Aggravation
Aggravation is an exaggeration by the subject of the described severity of symptoms that actually exist or are subjectively felt.
Aggravation can be a consciously determined activity or have a subconscious nature of occurrence.
The reasons for the aggravation of painful symptoms can be determined both by the true presence of the disease and by the personal and motivational characteristics of the person.
Behavior is considered aggravative when a person contributes to the deterioration of his own health or prolongs the period of illness (active form, when non-compliance with doctor’s recommendations, self-mutilation is possible) or exaggerates existing symptoms (passive form, when the number of complaints increases).
Pathological malingering is manifested not only by the subject’s intensification of the symptoms of the existing disease, but also by downplaying the effect of the treatment provided, which may not coincide with objective indicators of improvement. This condition is considered a mental disorder and requires appropriate clinical diagnosis and psychotherapy.
Unlike conscious simulation, aggravation can act as a symptom or characteristic of the degree of progression of psychopathology.
What is aggravation?
The causes of aggravation of existing symptoms are mental disorders or deviations that accompany hypochondriacal and hysterical accentuations, as well as those inherent in older people with significant mental changes.
Also, this behavior can develop as a result of chronic psychological trauma (reminder by others of a defect, over-concern), and have a neurotic nature.
The difficulty in diagnosing this disorder lies in its initial and superficial similarity with simulation, however, simulation always has a selfish motivation, while aggravative actions are an unconscious manifestation of the hidden desires of the individual and contribute to receiving attention or care.
In the course of establishing the authenticity of mental status and forensic psychiatric examination, doctors and investigators are faced with such phenomena as simulation and aggravation.
To determine, coordinate and adjust further actions, as well as decide the fate of the subject, it is very important to distinguish one from the other.
Thus, simulation is a deliberate, conscious, often planned act of behavior aimed at deliberately simulating non-existent symptoms and manifestations of mental or somatic disorders, the purpose of which is most often to avoid judicial punishment.
There may be an intensification of aggravative behavior, both during the investigation and at critical moments of decisions on the future fate of those already convicted.
More often during simulation, simulated behavior with a description of anamnestic indications is used than directly acting out painful symptoms.
Determining the truth of the picture of complaints comes down to clinical research, observation of the subject and psychological examination.
Simulation and aggravation are different processes, although simulation against the background of the presence of pathological disorders of the psychiatric register is aggravation.
Types of aggravation. It can be subconscious (inherent in a sick person), intentional (in order to obtain a benefit or a necessary outcome of events) and pathological (in mentally ill people). The subconscious has a person’s desire to receive sympathy and support.
It is often found in patients with a hysterical, hypochondriacal and psychopathic type of accentuation, anxious and suspicious individuals who monitor their health parameters very carefully and any illness is immediately considered serious, painful sensations are exaggerated.
https://www.youtube.com/watch?v=NkHLEpJaupQ
The reasons for aggravation for suggestible people are in reading medical literature and attributing diseases to themselves, in careless statements by a doctor or any representative of the medical staff.
Deliberate aggravation is motivated by profit.
It is divided into active (when the patient himself delays recovery or independently worsens his condition) and passive (exaggeration of symptoms, complaints about other phenomena not characteristic of this disease) forms.
When deliberately exaggerating the symptoms of a disease, aggravative behavior is criminally punishable if used for illegal purposes (receiving insurance payments, exemption from the army, etc.).
When the need arises to establish the fact of aggravation, the doctor or bailiff primarily focuses on objective data from examining the patient, obtaining the necessary tests, and not on his subjective descriptions of his well-being.
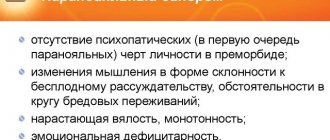
Pathological aggravation is considered from the perspective of aggravation of mental disorders.
Aggravation of mental disorders
Pathological aggravation implies an exaggeration of the symptoms of somatic and psycho-emotional illnesses in mentally ill people. It is a fairly common phenomenon in forensic psychiatric activities, occurring in the form of deliberate complaints about symptoms that were previously inherent and characterized the disease, but have now been stopped.
Psychiatric aggravation is divided into three main types of manifestation: meta-aggravation, super-aggravation and dissimulation. With meta-aggravation, a person deliberately seeks to prolong the most acute phase of the disease (depression, build-up of affective arousal).
Over-aggravation implies complaints about symptoms that are excluded in the case of a really diagnosable disease (intellectual-mnestic disorders in schizophrenia).
Dissimulation is the concealment of the disease or its manifestations, which are determined by the disease and the characteristics of its course (with exacerbation of schizophrenia and psychotic states, a person is not able to assess his condition himself, and the motives dictated by the disease require concealment of all symptoms).
Pathological aggravation carries symptoms that are preserved in memory from actually previously existing or retained residual manifestations of mental disorders.
Most often it occurs when mental illnesses are based on an organic nature (head injuries, vascular and hereditary diseases, mental retardation).
The most common exaggeration of intellectual failure, problems in the mnestic sphere, headaches, loss of orientation in society, and depressive manifestations.
Aggravation becomes a habitual form of behavioral patterns when the first aggravative behavior led to a successful resolution of the situation or acts as a standard reaction of a changed personality in critical situations.
This response mechanism is consolidated and may further reflect the depth and severity of mental damage (thus, with a decrease in the intellectual-mnestic sphere, aggravative behavior begins to look more and more grotesque and ridiculous).
The form and degree of manifestation of aggravation serves as a way to assess the severity of mental disorders, the degree and rate of progression of the disease. The more primitive, crude, and absurd the manifestations of aggravation, the greater the degree of mental disorder we can speak of.
Aggravation therapy includes drug therapy for the underlying disease and psychotherapy. The main goal of psychotherapy will be to search for hidden motives, human needs and bring them into the realm of consciousness, and at subsequent stages, search for various socially acceptable, relevant and appropriate ways to satisfy the identified requests.
Author : Practical psychologist Vedmesh N.A.
Speaker of the Medical-Psychological
Source: https://psihomed.com/aggravatsiya/
Simulation or aggravation?
Note 2
Aggravation and simulation are phenomena that are similar in their manifestations, but very different in the reasons for their formation.
Simulation is the deliberate reproduction of certain signs of a disease.
Absolutely healthy people with a specific (selfish) goal or people who suffer from mental disorders can simulate. The key difference between malingerers is their rather attentive attitude towards themselves and their own health; they never do something like that that could seriously harm it.
Note 3
Aggravation is an unintentional exaggeration of the symptoms of a disease that a person experiences or thinks that he is experiencing.
Aggravants may deliberately harm themselves, not take medicine, or refuse to consent to treatment in order to worsen their own condition.
The key difference between malingerers and aggravants is their attitude to their own health and condition. The first ones know for sure that they are lying, and they do not have this disorder (at the same time, they may have other illnesses that they do not complain about) and they always have a benefit or goal from such behavior
Aggravation: symptoms and methods of correcting this condition – Suppressed
This is its fundamental difference from simulation, when the disease is completely absent and the patient is not one.
A striking example of aggravation can be a child showing an abrasion on his knee with such sorrowful emotions, as if we were talking about the end of his life. In this case, everything is clear: the child wants to be pitied.
A typical portrait of an aggravant
What does an adult aggravant want? About the same. After all, most often people who are lonely and helpless in life, who have no one to rely on, come to see a doctor with such greatly exaggerated complaints. Or having a family, but not finding support in it.
The portrait of a typical representative of this category in everyday life is as follows. This is a middle-aged woman with an unfulfilled destiny, usually childless. She is burdened with numerous problems with work and is ready to “cry into her vest” to the first person she manages to talk to.
https://www.youtube.com/watch?v=MaWq_yvD3uw
It is extremely difficult to get rid of such a person, who is in no hurry to shut up and always finds new reasons to hold someone else’s attention for at least a few more minutes.
The face is very characteristic. These are sharpened features, mournfully pursed lips with downturned corners of the mouth and equally mournful, pleadingly waiting and at the same time empty eyes, as if for her everything had long been decided and finished. Moreover, it is not in her favor.
The manifestation of emotions in the course of presenting endless complaints or detailing one of them looks at the same time as carefully restrained, stingy and bashful, but at the same time methodical and unhurried. Even the pauses between phrases look like a continuation of complaints.
Behavior in a neuropsychiatrist's office is not very different from behavior in everyday life and leaves the impression that the patient has nowhere else to go and that she is ready to aggravate the rest of her life in the doctor's office.
Male aggravants look approximately the same and adhere to approximately the same line of behavior. Behavior dictated by the characteristics of a certain mentality.
Variety of reasons and types
Actively contributing to the deterioration of one’s own health, or taking measures to delay recovery are classified as active aggravation behavior, while exaggerating the severity of the condition and the significance of individual symptoms is regarded as passive aggravation.
By type, aggravation disorders are divided into:
- subconscious;
- intentional;
- pathological.
- The reasons for their occurrence fully or partially correspond to the category of disorder.
- If the subconscious type is based on the existence of an actual somatic disease, then the intentional one is a certain line of behavior that implies gaining benefit or giving current events the desired outcome.
- Pathological exaggeration of the severity of one’s condition is characteristic of mentally ill people or persons with mental states approaching psychopathology. That is, those suffering:
Drawing a strict line between subconscious and pathological aggravation is as difficult as assessing whether a patient is truly ill. Because the subconscious motivation in both options is the same - attracting attention, receiving sympathy and moral support.
On the aggravation of psychological and psychiatric disorders
And whoever searches will definitely find it. The next question is: what did self-inquiry give?
In search of an answer to this question, medical literature is methodically studied, television programs devoted to health are watched, or advice is sought from “those who know the truth” - fortune tellers and psychics. The information obtained contributes to even greater confidence in the seriousness of the existing symptom and the inevitable fatal outcome.
Conducted medical studies do not convince the patient of the insignificance of his disorder; on the contrary, they lead to the conviction that doctors are hiding something from him. Hence the insistence of demands to repeat the study, and to repeat it as thoroughly as possible.
Aggravations in psychiatric disorders are the conviction of a patient with a proven stable mental disorder in the mortal danger lurking behind the most harmless symptom. Thus, diarrhea repeated twice in a row can be regarded as a sign that, following the eruption of intestinal contents from the anus, the intestines will turn out, and then the entire body.
In psychiatric diseases, the patient’s attention can either be stubbornly focused on any one particularly disturbing symptom, or fixated on successively occurring conditions. The second category is more typical for elderly and senile people.
Aggravations in psychiatric disorders are divided into:
- meta-aggravation;
- super-aggravation;
- dissimulation.
The first option involves deliberately delaying the most acute stage of the disease, the second - complaints about symptoms that cannot exist in principle with a truly established disease.
Dissimulation is said to occur when there is an attempt to hide individual symptoms or the fact of exacerbation of psychopathology for one reason or another dictated by the disease.
To make a diagnosis
Including EEG, radiography with examination of cerebral vessels and other methods that allow assessing the level of cerebral blood supply.
If there is a pathological case, the patient is examined for mental disorder. In the case of a crime before the law, a forensic medical examination is carried out, and if necessary, the examination is carried out in a hospital setting. If the fact of pathological aggravation is identified and proven, the person is recognized as not responsible for his actions.
General approach to treatment
To apply the most rational and most gentle method of therapy, the type of aggravation disorder is taken into account.
- hypnotherapy;
- auto-training;
- relaxation therapy and the like.
If necessary, drug therapy is prescribed, including the use of targeted and general action drugs:
- vasodilators;
- sedatives;
- nootropic;
- general strengthening.
- It is rational to use exercise therapy, massage and similar methods that heal not only the patient’s psyche, but also his entire body.
- Pathological aggravations that have a psychiatric basis are treated by doctors of the appropriate profile.
About the consequences
Considering the thin line separating a neurotic disorder from a serious mental pathology, which often develops into a psychiatric one, relatives and friends should draw the patient’s attention to the fact of increasingly frequent cases of aggravation. And then gently encourage him to take measures to eliminate the causes that cause it. Measures taken together with the patient.
Measures that do not allow the knot of fears and life problems to transmit every day the increasingly thinning intangible structure called the will to live.
The concepts of “simulation”, “aggravation” and “dissimulation”.
The famous Russian psychiatrist, one of the founders of Soviet psychiatry, P.B. Gannushkin wrote: “Mental illness is associated with the state of the whole organism, with the innate constitution of the individual, with the state of his metabolism, with the functioning of the endocrine system, and finally, with the state of the nervous system... The brain is only the main arena in which all the action is played out and unfolds.” .
The causes of most mental illnesses are still largely unknown. It is also unclear the relationship between heredity, internally determined characteristics of the body and environmental hazards in their origin.
This situation creates the preconditions for the possibility of simulation* of mental disorders as one of the forms of protective behavior during problematic periods of people’s lives, one of the motives of whose behavior may be an attempt to avoid criminal liability for a crime committed at any stage of procedural actions. Emerging life problems significantly activate the defensive tendencies of the individual.
Simulation of mental disorders is an urgent ethical and legal problem in forensic psychiatry. The diagnosis of any mental disorder always carries a negative socio-ethical load. However, when used in a number of forensic psychiatric examination cases, it can help avoid criminal liability. For this reason, diagnosing the state of mental health of subjects of judicial investigation and civil proceedings always presents certain difficulties. The trend towards an increase in feigning behavior among persons brought to criminal liability is steadily growing.
Diagnosis of the state of mental health of subjects of judicial investigation and civil proceedings is a complex problem in forensic psychiatry. In SPE practice, simulation occurs in 2.0-3.5% of all cases of examination of offenders, and in women it is 2 times less common than in men. Simulation is typical for persons with repeated offenses, socially and pedagogically neglected, and those who have been isolated for a long time in a specific microenvironment.
* - according to S.I. Ozhegov’s explanatory dictionary of the Russian language, the word “simulate” means - by pretending, to create a false impression of the presence of something.
Feigning a mental disorder is behavior that pursues a specific goal - to depict or artificially induce (for example, with the help of medications) non-existent mental disorders. This is a deliberate, feigned behavior consisting of depicting non-existent signs of a mental disorder, committed for selfish purposes in the hope of avoiding punishment.
The trend towards an increase in feigning behavior among persons brought to criminal liability is steadily growing. More often this applies to people under investigation, less often to convicted people. The reasons (goals) for simulation in these cases are as follows:
§ change the course of the investigation and delay the trial;
§ obtain the necessary information;
§ predict investigative measures;
§ impose your version of the act on the investigation;
§ achieve a referral to the EP;
§ achieve benefits available only to mentally ill people;
§ mitigate the severity of the consequences of criminal actions;
§ create the impression that the crime was caused by painful motives and avoid criminal liability.
Among the malingerers, people with “certain psychiatric experience” predominate, have previously undergone a forensic psychiatric examination (FPE), and are aware of the grounds and practice of prescribing and conducting expert research. More often, these are socially and pedagogically neglected individuals who have repeatedly committed socially dangerous actions, to whom compulsory security and treatment measures or conditions of long-term social isolation were previously applied.
Both healthy (true simulation) and psychoabnormal persons can simulate (pathological simulation: occurs on an already pathological basis in psychopaths, neurotics, oligophrenics against the background of an existing disease or defect). Healthy people more often feign non-psychotic disorders; they are characterized by simple and crude forms of pretense. Patients (usually psychopathic individuals) feign productive (“+” - symptoms).
As mentioned above, pathological simulation is formed even in the presence of any mental disorders. Here they highlight:
- aggravation - a conscious and deliberate exaggeration of the symptoms of a currently existing disease or residual effects after a mental disorder suffered in the past (more often found in oligophrenics, patients with vascular diseases of the brain, consequences of head injury, in psychopathic individuals), it can be intentional (conscious) and unintentional (the patient’s unconscious desire to arouse the sympathy of the medical staff; in particular, mental retardation patients may begin to exaggerate their intellectual disability). Aggravants are characterized by two features: preservation of personality and awareness of their defect;
- metasimulation - a conscious prolongation of the disease or a targeted depiction of already disappeared psychopathological symptoms, for example, a previous reactive psychosis (for example, a patient with psychosis indicates the presence of already disappeared hallucinatory-delusional experiences in order not to be discharged from the hospital for some personal reasons);
- sursimulation (oversimulation) - depiction of psychopathological symptoms that are not characteristic of the existing disease (often occurs in schizophrenia in the form of a severe amnestic syndrome, behavior can be caricatured). Sometimes the doctor provokes the patient to introduce into his behavior symptoms that are not characteristic of the disease he is simulating, which subsequently confirms the pretense.
Depending on the time factor (chronological aspect), there are 3 types of simulation:
1. Pre-simulation
(before committing a crime). The goal is to prove the presence of a mental disorder in the past.
2. Simulation at the time of the crime
(to hide his true motives). The goal is to convince everyone that the crime was committed in a painful state.
3. Simulation after the crime
(in the form of defensive behavior in order to evade responsibility). The most common option on the SPE.
In the context of the topic under consideration, it should be noted that there is a concept opposite to “simulation”. This is a disclaimer. Dissimulation is a deliberate (conscious) concealment (concealment) of the presence of mental disorders. A form of pretending behavior that is the opposite of pretending. It is more common in delusional psychoses and schizophrenia. Patients try to leave a mental hospital in order to realize their intentions dictated by delusional ideas or to commit suicide (for example, in a state of depression). The reason may also be the desire to preserve one’s civil rights and legal capacity.
Simulation of mental disorders
Definition 1
Feigning mental illness is a conscious behavior based on the presentation of non-existent signs of mental disorders by pretending or artificially causing them in order to avoid punishment.
Individuals may turn to the simulation of mental disorders if they are brought to criminal liability, threatened with imprisonment after conviction, when trying to avoid conscription into the army, in order to acquire a category of disability in order to receive various benefits and privileges.
The most common reasons for pretending to have a mental disorder are:
- create the impression that the crime was due to painful reasons and evade criminal liability;
- change the general direction of the investigation and delay the trial process;
- acquire the necessary information;
- impose your own version of the act on the investigation;
- achieve referral to EPT;
- achieve benefits that are only available to mentally ill people;
- mitigate the severity of the consequences of criminal actions.
- Coursework 490 rub.
- Abstract 230 rub.
- Test work 200 rub.
Both mentally healthy people and mentally disabled people can resort to simulation.
Forms and methods of simulating mental disorder
A simulation with the task of avoiding legal liability can be divided into three time groups:
- preventive or preliminary simulation, which is carried out in the period preceding the crime; this kind of simulation is implemented in advance with the task of forming a judgment about an action of an illegal nature, as an act carried out in a state of mental illness;
- simulation, which is deliberately carried out during the period of an offense with the goal of concealing its actual motivation;
- subsequent simulation, which is carried out after the commission of a crime, as a conscious, directed behavior with the task of avoiding responsibility.
In forensic psychiatric practice, the latter option is most often noted.
There are two methods of simulation:
- simulation of the mental illness itself, when, through their own behavior and statements, they try to reproduce the pathological state of the psyche (which does not exist and never existed). Sometimes special medications are taken for this purpose, which temporarily cause a condition that can give the impression of a mental illness;
- simulation of anamnesis, when those simulating report incorrect information about a pathological condition that allegedly occurred in the past (most often supported by forged documents and invented confirmations from specially instructed relatives).
Thus, an impression is formed of a mental illness suffered in the past, which in fact did not exist.
The forms of true simulation depend on personal conditions, the main ones among which seem to be the person’s awareness of the symptoms and distinctive features of the course of mental illnesses, depending on his experience. As a rule, individuals often resort to simulating anamnestic information rather than a painful mental state.
Note 1
Fingering of a specific clinical form of the disorder is quite rare. More often, individual symptoms (hallucination, depression, memory impairment, autism) or syndromes (paranoid, paranoid, etc.) are simulated.
Chronologically (relative to the event of the crime), three types of simulation of mental disorders are distinguished:
- before committing a crime (with the task of forming the impression that even before that time the patient had a mental disorder);
- at the time of the crime (to argue that the crime was committed in an insane, unhealthy state);
- after committing a crime (as a defensive reaction of the psyche with the task of avoiding responsibility).
Simulation or aggravation?
Note 2
Aggravation and simulation are phenomena that are similar in their manifestations, but very different in the reasons for their formation.
Simulation is the deliberate reproduction of certain signs of a disease.
Absolutely healthy people with a specific (selfish) goal or people who suffer from mental disorders can simulate. The key difference between malingerers is their rather attentive attitude towards themselves and their own health; they never do something like that that could seriously harm it.
Note 3
Aggravation is an unintentional exaggeration of the symptoms of a disease that a person experiences or thinks that he is experiencing.
Aggravants may deliberately harm themselves, not take medicine, or refuse to consent to treatment in order to worsen their own condition.
The key difference between malingerers and aggravants is their attitude to their own health and condition. The first ones know for sure that they are lying, and they do not have this disorder (at the same time, they may have other illnesses that they do not complain about) and they always have a benefit or goal from such behavior
Diagnosis and treatment
Diagnosing these syndromes is quite difficult.
During simulation, laboratory tests and other diagnostic research methods that certify the absence of pathology can help make an accurate diagnosis.
With aggravation, such diagnostic methods often turn out to be ineffective, since the symptoms actually exist, and the severity of the patient’s condition is quite difficult to assess.
The main difference between the symptoms of aggravation and simulation from the true disease:
- the contrast between the number of complaints and their presented manifestations;
- insufficiency of symptoms - almost all diseases have a set of symptoms that imaginary patients cannot imitate;
- the presence of symptoms of mental disorders in the subject and demonstrative behavior;
- lack of or abnormal response to treatment;
- persistent inconsistencies in disorder history and complaints.
To diagnose aggravation and simulation of mental disorders in psychiatry, a medical consultation is used, which can confirm or refute the diagnosis.
As a rule, simulation does not require treatment and goes away on its own as soon as the patient ceases to benefit from his own condition. In severe cases, it is recommended to consult a psychologist.
Aggravation is treated by a psychiatrist as a mental disorder or personality disorder.
Thus, feigning mental illness is a deliberate feigned behavior that consists of demonstrating non-existent signs of a mental disorder, which is committed for selfish purposes in the hope of avoiding punishment. In all cases of simulation, there is awareness, purpose and intentionality.
Source: https://spravochnick.ru/psihologiya/simulyaciya_psihicheskih_rasstroystv/
The concept of dissimulation and aggravation of mental illness. Forensic psychiatric significance.
Simulation arising on pathological grounds. Defensive target behavior that arises on a pathological basis should be distinguished from true simulation. This kind of behavior can manifest itself in various forms.
Aggravation is a targeted exaggeration of mildly expressed symptoms of an existing disease or residual effects after a previous mental illness.
The phenomenon of aggravation is most often found in forensic psychiatric practice in patients suffering from oligophrenia, vascular diseases of the brain, in patients with traumatic brain lesions, and in psychopathic individuals. Aggravation is significantly more common in forensic psychiatric examinations than malingering.
Metasimulation (prolongation of the disease) usually manifests itself in the depiction of the prolongation of individual symptoms of a previously suffered mental illness. Forms of conscious prolongation of the symptoms of reactive psychosis that occur after arrest are usually observed. Such forms differ in the duration of their course and present difficulties both for forensic psychiatric examination and for psychotherapeutic influence.
Demonstration by mentally ill patients of symptoms that are not characteristic of the existing disease (oversimulation or sursimulation ) is a rare phenomenon and is recognized quite easily. It manifests itself in symptoms that are alien, unusual for the underlying disease, and reflect the pathological motivation of the behavior of mentally ill people.
The main methods for recognizing the simulation of mental illnesses mainly come down to clinical observation and experimental psychological research methods; additional paraclinical studies (electroencephalography, etc.) with computed tomography are also used.
Establishing simulation of mental disorders by healthy individuals does not present any great difficulties, in contrast to identifying simulation on pathological grounds.
When simulating on a pathological basis, the main importance for a forensic psychiatric assessment is to establish the nature and depth of the existing changes. When resolving expert issues, in the conclusion it is necessary to indicate the presence of simulation or aggravation, as well as the mental characteristics of the subject that do not exclude the ability to realize the actual nature and social danger of their actions and manage them.
Dissimulation of mental disorders is the deliberate concealment, concealment of an existing mental illness or its individual symptoms. A distinction is made between complete and partial dissimulation .
With complete dissimulation, patients deny that they have any mental disorders, both at the time of examination and in the past.
With partial dissimulation, patients hide only certain clinical manifestations, and talk about others in sufficient detail. Partial dissimulation includes cases when patients attribute all existing mental disorders to the past, completely denying them at the time of examination.
Dissimulation is resorted to by patients who fear hospitalization in a psychiatric hospital, deprivation of civil rights, or seek to be discharged from a psychiatric hospital, especially during the period of compulsory treatment.
Sometimes there are cases when delusional patients dissimulate in order to be discharged from the hospital in order to gain the opportunity to realize delusional ideas that, in their content, pose a high social danger (capturing imaginary persecutors, delusional revenge, etc.). Patients in a state of depression can also dissimulate, seeking to commit suicide.
The form of dissimulation chosen by patients largely depends on the extent to which they can critically realize what features of their behavior are perceived by others as a sign of illness. Manifestations of dissimulation also depend on the extent to which existing psychopathological disorders allow patients to control their behavior.
Thus, the ability to dissimulate indicates partial criticism of one’s painful experiences. At the same time, the presence of dissimulation reflects patients’ insufficient consideration of all the features of the real situation and insufficiently complete prediction of the consequences of their condition and behavior. This is especially common in patients with schizophrenia. Recognizing dissimulation, which prevents timely diagnosis of the true nature of the disease, often presents significant difficulties in forensic psychiatric practice.
To recognize dissimulation, anamnesis data indicating past psychotic states are of great importance. With dissimulation, despite the stingy, formal and evasive nature of the patients’ responses, which does not allow the identification of delusional experiences, symptoms always remain in one form or another, which cannot be dissimulated. Thinking disorders specific to schizophrenia in the form of some inconsistency, slippage, and peculiarities of emotional manifestations will be easily noticed by specialists. Some characteristic features are also manifested in behavior, pretentiousness, inappropriate facial expressions, and angular motor skills characteristic of patients. Psychological examination methods provide significant assistance in recognizing dissimulation.
Ascertaining dissimulation is especially important when deciding whether there are indications for hospitalization of a patient. The presence of dissimulation must be taken into account when choosing medical measures in relation to patients who have committed a socially dangerous act and are declared insane.
Aggravation and simulation of mental disorders
Every attending physician, sooner or later, encounters a patient who exaggerates or invents the symptoms of the disease. This could be a student who doesn't want to go to school, a grandmother who is bored alone, or a person suffering from mental illness. How to distinguish imaginary diseases from real ones and simulation from aggravation?
Manifestations
Most often, patients choose to simulate diseases and symptoms that do not require much effort to depict: delusional disorders, hallucinations, memory impairment, and so on.
Patients with actual illnesses usually depict the most “colorful” manifestations of their illness. Thus, aggravation of epilepsy, reactive psychosis, memory disorder, and so on is common.
At the same time, aggravation of seizures can be accompanied by real damage: patients “in a seizure” injure themselves, bite their tongues, or deliberately “bring” themselves to an attack.
Diagnosis and treatment
Diagnosing these syndromes is quite difficult.
When simulating, laboratory tests and other diagnostic research methods that indicate the absence of pathology help to make a correct diagnosis.
In case of aggravation, such diagnostic methods often turn out to be ineffective, since the symptoms are really present, and the severity of the patient’s condition is quite difficult to assess.
The main difference between the symptoms of aggravation and simulation from the true disease:
- Contrast between the number of complaints and their visible manifestations.
- Insufficient symptoms - almost all diseases have a complex of symptoms that imaginary patients cannot imitate.
- The presence of symptoms of mental disorders and demonstrative behavior in the subject.
- Abnormal response to treatment or lack thereof.
- Constant discrepancies in medical history and complaints
To diagnose aggravation and simulation of mental disorders in psychiatry, a medical consultation is used, which can confirm or refute the diagnosis.
Treatment
Simulation, as a rule, does not require treatment and goes away on its own as soon as the patient ceases to benefit from his condition. In severe cases, it is recommended to consult a psychologist.
Aggravation is treated by a psychiatrist as a mental disorder or personality disorder.
about simulating illness:
Source: https://opsihoze.ru/rasstrojstva-lichnosti-i-povedenija/kak-otlichit-mnimye-bolezni-ot-nastojashhih-i-simuljaciju-ot-aggravacii.html
Forms and methods of simulating mental disorder
A simulation with the task of avoiding legal liability can be divided into three time groups:
- preventive or preliminary simulation, which is carried out in the period preceding the crime; this kind of simulation is implemented in advance with the task of forming a judgment about an action of an illegal nature, as an act carried out in a state of mental illness;
- simulation, which is deliberately carried out during the period of an offense with the goal of concealing its actual motivation;
- subsequent simulation, which is carried out after the commission of a crime, as a conscious, directed behavior with the task of avoiding responsibility.
In forensic psychiatric practice, the latter option is most often noted.
There are two methods of simulation:
- simulation of the mental illness itself, when, through their own behavior and statements, they try to reproduce the pathological state of the psyche (which does not exist and never existed). Sometimes special medications are taken for this purpose, which temporarily cause a condition that can give the impression of a mental illness;
- simulation of anamnesis, when those simulating report incorrect information about a pathological condition that allegedly occurred in the past (most often supported by forged documents and invented confirmations from specially instructed relatives).
Too lazy to read?
Ask a question to the experts and get an answer within 15 minutes!
Ask a Question
Thus, an impression is formed of a mental illness suffered in the past, which in fact did not exist.
The forms of true simulation depend on personal conditions, the main ones among which seem to be the person’s awareness of the symptoms and distinctive features of the course of mental illnesses, depending on his experience. As a rule, individuals often resort to simulating anamnestic information rather than a painful mental state.
Note 1
Fingering of a specific clinical form of the disorder is quite rare. More often, individual symptoms (hallucination, depression, memory impairment, autism) or syndromes (paranoid, paranoid, etc.) are simulated.
Chronologically (relative to the event of the crime), three types of simulation of mental disorders are distinguished:
- before committing a crime (with the task of forming the impression that even before that time the patient had a mental disorder);
- at the time of the crime (to argue that the crime was committed in an insane, unhealthy state);
- after committing a crime (as a defensive reaction of the psyche with the task of avoiding responsibility).
How to distinguish imaginary diseases from real ones and simulation from aggravation
Aggressive behavior in humans can be caused by a variety of reasons.
- abuse of alcohol, as well as drugs that weaken the nervous system, which provokes the development of an aggressive, inadequate reaction to minor situations;
- problems of a personal nature, unsettled personal life (lack of a life partner, a feeling of loneliness, intimate problems that cause depression, and later turn into an aggressive state and manifest themselves at every mention of the problem);
- mental trauma received in childhood (neurosis received in childhood due to poor parental relations);
- strict upbringing provokes future manifestations of aggressiveness towards children;
- passion for watching quest games and thrillers;
- overwork, refusal to rest.
Aggressive behavior is observed in a number of mental and nervous disorders. This condition is observed in patients with epilepsy, schizophrenia, due to injuries and organic lesions of the brain, meningitis, encephalitis, psychosomatic disorders, neurasthenia, epileptoid psychopathy.
The causes of aggression are subjective factors (customs, revenge, historical memory, extremism, fanaticism of some religious movements, the image of a strong person introduced through the media, and even the psychological individual traits of politicians).
There is a misconception that aggressive behavior is more characteristic of people with mental illness.
There is evidence that only 12% of people who committed aggressive acts and were referred for a forensic psychiatric examination were diagnosed with mental illness.
In half of the cases, aggressive behavior was a manifestation of psychosis, and the rest had inappropriate aggressive reactions. In fact, in all cases there is an exaggerated reaction to circumstances.
Observation of teenagers has shown that television perpetuates an aggressive state through crime programs, which further enhances the effect. Sociologists, such as Carolyn Wood Sheriff, challenge the popular belief that sports act as ersatz war without bloodshed.
Long-term observations of teenagers at a summer camp showed that sports competitions not only do not reduce mutual aggressiveness, but only intensify it. An interesting fact was discovered about the removal of aggressiveness in adolescents. Working together in the camp not only united the teenagers, but also helped relieve mutual aggressive tension.