What is paranoid personality disorder
Paranoid personality disorder is a personality disorder in which a person is characterized by resentment and suspicion that goes beyond normal limits.
Any actions of the immediate environment (including neutral and completely harmless ones) are perceived as posing a threat to safety.
Causes of paranoid personality disorder
Symptoms
Paranoia is a disease in which the actions and actions of patients appear incomprehensible and inadequate to others. Thus, the symptoms of the disease are not so much external as behavioral:
- Often a paranoid person is characterized by excessive touchiness. Such a person does not forget grievances, often inventing them for himself.
- The paranoid person perceives any critical remarks addressed to him very violently and sharply. He considers this to be malicious intent towards himself.
- The patient is tormented by thoughts that he is constantly being betrayed by people around him, for example, family members or colleagues, just acquaintances and friends.
- The words and actions of the people around him cause the patient to think that all this is being done with malicious intent, that all this is directed specifically against him. In the words of people he hears evil threats against him.
- The patient develops suspicion directed towards everyone around him, even ordinary passers-by on the street. And even more so, he suspects his family members of evil intentions.
- The patient is able to track down his loved one for hours, suspecting him of infidelity. Jealousy haunts him.
Few people think that these symptoms are a disease and a person needs treatment. People around them simply consider such patients to be very arrogant and arrogant, and they often need help.
Severe symptoms
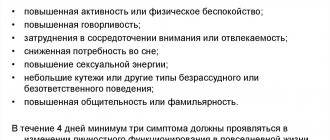
As the disease progresses, patients exhibit the following symptoms:
- isolation, manifested in the fact that a person stops sharing his thoughts and feelings with others, “anticipating” the use of the information received against him;
- black and white thinking;
- frequent conflicts that they provoke themselves;
- dissatisfaction with everyone and everything;
- painful perception of any negative event;
- tendency to prejudice;
- lack of sense of humor;
- the emotional background is mainly negative, the predominant reactions are anger, indignation, indignation.
Without the necessary therapy, the listed symptoms aggravate the person’s condition.
Paranoid personality disorder
Classification
Experts determine a certain type of paranoid psychosis in a patient, based on the symptoms, that is, on the type of delusional ideas that is most manifested in the patient. They can be like this:
- Delusions of persecution (most common). In any casual glance, the patient sees surveillance and believes that they want to cause him some harm.
- Delirium of jealousy. The patient is convinced of his spouse’s infidelity. This jealousy may also be related to the past of his other half; sometimes the patient may believe that his own child was not born from him at all, etc.
- Somatic delirium. The patient is sure that he suffers from serious illnesses, his health is seriously impaired.
- Delusions of grandeur - identifying oneself with historical characters, famous personalities, the hero of a literary work, etc.
- Erotomanic delusion is similar to delusions of grandeur, but the patient does not identify himself with a famous person, but ascribes to himself love from such a character.
- Mixed type of delusional disorder - combines symptoms and signs of various types of paranoid psychosis.
For any type of psychosis, mandatory examination and subsequent treatment by specialists is necessary.
Paranoid psychosis symptoms and signs
Psychosis refers to the collective name of a group of various mental disorders that are accompanied by psychopathological productive symptoms: delusions, pseudohallucinations, hallucinations, derealization, depersonalization. The patient has a distorted reflection of the real world, which is expressed in behavioral disorders, as well as the manifestation of pathological disorders of memory, perception, thinking, and affectivity. Psychosis does not give rise to new phenomena; it represents a loss of activity at higher levels.
The causes of psychoses of a diverse nature are identified, and they are divided into internal and external. External causes include: stress, psychological trauma, infections (tuberculosis, influenza, syphilis, typhoid); consumption of alcohol, drugs, poisoning with industrial poisons. If the cause of a disturbance in the state of mind is within a person, then endogenous psychosis occurs. It is provoked by disorders of the nervous system or endocrine balance. Endogenous mental disorders occur due to age-related changes in the body or as a consequence of hypertension, schizophrenia, and cerebral atherosclerosis. The course of an endogenous disorder is marked by duration, as well as a tendency to relapse.
Psychosis is a complex condition and it is often impossible to identify what exactly triggered its appearance. The first push can be caused by an external influence, to which an internal problem is added. The first place among external causes is given to alcohol, which can provoke alcoholic psychosis. The cause of psychosis is also old age and endomorphic disorders, clouding of consciousness. According to the characteristics of the course, reactive as well as acute psychoses are noted. Reactive psychosis is a temporary as well as reversible disorder that occurs due to (mental) trauma.
Acute psychosis has a sudden onset. It can be triggered by unexpected news of the loss of property, as well as the loss of a loved one.
This condition manifests itself in a distorted perception of the real world, as well as disorganization of behavior. The first signs of psychosis are a sharp decline in activity at work, increased stress, and impaired attention. The patient experiences various fears, mood swings, and is characterized by depression, isolation, mistrust, withdrawal, cessation of all contacts, and problems communicating with people. The sufferer develops interests in unusual things, for example, religion, magic. A person often worries, his perception of sounds and colors changes, it seems to him that he is being watched.
Often the disease has a paroxysmal course. This means that the course of this mental state is characterized by outbreaks of acute attacks, which are followed by periods of remission. The attacks are characterized by seasonality and spontaneity. Spontaneous outbursts appear under the influence of traumatic factors. There are also so-called single-attack courses that are observed at a young age. Such an attack is characterized by a significant duration and gradual recovery. In this case, working capacity is completely restored. Severe cases of psychosis progress to a chronic, ongoing stage. Such cases are characterized by symptoms that manifest themselves throughout life, even despite treatment.
A person suffering from mental disorders experiences a number of changes in behavior, emotions, and thinking. The basis of this metamorphosis is the loss of adequate perception of the real world. It becomes impossible for a person to realize what is happening, as well as to assess the severity of mental changes. The patient experiences a depressed state, he is haunted by hallucinations and delusional statements.
Hallucinations include talking to oneself, laughing for no reason, listening and falling silent, looking preoccupied. The feeling that a relative of the patient hears something he is unable to perceive.
Delusions are understood as changed behavior, the appearance of secrecy and hostility, direct statements of a dubious nature (persecution, one’s own greatness or irredeemable guilt.)
All mental state disorders are classified according to etiology (origin), as well as causes, and are distinguished as endogenous, organic, reactive, situational, somatogenic, intoxication, post-withdrawal and abstinence.
In addition, the classification of mental disorders necessarily takes into account the clinical picture and the prevailing symptoms. Depending on the symptoms, hypochondriacal, paronoid, depressive, manic mental disorders and their combinations are distinguished.
This condition rarely occurs in women after childbirth; it appears in the second to fourth week. The woman herself often does not feel postpartum psychosis. It is very important to diagnose the disease in a timely manner and begin treatment. Late diagnosis may delay recovery.
The cause of this condition is complications during childbirth and pain shock.
The more trauma a woman receives (physical, psychological) during childbirth, the more difficult the mental state disorder occurs. The first birth has a higher likelihood of mental disturbances than the second. A woman during her second birth already knows what to expect psychologically and does not experience such fear as during the first. Qualified medical care often does not reach the mother in labor, since no one pays attention to her psychological state. Relatives and doctors are more concerned about the physical health of the woman and the newborn, so the mother in labor is left alone with her psychological state.
Postpartum psychosis is often confused with postpartum depression. Postpartum psychosis is characterized by anxiety, insomnia or restless sleep, confusion, loss of appetite, delusions, lack of adequate self-esteem, and hallucinations.
Psychosis after childbirth is treated in a hospital. It is strictly forbidden for a mother to remain alone with her baby. Psychotherapy is indicated for nursing mothers; drug therapy is prescribed very carefully and under the mandatory supervision of medical staff.
This state is typical for a team, a group of people, a nation, where the basis is suggestibility and imitation. Mass psychosis also has a second name - a mental epidemic. As a result of massive mental disturbances, people lose adequate judgment and become possessed.
Cases of mass psychosis have a common formation mechanism. An inadequate state is characterized by non-collective behavior called a crowd. The crowd refers to the public (a large group of people) who are united by common interests and act very unanimously, as well as emotionally. Often in a crowd there is a collection of amorphous individuals who do not have direct contacts with each other, but are connected by a constant common interest.
Cases of mass psychosis include mass self-immolation, mass religious worship, mass migrations, mass hysteria, mass passion for computer games and social networks, mass patriotic, as well as false-patriotic frenzy.
In mass disturbances of the mental state of non-collective behavior, a huge role is assigned to unconscious processes. Emotional arousal is based on spontaneous actions that arise from impressive events and necessarily affect significant values. For example, the fight for your rights and interests. Sigmund Freud viewed this crowd as a human mass under hypnosis. A very dangerous and significant aspect of crowd psychology is its acute sensitivity to suggestion. The crowd either accepts or completely rejects any belief, opinion, idea, and hence treats them either as absolute truths or as absolute delusions.
All cases of suggestion are based on an illusion that is born in one of the individuals who has more or less oratory skills. The evoked idea, namely the illusion, becomes the core of crystallization, which fills the entire area of the mind, and also paralyzes people's ability to criticize. People with a weak psyche, with a history of deviations, depression and mental illness are especially susceptible to massive disturbances in their state of mind.
This condition is considered a more severe manifestation than paranoia, but it is milder than paraphrenia. Paranoid mental disorders are characterized by ideas of persecution, as well as influence with affective disorders. Often this condition is observed in organic and somatogenic disorders, as well as toxic mental disorders (alcoholic psychosis). Paranoid psychosis in schizophrenia is combined with mental automatisms and pseudohallucinosis.
Paranoid psychosis is characterized by vindictiveness and constant dissatisfaction with others. A person is sensitive to all refusals, as well as failures. The individual turns into an arrogant, jealous person, watching over his other half - his spouse.
Paranoid psychosis mainly occurs at a young age, predominantly in men. All these suspicions, which are characteristic of the patient, significantly worsen his life and introduce social restrictions. Such individuals cannot tolerate criticism and have a reputation as scandalous and arrogant people. This condition inevitably drives a person into self-isolation and, without treatment, the patient’s life turns into torture. To get rid of a paranoid mental disorder, timely psychotherapy is necessary. The psychotherapeutic approach aims to improve general life skills, improve the quality of social interaction, and strengthen self-esteem.
Paranoid psychosis is treated only with medication. Antidepressants, tranquilizers, and antipsychotics are used in treatment.
The disease has a second name - senile psychosis. This disorder is typical for people over 60 years of age and is characterized by a state of confusion. Senile mental disorders often resemble manic-depressive psychosis.
Senile psychosis differs from senile dementia in the absence of total dementia. An acute form of senile mental disorder is observed very often. The cause is somatic diseases.
The cause of senile mental disorders is often chronic or acute diseases of the respiratory tract, as well as heart failure, diseases of the genitourinary system, hypovitaminosis, and surgical interventions. Sometimes the cause is physical inactivity, poor nutrition, sleep disturbances, decreased hearing and vision. Chronic forms of senile disorders tend to occur in the form of depressive states, which are often observed in women. In mild cases, subdepressive states occur, which are characterized by lethargy, adynamia, a feeling of emptiness, and aversion to life.
In children, psychosis is severe. The disease is characterized by impaired ability to distinguish between reality and fantasy, as well as the ability to adequately assess what is happening. Any type of mental disorder significantly harms the baby’s life. The disease creates problems in thinking, controlling impulses, expressing emotions, and also spoils relationships with other people.
Psychosis in children takes many forms. Hallucinations are common when a child hears, sees, touches, smells and tastes things that do not exist. The baby makes up words, laughs for no reason, gets very irritated for any reason, and also for no reason.
An example of psychosis in children: after reading the fairy tale “Cinderella,” the child perceives himself as the main character and believes that the evil stepmother is nearby in the room. This perception by the baby is referred to as hallucinations.
Mental disturbances in children occur due to short-term as well as long-term physical conditions, long-term use of medications, hormonal imbalance, high fever, and meningitis.
Psychosis in a 2-3 year old child in many cases ends when his problems are resolved or become a little dull. In rare cases, complete recovery occurs after treatment of the underlying disease.
The disease in a 2-3 year old child is diagnosed after repeated examinations over several weeks. A child psychiatrist, neurologist, otolaryngologist, and speech therapist take part in the diagnosis.
Diagnostic procedures include a thorough physical and psychological examination, longitudinal observation of the baby's behavior, testing of mental abilities, as well as hearing and speech tests. The disease in children is treated by specialists only after a thorough examination.
Psychosis after surgery occurs immediately or two weeks later. Such disorders are observed after neurosurgical operations on the brain. Postoperative disturbances in mental state are characterized by confusion or stunned consciousness, affective-delusional disorder, and psychomotor agitation. The reason is the influence of anesthesia. Coming out of anesthesia is accompanied by oneiric episodes with autoscopic hallucinations or fantastic combined hallucinations, and is also marked by an emotional state that is close to ecstatic.
Principles of treatment
Treatment is prescribed by a psychiatrist (less often by a psychiatrist-psychotherapist). Depending on the severity of the mental disorder, it can take place on an outpatient basis, in a day or 24-hour psychiatric hospital. Moreover, if a person’s behavior is assessed by a medical commission as dangerous for himself and others, or very serious, treatment will be carried out by court decision, on an involuntary basis.
The therapeutic regimen is selected individually and may include several groups of drugs. But in any case, the basis of treatment is antipsychotics in various forms and dosages. According to the doctor's decision, typical or atypical antipsychotic drugs are used.
The following may also be prescribed:
- Sedatives, usually tranquilizers. They are used for a short period of time, according to indications and not in all patients. Designed to reduce the level of anxiety and affective charge, and relieve psychomotor agitation.
- Antidepressants. Indicated for depressive-paranoid psychosis and reactive psychogenic paranoid. But according to the doctor’s decision, they can also be used for milder secondary affective disorders.
- Correctors are drugs to reduce pathological extrapyramidal muscle tone that has developed as a complication of neuroleptic therapy.
Individual and group psychotherapy and psychocorrectional classes are also used. The objectives of such treatment are to develop sufficient criticism of hallucinatory-delusional experiences, acceptance of the need for treatment, and rehabilitation to return to normal life.
Structure of paranoid psychosis (syndrome)
Paranoid (paranoid) psychosis is a pathological condition based on disturbances in the content of thinking and perception disorders. It is characterized by persistence and a certain pattern of development. At the same time, there is no change in the depth and quality of consciousness, so the experiences are retained in memory even after the person exits the psychotic state.
The main pathopsychological components of paranoid psychosis:
- Delusions are persistent pathological ideas and beliefs that occupy the bulk of thinking and actively influence human behavior. At the same time, he develops a special delusional perception, when most of the events that occur are interpreted differently and “fit” into the picture of delusion. At the same time, a person builds a system of proof of his own rightness, which is well structured, cannot be adjusted externally, and is constantly updated. Delusions have unpleasant and even threatening content; most often with paranoid syndrome, ideas of persecution and harm arise. They are called persecutory.
- Perception disorders in the form of hallucinations. They generally correspond to the content of delirium and support its existence and development. Auditory hallucinations are the most common, but deceptions can also involve other senses.
- Altered affect (emotionally charged and depressed mood). Such changes are clearly noticeable when discussing experiences and when entering a situation that actualizes delirium. But mood can also be constantly low, which affects everyday behavior. In such cases, depressive-paranoid psychosis is diagnosed.
In classic paranoid hallucinations are true, that is, they are perceived as coming from the outside and are indistinguishable from real signals from the outside world. But more complex psychosis often occurs, when pseudohallucinations and the resulting delusions of influence appear. At the same time, a person feels “made” and “imposed” on his thoughts and actions, which he interprets as the appearance of external control and mental control.
Paranoid psychosis, characterized by delusions of influence and pseudohallucinations, is called Kandinsky-Clerambault syndrome or mental automatism syndrome. This is a more severe and complex version of a psychotic disorder.