Great Soviet Encyclopedia. - M.: Soviet Encyclopedia. 1969—1978.
SUBCORTAL STRUCTURES OF THE BRAIN - parts of the brain located between the cerebral cortex and the medulla oblongata. They have an activating effect on the cortex, participate in the formation of all behavioral reactions in humans and animals, in maintaining muscle tone, etc. ... Big Encyclopedic Dictionary
subcortical brain structures - sections of the brain located between the cerebral cortex and the medulla oblongata. They have an activating effect on the cortex, participate in the formation of all behavioral reactions in humans and animals, in maintaining muscle tone, etc. * ... ... Encyclopedic Dictionary
SUBCORTAL STRUCTURES OF THE BRAIN - parts of the brain located between the cerebral cortex and the medulla oblongata. They have an activating effect on the cortex, participate in the formation of all behavioral reactions of humans and animals, in maintaining muscle tone, etc. ... Natural history. encyclopedic Dictionary
subcortex (subcortical structures of the brain) - a part of the brain located between the cerebral cortex and the medulla oblongata. It includes: the optic thalamus, hypothalamus, limbic system and other basal ganglia, reticular formation of the brain stem, thalamus. P. participates ... Encyclopedic Dictionary of Psychology and Pedagogy
Subcortical functions are a set of physiological processes associated with the activity of individual subcortical structures of the brain (See Subcortical structures of the brain) or with their system. From an anatomical point of view, all ganglion formations are classified as subcortical,... ... Great Soviet Encyclopedia
SUBCORTICAL FUNCTIONS - SUBCORTICAL FUNCTIONS. The doctrine of the functions of P. formations, developed on the basis of anat. clinical (mostly) comparative anatomical and experimental physiological studies, dates back many years and cannot be considered as ... Big Medical Encyclopedia
The cerebral cortex is a layer of gray matter 1–5 mm thick that covers the cerebral hemispheres of mammals and humans. This part of the brain (See Cerebrum), which developed in the later stages of the evolution of the animal world, plays exclusively... ... Great Soviet Encyclopedia
Cerebral cortex - Central nervous system (CNS) I. Cervical nerves. II. Thoracic nerves. III. Lumbar nerves. IV. Sacral nerves. V. Coccygeal nerves. / 1. Brain. 2. Diencephalon. 3. Midbrain. 4. Bridge. 5. Cerebellum. 6. Medulla oblongata. 7.… …Wikipedia
Prefrontal cortex - Prefrontal cortex ... Wikipedia
HIGHER NERVOUS ACTIVITY - (HNI), integrative activity of the highest. departments center nervous system (CNS), which provides behavior, i.e. optimal adaptation of the body as a whole to external conditions. to the world. The structural basis of the GNI in all mammals (including humans) is the cortex... ... Russian Pedagogical Encyclopedia
Demyelination of the brain
The demyelinating process is a pathological condition in which the myelin of the white matter of the nervous system, central or peripheral, is destroyed. In this case, myelin is replaced by fibrous tissue, which leads to a disruption in the transmission of impulses along the brain pathways. This disease is an autoimmune disease and in recent years there has been a tendency to increase its frequency. The number of cases of detection of this disease in children and people over 45 years of age is also increasing; more and more diseases are being observed in geographical regions that were not typical for them. Research conducted by leading scientists in the fields of immunology, neurogenetics, molecular biology and biochemistry has made the development of this disease more clear, which makes it possible to develop new technologies for its treatment.
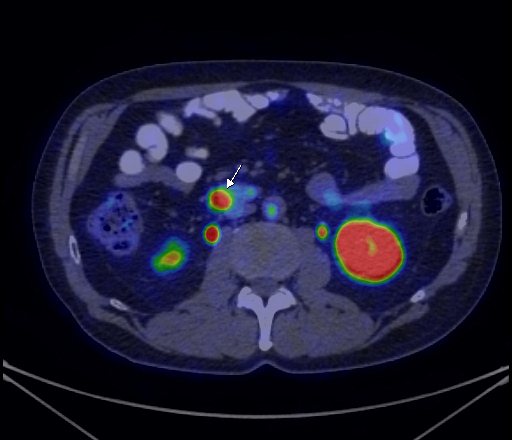
Question No. 6. What is an SUV?
SUV (Standardized Uptake Value)
is a value that reflects the intensity of radiopharmaceutical accumulation in the area of interest, for example, in a tumor.
The SUV indicator is calculated automatically by the software and measured in various units. In our Center, as in most domestic and foreign medical institutions where positron emission tomography is performed, it is customary to use g/ml as units for measuring SUV.
| 18F-FDG PET/CT data. Outlining a metabolically active malignant tumor of the left lung to measure SUV. In this case, the SUV value in the tumor is determined at the level of 13.52 g/ml. |
Causes
Demyelinating brain disease can develop for a number of reasons, the main ones are listed below.
- An immune reaction to proteins that make up myelin. These proteins begin to be perceived by the immune system as foreign and are attacked by it, resulting in their destruction. This is the most dangerous cause of the disease. The trigger for the launch of such a mechanism can be an infection or innate characteristics of the immune system: multiple encephalomyelitis, multiple sclerosis, Guillain-Barré syndrome, rheumatic diseases and chronic infections.
- Neuroinfection: Some viruses can attack myelin, resulting in demyelination of the brain.
- Failure in the metabolic mechanism. This process may be accompanied by disruption of myelin nutrition and its subsequent death. This is typical for pathologies such as thyroid diseases and diabetes.
- Intoxication with chemicals of various types: alcohol, narcotics, strong psychotropic substances, poisonous substances, paint and varnish products, acetone, drying oil, or poisoning with waste products of one’s own body: peroxides, free radicals.
- Paraneoplastic processes are pathologies that are a complication of tumor processes. Recent studies confirm that the interaction of environmental factors and hereditary predisposition play an important role in triggering the mechanism of this disease. A connection has been established between geographic location and the likelihood of the disease occurring. In addition, viruses (rubella, measles, Epstein-Barr, herpes), bacterial infections, eating habits, stress, and the environment play an important role.
This disease is classified into two types:
- myelinoclasty – a genetic predisposition to accelerated destruction of the myelin sheath;
- myelinopathy – destruction of the myelin sheath, already formed, as a result of any reasons not related to myelin.
The demyelinating process of the brain itself does not produce any clear symptoms. They completely depend on in which structures of the central or peripheral nervous system the given pathology is localized. There are three main demyelinating diseases: multiple sclerosis, progressive multifocal leukoencephalopathy and acute disseminated encephalomyelitis.
Multiple sclerosis is the most common disease among these, characterized by damage to several parts of the central nervous system. This is accompanied by a wide range of symptoms. The onset of the disease manifests itself at a young age - about 25 years and is more common in women. Men get sick less often, but the disease manifests itself in a more progressive form. Symptoms of multiple sclerosis are conventionally divided into 7 main groups.
- Damage to the pyramidal tract: paresis, clonus, weakened skin and increased tendon reflexes, spastic muscle tone, pathological signs.
- Damage to the brain stem and cranial nerves: horizontal, vertical or multiple nystagmus, weakening of facial muscles, internuclear ophthalmoplegia, bulbar syndrome.
- Pelvic organ dysfunction: urinary incontinence, urge to urinate, constipation, potency disorders.
- Damage to the cerebellum: nystagmus, ataxia of the trunk, limbs, asynergia, muscle hypotonia, dysmetria.
- Visual impairment: loss of acuity, scotomas, impaired color perception, changes in visual fields, disturbances in brightness and contrast.
- Sensory disturbances: distortion of temperature perception, dysesthesia, sensitive ataxia, sensation of pressure in the extremities, distortion of vibration sensitivity.
- Neuropsychological disorders: hypochondria, depression, euphoria, asthenia, intellectual impairment, behavioral disorders.
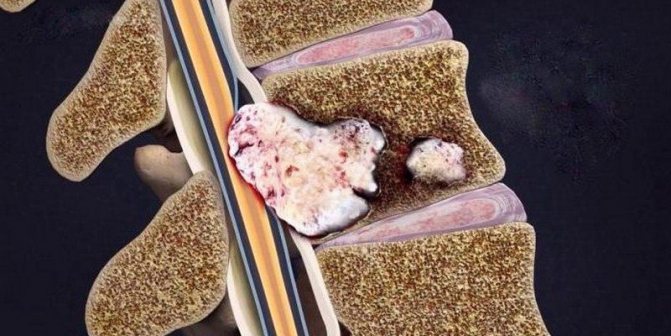
Symptoms of metastasis
One of the first causes of concern is pain. It can be piercing or oppressive in nature, appear locally or extend beyond the affected area. Pain of low intensity resembles the symptoms of osteochondrosis, but is rapidly progressive and more persistent. At the beginning, the pain is insignificant and is provoked by turning the neck, tapping the vertebrae, raising the leg in a straightened state, etc.
In subsequent stages, metastases provoke severe pain that does not stop even at rest or after drug anesthesia. The most common sensations are:
- Pain radiating to the arms (when affecting the neck) or legs (with metastases of the lumbar, sacral). Radicular syndrome manifests itself as an electric shock, lumbago or burning sensation. If the chest area is affected, the pain surrounds the torso;
- Aching pain caused by a local inflammatory process or anatomical sprains;
- When metastasis occurs in the spinal column, its walls become thinner and weakened. In the absence of adequate treatment, this can lead to fractures. They are recognized by the sudden onset of pain, aggravated by pressure.
A typical symptom of spinal metastases is pain that gets worse at night. When examined by a neurologist, tests for the presence of Neri's symptom and Minor's landing give positive results.
Increased degradation of bone tissue often causes hypercalcemia, which manifests itself in weakness, lethargy, unstable mood, cognitive impairment, memory impairment, poor appetite, arrhythmia, and hypertension. All this aggravates the patient's condition. Also among the symptoms of metastases located outside the spinal column, primary neoplasia is observed.

Diagnostics
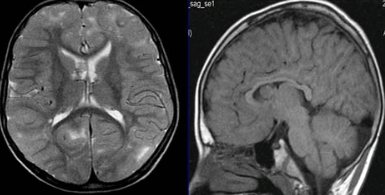
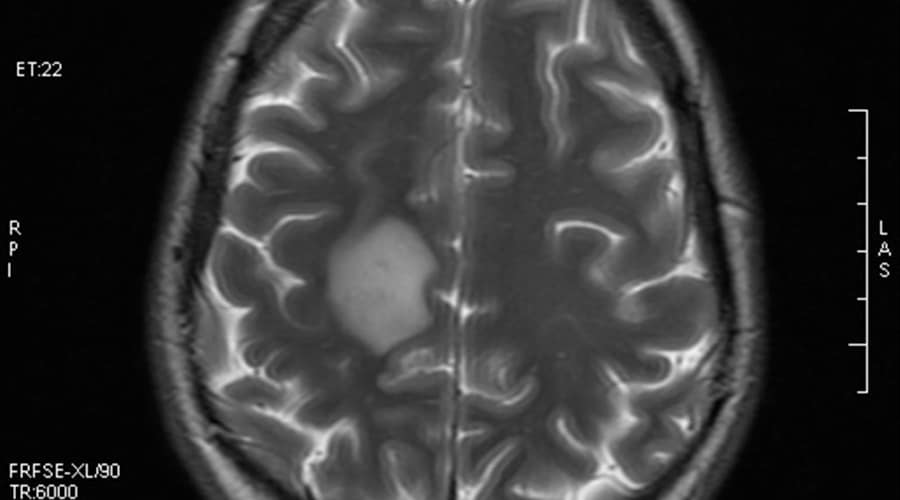
The most revealing research method that can identify foci of demyelination of the brain is magnetic resonance imaging.
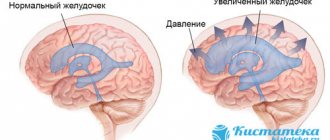
A characteristic picture for this disease is the identification of oval or round foci measuring from 3 mm to 3 cm in any part of the brain. Typical localization for this pathology is the area of the subcortical and periventricular zones. If the disease lasts for a long time, these lesions may merge. MRI also shows changes in the subarachnoid spaces and an enlargement of the ventricular system due to brain atrophy. Relatively recently, the evoked potential method began to be used to diagnose dimyelinating diseases. Three indicators are assessed: somatosensory, visual and auditory. This makes it possible to evaluate disturbances in the conduction of impulses in the brain stem, visual organs and spinal cord.
Electroneuromyography shows the presence of axonal degeneration and allows you to determine myelin destruction. Also, using this method, a quantitative assessment of the degree of autonomic disorders is made.
Oligoclonal immunoglobulins contained in the cerebrospinal fluid are subjected to immunological studies. If their concentration is high, this indicates the activity of the pathological process.
Measures for the treatment of demyelinating diseases can be specific and symptomatic. New research in medicine has made good progress in specific treatment methods. Beta interferons are considered one of the most effective drugs: these include Rebif, Betaferon, Avanex. Clinical studies of betaferon have shown that its use reduces the rate of disease progression by 30%, prevents the development of disability and reduces the frequency of exacerbations.
Experts increasingly prefer the method of intravenous administration of immunoglobulins (bioven, sandoglobulin, venoglobulin). In this way, exacerbations of this disease are treated. More than 20 years ago, a new, quite effective method for treating demyelinating diseases was developed - immunofiltration of cerebrospinal fluid. Research is currently underway on drugs whose action is aimed at stopping the demyelination process.
Corticosteroids, plasmapheresis, and cytostatics are used as specific treatments. Nootropics, neuroprotectors, amino acids, and muscle relaxants are also widely used.
Why does it occur
Hypodense formations in organs can appear as a result of the development of benign or malignant diseases. Among the most common provoking factors are the following conditions.
The neoplasm can be congenital, acquired, parasitic or inflammatory in nature. The tumor is presented in the form of a liquid, the cavity of which contains translucent liquid. The size can range from a few millimeters to 25 centimeters.
Also refers to benign formations formed from adipose tissue. The diameter of the tumor does not exceed 50 millimeters. To monitor the pathological process, an ultrasound examination is performed.
It is characterized by slow growth and almost never degenerates into a malignant form. If there is a rapid increase in volume, then additional diagnostics will be required.
Has some similarities with cystic formations. The peculiarity of such a tumor is that it has several chambers, which are separated from each other by a lined epithelium.
The presence of hypodense formations can also be caused by other benign neoplasms, abscesses, oncological pathologies (lymphoma, hemangiosarcoma, hepatoma, cholangiocarcinoma), primary cancer tumors, metastasis.
To determine which disease the described lesions indicate, an additional diagnostic examination is prescribed. As a rule, this is a biopsy, various blood tests, as well as other techniques that make it possible to more accurately determine the nature of the pathological process.
Metastases in the spine account for more than 90% of the total number of bone malignant neoplasms. The main negative feature is their multiple nature. Secondary lesions provoke fractures of varying complexity and severe pain.
The disease significantly impairs the quality and reduces life expectancy. That is why, at any hint of similar symptoms, you should immediately seek qualified medical help and undergo a comprehensive examination.
Symptoms and causes of gliosis foci in the white matter
Lesions in the white matter of the brain are areas of damage to brain tissue, accompanied by a violation of the mental and neurological functions of higher nervous activity. Focal areas are caused by infection, atrophy, loss of blood supply and trauma. Most often, affected areas are caused by inflammatory diseases. However, areas of change may also be of a dystrophic nature. This is observed mainly as a person ages.
Focal changes in the white matter of the brain can be local, single-focal, or diffuse, that is, the entire white matter is moderately affected. The clinical picture is determined by the localization of organic changes and their degree. A single lesion in the white matter may not affect the dysfunction, but massive damage to neurons causes a disruption in the functioning of nerve centers.
The set of symptoms depends on the location of the lesions and the depth of damage to the brain tissue. Symptoms:
- Pain syndrome. Characterized by chronic headaches. Unpleasant sensations intensify as the pathological process deepens.
- Rapid fatigue and exhaustion of mental processes. Concentration deteriorates, the volume of operative and long-term memory decreases. It is difficult to master new material.
- Flattening of emotions. Feelings lose their sharpness. Patients are indifferent to the world and lose interest in it. Previous sources of pleasure no longer bring joy and desire to engage in them.
- Sleep disturbance.
- In the frontal lobes, foci of gliosis disrupt the control of the patient’s own behavior. With deep violations, the concept of social norms may be lost. Behavior becomes provocative, unusual and strange.
- Epileptic manifestations. More often these are small convulsive seizures. Individual muscle groups contract involuntarily without threat to life.
Question No. 2. What is a radiopharmaceutical?
Radiopharmaceutical (RP)
is a compound consisting of a special substance and a radionuclide (isotope, radionuclide label). A special substance is responsible for the organ in which radiopharmaceuticals accumulate, and the radionuclide tag allows the diagnostician to see this accumulation in the image.
Currently, a very wide range of both special substances and radionuclide labels is used for the production of radiopharmaceuticals. Worldwide, the most commonly used special substance and radionuclide tracer compound in cancer patients is 18F-fluorodeoxyglucose (18F-FDG). In this compound, 18F acts as a radionuclide label, while FDG acts as a special substance.
At-risk groups
Risk groups include people exposed to the following factors:
- Arterial hypertension. They are at increased risk of developing vascular lesions in the white matter.
- Poor nutrition. People who overeat, excessively consume extra carbohydrates. Their metabolism is disrupted, as a result of which fatty plaques are deposited on the inner walls of blood vessels.
- Foci of demyelination in the white matter appear in older people.
- Smoking and alcohol.
- Diabetes.
- Sedentary lifestyle.
- Genetic predisposition to vascular diseases and tumors.
- Constant hard physical labor.
- Lack of intellectual work.
- Living in conditions of air pollution.
Treatment of metastases in the spine
Among the main areas of treatment are:
- Minimizing pain;
- Preventing compression of the spinal canal and collapse;
- Maintaining normal functioning of the central nervous system;
- Palliative care.
Methods used include drug therapy with diphosphonates and chemotherapy drugs, hormonal and radiation therapy, and surgical interventions. The need for radiotherapy and chemotherapy is determined by the sensitivity of the primary lesion. Diphosphonates help suppress hypercalcemia and minimize bone degradation.
Depending on the patient’s condition and prognosis, surgical intervention is divided into 2 types: decompressive (laminectomy), decompressive-stabilizing. Laminectomy excision has a relatively simple procedure and is well tolerated by cancer patients. The main disadvantage is the high percentage of relapses.
DSOs involve the use of implants, autografts, and fixatives and provide a longer-term effect. This type of intervention is quite traumatic and contraindicated in cases of developing decompensation of vital functions or significant dissemination of lesions.
Treatment and diagnosis
The main way to find multiple lesions is to visualize the medulla on magnetic resonance imaging. On layer by layer
Spots and pinpoint changes in tissue are observed in the images. MRI shows not only lesions. This method also reveals the cause of the lesion:
- A single lesion in the right frontal lobe. The change indicates chronic hypertension or a previous hypertensive crisis.
- Diffuse foci throughout the cortex appear when the blood supply is disrupted due to atherosclerosis of the cerebral vessels or.
- Foci of demyelination of the parietal lobes. It speaks of a disruption in the flow of blood through the vertebral arteries.
- Massive focal changes in the white matter of the cerebral hemispheres. This picture appears due to atrophy of the cortex, which forms in old age, from Alzheimer's disease or Pick's disease.
- Hyperintense lesions in the white matter of the brain appear due to acute disruption of the blood supply.
- Small foci of gliosis are observed in epilepsy.
- In the white matter of the frontal lobes, single subcortical foci are predominantly formed after a heart attack and softening of the brain tissue.
- A single focus of gliosis in the right frontal lobe most often appears as a sign of brain aging in older people.
Magnetic resonance imaging is also performed on the spinal cord, in particular on the cervical and thoracic regions.
Related research methods:
Visual and auditory evoked potentials. The ability of the occipital and temporal regions to generate electrical signals is tested.
Lumbar puncture. Changes in the cerebrospinal fluid are examined. Deviation from the norm indicates organic changes or inflammatory processes in the cerebrospinal fluid ducts.
A consultation with a neurologist and psychiatrist is indicated. The first studies the functioning of tendon reflexes, coordination, eye movements, muscle strength and synchrony of extensor and flexor muscles. The psychiatrist examines the patient’s mental sphere: perception, cognitive abilities.
Foci in the white matter are treated with several branches: etiotropic, pathogenetic and symptomatic therapy.
Etiotropic therapy is aimed at eliminating the cause of the disease. For example, if vasogenic lesions of the white matter of the brain are caused by arterial hypertension, the patient is prescribed antihypertensive therapy: a set of drugs aimed at lowering blood pressure. For example, diuretics, calcium channel blockers, beta blockers.
Pathogenetic therapy is aimed at restoring normal processes in the brain and eliminating pathological phenomena. Drugs are prescribed that improve blood supply to the brain, improve the rheological properties of blood, and reduce the need for oxygen in brain tissue. Vitamins are used. To restore the functioning of the nervous system, it is necessary to take B vitamins.
Symptomatic treatment eliminates symptoms. For example, for seizures, antiepileptic drugs are prescribed to eliminate foci of excitation. In case of low mood and lack of motivation, the patient is given antidepressants. If lesions in the white matter are accompanied by an anxiety disorder, the patient is prescribed anxiolytics and sedatives. If cognitive abilities deteriorate, a course of nootropic drugs is indicated - substances that improve the metabolism of neurons.
Norm of magnetic resonance imaging
What does “normal on an MRI of the brain” mean? These are the results of an MRI of a healthy person. Data is assessed according to several parameters:
- structures are developed correctly and fully, there are no displacements;
- Magnetic resonance signal is normal;
- the gyri and sulci are normal, do not have inclusions, inflammation or changes in structure;
- parts of the brain such as the sella turcica and the pituitary gland are clearly visible and have no pathologies;
- the perivascular, subarachnoid space is developed normally and has no pathologies;
- the ventricular system has normal standard dimensions (neither enlarged nor reduced), there are no pathologies;
- the ear canals, nasal sinuses, and eye sockets are clearly visualized, have normal sizes and regular shapes;
- general assessment is when there are no focal changes, brain tissue is developed normally, brain vessels are of the correct shape, do not have diffuse changes, are evenly filled, there are no bleeding, blood clots and purulent formations of various sizes.
Related and recommended questions
Please help me understand what kind of diagnosis this could be?
The study was carried out on: Magnetic resonance imaging scanner GE Optima MR360 Area of study: brain Study: Primary Contrast agent: Magnevist 469.01 mg/ml 20 ml Projection: tra, sag, cor Protocol: On the obtained images of sub- and supratentorial structures of the brain in In the frontal and parietal lobes of both hemispheres, multiple subcortical and periventricular lesions with a diameter of 3-7 mm are detected, without signs of perifocal edema (slightly hyperintense on T2 FLAIR and T2 WI, isointense on T1 WI and DWI, not accumulating contrast agent). No other focal changes in the MR signal were detected in the substance of the cerebral hemispheres, brainstem, corpus callosum and cerebellum. After intravenous contrast, no areas of pathological contrast enhancement were detected in the brain substance and meninges. The paranasal sinuses are pneumatized. Conclusion: Multiple lesions, probably of vascular origin, in the white matter of the frontal and parietal lobes of both cerebral hemispheres. Cavity Verge.
THANK YOU SO MUCH IN ADVANCE FOR YOUR REPLY!
Good afternoon. I have been having problems with my eyes for six months. The right eye is especially affected - in the morning, when pressing on the eyeballs (which happens when washing), there is severe pain and lacrimation, which goes away after 2-3 hours. Vision in the right eye dropped by 1.5 diopters to -5.25. The ophthalmologists prescribed treatment with antibiotics and Kornegel. For some time (a month) the symptoms subsided. But now everything is repeating itself again. The neurologist prescribed vascular injections and Cavinton under the tongue. He recommended doing an MRI. Attached are the MRI results. Please clarify, can the pathology detected on MRI cause such symptoms?
Thank you for your answer Alexander Anatolyevich.
Inside the eye pressure is within normal limits, but in the right eye it is always higher than in the left. And it changes. In the acute period on the right - 20, on the left - 18. During the period of absence of symptoms - 15 and 13. Over the course of 2 months, they were measured 3 times. Yesterday the doctor said that the outbreak is not terrible. We scrolled through all the scans - it is not visible in all projections. It is possible, he says, that this is an artifact, possibly a signal from the bones of the skull. I would like to know your opinion - is the prescribed treatment with Cortexin, Cereton and Cavinton adequate? And my next steps? Is it necessary to retake the MRI? and after what period? Or if there is an outbreak, will it never go away? Thank you.
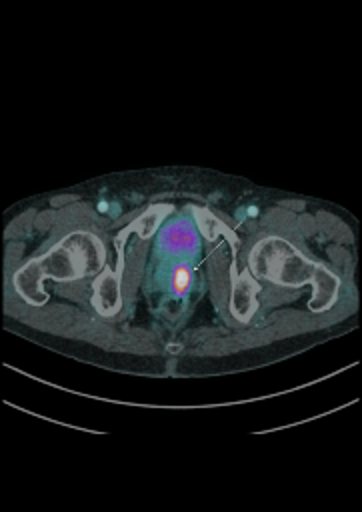
Question No. 4. What is pathological accumulation of radiopharmaceuticals?
Pathological accumulation of radiopharmaceuticals
– this is an increased accumulation of radiopharmaceuticals in organs and tissues, recorded in diseases, most often in malignant tumors.
|
| 68Ga-DOTA-TATE PET/CT findings in a patient with a neuroendocrine tumor of the jejunum. In the projection of a malignant tumor located in the jejunum, a focus of pathological hyperfixation of radiopharmaceuticals is determined. |
| 11C-choline PET/CT findings in a patient with prostate cancer. Condition after prostatectomy. Multiple foci of pathological accumulation of radiopharmaceuticals (metastases) are visualized in the skeletal bones. |
| ||
| 68Ga-PSMA PET/CT data in a patient with local recurrence of prostate cancer. Condition after radiation therapy. In the left parts of the prostate gland, a focus of pathological accumulation of radiopharmaceuticals is determined. | ||
Demyelination
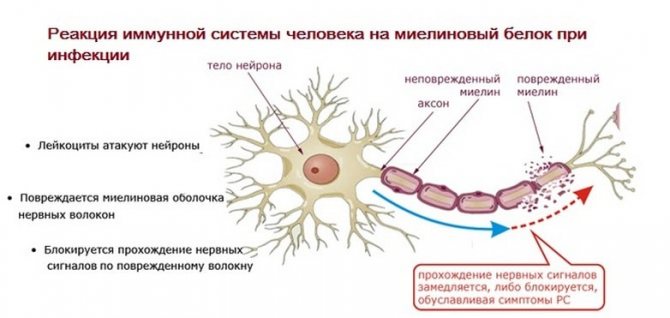
What demyelination of the brain is will become clear if we briefly talk about the anatomy and physiology of a nerve cell.
Nerve impulses travel from one neuron to another, to organs, through a long extension called an axon. Many of them are covered by a myelin sheath (myelin), which ensures rapid transmission of impulses. It consists of 30% proteins, the rest of its composition is lipids.
Development mechanism
In some situations, the myelin sheath is destroyed, which indicates demyelination. Two main factors lead to the development of this process. The first is associated with genetic predisposition. Without the influence of any obvious factors, some genes initiate the synthesis of antibodies and immune complexes. The antibodies produced are able to penetrate the blood-encephalitis barrier and cause myelin destruction.

Another process is based on infection. The body begins to produce antibodies that destroy the proteins of microorganisms. However, in some cases, the proteins of pathological bacteria and nerve cells are perceived as the same. Confusion occurs and the body attacks its own neurons.
At the initial stages of damage, the process can be stopped and reversed. Over time, the destruction of the membrane reaches such an extent that it completely disappears, exposing the axons. The substance for transmitting impulses disappears.
The following main causes underlie demyelinating pathologies:
- Genetic. Some patients have mutations in the genes responsible for the proteins of the myelin sheath, immunoglobulins, and the sixth chromosome.
- Infectious processes. They are triggered by Lyme disease, rubella, and cytomegalovirus infections.
- Intoxication. Long-term use of alcohol, drugs, psychotropic substances, exposure to chemical elements.
- Metabolic disease. As a result of diabetes mellitus, the nutrition of nerve cells occurs, which leads to the death of the myelin sheath.
- Neoplasms.
- Stress.
Recently, more and more scientists believe that the mechanism of origin and development is of a combined nature. Against the background of hereditary conditions under the influence of the environment and pathologies, demyelinating diseases of the brain develop.
It is noted that most often they occur in residents of Europe, some areas of the USA, the center of Russia and Siberia. They are less common in the population of Asia, Africa, and Australia.
General symptoms

When a metastasis appears, the supporting function of the vertebra is disrupted, it begins to gradually collapse, and pain occurs, which is either constant, intense, or occurs during physical activity.
The pain is located in the part of the spine where the lesion is located and does not shoot to other places. Due to a violation of the structure of the vertebra, pathological fractures develop, after which the pain becomes intense, constant and shoots along the nerve roots due to compression by the broken vertebra.
Symptoms of cancer intoxication that aggravate the patient’s condition and worsen the prognosis include:
- weakness;
- increased fatigue;
- weight loss;
- lack of appetite;
- nausea;
- vomiting of eaten food;
- low-grade body temperature;
- swelling on the face in the mornings, on the legs in the evenings;
- headache;
- decreased memory, attention;
- pale or yellow skin;
- decrease in the level of hemoglobin, red blood cells in the blood, increase in ESR.
The following symptoms indicate metastases of the cervical spine:
- pain in the back of the neck, shooting into one or both arms;
- disturbance of movements of the arms and legs with subsequent paralysis in them;
- urinary disturbance;
- loss of sensation in the arms and legs.

It is difficult to identify thoracic metastases, because in the early stages of the disease the symptoms are nonspecific and manifest as unpleasant sensations in the thoracic spine.
Fractures of the thoracic vertebral bodies do not immediately manifest themselves as severe pain, since the chest is a rib frame and compression of the roots occurs in advanced stages of the disease.
When malignant neoplasms appear in the thoracic segments, sensitivity decreases from the level of the chest and below to the legs, the pain has a girdling character along the intercostal nerves, simulating intercostal neuralgia.
Weakness gradually develops in the legs, difficulty urinating and irregular bowel movements.
Metastases to the bodies of the upper lumbar vertebrae cause muscle atrophy and weakness in the legs. There is severe pain in the lumbar region, which shoots into the hip joints, thigh to the level of the knee joint.
Complaints about the joints force patients to treat arthrosis of the hip joints.
If the lower lumbar and sacral regions are affected, the early signs will be pain in the lower back, as with radiculitis.
Then comes numbness of the perineum, incontinence or retention of urine and feces, impaired skin nutrition is manifested by dry and brittle nails, the appearance of cracks, and non-healing wounds.
Metastases of the lower sacral segments manifest themselves:
- urinary disorders,
- bowel movements and sexual function,
- impaired sensitivity of the perineum.
Pain in the spine first appears when no one thinks about the primary tumor. Blood and urine tests are normal, the patient’s well-being is not affected, movements and sensitivity are not impaired. Then the patient’s oncological history and additional examination methods help for diagnosis.
Classification
When describing demyelination, doctors talk about myelinoclasty - a violation of the membrane of neurons due to genetic factors.
Lesions that appear due to diseases of other organs indicate myelinopathy.
Pathological foci occur in the brain, spinal cord, and peripheral parts of the nervous system. They may be generalized in nature - in this case, the damage affects the membranes in various parts of the body. When isolated, the lesion is observed in a limited area.
Supratentorial lesions
They belong to the upper parts of the brain, in contrast to the subtentorial ones, which include the cerebellum and brain stem.
The occipital lobe, located above the tentorium, most often suffers from head bruises and birth injuries due to the fact that it is surrounded on all sides by the fluid of the cerebrospinal fluid spaces, which is incompressible upon impact. In this lobe, glial growths of vascular origin, not associated with injuries, most often occur.
According to the extent and prevalence, supratentorial gliosis is:
- Focal – localized in the form of a large single proliferation of neuroglial cells;
- Few (the term is used to reflect the presence of 2-3 lesions);
- Multiple, which is characterized by the presence of more than 3 hyperdense formations;
- Diffuse (multi-focal), affecting various parts of the brain. The number of small lesions in this case cannot be counted.
The clinical picture of the disease correlates with the number of dead neurons and the size of the lesion. A small formation of neuroglia may not make itself known.
Diseases
In medical practice, there are several diseases characterized by demyelinating processes in the brain.
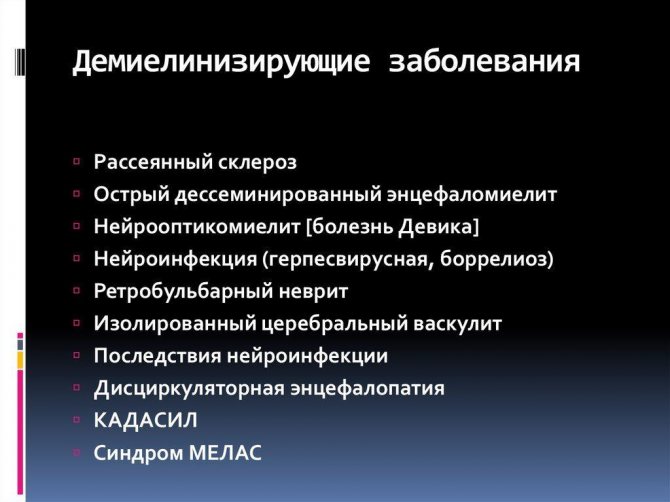
These include multiple sclerosis - in this form they occur most often. Other manifestations include Marburg and Devic pathologies, progressive multifocal leukoencephalopathy, and Guillain-Barré syndrome.
Multiple sclerosis
Approximately 2 million of the world's population suffers from multiple sclerosis. In more than half of the cases, the pathology develops in people between 20 and 40 years old. It progresses slowly, so the first signs are detected only after several years. Recently, it has been diagnosed in children aged 10 to 12 years. It occurs more often in women and city residents. More people living away from the equator get sick.
Diagnostics
The main method for detecting foci of brain demyelination is magnetic resonance imaging. It allows you to get an accurate picture of the disease. The introduction of a contrast agent delineates them more clearly, making it possible to highlight new lesions in the white matter of the brain.
Other testing methods include blood samples and cerebrospinal fluid testing.
Life expectancy for metastases in the spine
Primary neoplasms develop over a fairly long period. Secondary tumor formations appear already in incurable stages and are of a diametrically opposite nature, therefore in most situations they have an unfavorable prognosis.
Life expectancy with metastases in the spine largely depends on:
- Immune system;
- The severity of the patient's condition;
- Number of lesions;
- Types of neoplasms;
Metastasis to the spine has minimal survival rates. Even with the use of all available treatment regimens, in 90% of cancer cases, life expectancy rarely exceeds 24 months. On average it varies from 6 months to a year. If the localization of the neoplasm that appears initially is not established, patients live for about two months.
Despite this, the duration and quality of life should be predicted individually in each case.
It is worth remembering that the earlier the disease is detected, the more positive the prognosis will be. For example, adequate treatment (abdominal resection and vertebrectomy) of a single spinal metastasis predicts five-year survival in 50% of cases.
Favorable prognostic factors include slow growth and small size of the primary tumor, the presence of signs of sclerosis on X-rays, and the good condition of the patient.
In cancers of the breast, thyroid gland, kidneys, lungs, ovaries, prostate glands, and adrenal glands, metastases appear in the spine.
With a minimal degree of malignancy of the primary tumor, metastases appear decades after treatment for cancer of the uterus, stomach, and colon.
Sarcoma of the nasopharynx, lymphosarcoma, tumors of soft tissues, synovial membranes, lymphogranulomatosis, and myeloma metastasize to the spine.
The clinical picture is nonspecific. The pain does not appear immediately and it is important to regularly monitor whether lesions have appeared.
- Definition of the concept and mechanism of appearance
- General symptoms
- Clinical picture of lesions of the cervical spine
- Clinical picture of damage to the thoracic spine
- Clinical picture of lesions of the lumbar spine
- Clinical picture of damage to the lumbosacral spine
- Diagnosis of metastases
- Additional examination methods:
- Treatment of metastases
- Side effects of radiation therapy:
- Side effects of treatment with bisphosphonates:
- Folk remedies in the treatment of metastases
- Surgical methods of treatment
- Treatment prognosis
- Prevention