Symptoms
With such an illness as sluggish schizophrenia, symptoms quite often begin to appear in adolescence, but specific manifestations are revealed somewhat later. The long-term, gradual progression of the disease goes along with gradual personal deformations, but many patients with sluggish schizophrenia still manage to, in some sense, curb their illness and maintain the necessary level of social behavior and adaptation throughout their lives. The line between ordinary and low-progressive schizophrenia is very small. Slightly progressive schizophrenia is characterized by a high frequency of nervous and mental disorders. And in the first option, deviations in associative thinking predominate: a decrease in affective perception, a deficit of social interaction, deformation of associations and an ambivalent attitude towards many things. Considering ambivalence to be the main symptom of schizophrenia, it is divided into three types: emotional, volitional, and intellectual areas.
If you begin to notice any of the above symptoms in a loved one, you should immediately contact the Rehab Family clinic for highly qualified help.
Depression in schizophrenia: features of the course
The complex clinical picture of schizophrenia is based on positive and negative symptoms. Positive symptoms include delusions, hallucinations and thought disorders. Negative symptoms are represented by affective changes and are closely related to the development of depression in schizophrenia, which is a common and significant symptom of the disease.
Peculiarities
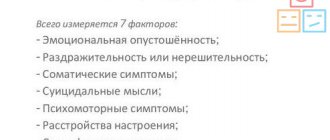
The incidence of depressive symptoms in schizophrenic disorder is about 40%, but this varies depending on individual circumstances. During an acute episode it increases to 60%, and in a post-psychotic episode it decreases to 20% during the chronic course of the disease and to 50% after the first attack.
An obvious connection has been established between the negative symptoms of the disorder and depression itself. These include the following manifestations:
- emotional dullness, absence or decrease in the intensity of manifested emotional reactions;
- poor speech;
- lack of opportunity to have fun;
- lack of motivation and will.
Depressive changes include:
- low mood;
- sleep disorders;
- low self-esteem;
- inability to have fun;
- apathy;
- decreased physical activity;
- pessimistic thoughts.
Depressive symptoms are quite common in schizophrenic disorder and occur in all its forms. In terms of prevalence, they are second only to hallucinatory, paranoid and apathetic states.
Due to the similarity of symptoms, it is sometimes very difficult to distinguish depression from negative symptoms. In addition, depression can provoke the development of secondary negative symptoms, which makes differentiation even more difficult.
Identifying depressive symptoms in the context of schizophrenic disorder becomes an important point of control.
The fact is that depression is a condition in which there is a high risk of suicidal thoughts and actually committing suicide.
Therefore, the previously existing assumption that the predominance of affective symptoms over positive ones in the clinical picture of the disorder indicates a more favorable course of the disorder is currently rejected.
Depression, in comparison with commanding hallucinations, is much more likely to provoke suicide attempts in schizophrenia.
It has been established that the mortality rate of such patients from suicide attempts is higher than in other disorders.
It is believed that depressive symptoms in the picture of schizophrenia provoke drug and drug addiction and increase the level of life dissatisfaction.
The most common theory of the occurrence of depressive states in this disorder is the personal reaction of patients to it. After experiencing the first episodes of the disease, a person develops a feeling of change, helplessness, and possible loss of professional prospects, friends, and family.
How does depression manifest in schizophrenic disorder?
Depressive manifestations against the background of schizophrenic pathology are very similar to its negative signs. This is, first of all, apathy, lack of vital energy, as well as mental anesthesia - a common symptom of endogenous depression. It is called painful insensibility.
In the foreground of the symptom is the loss or decrease in the degree of emotional reactions. The patient does not show any feelings towards loved ones and others, has an emotional response in relation to any activity, and is not capable of empathy - compassion.
Ethical and aesthetic aspects of behavior and perception are also not characteristic of him.
In addition to mental insensibility, the patient also feels bodily. It manifests itself as the absence of various types of sensations. Sometimes a person does not feel any part of the body.
In addition to those listed, other signs also include depressive schizophrenic manifestations. For example, gloominess, dissatisfaction, grumpiness, moodiness, irritability.
Depression often occurs in the prodrome, which then progresses directly to schizophrenia. In this case, its manifestations are anxiety and irritability, loss of strength, and insomnia. Such symptoms are often confused with banal overwork.
Increased tearfulness, sensitivity, irritability, pessimistic attitude, along with low self-esteem and “soul-searching” in the prodrome of schizophrenia are perceived as seasonal phenomena.
Depression with signs of withdrawal is characteristic both of the onset of the disorder and of its further development. This condition includes anxiety and symptoms of negative affectivity:
- anhedonia – inability to experience pleasure;
- apathy;
- indifference;
- monotonous, limited movements;
- decreased cognitive function;
- energy deficit;
- paucity of emotions.
Depressive manifestations in the form of borderline erotomania are characterized by tormenting memories of the object of love. At the same time, in the clinical picture, the phenomena of hypothymia, that is, low mood, are weakly expressed, but external expressive reactions predominate. Therefore, such depression is called hysteroidal.
Obsessive states of the depressive process in schizophrenia are characterized by increased anxiety, which can develop into generalized anxiety disorder. The process is joined by hypothymia and a tendency to pathological doubts, when a person needs to make a decision, make a choice.
Depressive episodes can be present not only at the beginning or the height of the disease, but also as its consequences. The negative social environment around a person contributes to this:
- poor relationships with relatives, loneliness;
- labeling;
- inability to perform professional or other activities;
- side effects of drugs.
Postschizophrenic depression manifests itself with standard depressive symptoms. This is a low mood, lack of interest in all areas of life and the constant presence of a feeling of dissatisfaction.
At the same time, the patient has mental and physical passivity. There is apathy, loss of strength, and decreased performance. Notes of aggression can be traced.
At the same time, some symptoms of the underlying disease also remain, but they do not come to the fore.
Post-schizophrenic depressive form develops in a quarter of patients and is characterized by a high risk of suicide.
How to differentiate schizophrenia and depression
It is very important in the context of schizophrenic disorder to highlight depression as one of its symptoms.
But given the similarity between depressive symptoms and negative schizophrenic symptoms, experts are faced with the problem of how to distinguish between these diseases.
We are talking about when a patient experiences a group of effective changes, but it is difficult to determine the diagnosis: depression or schizophrenia. The question arises: how are they different?
There are some criteria that help distinguish between these concepts. Schizophrenic disorder involves some strange or illogical behavior.
If you track the patient’s puberty, you should note his pathological character with personality disorders.
Schizophrenia is also confirmed by individual psychotic episodes, accompanied by fear, anxiety, depersonalization, and alienation.
Example: a young man complains of low mood, insomnia, and a feeling of constant anxiety that does not allow him to relax. Every time he falls asleep, he is visited by the same thoughts: I am a loser, I have achieved nothing in life.
The guy became distracted and his concentration was impaired. There are all the signs of a depressive disorder.
But from his anamnesis it is known that while he was at school, he paid little attention to the educational process and spent almost all his time on the street.
Subsequently, the man did not master any profession. He lived for his own pleasure, did not work. Attempts to engage in activities ultimately failed. Got married.
But the marriage did not last long: according to the patient, he had to separate from his wife because her father tried to poison her in order to appropriate the apartment for himself. The patient and his mother-in-law defended his wife, but soon the mother-in-law died.
Then the guy carried a knife with him everywhere in order to protect himself and his beloved in case of an attack. But, no longer able to deal with the problem alone, he decided to get a divorce.
The patient himself insists that massage will help cure him.
Costs of pharmacotherapy
As a rule, the main medications used to treat schizophrenic disorder are antipsychotics. They help cope with positive symptoms: eliminate delusions and hallucinations, but in some cases they can cause side effects in the form of neuroleptic depression, characterized by melancholy with signs of mental anesthesia.
The onset of neuroleptic depression are signs of akathisia. They are manifested by an internal feeling of restlessness, anxiety, which varies from mild, barely perceptible severity to irrepressible anxiety. There is a feeling as if she is eating the patient out from the inside. He cannot sit still and feels the need to constantly change his position.
A feature of the depressive state caused by neuroleptics are extrapyramidal symptoms in the form of parkinsonism, tremor, and hyperkinesis. Later, signs of mental anesthesia appear. Irritability, moodiness, importunity increases, and sleep is disturbed.
To reduce the likelihood of such side effects of antipsychotics in schizophrenia, they are prescribed in combination with antidepressants. The latter soften the manifestations of depressive symptoms and compensate for the neuroleptic effect.
Source: https://arbat25.ru/myi-lechim/psixicheskie-rasstrojstva/depressiya-pri-shizofrenii-osobennosti-techeniya
Signs
This disease develops so unnoticed by others and the person himself that it is almost never possible to identify the moment of its onset. The patient's activity slowly decreases, emotional flatness increases, the range of interests narrows, certain oddities in behavior appear, thinking and conversation become intricate. All these deformations in consciousness and behavior do not occur in weeks and months, but gradually accumulate and progress over many years.
When examining such problems as signs of sluggish schizophrenia, it should be noted that along with emotional impoverishment, the patient gradually begins to develop all kinds of fears, obsessions, hysterical attacks, and superficial depression. With low-progressive schizophrenia, depersonalization phenomena may be present - situations in which the patient perceives himself and his actions as if from the outside. At certain moments, the patient may experience hallucinations or various fragmentary delusional ideas. At the first signs of sluggish schizophrenia, you should immediately contact a competent clinic, which, of course, is the Russian Rehab Family clinic.
Schizophrenia and bipolar disorder differences
Diseases such as schizophrenia and bipolar disorder affect a large number of people around the world. Both men and women are susceptible to these diseases, but in the stronger half, this disorder may begin to manifest itself earlier. The first psychotic episodes appear from about 15-26 years old, while in women - only from 25-26 years old.
The appearance of symptoms of these diseases is rare before 10 and after 50 years.
Both diseases are considered severe mental disorders that require medication. Self-medication or traditional medicine in these cases are powerless and can aggravate the situation. Bipolar schizophrenia is difficult to diagnose due to the presence of symptoms associated with depression or nervousness.
Bipolar disorder is a mental disorder that manifests itself in a manic-depressive state of the patient.
The periods of these states abruptly replace each other. During breaks between these states, a person can lead a normal lifestyle. Intellect and behavior among others with this disorder remain the same. Relative to other mental illnesses, schizophrenia and bipolar disorder are the most difficult mental health disorders to diagnose.
During a manic attack, a patient may commit rash acts that would be unacceptable to a healthy person. For example, spend all your money, lose sleep for several days, quit your job for no reason. Alcohol and drugs pose a particular danger during mood swings. Their uncontrolled use can lead to health problems.
The patient's manic state is replaced by an attack of deep depression. The person will fall into despair because of the actions he has committed, will think about the hopelessness of the situation, and engage in self-flagellation.
The depressive and manic stages of the disease are followed by periods when the person is adequate and leads a normal life, but with an exacerbation of the disease, attacks can occur at any time.
A person’s mental health in such a situation will depend on a correct diagnosis and timely prescribed medications.
Schizophrenia is often confused with bipolar disorder, as these conditions have similar features:
- genetic predisposition;
- changes in the structure of the cerebral cortex;
- the presence of both depressive and impulsive aspects of behavior.
However, these are different diseases that cannot be cured at all, but with the help of medications and courses of psychotherapy, long-term remission can be achieved, during which the patient will lead a normal lifestyle.
Among the differences between one disease and another, one can highlight the fact that with schizophrenia, the patient develops obsessions and auditory hallucinations. Symptoms of schizophrenia are delirium, apathy, impaired thinking, decreased concentration, and inability to soberly assess the situation.
Bipolar disorder is characterized by euphoric mood, disordered thoughts, and unreasonable self-confidence.
The clinical manifestations of these conditions are similar. The causes of these disorders are deep depression, failures in life, work, relationships, as well as genetic predisposition. The transition from bipolar disorder to schizophrenia is impossible.
Thus, a person’s mental health depends on many factors in his life, including genetic predisposition. To avoid schizophrenia and other mental disorders or reduce the likelihood of their occurrence, it is necessary to avoid stressful situations, try to maintain peace of mind, and be balanced. If you suspect a change in your mental state, you should consult a specialist.
Bipolar affective disorder is a mental illness that alternates between depressing and elevating a person.
It would seem that a change of mood is inherent in everyone , but here everything is much more serious.
A rather dangerous disease if you do not pay attention to the symptoms of bipolar disorder.
Treatment
Unfortunately, it is impossible to give an absolute guarantee that anyone close to you will not have to face such a life difficulty as the treatment of sluggish schizophrenia or any other type of schizophrenia. Unfortunately, modern society is quite cruel to a person suffering from such an illness, and patients are very often left behind in life. The social environment of such people is afraid and abstracts from them, relatives become desperate in unsuccessful attempts to cure the patient, and schizophrenics still cannot understand what is really happening to them. It would be wrong to think that society is divided into mentally ill and mentally healthy. After all, no one has the right to set absolute boundaries of normality.
The difference between psychosis and schizophrenia: what is the difference?
An interesting question about the difference between psychosis and schizophrenia. I'm surprised by the people who ask this question. Well, don’t you see that the word “psychosis” begins with the letter p, and “schizophrenia” with the letter w? This is where they differ. Psychosis is the general name for serious mental disorders.
Schizophrenia is the name of a specific block of syndromes that are associated with the splitting of the thinking process, consciousness, and the presence of a certain mental defect. An episode of schizophrenia, no matter how it progresses, can also be called psychosis, since the disorder is of a mental nature.
It is also appropriate to use the terms “delirium” and “manifestation”. If you really want to share something, then separate neurosis and psychosis. True, the difference will be more legal than medical. Neurosis is also a mental disorder, but of a mild and reversible type.
They even talk about some kind of borderline state between health and disorder. Neurosis does not indicate insanity or incapacity, and therefore does not entail social restrictions or benefits.
Psychosis should be noted for schizophrenia to initiate proper treatment
Psychosis and schizophrenia
To say “psychosis” is to say nothing.
There are many psychoses that are not schizophrenia or are its semblance, its combination with something, but not exactly schizophrenia, as well as some psychotic forms of affective disorders.
Likewise, the term “schizophrenia” says little. We need to clarify which one it is. For example, simple schizophrenia is not accompanied by delusions or hallucinations, although it is also in the ICD 10 block with a code that begins with F20.
Schizophrenia is ambivalence of consciousness, a tendency towards autism, fragmented thinking, difficulties with adequately perceiving oneself and the world around us. Of course, schizophrenia is a psychosis, but not every psychosis is schizophrenia.
One of the signs of schizophrenia is ambivalence of consciousness
Diagnostics
To diagnose bipolar disorder and PMS, a mental health professional will ask a person questions about symptoms, including their severity and duration.
Will also ask about the person's family medical history, especially whether any relatives suffer from mental illness. A bipolar I diagnosis requires that a person has had at least one classic episode of mania that lasted at least 7 days or required hospitalization. People who experience a major depressive episode and an episode of hypomania may be diagnosed with bipolar II disorder.
https://www.youtube.com/watch?v=ytpressru
In cases where it is difficult to distinguish BPD from bipolar disorder, a doctor may focus on specific symptoms to help differentiate the two. These symptoms include:
- Dream. People with bipolar disorder typically have disrupted sleep cycles during periods of mania and depression. People with BPD have a regular sleep cycle.
- Mood swings: People with bipolar disorder typically experience cycles of mood swings that last anywhere from weeks to months. People with BPD typically have sudden, short-term mood swings that last a few hours or days.
- Self-harm: According to some estimates, 75% of people with BPD engage in self-harm. They may view self-harm as a means of emotional regulation or a way to control unstable or intense emotions. Although self-harm is less common in people with bipolar disorder, they have a higher rate of suicide attempts.
- Unstable relationships: Many people with BPD have intensely conflictual relationships. People with bipolar disorder may have difficulty maintaining relationships due to the severity of their symptoms.
- Mania: People with bipolar disorder act impulsively when they experience a period of mania. People with BPD also tend to act impulsively, but this behavior is not associated with mania.
Some additional information may help differentiate BPD from bipolar disorder, including:
- Family history. Mood disorders such as bipolar disorder and depression are usually hereditary, although researchers have not yet identified the specific gene responsible. People who have close family members with BPD are also at high risk of developing the condition.
- History of Trauma: The cause of BPD remains unclear, but many people with the condition have experienced trauma during childhood or adolescence. Examples of trauma include abuse, unstable family relationships, and exposure to conflict.