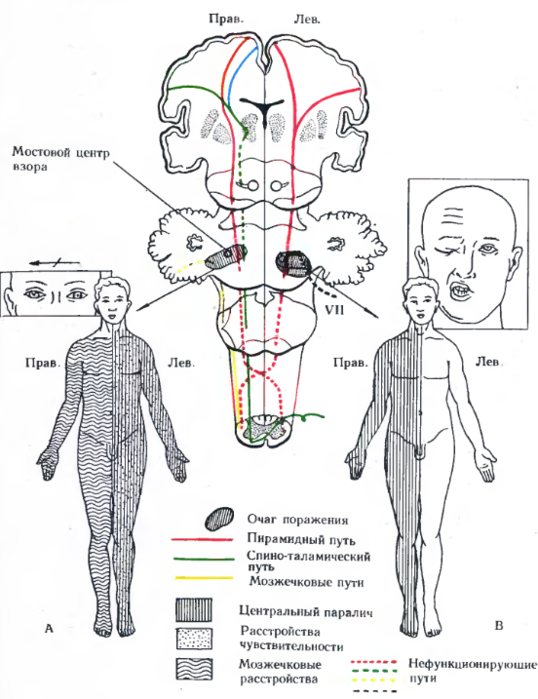
Bulbar alternating syndromes
- Avellis syndrome (palatopharyngeal paralysis) develops when the nuclei of the glossopharyngeal and vagus nerves and the pyramidal tract are damaged. It is characterized on the side of the lesion by paralysis of the soft palate and pharynx, on the opposite side by hemiparesis and hemihypesthesia. (in the diagram - A)
- Jackson syndrome (medial medullary syndrome, Dejerine syndrome) occurs when the nucleus of the hypoglossal nerve and the fibers of the pyramidal tract are damaged. It is characterized by a paralytic lesion of half the tongue on the side of the lesion (the tongue “looks” at the lesion) and central hemiplegia or hemiparesis of the limbs on the healthy side. (in the diagram - B)
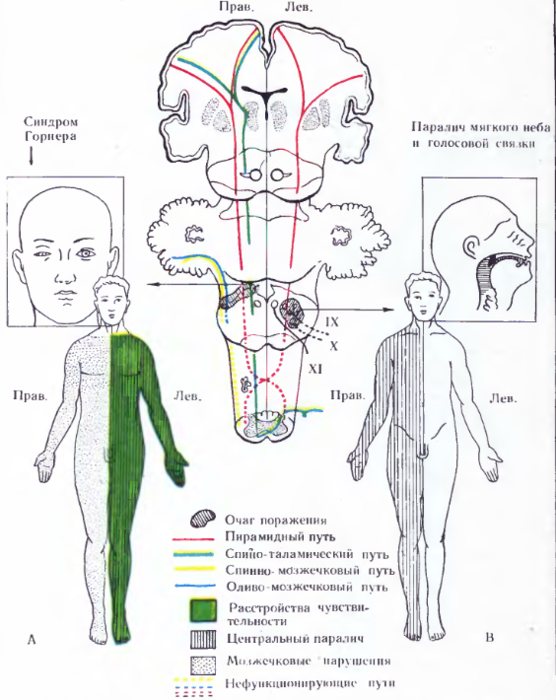
- Babinski-Nageotte syndrome occurs with a combination of lesions of the inferior cerebellar peduncle, olivocerebellar tract, sympathetic fibers, pyramidal, spinothalamic tracts and medial lemniscus. It is characterized on the side of the lesion by the development of cerebellar disorders, Horner's syndrome, on the opposite side - by hemiparesis, loss of sensitivity (In the diagram - A).
- Schmidt's syndrome is characterized by combined damage to the motor nuclei or fibers of the glossopharyngeal, vagus, accessory nerves and pyramidal tract. It manifests itself on the side of the lesion as paralysis of the soft palate, pharynx, vocal cord, half of the tongue, sternocleidomastoid and upper part of the trapezius muscle, on the opposite side - hemiparesis and hemihypesthesia. (In the diagram - B).
Wallenberg-Zakharchenko syndrome (dorsolateral medullary syndrome) occurs when the motor nuclei of the vagus, trigeminal and glossopharyngeal nerves, sympathetic fibers, inferior cerebellar peduncle, spinothalamic tract, and sometimes the pyramidal tract are damaged. On the side of the lesion, paralysis of the soft palate, pharynx, vocal cord, Horner's syndrome, cerebellar ataxia, nystagmus, loss of pain and temperature sensitivity of half the face are noted; on the opposite side - loss of pain and temperature sensitivity on the torso and limbs. Occurs when the posterior inferior cerebellar artery is damaged. Several options are described in the literature.
Reasons for development
Michael Jackson syndrome in adults may occur for the following reasons:
- The presence of intracerebral tumors, as well as neoplasms in any area of the body.
- Presence of traumatic brain injuries.
- Failed brain surgery.
- Various anomalies of vascular activity in the brain area.
- An inflammatory process that began in the substance and membrane of the bone marrow. This disease is called meningoencephalitis. It negatively affects the functioning of the cerebral cortex, causing seizures.
- Various infectious diseases.
- Congenital diseases.
It should be noted here that this syndrome, due to heredity, appears only in childhood, and by the age of 25 it completely disappears. However, possible relapses can also occur in older people.

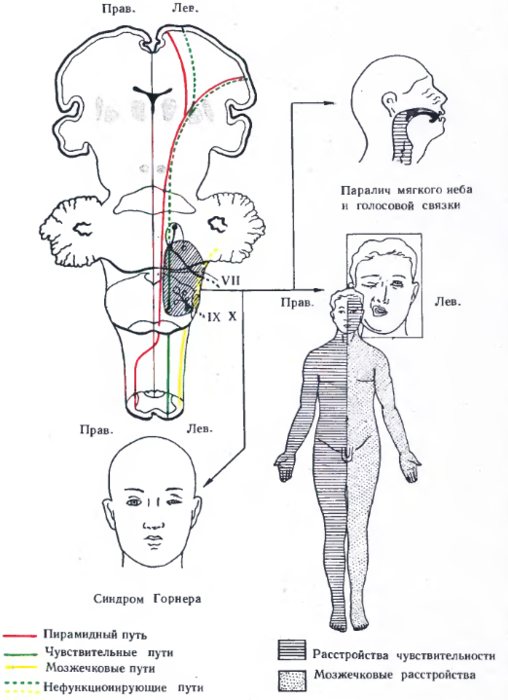
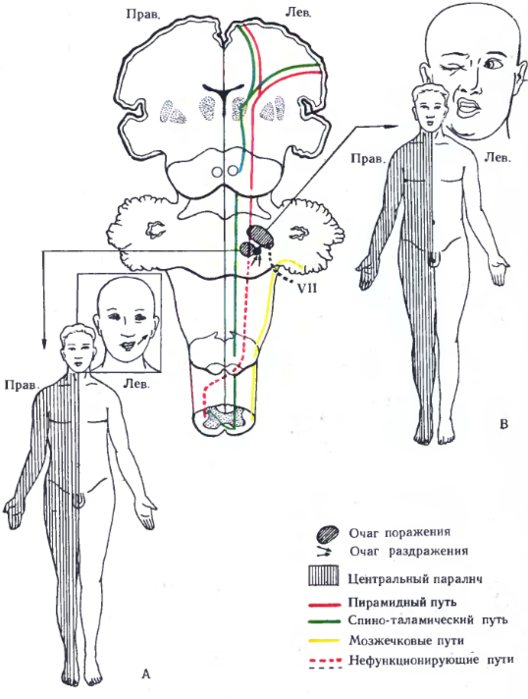
Pontine alternating syndromes
- Raymond-Sestan syndrome is observed with damage to the posterior longitudinal fasciculus, middle cerebellar peduncle, medial lemniscus, and pyramidal tract. It is characterized by paralysis of gaze towards the lesion, on the opposite side - hemihypesthesia, sometimes hemiparesis. (On the diagram - A)
- Millard-Gubler syndrome (medial pontine syndrome) occurs when the nucleus or root of the facial nerve and pyramidal tract are affected. It manifests itself on the side of the lesion as paralysis of the facial nerve, on the opposite side as hemiparesis. (In the diagram - B)
Brissot-Sicard syndrome occurs when the nucleus of the facial nerve is irritated and the pyramidal tract is damaged. It is characterized by facial hemispasm on the side of the lesion and hemiparesis on the opposite side (In the diagram - A). Foville syndrome (lateral pontine syndrome) is observed with combined damage to the nuclei (roots) of the abducens and facial nerves, the medial lemniscus, and the pyramidal tract. Characterized from the side of the lesion by abducens nerve palsy and gaze paralysis towards the lesion, sometimes by facial nerve palsy; on the opposite side - hemiparesis and hemihypesthesia (In the diagram - B).
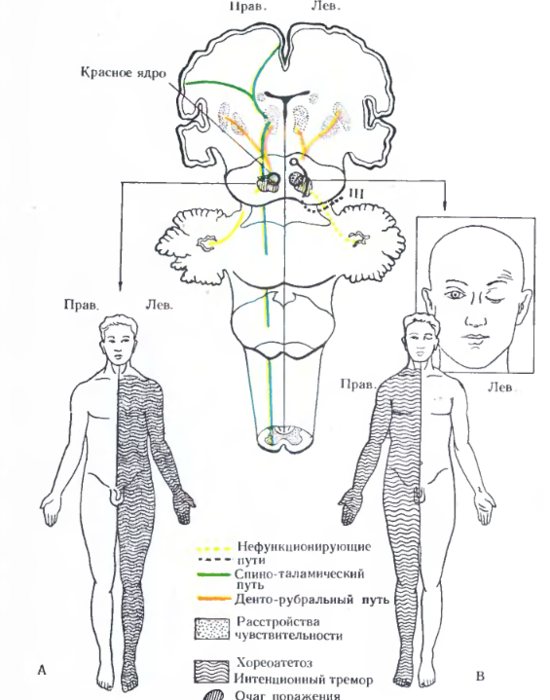
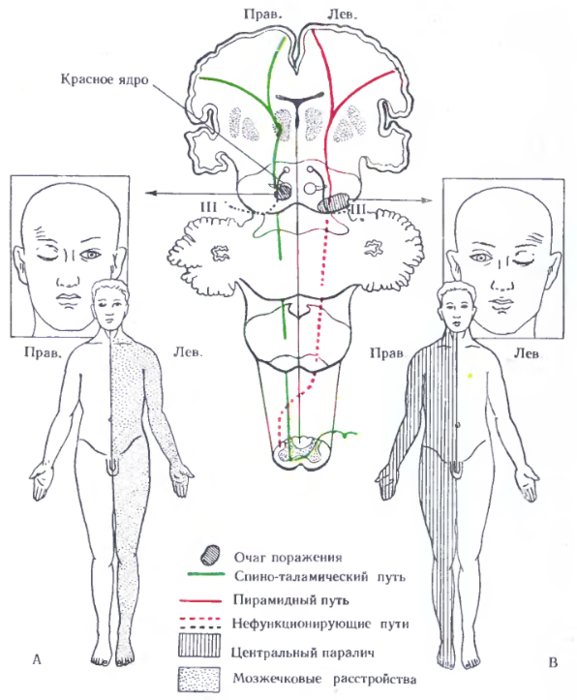
Peduncular alternating syndromes
- Benedict's syndrome (superior red nucleus syndrome) occurs when the nuclei of the oculomotor nerve, red nucleus, red nucleus-dentate fibers, and sometimes the medial lemniscus are affected. On the side of the lesion, ptosis, divergent strabismus, and mydriasis occur, on the opposite side - hemiataxia, eyelid trembling, hemiparesis without Babinsky's sign (In the diagram - B).
- Foix syndrome occurs when the anterior parts of the red nucleus and fibers of the medial lemniscus are affected without involving the oculomotor nerve. The syndrome includes choreoathetosis, intention tremor, and hemitype sensitivity disorder on the side opposite to the lesion. (in the diagram - A)
- Weber's syndrome (ventral mesencephalic syndrome) is observed when the nucleus (root) of the oculomotor nerve and the fibers of the pyramidal tract are damaged. On the affected side, ptosis, mydriasis, and divergent strabismus are noted, on the opposite side - hemiparesis. (In the diagram - B)
- Claude's syndrome (dorsal mesencephalic syndrome, inferior red nucleus syndrome) occurs when the nucleus of the oculomotor nerve, superior cerebellar peduncle, or red nucleus is damaged. It is characterized on the affected side by ptosis, strabismus, mydriasis, and on the opposite side by hemiparesis, hemiataxia or hemiasynergia. (On the diagram - A)
Nothnagel syndrome occurs with combined damage to the nuclei of the oculomotor nerves, the superior cerebellar peduncle, the lateral lemniscus, the red nucleus, and the pyramidal tract. On the side of the lesion, ptosis, divergent strabismus, and mydriasis are noted, on the opposite side - choreoathetoid hyperkinesis, hemiplegia, paralysis of the facial and tongue muscles.
Alternating syndromes associated with damage to several parts of the brain stem.
Glick syndrome is caused by damage to the optic, trigeminal, facial, vagus and pyramidal tract nerves. On the affected side - peripheral paralysis (paresis) of the facial muscles with their spasm, pain in the supraorbital region, decreased vision or amaurosis, difficulty swallowing, on the opposite side - central hemiplegia or hemiparesis. Cross hemianesthesia is observed when the nucleus of the spinal tract of the trigeminal nerve is damaged at the level of the pons or medulla oblongata and fibers of the spinothalamic tract. On the affected side there is a disorder of superficial sensitivity on the face of a segmental type, on the opposite side there is a disorder of surface sensitivity on the trunk and limbs.
Treatment methods
Most often, there is no hemorrhage; the disease is not fatal. But if left untreated, various life-threatening complications can develop. Therefore, if the above symptoms appear, measures should be taken immediately.

As soon as Wallenberg-Zakharchenko syndrome first appears, vital brain functions must be stabilized and tissue swelling removed. It is better to carry out all manipulations in the first hours after the attack.
Less damage will occur if help is provided in a timely manner. The recovery process will be easier and faster. With prolonged failure to provide assistance, irreversible changes occur, and this, in turn, provokes a person’s disability.
If breathing is impaired, oxygen therapy is necessary. For this, a mask or artificial ventilation is used.
Extracerebral alternating syndromes.
Alternating syndrome at the level of the spinal cord - Brown-Séquard syndrome - a combination of clinical symptoms that develop when half the diameter of the spinal cord is affected. On the affected side, spastic paralysis, conduction disorders of deep (muscular-articular sense, vibration sensitivity, sense of pressure, weight, kinesthesia) and complex (two-dimensional-spatial, discriminatory, sense of localization) sensitivity, and sometimes ataxia are observed. At the level of the affected segment, radicular pain and hyperesthesia, the appearance of a narrow zone of analgesia and termanesthesia, are possible. On the opposite side of the body, there is a decrease or loss of pain and temperature sensitivity, and the upper level of these disorders is determined several segments below the level of the spinal cord lesion. When lesions occur at the level of the cervical or lumbar enlargements of the spinal cord, peripheral paresis or paralysis of the muscles innervated by the affected anterior horns of the spinal cord develops (peripheral motor neuron damage). Brown-Séquard syndrome occurs with syringomyelia, spinal cord tumor, hematomyelia, ischemic disorders of the spinal circulation, injury, spinal cord contusion, epidural hematoma, epiduritis, multiple sclerosis, etc. True half-damage to the spinal cord is rarely observed. Most often, only part of half of the spinal cord is affected - a partial variant in which some of its constituent signs are absent. In the development of different clinical variants, the localization of the pathological process in the spinal cord (intra- or extramedullary), its nature and characteristics of the course, the different sensitivity of the afferent and efferent conductors of the spinal cord to compression and hypoxia, individual characteristics of vascularization of the spinal cord, etc. play a role. - diagnostic value. The localization of the lesion in the spinal cord is determined by the level of impairment of surface sensitivity. Asphygmohemiplegic syndrome (brachiocephalic arterial trunk syndrome) is observed with unilateral irritation of the nucleus of the facial nerve, vasomotor centers of the brain stem, and damage to the motor zone of the cerebral cortex. On the affected side there is a spasm of the facial muscles, on the opposite side there is central hemiplegia or hemiparesis. There is no pulsation of the common carotid artery on the affected side. Vertigohemiplegic syndrome is caused by unilateral damage to the vestibular apparatus and motor zone of the cerebral cortex due to circulatory disorders in the system of the subclavian and carotid arteries with impaired circulation in the labyrinthine (vertebrobasilar basin) and middle cerebral arteries. On the affected side - noise in the ear, horizontal nystagmus in the same direction; on the opposite side - central hemiplegia or hemiparesis. Optical-hemiplegic syndrome occurs with unilateral damage to the retina, optic nerve, and motor area of the cerebral cortex due to circulatory disorders in the internal carotid artery system (in the basin of the ophthalmic and middle cerebral arteries). On the affected side there is amaurosis, on the opposite side there is central hemiplegia or hemiparesis.
What else needs to be done?
Cardiac activity should be maintained, and also try to stabilize blood pressure at normal levels. After all, it is arterial hypertension that often leads to Wallenberg-Zakharchenko syndrome. The patient must take medications to lower blood pressure on an ongoing basis.
In addition, cardiac glycosides and nitrates are prescribed. It is necessary to normalize blood clotting and its thickness. Neuroprotectors protect brain cells. With the help of special medications, pain is relieved and muscles relax. Anticonvulsants and sedatives are also often prescribed.
Wallenberg-Zakharchenko syndrome is discussed in detail in this article.
Main factors of damage
Most often, alternating syndrome is caused by some forms of infections, including E. coli, streptococci, and various bacteria, which spread primarily in two ways: hematogenous and contact.
Foville syndrome in neurology appears hematogenously:
- due to metastatic abscesses that occur as a result of pneumonia, pulmonary abscess or infection of the valvular heart apparatus (endocarditis);
- with purulent lung lesions, which is considered the most common among others;
- if hygiene rules are not followed and sanitary standards are not met (administration of medications through a vein).
The source of the disease can be determined only in 80 percent of all cases. The symptoms of Foville syndrome are very pronounced.
Appearance by contact:
- due to the spread of purulent lesions in the oral cavity, pharynx, orbit or paranasal sinuses;
- infections that appear as a result of open damage to the skull and the appearance of subdural hematomas.
Therapeutic measures
Therapeutic therapy should first of all combat the etiology of the syndrome. Bilateral inferior rectus recession helps free up the superior gaze, improve convergence movement. Most often, specialists prescribe complex treatment using antibiotics and corticotherapy. If Parinaud's syndrome is of tumor origin, then surgery is used for treatment.
The main danger of such a syndrome is damage to neighboring areas of the body and worsening of the etiological condition. The main symptoms in most cases go away for a very long time, within several months.
But there have been cases of rapid improvement in the patient’s condition, normalization of intravenous pressure when using ventriculoperitoneal shunting. Complications occur in rare cases and are associated primarily with the etiology of the disease - benign tumors can begin to change, and pathogenic pathogens can spread to other parts of the central system.