Meningococcemia (meningococcal sepsis) is a generalized form of meningococcal infection. The disease is characterized by the entry of meningococci from the primary inflammatory focus into the bloodstream and their rapid reproduction. With the massive death of bacteria, endotoxins are released, the effect of which on the internal organs and systems of the body determines the clinical picture of the disease.
Most often, meningococcemia in children develops between the ages of 3 months and 1 year. Among all generalized forms of meningococcal infection, meningococcemia ranges from 35 to 43%.
Rice. 1. The photo shows meningococcemia (meningococcal sepsis).
How does meningococcemia develop?
From the lesion with macrophages in which viable bacteria are preserved, or through the lymphatic tract, meningococci enter the blood. Meningococcal sepsis or meningococcemia develops. The spread of infection is facilitated by many factors: the virulence of pathogens, the massiveness of the infectious dose, the state of the body’s immune system, etc. During the period of meningococcemia, foci of secondary lesions and immunological reactions are formed. The disease progresses rapidly, unpredictably and is always very difficult.
The massive death of meningococci and the release of endotoxin is accompanied by toxic reactions. The acid-base state, hemocoagulation, water-electrolyte balance, the function of external and tissue respiration, and the activity of the sympathetic-adrenal system are disrupted.
Endotoxin of pathogens affects blood vessels, stasis and multiple hemorrhages are formed in the skin, mucous membranes and internal organs. Intravascular coagulation syndrome (DIC) develops. Hemorrhage into the adrenal glands leads to the development of Waterhouse-Friderichsen syndrome and infectious-toxic shock. Internal organs are affected, dysfunction of which leads to the death of the patient.
Rice. 2. The photo shows meningococcemia in children. Extensive hemorrhages are visible on the skin. The photo on the left shows skin necrosis.
The first symptoms of meningitis in children and adults: what does the rash look like?
Meningitis is a fairly serious disease. In order for the prognosis of this disease to be favorable, it is necessary to begin treatment in a timely manner, otherwise the consequences will be severe.
Children are especially susceptible to this disease, so parents need to know all the signs of meningitis so as not to miss the onset of such a terrible pathology.
Meningitis
Meningitis is a disease that affects the membranes of the membranes of the brain and spinal cord, while the cells of the organ itself are not damaged. The pathological process occurs outside the meninges. There are two types of this disease, bacterial and viral.
Most often, meningitis is viral in nature, occurring due to advanced and untreated viral infections. Bacterial types of this disease are much less common, but damage the brain more seriously and its consequences are more severe.
Almost every year, outbreaks of viral meningitis occur in certain areas, affecting in most cases children and young people, but in this case the disease cannot be called fatal, since with timely and adequate treatment it recedes.
You can get meningitis for various reasons, but there are risk factors that can affect the body's protective functions, weakening them.
Risk factors:
- Frequent drinking of alcohol.
- Smoking.
- Hypothermia.
- Insolation.
This disease has its own classification and differs by type. Each type of this disease requires a special approach to therapy. In addition, meningitis can be primary and occur independently, or secondary, that is, develop against the background of an existing infection.
Types of meningitis:
- Staphylococcal.
- Tuberculous.
- Enteroviral.
- Herpes.
- Fungal.
Many people ignore diseases of viral origin, believing that they do not pose a danger, but if such ailments are not treated, they can cause complications in the form of meningitis.
Rash due to meningitis in children and adults
The presence of a rash during meningitis allows you to quickly and accurately establish a diagnosis. Young children cannot describe their condition, which makes diagnosis difficult, however, when a rash appears on the skin, the clinical picture becomes clear. In both children and adults, a skin rash usually appears on the first day of illness, but there are situations when such a symptom appears two days after the onset of the disease.
Rashes due to meningitis indicate that it is necessary immediately , especially since the area of such lesions is increasing at enormous speed. The size and appearance of these skin manifestations indicate the type of meningitis pathogen. The wider the affected area and the brighter the rash, the more severe and dangerous the pathological process.
Typically, skin rashes appear with bacterial meningitis ; the viral nature of this disease is often not accompanied by a rash.
Signs and symptoms of meningococcemia
The incubation period for meningococcemia ranges from 5 to 6 days. Fluctuations range from 1 to 10 days. The onset of the disease is most often acute and sudden. The generalization of the process is indicated by the deteriorating general condition of the patient, a significant increase in body temperature, increasing headache, increasing pallor of the skin, tachycardia and shortness of breath. Muscle and joint pains, rashes on the skin and hemorrhages on the mucous membranes appear.
A rash with meningococcemia appears in the first hours of the disease. Hemorrhagic elements can be enormous in size and accompanied by skin necrosis. Along with the hemorrhagic rash, hemorrhages are observed in the conjunctiva of the eyes and sclera, mucous membranes of the nose and pharynx, and internal organs. Sometimes gastric, nasal and uterine micro- and macrobleedings and subarachnoid hemorrhages occur.
An extremely severe form of meningococcemia is complicated by damage to the heart and its membranes, thrombosis of large vessels, infectious-toxic shock, hemorrhage in the adrenal glands (Waterhouse-Friderichsen syndrome). Violations of the functions of vital organs lead to the death of the patient.
In some cases, there is a milder course of the disease and atypical meningococcemia, which occurs without skin rashes. In this case, the clinical picture of the disease is dominated by symptoms of damage to one or another organ.
Very rarely, meningococcemia can become chronic or recurrent. The disease occurs with low-grade fever, often with a rash and joint damage. The disease lasts for months and even years. Months after the onset of the disease, the patient may develop endocarditis and meningitis. Periods of remission are characterized by the disappearance of the rash and normalization of body temperature. With chronic meningococcemia, erythema nodosum, subacute meningococcal endocarditis and nephritis can develop.
Rice. 3. The photo shows a chronic form of meningococcemia.
Diagnostics
The doctor interviews and examines the patient. A meningitis rash is not always immediately apparent on physical examination, no matter what it looks like. More often, the doctor focuses on symptoms such as intense, excruciating pain in the head area, repeated vomiting attacks, forced position of the torso and other meningeal signs, confusion and disturbance of higher mental functions.
The clinical picture contains signs: hyperesthesia (increased sensitivity to light, tactile, sound stimuli), psychomotor agitation or lethargy, apathy, lethargy, pain in the joints and muscles. Patients often experience a significant decrease in blood pressure and heart rhythm disturbances (tachycardia).
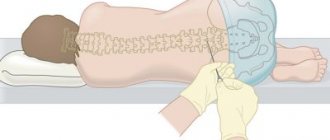
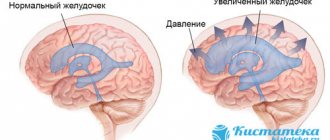
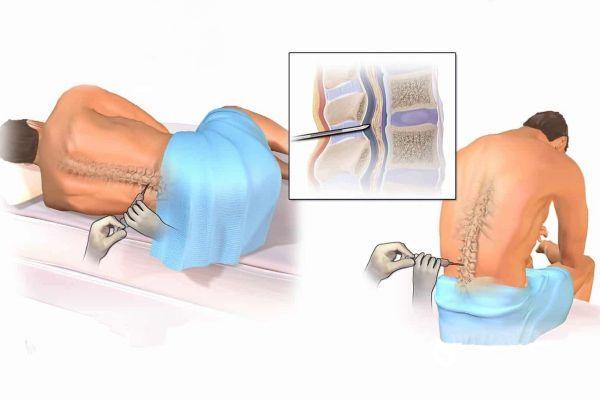
Laboratory tests include a coagulation test, which shows blood clotting characteristics. The main method of laboratory diagnosis is lumbar puncture, which allows you to confirm the diagnosis and identify the type of infectious agent.
The appearance of rashes in the face, eyelids, and upper torso in the early stages of meningitis is considered an unfavorable prognostic sign.
A poor prognosis is also associated with thrombocytopenia (low platelet concentration in the blood). Differential diagnosis is carried out in relation to diseases for which the appearance of skin rashes and similar symptoms is typical - for example, measles and scarlet fever, hemorrhagic vasculitis, mononucleosis of infectious origin.
Rash due to meningococcal infection
Under the influence of endotoxin, which is released during the mass death of meningococci, the walls of arteries and arterioles are damaged and their permeability increases. Intravascular coagulation syndrome (DIC) develops. The blood clotting system starts. Blood clots form in the blood vessels, which significantly impedes blood flow. As a compensatory mechanism, the body activates the anticoagulant system. The blood begins to thin out, causing blood clots to form in the patient’s body and bleeding to develop.
The rash due to meningococcal infection has the character of hemorrhages (bleeds), which appear on the skin and internal organs and have different sizes. Hemorrhages in the adrenal glands are especially dangerous. The developed Waterhouse-Friderichsen syndrome and dysfunction of vital organs lead to the death of the patient.
Rice. 4. The photo shows hemorrhages in the peritoneum (left) and the mucous membrane of the tongue (right).
A rash with meningococcal sepsis appears already in the first hours of the disease. Initially on the distal limbs and then spreads throughout the body.
Its signs:
- Petechiae are pinpoint hemorrhages in the skin and mucous membranes.
- Ecchymoses are small hemorrhages (from 3 mm to 1 cm in diameter).
- Bruises are large hemorrhages.
With significant skin lesions, necrosis appears - difficult-to-heal ulcers, in the place of which keloid scars remain during healing.
Rice. 5. The rash due to meningococcal infection has a purplish-red color and does not disappear with pressure.
The elements of the rash are dense to the touch, rise above the skin, and have a star-shaped shape. The rash of meningococcemia sometimes appears on the face and ears. Rash-free skin is pale in color. Often, before the rash appears on the skin, hemorrhages appear on the mucous membranes of the oral cavity, conjunctiva and sclera. When the choroid of the eyeball becomes inflamed, the iris becomes rusty in color.
The more severe the meningococcemia, the larger the area of bruising. Huge rashes are always accompanied by the development of infectious-toxic shock.
As the patient recovers, petechiae and ecchymoses become pigmented. A small rash goes away within 3 days, a large rash within 7-10 days. Large bruises become necrotic and crusty. After the crusts are rejected, tissue defects of varying depth remain, healing with a scar. Damage to the skin of the tip of the nose, ears and phalanges with a finger occurs as dry gangrene.
Meningitis rash: you need to be able to recognize it in time
Meningitis is an infectious disease.
When microorganisms of a pathogenic group enter the tissue of the pia mater or the cerebrospinal fluid, an inflammatory process develops, which is accompanied by a number of characteristic symptoms.
One of them is a rash on the body. It indicates blood poisoning and is generalized. A rash with meningitis is evidence of the spread of infection throughout the body.
What is the danger of the disease
Airborne infection poses a threat to the health and life of not only the sick person. It can spread among a group of contact persons with lightning speed, especially if these are young children.
It is especially dangerous when the source of infection is an apparently healthy carrier who himself does not know about his danger to others.
How to protect yourself from such a disease
Through the efforts of doctors and pharmacists, a vaccine was invented to immunize healthy individuals. However, it is not multicomponent and has an effect only if the vaccinated person’s body receives exactly the pathogen to which it has developed immunity. This means that the effectiveness of vaccination can only be ensured if the pathogen is known.
The appearance of a meningeal rash on the body, whether it is a primary or secondary sign of meningitis, is a dangerous signal. An emergency medical team must be called immediately. One of the determining factors for the effectiveness of treatment is its efficiency and timely initiation.
Treatment of the disease is labor-intensive and multicomponent. A professional approach to its appointment is required. Accurate adherence to the doctor’s instructions will allow you to avoid possible negative consequences and save the patient’s life.
Source: https://nevrology.net/sindromy-i-zabolevaniya/infektsionnye/syp-pri-meningite.html
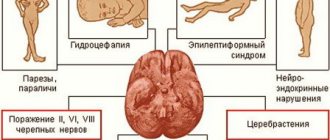
Signs and symptoms of meningococcal infection in heart disease
Meningococcal toxin contains an allergenic substance, which leads to pronounced sensitization of the body from the moment it colonizes the nasopharynx. The formed immune complexes settle on the walls of blood vessels, increasing the damaging effect (Schwartzman-Sanarelli syndrome). Sensitization of the body underlies the development of arthritis, nephritis, pericarditis, episcleritis and vasculitis.
Meningococcal carditis accounts for half of all cases of damage to internal organs due to meningococcal infection. Toxic damage to the heart affects the endocardium, pericardium and myocardium. The contractility of the heart muscle decreases, and the heart rate increases. Hemorrhages into the heart muscle, tricuspid valve and subendocardial space lead to the development of cardiac weakness, which is often the cause of death of the patient.
When infection enters the pericardium, purulent pericarditis develops. On auscultation, a pericardial friction rub is heard.
Elderly people often develop myocardiosclerosis after an illness.
Rice. 13. The photo shows hemorrhages in the endocardium (left) and pericardium (right) with meningococcal sepsis.
Signs and symptoms of meningococcal infection in the lungs
When the vessels of the lung tissue are damaged, a specific inflammation develops - meningococcal pneumonia. The disease develops against the background of severe intoxication.
The liquid sweats into the lumen of the alveoli, innervation is disrupted, the level of affinity of hemoglobin for oxygen decreases, respiratory failure and pulmonary edema develop, and the pleura may be affected. Initially, there is a focal lesion, but over time the infection spreads to the entire lobe of the lung. When you cough, a large amount of sputum is produced.
Recovery from meningococcal pneumonia is slow. The patient has been bothered by a cough for a long time, and asthenia develops.
Rare forms of meningococcemia
Damage to the paranasal sinuses
Inflammation of the paranasal sinuses occurs with meningococcal nasopharyngitis and with a generalized form of infection.
Urethral lesion
Meningococcal nasopharyngitis can cause specific urethritis in homosexuals during orogenital contact.
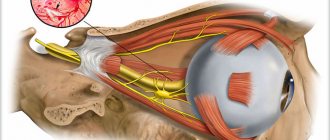
Meningococcal iridocyclitis and uveitis
With meningococcal sepsis, the choroid of the eyes can be affected (uveitis). The lesion is often bilateral. Vitreous opacification is noted. It detaches from the retina. In places of peeling, rough adhesions form. Visual acuity decreases. secondary glaucoma and cataracts develop .
With inflammation of the ciliary body and iris (iridocyclitis), severe pain appears already on the first day, visual acuity sharply decreases, even leading to blindness. The iris protrudes forward and takes on a rusty tint. Intraocular pressure decreases.
Involvement of all tissues of the eyeball in the inflammatory process (panophthalmitis) can result in complete blindness.
Rice. 15. Meningococcal uveitis (left) and iridocyclitis (right).
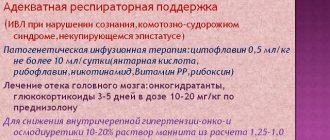
Fulminant form of meningococcemia
The fulminant form of meningococcemia or Waterhouse-Friderichsen syndrome is an acute sepsis accompanied by multiple hemorrhages in the adrenal glands. The disease occurs in 10 - 20% of cases of generalized meningococcal infection and is the most unfavorable form in terms of prognosis. The mortality rate ranges from 80 to 100%.
Signs and symptoms of fulminant meningococcemia
With the disease, multiple extensive hemorrhages into the skin and the rapid development of bacterial shock are noted. With hemorrhages in the adrenal glands, a deficiency of gluco and mineralocorticoids occurs, as a result of which disturbances in the metabolism and function of a number of organs and systems quickly occur in the patient’s body. The developed crisis (acute adrenal insufficiency) proceeds like Addison's disease and often ends in death.
The fulminant form of meningococcemia occurs suddenly. Body temperature rises significantly - up to 40°C, severe headache and nausea appear. The patient becomes lethargic. Large areas of hemorrhage appear on the skin.
Blood pressure drops, tachycardia appears, the pulse becomes thready, breathing quickens, and diuresis decreases. The patient falls into a state of deep sleep (stupor). Coma develops.
At what temperature should you call an ambulance in a child?
If a child has a common cold, the local pediatrician will prescribe treatment and the illness will soon go away. However, high fever in children often accompanies other illnesses. And in some cases you need to immediately call an ambulance.
— Against the background of a high temperature, the child begins to vomit. Theoretically, this could indicate both ordinary food poisoning and the reaction of the child’s nervous system to fever (a spasm of the esophageal sphincter occurs). However, he definitely needs urgent help! After all, vomiting sometimes indicates serious meningitis or a serious intestinal infection, in which dehydration quickly develops.
— The child developed a rash of any nature. Purple spots or a rash in the form of bruises that appear right before your eyes should be especially alarming. These are signs of meningococcemia, a dangerous infection. The child urgently needs antibiotics!
- Headache, lethargy, lethargy, drowsiness in a child with a temperature above 38.5 C is a very serious symptom, indicating a severe infection. Doctors from the ambulance team will provide first aid and take the child to the hospital.
— Fever in children can be brought down with ibuprofen or paracetamol in an age-appropriate dosage, but if you notice that the drugs do not work and the child’s temperature does not go down, call an ambulance.
Infectious-toxic shock with meningococcemia
Infectious-toxic shock develops in fulminant forms of meningococcal infection and is its most dangerous complication.
Infectious-toxic shock is based on bacterial intoxication. As a result of the massive death of meningococci, endotoxins are released, which damage blood vessels and lead to paralysis of small vessels. They expand, the blood in the vascular bed is redistributed. A decrease in the volume of circulating blood leads to disruption of microcirculation and a decrease in its perfusion to organs and tissues. Intravascular coagulation syndrome develops. Redox processes are disrupted. The function of vital organs decreases. Blood pressure drops rapidly.
The administration of penicillin leads to massive death of meningococci and the release of endotoxin, which aggravates the development of shock and accelerates the death of the patient. In this case, instead of penicillin, chloramphenicol should be administered. After the patient has recovered from shock, the administration of penicillin can be continued.
The development of infectious shock can be judged by the following signs:
- rapid spread of the rash and its appearance on the face and mucous membranes,
- decrease in blood pressure, increase in tachycardia and shortness of breath,
- rapid increase in disturbance of consciousness,
- development of cyanosis and hyperhidrosis,
- a decrease in leukocytes and neutrophils in the peripheral blood, the appearance of eosinophilic granulocytes, a slowdown in ESR,
- decreased protein, severe acidosis, decreased blood sugar.
The body temperature of patients rapidly drops to normal levels. Excitement is noted. Urine stops coming out. Prostration develops. Convulsions appear. The patient's death occurs.
Rice. 18. The photo shows meningococcal infection in an adult.