An epidural hematoma of the brain is an intracranial collection of blood that is located between the inner wall of the skull and the dura mater of the brain, resulting in compression of the brain tissue.
The incidence of this pathology is approximately 1% of all cases of head injuries.
On average, the volume of a cerebral hematoma reaches 120 ml, the size of a small hematoma is 30 ml, and the size of a large one is 250 ml. The size is approximately 7-8 cm. Often, an epidural hematoma affects one or two lobes of the brain.
Most often, lesions occur in the temporal zone and adjacent areas. This lesion is characterized by a dense central part, which tapers towards the periphery.
Deformation of the dura mater and brain matter occurs due to the incompressibility of the hematoma. In other words, it exerts pressure on the shell due to its mass, and a dent of a certain size is formed.
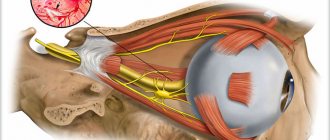
The source of bleeding in most cases is an artery with branches, less often - veins and sinuses, and only in exceptional cases - spongy tissue, which is located between the inner and outer layers of the skull.
In children who have not reached the age of two, the dura mater of the brain is much more tightly fused with the inner surface of the skull than in an adult. That is why such pathology practically does not occur at this age.
Causes of hematoma
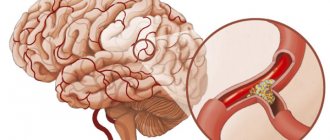
In most cases, hematomas of this type are of traumatic origin. However, a pathological condition can also develop. It is caused by a rupture of a blood vessel. People suffering from a sharp increase in blood pressure are at risk.
So, let's figure out what can trigger the development of a disease such as an epidural hematoma. The causes of its occurrence are traumatic brain injury caused by a small object. These include a hammer, stick, stone. Upon impact, the affected area is relatively small. The development of a hematoma is influenced not only by the force of the blow, but also by the position of the head. If it is motionless, then the risk doubles. A blow to a fixed object can also lead to the formation of blood clots in the brain. That is, a person, while in motion or in a standing position, falls and hits a door, corner of a table or shelf.
As a rule, as a result of injury, the skull is locally deformed. A characteristic depression may appear in this place. When an impact occurs on the damaged area, the bone is pressed into the cranial cavity. This causes rupture of blood vessels, which leads to bleeding.
Where is the danger hiding?
As a rule, with a head injury, a concussion occurs, but in the case of rupture of venous or arterial vessels, subdural and epidural hematomas can develop, differing from each other in the nature of compression of the brain and localization.
What is the difference between a subdural and epidural hematoma
The occurrence of a bruise is almost always associated with a head injury, and the nature of its occurrence can be different, for example, a subdural or epidural hematoma occurs due to:
- A blow with a blunt object to the skull area leads to indentation or fracture of the bones of the skull; as a result, venous or arterial vessels may rupture, leading to hemorrhage.
- A blow to the head while falling from a moving vehicle, falling out of a window, etc., which is also accompanied by indentation of the skull bones, leads to similar consequences.
Subdural
The most common form. Subdural hematoma of the brain is characterized by the ability to affect several areas of the brain, as it is correctly localized between the arachnoid membrane of the brain and the dura mater. In most percent of cases, it occurs as a result of rupture of the venous vessels of the head, in particular when the bridging veins rupture.
The bridging veins connect the dura mater with the soft mater.
Classification:
- acute;
- subacute;
- chronic.
Acute – occurs in the first few hours after injury.
Subacute – manifests itself within a few days (no later than 2 weeks).
Chronic – makes itself felt after a few weeks.
If in the case of the acute type the main cause is primary hemorrhage, then subacute subdural hematoma or chronic can occur with secondary hemorrhage.
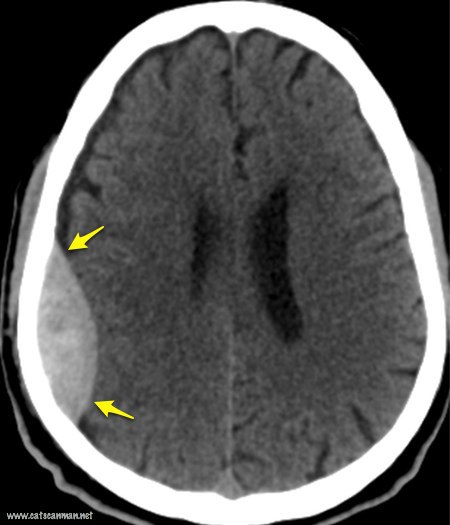
Subdural hematoma in the picture
In addition, there is a danger of developing reverse hemorrhage, which is a bruise formed on the side opposite to the point of impact.
Epidural
An epidural hematoma occurs as a result of a head injury, but in this case the bones of the skull are depressed, which explains the location of the bruise. Unlike the subdural, it almost always forms at the site of the impact, and not on the opposite side.
In addition to local, epidural hematoma of the head can be general - that is, affect several parts of the brain.
Classification:
- acute;
- subacute
No chronic course of this disease was observed.
As a rule, a hematoma is formed due to bleeding from the middle meningeal artery (in most cases) or from the anterior ethmoidal artery, so localization is noted in the temporal and frontal lobes of the brain. Blood accumulates between the skull and the dura mater.

The middle meningeal artery is the largest blood vessel that arises from the maxillary artery
The anterior ethmoidal artery is one of the arteries of the ophthalmic region
Adults are more often susceptible to this hematoma, since young children have structural features of the skull that physically do not allow such hemorrhage to occur.
The volume of accumulated blood averages from 40 to 200 ml, the diameter is usually 7-8 mm.
Localization and area of damage
Epidural hematoma is measured in the following units:
- diameter – in centimeters;
- volume – in milliliters.
Most often, a blood clot has a peculiar shape, resembling a lens. Its volume can vary from 30 to 250 ml. Average indicators include those hematomas that are 100 ml. Due to its special shape, the thickness of the formation in the central part reaches 4 cm, and towards the edges it practically disappears. Since this hematoma is caused by an object with a small traumatic area, it is about 8 cm in diameter. It is most often limited to one or two lobes of the brain. The most common places where this type of hematoma can form are the parietal and temporal regions. In some cases it goes a little beyond their boundaries.
Therapeutic measures
There are two ways to treat epidural hematoma: conservative and surgical.
The first method is suitable for small injuries that are not complicated by brain injuries. The symptoms of mild hematoma are mild.
But most EDHs require surgery. First of all, to relieve pressure, a milling hole is made, through which part of the blood is aspirated; this procedure relieves pressure on the brain. Subsequently, the neurosurgeon performs a craniotomy to completely remove the hematoma, treat the damaged areas and seal or suturing the bleeding vessels.
Postoperative therapy is also important, which includes the removal of edema and neurometabolic treatment. Symptomatic therapy also includes massage, physiotherapy and exercise therapy.
Source of bleeding
Having figured out how an epidural hematoma forms, it is easy to understand what exactly is the source of bleeding. During the strike, deformation of the skull occurs, which leads to rupture of blood vessels. The latter are closely related to the dura mater of the brain. Most often, deformation of the meningeal artery occurs. Less common are cases where bleeding occurs due to rupture of the diploe vessels and meningeal veins. Blood leaving them forms a hematoma, which can lead to cerebral edema.
Etiopathogenesis
Subdural hematomas caused by trauma are called “traumatic.” Subdural hematomas are much more likely than epidural hematomas to be caused by pulsed, diffuse acceleration-deceleration injuries due to the application of rotational or linear forces of different directions, while shaking of intracranial structures contributes to stretching and damage to small bridging veins. Subdural hemorrhage is a classic finding in shaken baby syndrome, which is also characterized by the development of intra- and preretinal hemorrhages caused by the same mechanism of action. In addition, subdural hematomas are typical in elderly people and alcoholics with signs of brain atrophy. Brain atrophy is associated with elongation of the bridging veins, which increases the likelihood of rupture of the latter during impulse trauma. Also, the formation of a subdural hematoma can be facilitated by a decrease in cerebrospinal fluid, and, accordingly, subarachnoid pressure, which leads to divergence of the dura and arachnoid meninges, tension and rupture of the bridging veins. SDH is more often observed in patients taking anticoagulants and antiplatelet agents (warfarin, aspirin).
Risk factors
Childhood and old age increase the likelihood of developing SDH. As brain volume decreases with age, the subdural space expands and the bridging veins become longer and more mobile. This factor, coupled with the fragility of the vessel walls in older people, makes them more susceptible to SDH. Young children also have a wider subdural space than young adults, making them more likely to develop SDH; This accounts for the typical formation of SDH in shaken baby syndrome. In young people, a risk factor for SDH is the presence of arachnoid cysts.
Other risk factors include taking anticoagulants, alcoholism and dementia.
Subacute form
This course of the disease is vaguely similar to the acute form. However, it is characterized by a number of individual symptoms:
- After about 20 minutes there is a light interval. Its duration is up to 12 days.
- Life support functions remain unchanged.
- In rare cases, a jump in blood pressure is observed.
- Symptoms are mild.
- The patient is fully conscious, less often slightly stunned.
- Bruises develop in the fundus.
After the end of the light period, the condition of the injured person deteriorates sharply.
Acute form
An acute epidural hematoma can develop in three ways. There is a bright interval:
- pronounced;
- poorly expressed;
- completely absent.
Most often, the latter option occurs when extensive injuries occur, which cause severe brain damage. In this case, the patient may fall into a coma. As a rule, no positive dynamics are observed. In the acute form, when there is no light gap, there is a high probability of death.
Classification
Subdural hematomas are divided into acute, subacute and chronic, depending on the speed of their formation. Acute SDH of traumatic origin are the most common cause of mortality from TBI and have a high mortality rate in the absence of timely treatment - surgical decompression.
Acute bleeding is often caused by high-velocity acceleration-deceleration trauma, and its severity correlates with the size of the hematoma. The most severe are SDH, combined with brain contusion. Venous hemorrhage in acute SDH develops much faster compared to chronic ones, however, epidural hematomas caused by arterial hemorrhage usually develop even faster. Despite this, mortality rates from acute SDH exceed mortality from epidural hematomas and diffuse brain damage, since acceleration-deceleration trauma, sufficient in strength for the development of SDH, entails other severe injuries. The mortality rate for acute SDH is 60 - 80%.
A chronic subdural hematoma forms over several days or weeks as a result of a lesser trauma, and in 50% of cases patients cannot indicate a history of trauma. Chronic SDH may remain unrecognized for months or even years after injury until clinical manifestations occur. Bleeding from chronic SDH is usually slow or consists of several episodes of minor bruising, and usually stops spontaneously. Small chronic SDH up to 1 cm in thickness have a significantly better prognosis than acute SDH; Thus, one study indicated that only 22% of patients with such chronic hematomas had an outcome worse than “good” or “complete recovery.” Chronic SDH is common in old age.
The light interval is weakly expressed
In severe traumatic brain injuries, the epidural hematoma occurs with a weakly defined light interval. In this form, the patient may fall into a coma with initial loss of consciousness. It lasts several hours. This is followed by the stage of stupor, and after this the patient goes into deep stupor. In this state, maintaining contact with the patient is quite problematic. Doctors observe disruption of life support functions. This form is characterized by the fact that a weakly expressed light interval can last several days. After which the patient again falls into a coma. He may develop paralysis. His condition becomes extremely serious.
Symptoms of spinal epidural hemorrhage
Spinal epidural hemorrhage manifests itself with sharp pain in the part of the spine where the vascular accident occurred. The pain is similar to pain with radiculitis and is caused by irritation of the spinal roots by blood pouring into the epidural space. After a few hours (sometimes minutes), the pain subsides, and spinal conduction disorders come to the fore. Muscle weakness occurs and progresses, reaching the level of plegia below the level of the lesion. There is a decrease in muscle tone, sensory conduction disturbances, and a symmetrical decrease in periosteal and tendon reflexes. Pelvic function disorder is characterized by urinary incontinence.
Features of the clinical picture of hemorrhage depend on its location. In patients over 40 years of age, in the vast majority of cases, epidural hemorrhages are observed in the lumbar and sacral regions, in persons under 40 years of age - in the cervical and thoracic regions. The dorsal localization of the resulting epidural hematomas predominates.
Acute form with a pronounced light gap
Most often, with this type of hematoma, the light gap is clearly visible. This course of the disease is considered classic. It develops as follows:
- Head injury.
- Lucid interval.
- The onset of a sharp deterioration.
If the injury is classified as mild to moderate, the patient may briefly lose consciousness. He has weakness, residual stupor and headache. There are often cases of amnesia. There is a decrease in reflex activity. This condition can last several hours, after which the patient rapidly deteriorates. The following symptoms appear:
- Severe, persistent headaches.
- Repeated vomiting.
- Drowsiness and secondary loss of consciousness.
- Stupor progressing to coma.
- The pupil does not react to light.
- Bradycardia and a sharp increase in blood pressure.
Main manifestations
Epidural hematoma is a problem that develops in three ways. In the classic version, the patient loses consciousness for a while, after which he partially or completely recovers. The patient has:
- headache and dizziness;
- weakness is observed;
- in some cases, memory deteriorates and the person forgets what happened before the injury.
Deterioration in health is observed over several hours. The patient suffers from nausea, attacks of vomiting, increased headaches, and increased agitation. In this case, the patient may lose consciousness again and fall into a coma. The clinical picture gradually develops in the form of:
- increased blood pressure in the arteries;
- respiratory rhythm disturbances;
- increase in heart rate.
With this development of events, the pupil dilates and the eyelid droops on the side where the hemorrhage occurred. On the opposite side, there is an increase in tendon reflexes and the development of muscle weakness. This condition is called pyramidal insufficiency.
If the patient is seriously injured, he quickly loses consciousness and develops into a coma. Relief of the condition does not occur until surgery is performed. In this case, the probability of death of the patient is high.
Diagnostics
If the patient experiences symptoms such as the presence of a light gap, severe pain in the head, contralateral paresis, meningeal edema, a sharp jump in blood pressure, homolateral mydriasis, then a full examination must be carried out without delay.
Diagnosis of epidural hematoma includes magnetic resonance imaging and computed tomography. In order to correctly determine the location of the hematoma, a neurologist and neurosurgeon are consulted. During the examination, doctors look for symptoms of brain damage. Based on them, a complete clinical picture is compiled. In case of severe traumatic brain injury, the patient must undergo an x-ray, thanks to which the presence of a fracture can be determined.
Clinical manifestations
The clinical manifestation of a subdural hematoma has a slower onset than with an epidural hematoma, due to the lower rate of venous bleeding compared to arterial bleeding. The clearly defined “clear gap” that is classic for an epidural hematoma may not be observed; the timing of the manifestation of symptoms varies extremely - both immediately after the injury, within a few minutes, and delayed, after two weeks. In addition, in contrast to the classic “bright gap”, the change in the state of consciousness in SDH is often wave-like and gradual.
When the volume of hemorrhage is sufficient to compress the brain, signs of intracranial hypertension or focal neurological symptoms due to damage to the medulla appear. The clinical picture of SDH is extremely variable. In addition to the volume of the hematoma, its location, etc., the mechanism of injury of acceleration-deceleration with counter-impact is important, which often entails bilateral brain damage.
Impaired consciousness in SDH, in contrast to the manifestations of epidural hematoma, often develops not according to the stem type, but according to the cortical type, and may have amentive, oneiric manifestations, the development of “frontal” symptoms with decreased criticism, absurd behavior, etc. is typical. excitement, a typical wavy headache with a meningeal tint or a hypertensive nature, increased headache is accompanied by vomiting. Epileptic seizures occur, often generalized. In half of the cases bradycardia is observed. There are congestion in the fundus, with chronic SDH - with elements of atrophy of the optic nerve nipple. The combination of SDH with severe brain contusion may be accompanied by brain stem disorders such as respiratory and hemodynamic disorders, diffuse changes in muscle tone and reflex sphere.
Epidural hematoma: treatment
Patients diagnosed with this type of hematoma are treated in two ways: surgical and conservative. The latter method is permissible only if the formation does not exceed 50 ml in volume. The doctor also makes sure that blood clots do not provoke the appearance of compression of brain tissue. Most often, a conservative treatment method consists of prescribing drugs that stop bleeding. These include hemostatic agents. In order to prevent brain swelling, the patient must take diuretics. If the hematoma is accompanied by other symptoms, the doctor prescribes medications to stabilize them. As a rule, craniotomy is not performed on a patient in this condition. The hematoma resolves on its own in about a month.
Surgical intervention for this type of pathology is used in most cases. The patient undergoes osteoplastic or resection trepanation. Thanks to these actions, it becomes possible to quickly reduce pressure on brain structures. And this, in turn, allows you to avoid serious consequences. If there is no bone fracture in the area where the epidural hematoma is located, the operation begins with drilling a burr hole directly on the injured area. Through it, a certain part of the accumulated blood is removed. After this, a full trepanation is performed, thanks to which the surgeon gains access to the hematoma. Having removed it, he ligates the bleeding vessel.
After the operation, the patient is prescribed special drug treatment. It includes drugs that eliminate soft tissue swelling. Thanks to targeted treatment, it is possible to minimize the risk of developing severe complications. The recovery period itself lasts up to 6 months. During this time, the patient must observe bed rest and a specially designed diet.
Characteristic symptoms
With an epidural hematoma, characteristic signs are observed that cannot be ignored. The peculiarity of this pathology is that there is a certain period after the injury, during which the person feels normal. As a rule, it ranges from 30 minutes to several hours. Then a sudden loss of consciousness occurs and characteristic symptoms immediately appear.
Specific manifestations depend on how severe the injury was, as well as on the individual characteristics of the patient. There are a number of signs that are most often found with epidural hematoma.
You cannot delay after detecting symptoms, because this will lead to complications and negative consequences. You should not expect that negative manifestations will go away on their own over time; you should immediately consult a doctor.
Symptoms:
- Intense dizziness.
- General weakness and high fatigue.
- Nausea and vomiting.
- Memory loss. It can be either short-term or long-term.
- Soreness in the head.
- High blood pressure.
- Emotional overexcitement.
- Loss of consciousness and coma.
- Speech impairment, a person cannot pronounce certain letters or sounds.
- Numbness of the limbs and paralysis.
- Cramps.
In this case, the patient’s pupils often dilate, and the eyelid droops on the side where the epidural hematoma is located. At the same time, weakness in the muscles is observed in the opposite area.
To make an accurate diagnosis, it is not enough to know the characteristic symptoms. It is imperative to undergo professional diagnostics to clarify the pathology and determine treatment methods.
Epidural hematoma: consequences and prognosis
According to statistics, death from this disease occurs in 25% of cases. The reason for this high mortality rate is the delay in making an accurate diagnosis. Incorrect treatment can lead to the death of the patient. Serious consequences can only be avoided if all necessary measures have been taken in a timely manner.
A positive prognosis is possible in almost 100% of cases for small hematomas. Most patients experience complete recovery of all neurological functions. But it is impossible to completely get rid of headaches. They also notice impaired vision and mental abilities, and their memory deteriorates significantly.
If a patient with a large hematoma of this type has undergone craniotomy, a favorable outcome is possible in approximately 40% of cases. As a rule, in these patients, all impaired functions that were a result of the impact of trauma on the brain are not restored.
Rehabilitation and prognosis
Rehabilitation after surgery to remove a hematoma includes:
- stay in the intensive care unit (postoperative care is provided here, vital signs are monitored);
- assessment of pupil reaction, identification of neurological disorders (performed after the cessation of anesthesia);
- conducting a general blood test (helps identify signs of postoperative anemia and water-electrolyte imbalance);
- intravenous infusion of saline and glucose (aimed at preventing dehydration and exhaustion of the body; after the patient switches to independent nutrition, the infusion is stopped);
- performing breathing exercises to prevent congestion in the lungs;
- administration of antibacterial and painkillers;
- removal of surgical staples (performed on the 7th day after trepanation, before this time you cannot wash your hair).
Important information: How to get rid of a bruise after an injection into a vein and what to do to remove the hematoma
When the operation is performed in the first hours after injury, no dangerous complications arise. Without treatment, the prognosis becomes unfavorable. Acute hematoma is fatal in 60% of cases. When brain tissue is damaged, paralysis and paresis of the limbs occur.