The trigeminal nerve is located in the facial part, and since people do not cover their faces even in winter, it can easily get cold.
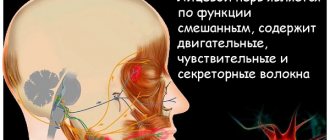
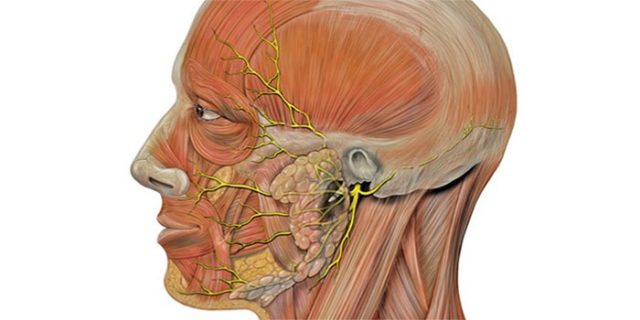
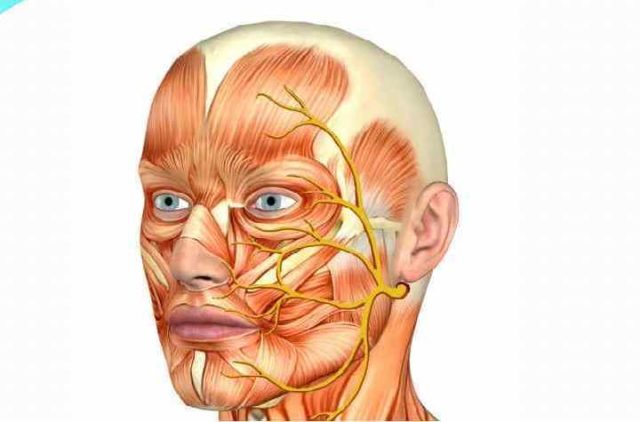
To do this, you just need to be in a strong draft or stay in the cold for some time. Inflammation of the trigeminal nerve is always inappropriate. In addition to severe pain, the disease is accompanied by other troubles that can develop into a serious problem. The trigeminal nerve is very important, because it is responsible for the sensitivity of the eyes, the mobility of facial muscles, and provides the glandular tissue with nerve cells. Outwardly, it resembles a node with three branches: the ophthalmic branch runs above the eyebrows, the maxillary nerve runs on both sides of the nose slightly below the eyes, and another branch stretches from the corners of the mouth to the chin, the mandibular nerve. This complex system can become inflamed for various reasons. Doctors call the following the most common:
• hypothermia;
• mechanical impact (impacts, injuries);
• diseases of ENT organs;
• nervous overstrain;
• malocclusion;
• presence of herpetic infection;
• unqualified treatment of dental and cold diseases;
• age-related deterioration of blood circulation;
• food poisoning.
According to statistics, the trigeminal nerve becomes inflamed more often in those who have reached 40 years of age. Elderly people suffering from various vascular pathologies (hypertension, atherosclerosis, endarteritis and others) are also at risk. In order to begin treatment for inflammation of the trigeminal nerve in time, it is necessary to recognize its symptoms and find out the cause. For a specialist, this is not particularly difficult, since this illness is almost always accompanied by characteristic, pronounced symptoms, and it is almost impossible to attribute them to any other illness.
Inflammation of the trigeminal nerve
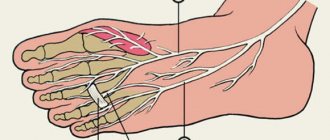
The trigeminal nerve is a ganglion that gives rise to three “branches” that exit directly from the brain stem.
Three “branches” reach directly to the human face, supplying it with nerves and connecting it with the central nervous system. The trigeminal nerve exits the skull through three different foramina. The first “branch” comes out through symmetrical points that are located slightly above the person’s eyebrows (the so-called ocular process). The second, emerging, passes along both sides of the nose (just below the eye area and close to the cheeks) and is therefore called the maxillary, the third “branch” exits in the lower jaw (mandibular) in the direction from the corners of the mouth to its center.
With inflammation of various processes of the trigeminal nerve, pain is observed, localized in various places of the face. When the first “branch” is inflamed, pain occurs above or below the brow ridge, in the forehead and in the front part of the temporal region of the head. When the second and third “branches” of the trigeminal nerve become inflamed, pain occurs in the upper and lower jaws, respectively, which, in turn, causes severe toothache.
Next, we will talk about the types of neuralgia, causes and methods of treatment. But if you are experiencing unbearable pain right now, make an appointment with us. When making an appointment, tell the administrator that you need emergency assistance, and they will find an appointment for you as soon as possible. An appointment with a dentist can be made by calling 8 or using the online appointment form.
Causes of pathology
Maxillofacial inflammation can occur for many reasons. They can be divided into several groups, which will be presented in the table below.
| Pathway of inflammation transmission | Characteristic | Causes |
| Odontogenic | Transmission occurs through infection through diseased teeth. This develops as follows: pathogenic microorganisms approach the root canal through the pulp, and periodontitis appears. |
- untreated caries;
- pulpitis;
- flux;
- periodontitis, etc.
There are also several predisposing factors that can trigger the development of an inflammatory process in the jaw:
- poor nutrition, stress and overwork, leading to a weakening of the body’s defenses;
- hypothermia;
- the presence of carious teeth (the more there are, the higher the risk of developing the disease);
- the presence of acute or relapse of chronic inflammatory foci, etc.

The clinical picture depends on how severe the inflammatory process is and how the severity of its course is assessed.
Speaking about the general group of symptoms, we can highlight the following signs:
- symptoms of intoxication of the body appear (body temperature rises, the patient feels weak, apathetic, his sleep is disturbed and his appetite disappears);
- around the inflamed area there is hyperemia of the skin, as well as swelling and pain when pressed;
- with strong compression of the upper and lower jaw, you can hear a crunch;
- due to possible displacement of the jaw bones, distortion of facial shape occurs;
- severe pain occurs when eating or talking;
- after sleep, it is difficult for the patient to open his mouth;
- Dizziness, headaches, and decreased sound acuity may occur;
- pain occurs with irradiation to the back of the head, ear, temple.
Attention: the chronic course of the disease occurs with less severe symptoms. The pain is characterized by less severe and sharp pain that occurs during sleep or in the morning. Pain increases when eating or talking. If the inflammatory process occurs in a purulent form, a dense formation is formed, in the place of which the skin becomes stretched with a bright red tint.
If inflammation of the maxillofacial nerve occurs, the clinical picture may be supplemented by the following symptoms:
- cyclical acute excruciating pain that occurs in attacks, especially when chewing food, talking, while washing, etc.
- the face may turn red at the time of pain, drooling or lacrimation may occur;
- There may also be pain in the tooth if the second or third branch of the innervation of the trigeminal nerve is affected.
Any warning symptoms should not be ignored by a specialist. Only a doctor can adequately assess the extent of the lesion, its cause and prescribe treatment.
To understand the disease in more detail, we offer you several important points:
- The pathology most often occurs in an acute form.
- In the case of dental origin of the inflammatory process, the affected gum will turn red, become swollen and painful. When purulent masses penetrate into the gum area, it may recede and loosen the tooth.
- If the inflammation is localized in the premolars and molars, the lip, wings of the nose and the bottom may swell.
- With a palatal purulent lesion, swelling of the lymph nodes in the submandibular region will be noticeable. Such inflammation is often provoked by carious processes in the roots of molars and premolars, and incisors. It can spread to the area of the pharynx, tongue and the entire oral mucosa, and with an increase in the volume of purulent exudate, any meal or attempt to speak can be very painful. When the tissue thins and the thin film breaks through, purulent masses enter the oral cavity, and then can reach the gastrointestinal tract, and this is fraught with other serious complications.
- Odontogenic inflammation of the maxillary sinus can affect the area of the eyes and eyelids, and swelling can spread to the cheekbones, temples and cheeks. Swelling of the eyelids leads to narrowing of the palpebral fissures.
- The inflammatory process in the parotid region often provokes damage to the salivary glands.
Attention: The abundance of purulent exudate is a fundamental factor in the appearance of intoxication of the body, as well as in the occurrence of phlegmon, and then an abscess. These conditions threaten not only the patient’s health, but also his life.
Types of trigeminal neuralgia
Trigeminal neuralgia is divided into two types. The first, the so-called true trigeminal neuralgia, is a holistic disease caused in most cases by compression of the nerve or disruption of the blood supply. The second type - secondary trigeminal neuralgia - is a symptom of a general disease of the body. It could be a tumor or a serious infection.
In most cases, doctors diagnose inflammation of one of the processes of the trigeminal nerve, but in some situations inflammation of two or three processes occurs at once. Inflammation can affect either one side of the face or both, and in different combinations.
Causes of inflammation of the trigeminal nerve
Doctors believe that the main cause of inflammation of the trigeminal nerve is compression of it either inside the skull or outside it. Inside the skull, the trigeminal nerve can be compressed as a result of the formation of tumors, in most cases resulting from some kind of head injury.
Also a fairly common cause of inflammation of the trigeminal nerve is internal venous or arterial displacement.
Other causes of trigeminal neuralgia include:
- the presence of a chronic inflammatory process, viral or bacterial infection in the body;
- herpes infection (herpes);
- a brain tumor;
- scarring in the brain stem;
- failure of anesthesia during treatment or tooth extraction.
Most often, inflammation of the trigeminal nerve affects women at pre-retirement and retirement age (usually from fifty to seventy years). If trigeminal neuralgia is diagnosed in a young man or girl, then most likely its cause is a change in the arteries of a sclerotic nature or a strong dilatation of blood vessels.
How does inflammation of the trigeminal nerve manifest?
The main symptom of inflammation of the trigeminal nerve is severe pain that occurs in the facial part. The pain really has a powerful force and shooting character, so it is very difficult for the patient to calmly endure painful attacks. The pain intensifies when performing the slightest actions with the facial muscles and jaws - yawning, chewing, laughing, and performing daily oral hygiene. At the same time, the sensitivity of the skin on the inflamed side of the face decreases.
The next painful attack is accompanied by a rapid dilation of the patient’s pupils and the same rapid contraction of facial muscles. Increased tear production may begin.
Pain with trigeminal neuralgia is severe, but not constant. The pain occurs for a few seconds and is interrupted for a while. But if the intervals between painful attacks are short, then it seems that the pain is constant. Trigeminal neuralgia is dangerous because the interval between attacks can be several weeks, and sometimes even several months. But after this period, the pain will certainly return. A long break does not mean that the disease has passed, so if you have already noticed symptoms of neuralgia once, you should immediately consult a doctor.
Symptoms of inflammation of the upper and lower jaw nerves and their treatment tactics
In the facial part, the largest is the trigeminal nerve. It received its name due to the presence of 3 branches emerging from its node in the temple area: orbital (above), maxillary (middle) and mandibular (bottom). They provide tissue sensitivity and muscle movement on the head. For various reasons, inflammation can affect the entire trigeminal nerve or 1-2 of its branches.
Introduction
Conservative treatment involves the use of drugs of different types of action on the fibers of the facial part of the head. Inflammation is relieved with hormonal, anticonvulsant, antibacterial (if it is caused by pathogenic microflora) and anti-inflammatory drugs.
Disease of the jaw nerve often manifests itself as a result of injury or hypothermia, especially in the facial area of the head. Disorders of the functioning of the trigeminal nerve often arise due to damage to the fibers by the herpes virus.
Neuralgia symptoms can last more than 24 months. To overcome intoxication due to an inflammatory process affecting the trigeminal or other facial nerve, it is necessary to adhere to a diet throughout the entire recovery period. In some cases, fasting is included in treatment to detoxify the body.
Symptoms of inflammation
If the functioning of at least one branch of the trigeminal nerve is disrupted, the superficial and/or deep sensitivity of the corresponding facial region is completely or partially lost.
The pathology manifests itself in the same way: muscles contract incompletely or unevenly or there is tonic tension (prolonged spasm), discomfort, decreased (anesthesia) or increased (hyperesthesia) tactile sensitivity.
Symptoms of inflammation of the maxillary nerve are associated with the disappearance of skin sensitivity in the following areas:
- lower eyelid;
- upper cheek area;
- maxillary sinus;
- at the outer corner of the eye;
- lateral area of the face;
- mucous membrane in the area of the wings of the nose;
- the upper jaw and the teeth and lips located on it.
Additional symptoms: sharp or aching pain, involuntary twitching of the lower eyelid (tic) appears in the area of the affected branch II. If pain is added in the eye area and the entire area above it (under the eyebrow, on the forehead), it means that the inflammation has affected the orbital nerve.
Symptoms of damage to the III (mandibular) branch:
- loss of sensation;
- paresis or paralysis of the masticatory muscle;
- asymmetry of the muscular contour.
The susceptibility of soft and hard tissue in the area of the lower jaw and the mucous membranes adjacent to it in the oral cavity increases or decreases.
Inflammation of the nerve causes symptoms such as pain on palpation or loss of tactile sensations in the area of the outer and inner side of the lower lip, as well as the cheek.
The lesion may affect the gums, teeth, mandibular bone (from the chin to the corner under the earlobe), tongue and sublingual area.
Symptoms of paresis or paralysis due to nerve inflammation:
- reduced strength of chewing muscles (weak bite);
- the mouth is slightly open, while the jaw is shifted towards the source of the disease;
- the mandibular reflex is impaired (the speed of pulling the jaw upward).
However, when one of the branches is inflamed, symptoms often appear in the adjacent area of the face. If, for example, the middle nerve is affected, stronger pain and other sensations may appear in the area of the I and III branches. When the inflammation affects the gasser node itself or its root, the pathology spreads completely to one side, rarely to both parts of the face.
Symptoms of neuritis are expressed as a tic with increased attacks of sharp pain. It can be acute, paroxysmal, limited to one area or covering half of the face on the affected side. Additionally, the vasomotor reaction of the vascular system and secretory function are disrupted, since the central nervous system is always connected to all tissues and glands of the body. In this case, it is the thyroid gland.
Diagnosis and treatment of inflammation of the jaw nerves
If the patient complains of various discomforts in the area of the facial nerve, the doctor checks the sensitivity of this area and the correct movement of the muscles. To begin adequate treatment, the doctor first collects anamnesis, examines the person, and, if necessary, prescribes tomography: MRI, CT.
Research methods:
- touching the surface of the skin with a cotton swab (tactile reaction);
- tingling with a needle in the Zelder area (pain sensitivity);
- palpation of the path of the branches;
- please clench and unclench your jaws, open and close your mouth (motor ability).
When diagnosing, it is important to determine the degree of functioning of all branches of the trigeminal nerve. The doctor also examines the strength of the jaw and conjunctival reflex.
Therapy using official medicine methods
The trigeminal nerve, regardless of which branch is affected by inflammation, is treated comprehensively. To eliminate the causes, the doctor, taking into account the complexity of the process, may choose a method of drug therapy or surgical intervention. Treatment involves dietary nutrition, physiotherapy, and the use of herbal remedies (herbs).
Pain is relieved with medications such as Carbamazepine, Gabapentin, Oxcarbazepine, Clonazepam, Baralgin, Nimesil, Trimecain, Ibuprofen and other drugs with a similar effect on the facial and trigeminal nerve.
Treatment rarely includes narcotics for pain relief if classical analgesics are ineffective.
Suitable sedatives include Sodium hydroxybutyrate and Amitriptyline. Additionally, Rosolacrit, vitamin preparations with a predominance of vitamins B6, B12, and immune-stimulating agents (Echinacea purpurea and others) are prescribed.
Drug treatment of inflammation that has developed for other reasons:
- for herpes infection - Gerpevir, Laferon;
- due to atherosclerosis - Atoris, Rosuvastatin.
When a patient's inflammation is caused by multiple sclerosis, medications are prescribed that should restore the nerve, more precisely, its myelin sheath. Treatment of vessel aneurysm is carried out only by surgical methods.
Treatment using traditional medicine methods
At home, therapy is carried out with regular consultations with a neurologist. Inflammation of the nerves is treated with herbs together with medications, physiotherapy, and other methods. Heat compresses are allowed to be used only if there is no purulent focus in the facial area.
When treating inflammation of the nerves, the following drugs can be used:
- bay oil (to lubricate);
- beet juice (gauze pads in the ear);
- marshmallow root, fresh wormwood (compresses);
- hibiscus, chamomile (tea);
- aloe juice (inside).
Externally, folk remedies are applied to areas of nerve damage, to the submandibular lymph nodes, maxillary sinuses, and into the ear canal. Before starting treatment, be sure to familiarize yourself with the contraindications of the herbal medicine.
Conclusion
Inflammation of the facial or trigeminal nerve, a disease that can cause severe complications, should only be treated under the supervision of a neurologist, even if therapy is carried out at home. We must not forget about preventive measures: prevent the development of chronic pathologies in the body, including localization in the ENT organs, avoid drafts and lead a healthy lifestyle.
Source: https://provospalenie.ru/nerva/chelyustnogo.html
Why do teeth hurt when the trigeminal nerve is inflamed?
How is inflammation of the trigeminal nerve related to teeth? The connection here is the most direct. Firstly, severe pain during attacks “radiates” to the upper or lower jaw (depending on which nerve extension is inflamed), and sometimes to both jaws. This causes severe and unbearable toothache.
Secondly, those nerves that are found in the upper and lower teeth and gums are directly connected to the trigeminal nerve. The second branch of the trigeminal nerve innervates the upper teeth and gums, and the third, respectively, the lower jaw and gums.
The trigeminal nerve can also be damaged during a number of dental manipulations. Unsuccessful tooth extraction or improper filling, surgical intervention in the jaw structure that ended unsuccessfully, and injuries can cause trigeminal neuralgia.
It is very important to distinguish inflammation of the trigeminal nerve from other diseases of the oral cavity, in particular pulpitis - inflammation of the internal dental tissues. A characteristic sign of inflammation of the trigeminal nerve is that, despite severe pain, the sensitivity of the teeth does not increase when they come into contact with cold and hot foods, and hypothermia or heating does not provoke the onset of a new pain attack. Acute tooth sensitivity is a symptom of pulpitis.
When the trigeminal nerve is damaged in the jaw area, acute toothache, pain in the chin, ears and sometimes in the lower lip occurs. The pain may become increasingly intense, and often the patient continues to feel a dull ache after the attack.
Neuralgia of the ear ganglion
Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
What is neuralgia of the ear ganglion?
Pathology of the ear autonomic ganglion, which manifests itself in the form of paroxysms of vegetalgia and affects not only the ear, but also the ear region - neuralgia of the ear ganglion. During attacks, acute pain can radiate to the lower jaw, back of the head, shoulder girdle, arm and upper chest.
May be accompanied by congestion, clicking, hypersalivation. In this case, hearing is not impaired. The pathology is diagnosed by a neurologist with the assistance of a dentist, otolaryngologist and other specialized specialists.
Complex therapy includes medications for the relief of painful paroxysms, metabolic drugs, vascular and decongestants, as well as physiotherapeutic procedures and reflexology.
General information about the disease
The auricular autonomic node is called a ganglion. It is a collection of interneurons of the parasympathetic and sympathetic nerve pathways.
Parasympathetic fibers enter the node through the branches of the glossopharyngeal nerve, and sympathetic fibers through the plexus of the middle meningeal artery. Postganglionic fibers are part of the auriculotemporal nerve, which in turn is a branch of the trigeminal nerve.
They extend to the temporal region and the ear gland, providing autonomic innervation of the vessels and gland.
Neuralgia of the ear ganglion can be classified as vegetative ganglionitis of the head. This category of pathologies includes:
- Ciliary ganglionitis;
- Neuralgia of the sublingual and submandibular node;
- Cervical truncite;
- Ganglionitis of the superior cervical sympathetic and pterygopalatine nodes.
According to statistics, neuralgia of the auricular nerve most often affects young and middle-aged women.
Why does this pathology occur?
The etiopathogenetic mechanism of the development of the disease is irritative. /
It develops reflexively if pathological vegetative impulses are received from chronic infectious foci or somatic organs suffering from an inflammatory process.
Diseases that are localized directly next to the ear node are especially dangerous.
These include:
- Periodontitis;
- Gingivitis;
- Stomatitis;
- Periodontitis;
- Ethmoiditis;
- Sinusitis;
- Frontitis;
- Sinusitis;
- Tonsillitis;
- Purulent otitis;
- Stones in the parotid gland;
- Sialadenitis;
- Mumps.
Neuralgia of the auricular nerve, provoked by a general infectious process, is less common. The primary diseases in this case include:
- Syphilis;
- Tuberculosis;
- Protracted sepsis.
Also, the root cause of neuralgia can be a separate infectious focus:
- Urethritis;
- Cystitis;
- Pyelonephritis.
Or somatic diseases:
- Cholecystitis;
- Cirrhosis;
- Gastroduodenitis;
- chronic renal failure;
- Adnexitis.
Sometimes the provoking factor is an endocrine disorder: diabetes mellitus or hyperthyroidism.
Symptomatic picture
Characteristic symptoms are attacks of vegetation. They occur in the ear, parotid area, or in front of the opening of the ear canal on the side of the affected area. The pain is intense or burning.
It radiates to the neck, back of the head, lower jaw and shoulder girdle. Due to the mechanism of pain irradiation, it spreads to the upper part of the thoracic region and the arm on the affected side.
The duration of the attack ranges from several minutes to an hour or more.
Occasionally, paroxysm is accompanied by clicking or congestion in the ear. They are caused by reflex muscle spasms of the auditory tube. Also, during an attack, hypersalivation is noted, while at rest increased salivation does not occur.
Neuralgia can be triggered by:
- Hypothermia;
- Consumption of hot food and drinks;
- High physical activity;
- Psycho-emotional stress.
Since the autonomic nervous system depends on external factors such as temperature changes, changes in daily patterns, barometric pressure, etc., the autonomic system has a rhythmic character. It occurs most often at night and in the evening. In spring and autumn, neuralgia may worsen.
Hearing function remains unchanged during the period of illness.
Diagnostic methods
Very often, patients come for help to an otolaryngologist or dentist, and doctors of this specialty refer them to a neurologist.
To make a diagnosis, the neurologist collects anamnesis, palpates Richet's points and sclerotomal points of the mandibular, auriculotemporal and mental nerves. On palpation there is a sharp pain.
Hyperalgesia of the parotid region confirms neuralgia. To clarify the diagnosis, a lidocaine or novocaine blockade can be performed.
It is very important to correctly determine the etiology of the disease. For this you need:
- Dental examination;
- geometry;
- Ultrasound of the parotid salivary gland;
- Rhinoscopy;
- Otoscopy;
- X-ray of the paranasal sinuses.
- Pharyngoscopy.
In some cases, consultation with a gastroenterologist, urologist, endocrinologist may be required, as well as gastroscopy, ultrasound of the kidneys or abdominal cavity, and analysis of thyroid hormones.
Neuralgia should be distinguished from otitis media, cysts and stones of the parotid gland, tumors, mumps and eustachitis.
Therapy
To quickly stop paroxysms of vegetalgia, you need to take analgesics and anti-inflammatory drugs. These include:
- Acetylsalicylic acid;
- Metamizole sodium;
- Novocaine blockades;
- Aminophenazone.
These drugs are combined with ganglion blockers, sedatives and antispasmodics. If necessary, the patient is prescribed sleeping pills. To achieve an additional analgesic effect, ultraphonophoresis with hydrocortisone or electrophoresis with novocaine on the ear area is indicated.
Vascular and metabolic therapy is also required:
- A nicotinic acid;
- B vitamins;
- Pentoxifylline.
Antihistamines will help reduce swelling. If symptoms characteristic of irritation of parasympathetic fibers predominate in the clinic, anticholinergic therapy is required: diphenyltropine, platyphylline.
In case of intolerance to drug therapy, the following is required:
- Magnetic puncture;
- Acupuncture;
- Laser punctures.
During convalescence, amplipulse therapy, DDT, and electrophoresis with hyaluronidase can be prescribed.
To effectively treat neuralgia, it is necessary to eliminate the root cause of the disease.
Treat an inflammatory or infectious focus, regularly carry out sanitation of the oral cavity and therapy for chronic somatic diseases. Correction of endocrine disorders is also necessary.
According to indications, surgical dissection of adhesions, removal of tumors and parotid stones, maxillary sinusotomy, ethmoidotomy, etc. may be prescribed.
Source: //mrt-v-msk.ru/nevralgiya-ushnogo-uzla/
Treatment of inflammation of the trigeminal nerve
The first stage of treatment for inflammation of the trigeminal nerve is medication. It is aimed at reducing the strength and frequency of pain in the patient. Most often, doctors prescribe anticonvulsants to a patient suffering from trigeminal neuralgia. Sedatives are also used.
Physiotherapeutic procedures, as well as resorption therapy to relieve the inflammatory process, have a good therapeutic effect. Next, the doctor may recommend the use of laser treatment, in which the laser is directed cutaneously to the area where the processes of the trigeminal nerve exit the skull.
Our clinic is located in the same building as the multidisciplinary clinic “Diamed on Shchelkovskaya”, where special conditions for receiving physiotherapeutic procedures are organized for dental patients. The clinic’s physiotherapy room is equipped with modern equipment, including a laser physiotherapy device, with which you will feel relief after the first procedure. The pain will go away and you can return to normal eating. Make an appointment with a dentist by calling 8 or using the online appointment form. The doctor will make an accurate diagnosis and refer you for treatment.
Anatomy
The trigeminal nerve, which includes the maxillary and mandibular branches, contains motor and sensory nuclei. The maxillary nerve consists of three branches:
- infraorbital;
- nodal;
- zygomatic
The infraorbital branch is considered the most powerful branch of the maxillary nerve. It is its direct continuation and, passing under the eye along the groove, reaches the canal in the canine fossa. Here it is divided into branches that innervate:
- lower eyelids and skin around the corner of the eyes;
- the inner and outer parts of the nasal passages;
- skin and mucous membrane of the upper lip, wings of the nose;
- the area near the upper teeth, including the large molars.

Four branches of the maxillary nerve are responsible for the innervation of the teeth of the upper jaw, each of which ensures the transmission of impulses to a strictly defined zone (incisors, canines, small and large molars). These parts in the area of the nasolabial triangle form a rather large knot. Fibers extend from it, providing innervation to the gum tissue.
The nodal branches are represented by several short processes that run along:
- upper palate;
- pharynx (behind the trunk of lingual nerve fibers);
- bottom of both eyes;
- medial and lateral sides of the nasal sinuses.
The nodal branch, connecting its ends with the facial nerve, runs along the bottom of the eye and stops in the cheek, temple and forehead. This section provides exceptionally sensitive perception.
The anatomy of the mandibular nerve is more complex. It exits the cranial cavity through the foramen ovale and extends towards the temporal plexus. Here it is divided into sensory and motor fibers.
The sensitive part of its branches is divided into:
- auriculotemporal;
- buccal;
- lingual;
- lower lunulae.
The auriculotemporal region innervates:
- parotid salivary gland;
- temporomandibular joint;
- part of the temple, ear canal and eardrum.
The buccal branch transmits impulses to the mucous membrane on the inside of the cheek and the corner of the mouth, and the lingual branch - to:
- anterior two-thirds of the tongue;
- sublingual and submandibular salivary glands;
- mucous membrane at the bottom of the mouth;
- pharynx;
- palatine tonsils.
Alveolar nerve fibers running in the mandibular canal innervate the gums and teeth. Also, this branch extends beyond the oral cavity and transmits impulses to the lower lip and chin.
The motor portion of the mandibular nerve is represented by fibers that provide innervation to the muscles responsible for chewing, tension of the tympanic membrane and palatine curtain, and jaw movement.
How to quickly cure neuralgia (inflammation) of the facial nerve
Neuralgia of the facial nerve is a condition in which sharp pain occurs in the area of the nerve trunks located in the temporal part of the head. Since the facial nerve is paired, each half of the face innervates its own section of motor fibers, and therefore most often one half of the face is affected. When the nerve is inflamed, the movement of the facial muscles is disrupted or distorted. ICD-10 disease code: M 79.2 – neuralgia and neuritis, unspecified
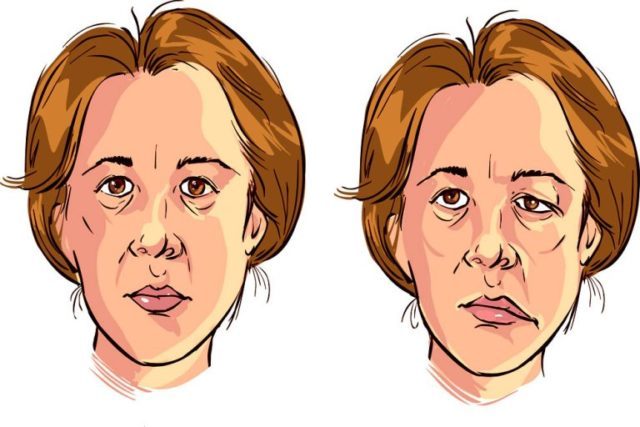
When the facial nerve becomes inflamed, paresis or plegia of the facial muscles occurs, i.e. they weaken or stop moving completely, which is visually noticeable. In addition, the facial nerve contains a large number of taste, pain and secretory fibers, which, when irritated, cause a certain pain syndrome in certain parts of the face: tearfulness, toothache, loss of taste sensitivity, etc.
Neuralgia affects both men and women equally. The frequency is about 25 people per 100,000 population. In most cases, neuralgia is of a vascular nature, but in 80% of cases its true cause cannot be determined.
Symptoms
With inflammation of the submandibular nerve, symptoms are usually determined depending on the location of the pathological process. In most cases, acute pain occurs, which radiates along the affected fibers. But when the maxillary nerve is pinched, the symptoms may differ from the manifestations of mandibular neuralgia.
Traditionally, in addition to pain, the patient with neuritis decreases or increases the sensitivity of a particular part of the face.
Uneven contraction or tonic tension (spasm) of local muscle fibers is possible.
When the nerves of the upper jaw are damaged, sensitivity in the area decreases:
- maxillary sinus;
- upper cheek;
- lower eyelid;
- outer corner of the eye;
- side of the face;
- oral mucosa on the upper jaw;
- upper jaw.
The intensity of pain when nerves and jaw are damaged depends on the characteristics of the disorder. This symptom is acute and aching in nature. The pain may spread towards the eye, indicating damage to the entire trigeminal nerve. Also, with this localization of the pathological process, tic of the lower eyelid is often observed.
When the mandibular nerve fibers are damaged, symptoms appear as:
- decreased sensitivity in the area of the lower jaw and chin;
- paresis or paralysis of the muscles that provide chewing function;
- facial asymmetry.
If the nerve fibers of the lower jaw are affected, the patient experiences increased sensitivity of the hard tissue and mucous membrane to food or palpation.
Such susceptibility is observed both along the entire length of the affected fibers and in the following areas:
- gums;
- teeth;
- mandibular bone;
- language;
- sublingual area.
If paresis or paralysis develops, then a weak bite and the inability to pull the lower jaw upward are of concern. Due to the latter disorder, the patient's mouth remains constantly open.
If damage to the mandibular nerve is suspected, an external examination of the patient and palpation of the problem area are first performed. This form of neuritis is indicated by the inability to close the jaws, muscle spasms, and painful sensations that occur when touched.

Additionally, CT, MRI and electromyography are performed. The first two methods help determine the causes of neuritis and identify the localization of the pathological process. EMG assesses the degree of conduction of nerve fibers and allows one to differentiate neuralgia from other pathologies that have similar symptoms.
Main causes of facial neuralgia
In most cases, neuralgia is the result of hypothermia or drafts, since the peak incidence occurs in the off-season, September and March, when the deceptive sun is still (or already) warming and cold winds are blowing. Lack of headwear, clothing not appropriate for the weather and open windows contribute to inflammation of the facial nerve.
A sharp change in temperature causes a spasm of the vessels supplying the nerve, as a result of which it is compressed in the walls of the bone canal and swelling appears. Because of this, the supply of the nerve is weakened and an acute pain symptom appears. Modern neurologists have come to the conclusion that the etymology of this condition is also compression of the nerve by vessels or abnormally enlarged sclerotic plaques.
The cause of neuralgia may also be other reasons:
- Inflammatory processes (otitis, meningoencephalitis) occurring in the middle ear;
- brain tumors;
- injuries to the facial and temporal parts of the skull;
- inflammatory reaction after surgery;
- narrowing of the bone canal as a result of periodontal disease, caries or sinusitis;
- specific bone structure;
- hereditary factor;
- the result of a herpes infection.
Important! Neuralgia can also appear as a result of age-related changes, against the background of decreased immunity and decreased tissue resistance to external factors.
If the true cause of neuralgia cannot be established, it is considered idiopathic.

Symptoms of neuralgia
When the facial inflammation occurs, the functions of the muscles of the forehead, eyebrows, cheeks and jaw are disrupted. The most painful parts are the chin and the area around the eyes. As a rule, neuralgia appears on one side of the face, but in rare cases a bilateral form occurs.
The sensations may vary, but there are common manifestations that indicate inflammation of the facial nerve: burning-twitching pain in the nasolabial triangle, which lasts from a few seconds to 2-3 minutes. Then the pain subsides, but quickly spreads to other parts of the face nearby.
Important! With facial neuralgia, inflammation most often affects only one half of the face.
During an attack of sharp spontaneous pain, a person suddenly freezes in place and is unable to move further. The skin first turns pale and then may turn red. The first response is to rub the affected part of the face with the palm of your hand. Sharp pain can radiate to other parts of the head: teeth, ear, scalp.
As a result, the following symptoms may appear:
- lacrimation;
- burning in the place where the pain was most intense;
- increased salivation and uncontrolled drooling;
- spots on the skin or redness;
- reduction of pain when pressing;
- deformation of the lips when opening the mouth;
- eyelids do not close completely;
- the person does not fully move his lips (cannot fold them into a tube and kiss);
- pain does not bother you at night;
- may appear near the ear.
All these symptoms complicate normal activities: eating, brushing teeth, speaking loudly, etc.
For everyone who suffers from facial neuralgia, the sensations are individual. Common features are the appearance of pain and distortion of facial expressions.
Clinical picture: symptoms and signs

Symptoms of the disease can be divided into two main groups:
- Pain syndrome.
- Specific manifestations.
The pain is usually localized in the temple area, in the ear, and also in the temporomandibular joint. It usually occurs during meals.
Specific manifestations include swelling in the area of inflammation (in the temple area), increased sweating and salivation, redness of the skin at the site of injury.
Typically, patients suffering from Frey's syndrome complain of:
- burning pain;
- throbbing pain that radiates to the lower jaw;
- attacks of sweating during meals (large drops of sweat appear on the forehead and temples);
- increased salivation.
In some cases, in addition to swelling and increased sweating, the patient experiences sensations of heat and tingling. The disease usually develops against the background of a so-called functional disorder of the nervous system.
All symptoms tend to manifest themselves and intensify while eating. This is due to the etiology of the disease. The patient reacts especially sensitively to sour and salty foods - they aggravate the symptoms.
Additional symptoms and manifestations that may be associated with Frey's syndrome include redness and warmth in the affected areas. This is a rare but important complaint.
What is the danger of the disease
Neuralgia is a condition that can be easily provoked if you are careless about your health. This disease is unfamiliar to some, some have experienced it once, others are less fortunate, and periods of exacerbation are followed by periods of remission.
The danger of facial neuralgia is that it can begin to progress over time: periods of exacerbations become more frequent, and the pain intensifies each time. The patient lives with a subconscious expectation of an attack, which cannot affect his psychological state. Patients leave work, become self-absorbed, and become depressed. They no longer care what they look like - they have lost interest in life.
There are several degrees of damage to the facial nerve:
- Easy. Facial expressions are not impaired, muscle weakness is revealed only with a thorough examination. There may be slight drooping of the corner of the mouth and difficulty closing the eyelid;
- Moderate. Facial paresis is noticeable, but does not change his expression too much. Closing the eyes requires little effort. The mobility of the forehead muscles is preserved;
- Medium-heavy. Manifests itself in the form of pronounced facial asymmetry. The forehead muscles are motionless, it is difficult to close the eye;
- Heavy. Muscle movements are barely noticeable, the eye does not actually close (Bell's palsy), the forehead muscles are motionless;
- Extremely severe total plegia. The affected side of the face is completely immobilized. Restoration of facial expressions is practically impossible.
If neuralgia is diagnosed and treated in a timely manner, the consequences for the body will be minimal.
Necessary diagnostics
Treatment of neuralgia is the field of activity of a neurologist. First of all, he conducts an examination, and then prescribes a number of studies that will help clarify the diagnosis:
- UAC;
- ENMG (electromyography), determines the degree of nerve damage;
- radiography of the temporal bone and sinuses to exclude ENT disease;
- MRI of the brain, which will help rule out the presence of a tumor in the brain, stroke or other diseases.

Diagnostic methods

When the first suspicious symptoms appear, the patient is recommended to consult a doctor for diagnosis.
To make an accurate diagnosis, the doctor studies all the symptoms and manifestations of the disease, the patient’s complaints, collects anamnesis, and examines the affected area. To make an accurate diagnosis, laboratory and instrumental studies are carried out , including specialized tests.
The essence of specialized tests is to carry out laboratory manipulations in order to confirm or refute the alleged diagnosis. The manipulations are aimed at identifying the body’s specific reaction to external stimuli (physical, chemical effects). Such tests are used in all branches of medicine, including neurology.
Treatment
When treating facial neuralgia, the main goal is to stop the inflammatory process and eliminate it. Therefore, treatment should be comprehensive and include medication, massage, special gymnastics and folk remedies.
Medication
Taking non-steroidal anti-inflammatory drugs such as Diclofenac, Ibuprofen, Nise, Meloxicam will help relieve acute pain.
Taking Prednisolone will help relieve swelling and improve blood circulation. It is advisable to start taking it from the first days of illness.
To relieve spasms of the facial nerve, anticonvulsants are prescribed, such as Tegretol, Trileptal, Diphenin.
Taking antidepressants will help you endure pain more calmly and improve your psychological state, because each of us has a different pain threshold, and maintaining calm is extremely important.
Prevention of facial neuralgia
Since inflammation of the facial nerve in most cases is associated with the off-season, special attention should be paid to prevention during this period. To do this, you need to take care of your immunity in a timely manner, avoid hypothermia, avoid drafts and direct exposure of the wind to areas of the face that have already suffered inflammation.
In addition, it is important to harden yourself and choose clothes and hats that are appropriate for the weather. You should undergo timely examination and treatment by a dentist and ENT specialist.
Remember, neuralgic pain of the facial nerve is one of the most severe and difficult to treat. Timely preventive measures will help you avoid an unpleasant condition and lead a full life.
Treatment methods
Treatment tactics are selected based on the characteristics of the causative factor. Drug therapy is mainly used, the effect of which is aimed at relieving the symptoms of the disease and eliminating inflammation, including pain relief.
If the maxillofacial nerve is damaged, painkillers are used at the beginning of treatment:

If treatment of neuritis with analgesics does not produce a positive result, then narcotic medications are prescribed. In severe cases, trunk anesthesia is performed, in which anesthetic medication is injected directly into the affected area.
Treatment for neuritis of the submandibular nerve is determined taking into account the symptoms and characteristics of the provoking factor. Broad-spectrum antibacterial drugs are used in therapy. Additionally, antiherpetic medications are prescribed. To restore nerve conduction, B vitamins are prescribed.

Neuralgia of the submandibular nerve fibers cannot be treated using traditional medicine. Such treatment is used only in consultation with a doctor to relieve concomitant symptoms. Helps reduce the intensity of pain:
- chamomile or hibiscus tea;
- bay oil;
- beet juice;
- aloe juice (taken orally);
- compresses from decoctions of fresh wormwood or marshmallow root.
Neuritis is also treated using physiotherapy methods: electro- and phonophoresis, UHF and others. Massaging the affected area during an exacerbation is prohibited.
Pain after dental implantation, tooth implant hurts
During dental implantation, the trigeminal nerve and its branches, the alveolar nerve plexus, may be damaged as a result of:
- Screwing the implant into the canal where the trigeminal nerve or its branches lies;
- Inflammation in the implant area (infection and/or implant rejection).
Some pain during the implant healing process is normal. If the pain after dental implantation lasts too long, is very severe, or is accompanied by numbness of the lip or cheek, we can check the condition of the trigeminal nerve using electromyography and a neurological examination based on the characteristic loss of facial sensitivity and the spread of pain along the trigeminal nerve system.
The rejection reaction and inflammatory processes in the implant area are usually clearly visible with CORRECT X-ray examination and computed tomography.
Implants in the lower and upper jaw. Pain after dental implantation

There may be direct pressure from the implant on the nerve or inflammation in the implant area with tissue swelling, edema and subsequent pressure on the nerve.
Inflammation of the lower and upper jaw
Inflammatory process in the jaw
Inflammation of the jaw is a serious disease that can have serious consequences. When the first symptoms appear, you should immediately consult a doctor and begin treatment. Inflammation of the jaw is the cause of many complications, although it is not so common in dental practice.
The etiology of the disease is different, but often the cause of its appearance is infection. Treatment of the inflammatory process can take quite a long period of time, even with timely diagnosis.
Classification of the disease
The inflammatory process in the jaw can be classified into several types:
- Osteitis. In this case, the spongy substance in the bone tissue becomes inflamed. It does not last long and takes the form of periostitis.
- Periostitis . The inflammatory process is localized in the periosteal tissue of the jaw and is the result of a complication of periodontitis. Speaking about the clinical picture, the following symptoms can be identified:
- The gums around the diseased tooth begin to swell, it becomes hyperemic and swollen;
- strong painful sensations appear;
- it is possible to discharge purulent contents from the swollen gums.
If a purulent cavity occurs, fistulas may form to allow the pus to escape. In advanced situations, an intensification of the pathological process and purulent inflammation of bone tissue is possible.
- Osteomyelitis. In this case, all layers of bone tissue are affected, and most often this is observed in the lower jaw.
The disease with neuritis is especially difficult, i.e. when the trigeminal nerve is also involved in the process. If inflammation of the jaw nerve occurs, the symptoms are expressed in excruciating pain, mainly on one side of the face.
Inflammation of the nerve under the jaw
There are also several forms of jaw inflammation:
- Acute course of the disease. Pain and inflammation are localized in one place. Symptoms of body intoxication appear quite sharply.
- In the subacute form, the patient feels a little better and may think that the disease has subsided, but this is not so. The inflammation still continues, it’s just that a fistula has formed and pus has broken through, so the pain has subsided somewhat.
- In the chronic form there are no special clinical symptoms, but during this period there is a great danger to the patient’s health, since untreated inflammatory foci can cause more serious complications.
It is very important to notice the disease in time and consult a doctor for help.
Inflammation of the lower and upper jaw
So how does inflammation occur? There are several pathways through which infectious agents penetrate the bone marrow and bone. As a result, the periosteum becomes inflamed, swells, and periostitis develops.
Depending on the severity of periostitis, the following forms can be distinguished:
- The form is simple. Appears as a result of injuries, severe bruises and fractures.
- The form is fibrous. As fibrous tissue grows, the layers of the periosteum thicken.
- Ossifying form. In this case, the tissues also grow, and the formation of a chronic inflammatory process begins.
- The form is purulent. Purulent cavities form. The more there are, the more serious the danger to the body.
Moreover, when abscesses form, the process spreads to the entire bone and the development of limited osteomyelitis begins with the gradual capture of large areas of the jaw.
Photo of periostitis of the lower jaw
Upper jaw
Inflammation of the upper jaw is somewhat different from a similar process in the lower jaw. Especially in this case, the orbit, maxillary sinus, and middle ear are vulnerable.
Due to the fact that inflammation often develops covertly, the disease is diagnosed already in the later stages, and this is fraught with the development of various complications due to the release of large volumes of purulent masses.
These may include the following consequences:
- phlegmon;
- abscess;
- sepsis (blood poisoning);
- decreased mobility of facial veins, etc.
Also, involvement of the maxillary sinus in the pathological process can cause the development of sinusitis, sinusitis, etc.
To understand what this entails, let's look at its functions:
- forms nasal breathing;
- develops an individual timbre and sonority of the voice;
- participates in odor recognition.
In addition, the ciliated epithelium, located in the maxillary cavities, also performs a cleansing function, so inflammation in the right maxillary sinus, left, or on both sides is considered a fairly serious complication requiring medical intervention.
Lower jaw
As a result of the progression of purulent periostitis, inflammation of the lower jaw develops. A feature of this disease is that the pathological process can affect not only bones, but also soft tissues.
In frequent cases, the cause of the pathology is the odontogenic route of infection as a result of advanced carious processes in the teeth or untreated periodontitis. To learn more about inflammation of the lower or upper jaw, we suggest watching the video in this article.
Causes of pathology
Maxillofacial inflammation can occur for many reasons. They can be divided into several groups, which will be presented in the table below.
| Pathway of inflammation transmission | Characteristic | Causes |
| Odontogenic | Transmission occurs through infection through diseased teeth. This develops as follows: pathogenic microorganisms approach the root canal through the pulp, periodontitis appears. The inflammatory process then spreads to the periosteal tissue, and then affects all layers of the bone. In this case, there is also a great danger of infection (usually anaerobic bacteria, streptococci, staphylococci) entering the lymph nodes with subsequent infection | The following diseases can provoke such a disorder:
|
| Hematogenous | Infection of the jawbone occurs primarily through the blood. If there is a pathological focus in any organ or system, the infection through the circulatory system can reach the bone tissue of the jaw and cause its inflammation. First, the bone itself may be affected, and then the teeth. Most often, this route of transmission occurs against a background of weakened immunity. | This includes:
|
| Traumatic | Appears as a result of physical damage to the jaw bone | Mechanical damage can occur as a result of the following reasons:
|
Causes of jaw inflammation
There are also several predisposing factors that can trigger the development of an inflammatory process in the jaw:
- poor nutrition, stress and overwork, leading to a weakening of the body’s defenses;
- hypothermia;
- the presence of carious teeth (the more there are, the higher the risk of developing the disease);
- the presence of acute or relapse of chronic inflammatory foci, etc.
What symptoms accompany the inflammatory process?
The clinical picture depends on how severe the inflammatory process is and how the severity of its course is assessed.
Speaking about the general group of symptoms, we can highlight the following signs:
- symptoms of intoxication of the body appear (body temperature rises, the patient feels weak, apathetic, his sleep is disturbed and his appetite disappears);
- around the inflamed area there is hyperemia of the skin, as well as swelling and pain when pressed;
- with strong compression of the upper and lower jaw, you can hear a crunch;
- due to possible displacement of the jaw bones, distortion of facial shape occurs;
- severe pain occurs when eating or talking;
- after sleep, it is difficult for the patient to open his mouth;
- Dizziness, headaches, and decreased sound acuity may occur;
- pain occurs with irradiation to the back of the head, ear, temple.
Attention: the chronic course of the disease occurs with less severe symptoms. The pain is characterized by less severe and sharp pain that occurs during sleep or in the morning.
Pain increases when eating or talking.
If the inflammatory process occurs in a purulent form, a dense formation is formed, in the place of which the skin becomes stretched with a bright red tint.
If inflammation of the maxillofacial nerve occurs, the clinical picture may be supplemented by the following symptoms:
- cyclical acute excruciating pain that occurs in attacks, especially when chewing food, talking, while washing, etc.
- the face may turn red at the time of pain, drooling or lacrimation may occur;
- There may also be pain in the tooth if the second or third branch of the innervation of the trigeminal nerve is affected.
Any warning symptoms should not be ignored by a specialist. Only a doctor can adequately assess the extent of the lesion, its cause and prescribe treatment.
A few facts worth noting
To understand the disease in more detail, we offer you several important points:
- The pathology most often occurs in an acute form.
- In the case of dental origin of the inflammatory process, the affected gum will turn red, become swollen and painful. When purulent masses penetrate into the gum area, it may recede and loosen the tooth.
- If the inflammation is localized in the premolars and molars, the lip, wings of the nose and the bottom may swell.
- With a palatal purulent lesion, swelling of the lymph nodes in the submandibular region will be noticeable. Such inflammation is often provoked by carious processes in the roots of molars and premolars, and incisors. It can spread to the area of the pharynx, tongue and the entire oral mucosa, and with an increase in the volume of purulent exudate, any meal or attempt to speak can be very painful. When the tissue thins and the thin film breaks through, purulent masses enter the oral cavity, and then can reach the gastrointestinal tract, and this is fraught with other serious complications.
- Odontogenic inflammation of the maxillary sinus can affect the area of the eyes and eyelids, and swelling can spread to the cheekbones, temples and cheeks. Swelling of the eyelids leads to narrowing of the palpebral fissures.
- The inflammatory process in the parotid region often provokes damage to the salivary glands.
Attention: The abundance of purulent exudate is a fundamental factor in the appearance of intoxication of the body, as well as in the occurrence of phlegmon, and then an abscess. These conditions threaten not only the patient’s health, but also his life.
Diagnostic and treatment methods
In its acute form, it is much easier to recognize the disease than in its chronic form, since the symptoms are pronounced and not as erased as in the latter case.
When visiting a doctor, the patient may be offered the following diagnostic methods:
- laboratory research;
- magnetic resonance imaging (MRI);
- external examination of the patient, palpation and history taking;
- conducting ultrasound diagnostics;
- computed tomography (CT);
- X-ray examination;
- examination by highly specialized doctors (ophthalmologist, otolaryngologist, etc.).
Instructions for treating an inflammatory process in the jaw always involve an integrated approach. In the presence of an infectious agent, the use of antibacterial drugs is always required, and in the presence of purulent exudate, consultation with a facial surgeon is necessary.
If an opening is necessary, inflammation under the jaw or in any other area is eliminated by creating space for the drainage of pus, and then cleaning the area and administering antibiotics to prevent relapse.
At the time of therapy, the jaw is provided with complete rest. This point can be achieved by applying a sling-shaped bandage for 2-3 days or a special plate between the teeth.
The diet must be high in calories, and the food must be of a liquid consistency at the optimal temperature. In case of severe pain, painkillers are prescribed, the price of which can be either low or quite high.
Also in the treatment of pathology it is possible to use the following methods:
- physiotherapeutic procedures;
- compresses with bee venom;
- electrophoresis with medications containing iodine;
- paraffin therapy;
- use of traditional methods.
Maxillofacial inflammation requires an immediate visit to the doctor. The use of decoctions alone or self-medication can provoke serious complications, and even in the case of a later recovery, the disease will become chronic and thus ensure fairly frequent relapses for many years to come.
Do not forget that next to the jaw there are eyes, canals and maxillary sinuses, which communicate with the meninges. Damage to sensitive cells in this area is fatal, so you should take your health more seriously.
Source: https://Denta.help/hirurgicheskaya/vospalitelnye/vospalenie-chelyusti-396
The jaw hurts and clicks after prosthetics or dental treatment
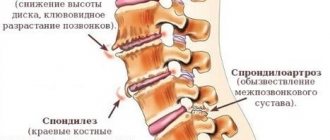
Dysfunction of the temporomandibular joint. The lower jaw is connected to the skull by two temporomandibular joints. Impairment of the function of these joints is possible after the installation of a denture, crown, bridge, any treatment or tooth extraction if this leads to malocclusion and/or damage to the temporomandibular joint. This is a typical complication after dental prosthetics. Read more about treating TMJ dysfunction here
Temporomandibular joint dysfunction
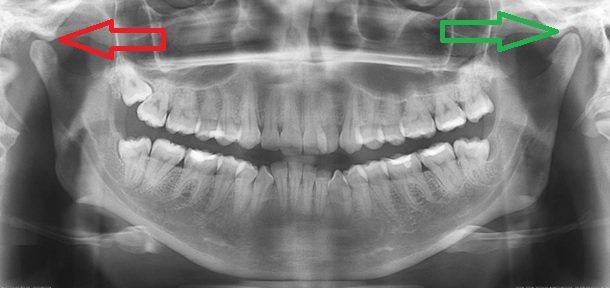
The green arrow indicates a healthy joint. The red arrow points to the joint that remains in the “open” position when the mouth is closed. This leads to wear and tear of the articular cartilage, pain and clicking when opening and closing the mouth. One of the reasons is the incorrect position of the upper right “eight” (tooth 1_8 lies horizontally).
How can we help you:
- Anti-inflammatory treatment will help relieve pain. If necessary, we inject anti-inflammatory medication directly into the lower jaw joint . This brings relief within a few minutes .
- Injection of botulinum toxin preparations (for example, Botox or Dysport) into spasmodic muscles. This is relevant in the case of an excessive increase in the tone of the masticatory muscles, if it is the muscles that are the “culprit” of dysfunction of the temporomandibular joint.
- Treatment by an osteopath. An osteopath works with the joints and muscles of the jaw using gentle manual techniques. This way you can solve a lot of problems that cannot be solved in classical dentistry. More about osteopathy
- Introduction of chondroprotectors (medicines for nutrition and restoration of cartilage) into the temporomandibular joint. Read more about cartilage restoration
The most common cause of facial pain is not the trigeminal nerve!
As we said earlier, many patients and, unfortunately, doctors believe that the most common and obvious cause of facial pain is trigeminal neuralgia.
It is also called trigeminal neuralgia. And treatment with carbamazepine (aka finlepsin) is prescribed - severe, often disrupting well-being, long-term and... useless. After all, an incorrect diagnosis and subsequent ineffective treatment lead to complete hopelessness, the desire to take any painkiller in uncontrolled quantities and disbelief in the possibility of pain relief. But in fact, trigeminal neuralgia is very rare - only 0.3% of people suffer from this severe and often painful disease.
However, in reality, the most common cause of chronic facial pain is dysfunction of the temporomandibular joint. This disease is at least 15 times more common than trigeminal neuralgia and has nothing to do with the trigeminal or any other nerve in the face.
Let's talk about what it is and what can also cause severe, frequent and long-term pain in the face.
SO WHAT IS TEMPOROMANDibular JOINT DYSFUNCTION?
The temporomandibular joint connects the lower jaw to the temporal bone and is therefore located immediately in front of the ear on each side. The joint allows the lower jaw to move up, down, forward and sideways - that is, the movements necessary for chewing food. And these movements become possible with the help of muscles - chewing, temporal and pterygoid.
Both the joint itself, and, in particular, the muscles surrounding it, have a huge number of pain nerve endings, so all these structures are very often the source of pain.
Today, the term “temporomandibular joint dysfunction” also refers to the pathology of the joint itself,
which, by the way, does not hurt so often,
and,
more importantly,
tension in the masticatory, temporal and pterygoid muscles
.
In the vast majority of cases, the cause of pain is myofascial pain syndrome in these muscles, which often develops even without pathology of the joint itself. With myofascial pain syndrome, pain can be felt not only in the area of the muscle itself, but also be reflected in distant areas, for example, in the ear, head, neck and even shoulders.
WHAT ARE THE SYMPTOMS?
- Facial pain, usually localized to the cheeks and jaw
- Fatigue, tension and discomfort in the face, feeling as if you have been chewing for a long time
- Pain when chewing
- Pain in or behind the ear
- Neck and shoulder pain
- Headache, usually in the temple area on one or both sides
- Sometimes you may hear a crunching or clicking noise when you open or close your mouth. This usually indicates a pathology of the temporomandibular joint itself, but may not be accompanied by pain.
SO MY EAR PAIN MAY NOT BE ACTUALLY CAUSED BY EAR PROBLEMS?
Yes, that is right. This disease was therefore first described by a Canadian ENT doctor when he was unsuccessfully trying to cure what he thought was otitis media.
It turned out that pain in the ear and behind the ear can be caused by problems with the temporomandibular joint and muscle tension in the masticatory group.
When the so-called myofascial pain syndrome forms in these muscles, that is, trigger points appear in tense and painful muscles, any movements in the jaw can cause pain not only in the face, but also in the temples, behind the ear, and even in the neck.
DO I UNDERSTAND CORRECTLY THAT EVEN THE NECK CAN HURT WITH TMJ DYSFUNCTION?
Yes, that's exactly it. As we have already said, with the development of myofascial pain syndrome in the masticatory muscles, pain can be felt not only in the face, but also in the neck and behind the ear. And this is exactly the example you can see in the video, which I will present a little later.
OK, WHY DOES THIS DISEASE ARISE AT ALL?
Nobody knows for sure. It is believed that various causes and even a combination of them can lead to the development of TMJ dysfunction. Let's discuss the most common of them:
- Bruxism. We have already said before that bruxism is the involuntary clenching of teeth during sleep, which is accompanied by grinding of teeth and morning fatigue in the face. The grinding noise is usually quite pronounced and can be heard by others. Imagine that the masseter muscle is one of the five strongest muscles in our body. Yes, yes, it may seem small and not the most significant to you, but it is so. The muscles of the masticatory group, when tense, can exert a load of 25 kilograms on the front teeth and 91 kilograms on the molars! Now let's think about why bruxism can lead to pain in the head and face. Of course, squeezing with such force can ultimately lead to tension and soreness in the chewing muscles and the development of myofascial pain syndrome. Many people also involuntarily clench their teeth during the day (daytime bruxism), especially when working hard and thinking about unpleasant things. This also needs to be paid attention to. And, of course, bruxism is extremely harmful to teeth, as it leads to high abrasion, as well as damage to crowns and expensive implants.
- Emotional disorders. A high level of anxiety is one of the most common causes of muscle tension in the face and the appearance of their soreness, because clenching your teeth and pulling your shoulders up is an involuntary muscle reaction with which the body responds to stress
- TMJ dysfunction may coexist with other chronic pain, most commonly chronic migraine.
- Injuries, poor posture and head position
- And what is most interesting, it has recently become known that malocclusion has very little significance for the development of TMJ dysfunction and facial pain.
- And of course, if you are undergoing long-term orthodontic treatment at the dentist, pre-existing tension in the chewing muscles can intensify and cause severe pain in the face.
HOW SHOULD A DOCTOR EXAMINATE MY JOINT
So, if you are worried about pain in the face, ear, neck or headache, your doctor should always evaluate the condition of the temporomandibular joint and the muscles surrounding it.
He will ask you to open your mouth as much as possible, see how well you can do this, listen to whether this causes grinding or crunching in the joint, and also palpate the joint through the external auditory canal.
And, most importantly, the doctor must palpate (feel) the temporal and masseter muscles to assess their level of tension, soreness and the presence of myofascial trigger points. And if you feel pain not in your face, but, for example, behind the ear or in the temple, when you find these points, your pain will immediately be reproduced, and the diagnosis will become obvious.
AND WHAT SHOULD I DO NOW - HOW TO REDUCE THE PAIN?
Acute pain can be reduced by taking various over-the-counter painkillers, applying heat or cold, avoiding solid foods and tall burgers :-), and avoiding opening your mouth too much for a while.
However, in most cases the pain is chronic and lasts for a long time. In this case, the main role is played, of course, not by inflammation, but by muscle tension. In this situation, you need to learn stress management techniques and treat anxiety disorders to reduce the likelihood of nighttime and especially daytime bruxism, and also be careful not to clench your teeth.
To treat nocturnal bruxism, dentists may suggest custom splints to wear at night, but experience shows that many people refuse to wear them due to discomfort and aesthetic reasons.
In recent years, botulinum toxin type A has been used to treat facial pain associated with muscle tension in the masticatory group, regardless of whether you have bruxism or not. Botox effectively relaxes tense muscles in just 2-3 weeks, and its effect lasts several months.
In addition, having extensive experience using Botox in the treatment of chronic migraines, we understand that the drug not only relaxes muscles, but also has a healing effect on chronic pain.
The drug can be administered to treat active pain associated with dysfunction of the temporomandibular joint, to treat bruxism, as well as prophylactically in case of tension in the masticatory muscles, if you are undergoing orthodontic treatment or maxillofacial surgery. This will make the dentist’s work easier and remove unnecessary stress from the joint.
As we said above, in every second patient with chronic migraine we also find pain and tension in the masticatory muscles. So if you're considering Botox to treat chronic migraines, ask your doctor about injecting at least a small dose into the muscles of mastication.
I also have a video on my blog about how we administer Botox to treat chronic facial pain.
And, as always, send in questions!
Source: https://zen.yandex.ru/media/id/5a5f25b92480908826c2703c/5bc0575c782b5d00aed4f38b
Sinusitis, maxillary sinus cyst, loss of sense of smell after visiting the dentist
The roots of the teeth of the upper jaw can normally be adjacent to the maxillary (maxillary) sinuses of the nose and even survive in them . Sinusitis, maxillary sinus cyst and loss of smell are possible when infection or filling material penetrates from the teeth into the paranasal sinuses. Unfortunately, this is not uncommon. Moreover, some cases of persistently recurrent sinusitis are associated with infection penetrating from the roots of the teeth . In this case, a possible symptom is a strong unpleasant odor from the nose and mouth.
Odontogenic sinusitis after treatment by a dentist
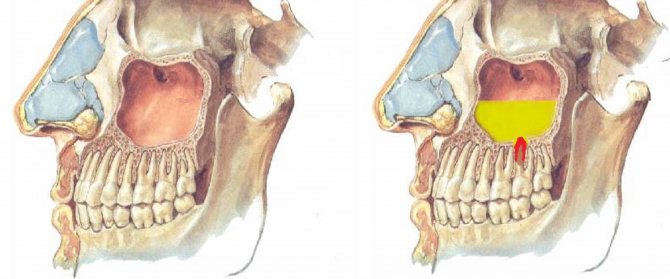
Odontogenic sinusitis (scheme). Teeth and maxillary sinus. On the left is the norm. On the right – the root of the “seven” (tooth 2_7) is destroyed, inflammation around the destroyed root, pus in the maxillary sinus.
Filling material in the maxillary sinus and sinusitis after filling the “six” canals (tooth 2_6). Pain in the left side of the face after visiting the dentist.
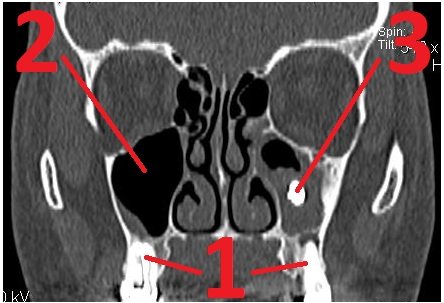
1 – roots of teeth, 2 – normal, air in the right maxillary sinus (front view, the air looks black in the picture), 3 – in the left maxillary sinus there is a fragment of filling material surrounded by an inflammatory shaft. The patient had been mistakenly receiving treatment for trigeminal neuralgia for a long time.
Cysts of the maxillary (maxillary) sinuses in diseases of the roots of the teeth.
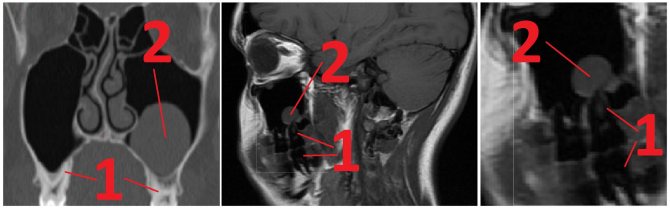
1 – roots of the teeth, 2 – cysts of the maxillary sinuses, growing from the roots of the teeth (cysts are round “bubbles”, they look gray in the picture).
How can we help you:
- Let's find the source of pain after dental treatment;
- We will treat inflammatory processes, sinusitis, sinusitis and neurological complications; if necessary, your health will be taken care of jointly by a neurologist and an ENT doctor. Treatment of sinusitis without puncture