Etiology and pathogenesis of optic neuritis
The disease is provoked by inflammatory processes of the eyeball (retinitis, keratitis, iridocyclitis, panophthalmitis), orbit (periostitis, phlegmon) and brain (meningitis, arachnoiditis, encephalitis). The disease can also be provoked by infectious lesions of the nasopharynx: frontal sinusitis, sinusitis, tonsillitis, chronic tonsillitis, pharyngitis). Patients with malaria, tuberculosis, ARVI, gonorrhea, and diphtheria are at risk of developing neuritis of the facial nerve.
Common causes of the disease are blood diseases, traumatic brain injuries, alcoholism, diabetes mellitus, gout, and autoimmune disorders. Optic neuritis often occurs in multiple sclerosis. The basis of the disease in this case is the process of destruction of the myelon sheath of nerve fibers. This process is called demyelination. It is not inflammatory, but it is still classified as retrobulbar neuritis due to the similarity of symptoms.
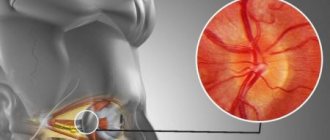
The inflammatory process during neuritis covers both the optic nerve sheath and its trunk. Edema resulting from inflammation and infiltration cause compression of the optic fibers and their subsequent degeneration, which leads to deterioration of vision. After the inflammation is removed, some of the nerve fibers can restore their functions, so vision will improve. In severe cases of pathology, nerve fibers decay in patients. As a result, atrophy of the optic nerve occurs, which leads to irreversible consequences for the patient’s vision.
Types of optic neuritis
In accordance with the localization of the lesion, 2 forms of pathology are distinguished: intrabulbar and retrobulbar neuritis.
The first is characterized by changes in the optic disc and is considered the most common type of disease in children. This form affects the intraocular part of n. Opticus from the level of the retina to the lamina cribrosa.
Retrobulbar neuritis is characterized by an inflammatory process in the area of the optic nerve localized between the orbit and the optic chiasm. It usually develops in women 30-50 years old and is combined with multiple sclerosis.
If papillitis affects the layer of nerve fibers of the retina, the disease is called neuroretinitis. This form develops with certain diseases - Lyme disease, syphilis, viral pathologies.
Classification of optic neuritis
In neurology, it is customary to divide optic neuritis into several types, depending on the location of inflammation and its etiology. According to the etiological classification, optic neuritis can be demyelinating, parainfectious (a consequence of vaccination or viral infection), autoimmune (caused by autoimmune diseases), infectious (provoked by Lyme disease, syphilis, cryptococcal meningitis), toxic (a consequence of methyl alcohol poisoning).
Ophthalmoscopic classification:
- Retrobulbar. This type of neuritis is characterized by inflammation of the optic nerve after it leaves the orbit. It occurs mainly in multiple sclerosis. During ophthalmoscopy, no changes in the optic disc are observed. Typically, pathological changes appear in the late period of the disease, when inflammation covers the intraorbital part of the nerve.
- Intrabulbar (papillitis) is a pathological process characterized by damage to the optic nerve head. The pathology manifests itself as disc edema and hyperemia of varying degrees, which are accompanied by parapillar hemorrhages. Often this type of neuritis occurs in children.
- Neuroretinitis is a papillitis that is combined with inflammation of the nerve fibers of the retina. This pathology is characterized by the appearance of a “star figure” in the macular area, which is a solid exudate. Serous macular edema and parapapillary retinal edema are sometimes observed. Neuroretinitis is one of the rarest types of optic neuritis, usually occurring due to a viral infection, syphilis, or cat scratch disease.
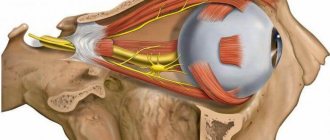
Brief anatomy
The optic nerve consists of axons of retinal neurons, whose function is to perceive images and transmit nerve signals to the optical centers of the brain. N. opticus contains more than 1 million axons. It originates in the optic nerve head, located on the retina. Inside the orbit it passes into the intrabulbar part. After the nerve leaves the orbit, it passes into the cranial cavity. This part is called retrobulbar.
In the area of the sella turcica n. The Opticus crosses over, where a partial exchange of fibers between the right and left sides of the nerve occurs. It ends in the optical centers of the midbrain and diencephalon.
The nerve is quite close to some structures - the orbit, the brain, the cerebral membranes. This “neighborhood” contributes to frequent optic neuritis with inflammation of the orbit, brain and its membranes.
Symptoms of intrabulbar neuritis
Intrabulbar optic neuritis has an acute onset. The inflammatory process can be provoked by pathogens such as staphylococcus, streptococcus, influenza and herpes viruses. The infection penetrates the optic nerve through the vitreous and perivascular spaces. Inflammation of the nerve can be total or partial. Total inflammation is characterized by a sharp decrease in normal vision. With partial damage to the nerve, vision may remain normal, but paracentral and central scotomas of oval, round and arch-like shapes are noted. Patients also have reduced color vision.
All pathological changes are usually concentrated in the area of the optic nerve head. The disc itself is hyperemic, its shade merges with the background of the retina, its tissue is edematous, and the edema has a pronounced exudative character. The boundaries of the disc are blurred, and there is no excessive prominence. The fundus of the eye with this optic neuritis is poorly and unclearly visible. Hemorrhages can be seen on the disc, the veins are slightly dilated.
The acute period of the pathology lasts about 3-5 weeks, after which the swelling begins to gradually subside, the boundaries of the disc become clearer, and all hemorrhages resolve. As a result, recovery and complete restoration of normal vision are possible, even if the prognosis was initially unfavorable. However, if the disease is severe, the death of nerve fibers, their disintegration and gradual replacement by glial tissue is possible. The prognosis for the patient is unfavorable, since optic nerve atrophy occurs. The degree of atrophy varies from minimal to complete, which leads to a sharp deterioration of vision.
Prevention
As you know, one disease often entails another, and inflammation of the optic nerve can develop as a result of other ailments. In order to reduce the risk of neuritis, you must follow several rules:
- avoid injuries associated with the skull, and in particular with the orbits and the eyes themselves;
- lead a healthy lifestyle, do not drink alcohol, especially in large quantities and often;
- Strengthen your immune system in every possible way, harden yourself and take enough vitamins;
- A healthy diet and compliance with all hygiene rules also play an important role;
- try to prevent infectious diseases, including sexually transmitted diseases;
- undergo regular preventive medical examinations.
Optic nerve atrophy Glaucoma Trigeminal neuralgia Eye keratitis: photos, symptoms and treatment Increased intraocular pressure: symptoms, causes and treatment Conjunctivitis
Symptoms of retrobulbar neuritis
Retrobulbar neuritis refers to inflammation of the optic nerve, which occupies the area from the eyeball to the chiasm. There are three forms of this pathology: peripheral, transversal, axial. Each form of neuritis has its own symptoms. The most common is the axial form of retrobulbar neuritis, which is characterized by localization of inflammation in the aximal bundle. The patient experiences the appearance of central scotomas in the visual field and decreased vision.
The most severe form of the disease is considered transversal, since it is characterized by the spread of inflammation to the entire tissue of the optic nerve. The patient's vision gradually decreases and blindness may occur. Inflammation usually begins in the axial fascicle or at the periphery, after which it spreads through the septa to the rest of the tissue. The peripheral form of neuritis begins to develop with inflammation of the optic nerve sheaths, which then spreads to its tissue. The inflammatory process is characterized by the accumulation of exudative effusion in the subarachnoid and subdural space of the optic nerve. Patients note severe pain in the orbital area, which begins to intensify when the eyeball moves. Central vision remains normal. All types of neuritis are characterized by the absence of changes in the optic nerve head.
Retrobulbar neuritis can occur in acute and chronic forms. In the acute course of the disease, a decrease in visual acuity occurs a couple of days after the onset of inflammation. In the chronic course of the pathology, vision decreases gradually. Typically, a chronic course of the disease occurs in the case of diabetes mellitus. This form of the disease occurs mainly in men. Almost always the lesion is bilateral, and visual acuity decreases very slowly. At the beginning of the disease, the optic discs are normal, but their temporal pallor gradually appears.
Diagnosis of optic neuritis
Optic neuritis is diagnosed by a neurologist and an ophthalmologist. The disease is accompanied by severe symptoms, so an ophthalmologist can diagnose it after a clinical examination of the patient. During an ophthalmological examination, the doctor compares the patient’s complaints with the results of ophthalmoscopy and visual acuity testing.
It is more difficult to correctly diagnose neuritis, which is not characterized by blurred vision or swelling. To make a diagnosis, differential diagnosis is indicated. Optic neuritis must be distinguished from pseudoneuritis and congestive disc. A patient suffering from pseudoneuritis retains normal visual functions. As for the congestive disc, this pathology differs from neuritis in the presence of papilledema and the preservation of normal vision. Fluorescein angiography of the fundus is considered the most accurate diagnostic method, which allows differentiating other pathologies from neuritis.
It is possible to distinguish retrobulbar neuritis from ordinary neuritis due to the discrepancy between visual acuity and the intensity of disc changes. Retrobulbar neuritis is indicated by a sudden decrease in vision with minimal changes in the optic nerve head. The neurologist can additionally prescribe consultations with a rheumatologist, infectious disease specialist, immunologist, as well as conducting studies such as blood culture for sterility, PCR studies, MRI of the brain, RPR test, ELISA.
Treatment and prognosis of optic neuritis
Urgent hospitalization is indicated for patients. Treatment of the disease is aimed at suppressing the inflammatory reaction and infection, desensitization, immunocorrection, dehydration, and activation of metabolism in the tissues of the central nervous system. In the first week of treatment, antibiotics, intravenous infusions of glucose, diacarb with potassium preparations (panangin), corticosteroids, administration of magnesium sulfate, B vitamins, nootropil, actovegin are prescribed.
In parallel with drug therapy, doctors find out the causes of the disease. After identifying the causes of optic neuritis, specific treatment is prescribed to eliminate them. This could be immunocorrective or antiviral therapy for herpes, specific treatment for tuberculosis, surgical treatment of sinusitis.
The patient may require emergency treatment, which includes detoxification measures. Prescribe oral administration of a 30% solution of ethyl alcohol in a dose of 100 ml, gastric lavage with a 4% solution of baking soda and other measures that are usually used for acute poisoning. If the patient has symptoms of optic nerve atrophy, he is additionally prescribed antispasmodics and medications that improve microcirculation (trental, nicotinamide, sermion, nicotinic acid).
The prognosis for the patient depends on the type of disease and severity. If you start treating the pathology on time and choose the most optimal tactics, you can achieve a complete recovery of the patient. However, often after the end of treatment, partial (in rare cases complete) atrophy of the optic nerve occurs.
Treatment of neuroma
A radical treatment method is removal of the neuroma, which can be performed by open surgery or radiosurgery. Surgical removal is advisable for a large tumor, if an increase in its size is detected over time, or if a neuroma grows after radiosurgery.
The operation often results in deafness and facial nerve paresis. Stereotactic radiosurgical removal is possible for neuromas smaller than 3 cm.
It is also performed in elderly patients with prolonged growth after subtotal resection and in cases where the risk of surgery is significantly increased due to somatic pathology.
Radiation therapy for neuroma has indications similar to those for radiosurgery. Radiation is not a way to remove the tumor, but it prevents its further growth and avoids surgery.
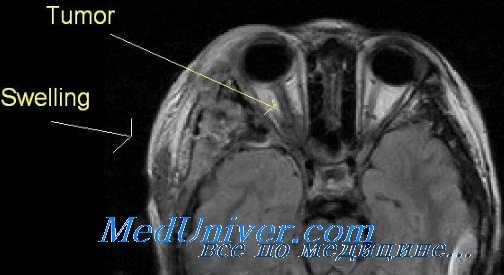
Patients with a neuroma accidentally detected by CT or MRI without clinical symptoms, patients with long-term hearing disorders and elderly patients with mild symptoms are advised to wait and see with constant monitoring of the size of the formation and the dynamics of clinical symptoms.