This type of headache is the most common of all existing ones. Statistics say that such symptoms occur in almost all inhabitants of the planet - in nine cases out of ten. Most often, tension headaches occur in people aged 20 to 35 years, and mainly affect the fair sex.
Tension headache - tension or tensor (from the English tension - tension) is manifested by prolonged monotonous, pressing or squeezing sensations. However, this pain cannot be called severe.
The consequences of such pain are expressed by chronic fatigue, nervousness, sleep disorders, loss of appetite, and a decrease in general tone. In addition, painful sensations are clearly expressed with loud music and exposure to harsh light.
Tension headache: symptoms
TTH is observed in adults (usually aged 30-40 years), adolescents, and children. This type of headache occurs much more often in women than in men. Mental workers and drivers are especially susceptible to the disease. Their primary pathology occurs due to muscle strain in certain areas of the neck. The risk group also includes watchmakers, jewelers, and representatives of other professions who constantly have to strain their eye muscles.
There are two forms of the disease:
- episodic - diagnosed after 10 attacks that meet the criteria for tension-type headache, lasting at least 30 minutes, up to 15 exacerbations per month. Occurs as a result of overwork, increased physical or mental activity, and stress. It manifests itself as a short-term pressing sensation in the area of the back of the head, forehead, and often the entire head hurts. An attack can last up to several hours; without taking painkillers it can last for several days;
- chronic – with attacks lasting for 3 months, more often than 15 times a month. It is characterized by severe pain in the forehead, occipital region, and spasms of the neck muscles. Compared to the episodic form, the symptoms are more pronounced and therefore more difficult to respond to analgesics. The duration of the attack can reach one month.
Both forms of tension-type headache require early diagnosis and timely treatment.
Regardless of the form, the symptoms of the disease are:
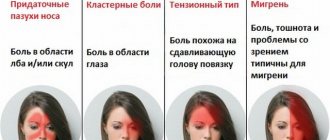
- bilateral or unilateral pain, spreading to the second half of the head, starting from the occipital region, moving upward (discomfort is felt when pressing on the neck, occipital region);
- squeezing, pressing sensations without noticeable pulsation, as if covering the cranium;
- moderate-weak, moderate pain intensity;
- absence of gagging, nausea, painful sensitivity to sounds and light;
- discomfort from wearing a hat, combing hair;
- increased pain in the second half of the day, as well as after severe stress.
To make a diagnosis, at least two of the listed symptoms must be present.
Forum tension headache treatment forum
Dear Dmitry! TTH is a very common type of primary headache. Unfortunately, general practitioners (including neurologists) make a number of mistakes when diagnosing and treating tension-type headache.
TTH is defined as a headache that occurs in response to mental stress, which is the result of acute or chronic stress.
Mental stress can be accompanied by increased tone of the frontal, temporal, occipital, and trapezius muscles. Tense muscles spasm the vessels located in them, which leads to ischemia and swelling and increases pain.
Not everyone reacts to stress with a headache; for this you need to have a special personality with a tendency to fixate on your somatic sensations and neurotic reactions. In addition to personal characteristics, the specific functioning of the brain with increased activity of cerebral pain systems and insufficiency of anti-pain mechanisms also plays an important role.
The prevalence of HDN in the population reaches 70%. Headaches of this nature can occur at almost any age. Women suffer somewhat more often from TTH.
Criteria for HDN.
The International Headache Association offers the following diagnostic criteria for tension-type headache:
· The duration of the headache episode should be at least 30 minutes. With episodic tension-type headache, the headache lasts for 30 minutes. up to 7 days. With chronic tension-type headache, daily, almost continuous headaches are also possible.
· The nature of the headache is very specific. These are squeezing, tightening, squeezing, monotonous pains. Throbbing pain is not typical for tension-type headache.
· According to localization, the headache is diffuse and always bilateral. In this case, one side may hurt more intensely. Patients quite figuratively describe the localization of their pain - “the head was pulled together with a helmet, a hoop, a helmet, a vice.”
· It is important that the headache does not get worse from normal daily physical activity. Despite the headaches, patients usually continue to work, although the quality of the work performed undoubtedly deteriorates.
· At the height of the headache, accompanying symptoms may appear: fear of light and sound, anorexia or nausea. Accompanying symptoms, as a rule, are not presented all together, but are observed in isolation and are clinically mild. However, in patients with severe chronic tension headaches, and at the height of a painful attack, the above symptoms may be present simultaneously.
Typical mistakes of general practitioners.
In diagnosing “headache syndrome,” I see at least four typical mistakes made by medical practitioners.
1) Overdiagnosis of “hypertensive headache”;
2) Overdiagnosis of “dyscirculatory encephalopathy”;
3) Overdiagnosis of “post-traumatic encephalopathy”;
4) Overdiagnosis of “vegetative-vascular dystonia”.
In order: - in the first case, TTH is easily mistaken for a “stable” and “pathognomonic” sign-marker of essential (primary) or secondary arterial hypertension. This is wrong. T.N. hypertensive headache occurs ONLY in the case of “acute hypertensive encephalopathy”, i.e. in case of cerebral edema due to hypertensive crisis (eclampsia)! When the following conditions are met: - if diastolic blood pressure sharply increases by more than 25% of the initial level; —and if diastolic blood pressure has increased ABOVE 120 mm Hg. —plus, neurological signs of acute encephalopathy syndrome. And that's it! Nothing there, “something in my head hurts today, probably blood pressure; I’ll suck a corinfarchik”—not clinically significant!
-Second. Dyscirculatory encephalopathy (DEP). Both patients and doctors have a distorted judgment that “old age is a disease”, “and age above 50 (or even 40) is already old.” Therefore, often, when a 50-year-old woman complains of a “headache,” the doctor reacts stereotypically: “Well, age, dear—what did you want? pressure 160/90, head—noisy?! spinning?!; get Dz: DEP 2-3 tbsp., buy Picamilon and drink to your health!”
Dyscirculatory encephalopathy is, first of all, a syndrome of chronic encephalopathy. Oh, that means: ALWAYS, cognitive impairment! Which, moreover, must be differentiated from depression (in which cognitive impairment is also common). And, episodes of non-systemic dizziness (non-vertebrogenic) - with anxiety.
Therefore, if a 50-year-old woman complains of constant headaches, tinnitus, attacks of dizziness, episodes of increased blood pressure, forgetfulness and absent-mindedness, then this is not DEP 2-3 tbsp. with “astheno-neurotic syndrome”, and TTH with anxiety-depressive syndrome.
-Third. Post-traumatic encephalopathy. (They also like the labels: mixed (toxic and traumatic origin) encephalopathy; nonsense!)
Here the stereotype is: “yeah, as a child I fell off a swing... I fought at school... I got hit on the head... I even lost consciousness!!! and then there was vomiting!!! Well, that means you didn’t go to the emergency room... well, exactly, post-traumatic encephalopathy! That’s why you, a young man, even have a headache..."
A concussion is a fundamentally REVERSIBLE condition! (unlike bruise of the brain and intracranial hematoma)
And no matter how many punches a person gets into his head, he does not become an encephalopath (an exception is a professional boxer-loser if he does not have time to recover after another knockout loss).
Therefore, to “sculpt” everyone and everyone as post-traumatic encephalopathy ONLY on the basis of a dubious anamnesis is overdiagnosis.
And further. Post-traumatic encephalopathy, again using neurological language, is a syndrome of chronic encephalopathy, which means STRAIGHT cognitive impairment must be present.
As a result, in a patient younger than 30 years old, we observe the same tension headache.
- Fourth. The diagnosis “vegetative-vascular dystonia” (“neuro-circulatory dystonia”) is often unreasonably used, where it is customary to “merge” the patient’s complaints about headaches...
And here there are “problems”... VSD is, FIRST OF ALL, a syndrome. That is, even if the doctor “attributed” the patient’s complaints of headache to the VSD syndrome, then he must go to the nosological unit (i.e., to the cause, not the consequence of the disease)…
Causes
TTH is a neurological disease that occurs as a result of:
- psycho-emotional stress, depression, prolonged stress of a negative or positive nature;
- long-term stay of the muscle fibers of the neck, upper back, eyes in a tense static state;
- increased fixation of attention, strong concentration;
- long-term unsystematic use of analgesics, tranquilizers;
- sleeping in an uncomfortable position.
Consequences
Often, due to the mild severity of the symptoms of tension-type headache, a person gets used to it and simply does not pay attention to the pain. Meanwhile, tension within the body increases, ultimately leading to depression, nervousness, aggressive behavior, and psychosis. If TTH becomes pronounced, the patient cannot relax, feels weak, gets irritated for no apparent reason, and gets tired quickly.
When you try to cope on your own, without the use of professional complex therapy, the situation quickly worsens. Episodic attacks turn into systematic ones, which leads to a decrease in the level of performance, disorder of behavior and character of a person.
Diagnostics
HDN cannot be detected by instrumental and laboratory medical examination methods. To identify a disease, an analysis of the patient’s general health and complaints is required. In order to diagnose HDN, a specialist conducts an examination and performs tests, based on the results of which a final diagnosis is made and complex therapy is selected.
The main diagnostic methods include:
- taking anamnesis;
- examination by a neurologist;
- identifying pain in the head, cervical spine, and upper back by palpation;
- MRI, CT, examination of the blood vessels of the brain, neck (for the possibility of organic lesions);
- blood and urine tests.
Patients are advised to keep records of the progress of headache attacks. Keeping a diary will help the doctor when making a diagnosis and selecting effective treatment.
Diagnosis of special cases
Statistics show that 85% of cases of tension-type headache can be cured relatively easily. If you are “lucky enough” to be in the remaining 15%, you will have to resort to a serious examination.
Try to analyze when, at what time of day, with what frequency a tension headache occurs, what is its intensity and nature, what precedes its appearance and disappearance. It is advisable to keep a diary of all these events in chronological order. It is useful to include data on the number of medications taken to relieve pain. The broader the information, the more accurately the diagnosis will be determined, and medications and procedures that are not necessary will not be used.
Survey
- Magnetic resonance aniography. This study allows us to identify arterial and venous malformations, aneurysms, as well as pathologies of the vessels of the neck and cerebral arteries;
- Magnetic resonance imaging. Allows you to accurately diagnose post-stroke lesions, sinusitis, traumatic lesions and many other diseases. This method is indispensable for in-depth study of the brain, spinal cord and for diagnosing tumors in the early stages of development;
- Laboratory research. They are aimed at identifying and identifying inflammatory processes caused by various infections.
Physiotherapy methods
With frequent attacks of tension-type headache, taking painkillers does not always solve the problem. In some cases, this may, on the contrary, worsen the situation. Most often, patients are prescribed complex preventive treatment, the purpose of which is to reduce pain sensitivity and prevent further development of the disease.
The therapy uses stress-reducing, muscle relaxing, non-drug treatment methods that reduce the electrical activity of the brain, among which the most effective are:
- manual therapy;
- exercise therapy;
- physiotherapy for the head and neck area;
- carboxytherapy;
- ILBI;
- mesotherapy;
- acupuncture;
- blood ozonation;
- multimag (Headache program);
- MDM therapy;
- myorhythm;
- micropolarization of the cerebral hemispheres;
- cutaneous electrical neurostimulation.
New approaches in the treatment of chronic tension headaches
About the article
6285
0
Regular issues of "RMZh" No. 8 dated April 21, 2010 p. 491
Category: Neurology
Authors: Naprienko M.V. 1, Filatova E.G. 2 1 Cephalgolog LLC, Moscow 2 Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after. THEM. Sechenov Ministry of Health of Russia (Sechenov University), Moscow
For quotation:
Naprienko M.V., Filatova E.G. New approaches in the treatment of chronic tension headaches. RMJ. 2010;18(8):491.
The term “tension-type headache” (TTH) was proposed for inclusion in the first International Classification of Headaches, published in 1988. TTH is the most common type of headache, its share in the total structure of headaches is 54%.
The term “tension-type headache” (TTH) was proposed for inclusion in the first International Classification of Headaches, published in 1988. TTH is the most common type of headache, its share in the total structure of headaches is 54%. TTH is divided into episodic (rare and frequent) and chronic forms [1]. The incidence of chronic tension-type headache (CHTH) in the population is relatively low and amounts to about 2%. In episodic forms, the number of days with headache does not exceed 15 per month or 180 per year. In chronic forms, the number of days with headache is more than 15 per month or 180 per year. Episodic pain, especially rare, as a rule, does not significantly affect the quality of life of patients, usually does not exceed 4–5 points in intensity and occurs with significant emotional, physical stress or as a reaction to emotional stress. Episodic tension headache in most cases goes away on its own and does not require drug treatment. CHF has a more pronounced intensity - 5-7 points on the visual analogue scale (VAS), - significantly disrupts the social activity of patients, reduces performance, and worsens the quality of life. In specialized headache clinics, the number of patients with CGTH reaches 70%, of which half suffer from CGTH [3]. This is primarily due to significant difficulties in diagnosis and especially treatment, as well as severe maladaptation of patients and a decrease in their quality of life. Among the factors causing chronic pain, the leading role is played by emotional disorders, the leader among which is depression. Abuse of analgesics, especially combination drugs, also contributes to the transformation of frequent episodic pain into chronic pain [2]. The pathophysiological basis of chronic pain, and chronic headache in particular, is a violation of pain modulation, sensitization of peripheral and central nociceptors. With TTH, the source of pain is tense pericranial muscles, their fascia and tendons. Several factors may play a role in the sensitization of peripheral receptors: mechanical stress, ischemia, and chemicals. Numerous EMG studies in TTH have shown normal or slightly increased muscle activity, which cannot lead to ischemia. However, all of these studies used surface electrodes. Recent work using needle electrodes has shown an increase in muscle activity at so-called myofascial trigger points. Prolonged increases in the activity of such motor units can lead to microtrauma and release of metabolites, as well as sensitization of peripheral nociceptors. Central sensitization is an increase in the excitability of neurons in the central nervous system when pain continues. Central sensitization develops as a result of sensitization of peripheral receptors. At this stage, peripheral receptors already have spontaneous activity, even in the absence of peripheral stimulation. Central sensitization is characterized by the phenomenon of allodynia (the occurrence of pain in response to a non-painful stimulus). As you know, a severe headache can be accompanied not only by nausea, photo- and phonophobia, but also by sensitivity or pain when touching the scalp and periorbital area. These signs are more pronounced with migraine pain, but can also appear with CHF - the pain loses its specificity with chronicity. In all patients with chronic headache (CH), regardless of the nature of the initial pain (migraine or TTH), signs of both peripheral and central sensitization are detected both clinically and experimentally. The periaqueductal gray matter (PAG), located in the rostral brainstem, plays a critical role in descending pain modulation. There are two types of neurons here: off-cells and on-cells. When off-cells are excited, spinal nociceptive processes decrease; when on-cells are activated, on the contrary, pain increases. Under normal conditions, there is a balance in the activity of the off- and on-cell populations. In chronic pain, this balance is disturbed towards the predominance of on-cell activity. Extensive connections with the prefrontal cortex, limbic system, hypothalamus, amygdala, and cingulate gyrus provide cognitive modulation of pain. The descending efferent fibers of the neurons of the periaqueductal substance end in the dorsal horns of the spinal cord at all levels. Treatment of chronic headache is a complex task: antidepressants and muscle relaxants are used, as well as a set of non-drug methods aimed at reducing muscle tension and increasing the activity of antinociceptive systems. If there is abuse of analgesics, a necessary condition for treating patients is the abolition of analgesics. The drug Katadolon (flupirtine) is a fundamentally new analgesic with neuroprotective properties and muscle relaxant effects. The mechanism of action of the drug differs from analgesics and NSAIDs (antiprostaglandin effect), as well as muscle relaxants, widely used in clinical practice. Catadalone has an antagonistic effect on NMDA receptors. The drug is capable of selectively opening K+ ion channels, which leads to stabilization of the membrane of afferent neurons, which prevents the transmission of nociceptive stimuli and the reduction of muscle tension, and also protects neurons from excessive excitation [4,6]. Katadolon is capable of both preventing chronic pain and reducing chronic pain. Foreign clinical studies of the drug have shown its high effectiveness in the treatment of acute, subacute and chronic pain in models of myofascial pain, musculoskeletal pain in the neck and back, as well as tension-type headache [5]. Purpose of the study: to study the effectiveness of Katadolon in the treatment of chronic tension headaches. Objectives of the study: 1. Study of the dynamics of the clinical picture of CHF (frequency, pain intensity), as well as psycho-vegetative disorders and sleep disorders during treatment with Katadolon. 2. Study of the muscle relaxant effect of Katadolon on the tension of the pericranial muscles. 3. Study of the analgesic effect of Katadolon in the treatment of CHF. 4. Study of the influence of Katadolon on the quality of life of patients with CHF 5. Study of the influence of Katadolon on the activity of antinociceptive systems in CHF. 6. Evaluation of the clinical effectiveness of the drug. 7. Study of undesirable side effects of the drug in the treatment of CHF. Research methods: – Clinical and neurological examination. – To determine the condition of the muscles in accordance with the recommendations given in the International Classification of Headaches, muscle palpation was used with further assessment of the severity of tension in the pericranial muscles (frontal, temporal, posterior cervical, trapezius, sternocleidomastoid) on a 3-point scale (0 - no tension; 1 – weak; 2 – moderate; 3 – pronounced). – Keeping headache diaries (registration of frequency, duration, headache intensity according to VAS, number of analgesic medications taken). – Comprehensive Pain Questionnaire (CPI) – Questionnaire for the Severity of Autonomic Disorders (SVD Questionnaire) – HADS Self-Assessment Anxiety and Depression Scale. – Questionnaire for clinical assessment of night sleep quality. – Quality of life questionnaire. – Study of the state of pain systems using the nociceptive flexor reflex method to determine the pain sensitivity threshold and reflex threshold (R III). – Questionnaire for registration of unwanted side effects. Statistical data processing was carried out using the computer program “STATISTICA for Windows”. Parametric and nonparametric methods of statistical analysis (Student, Wilcoxon, Mann–Whitney) were used. When comparing variation series, significant differences were taken into account (p<0.05). Results of the study The study included 30 people, patients of the Clinic for Headache and Autonomic Disorders of Academician A.M. Veina (Moscow) with an average duration of chronic hypertension of 10.5 years. The diagnosis of CGTH met the criteria of the International Classification of Headache Disorders II Revision 2004 [1]; attacks in patients were observed for a period of at least 6 months, at least 15 days a month, at least 4 hours a day. An additional criterion for inclusion in the study was cessation of taking psychotropic drugs and muscle relaxants 7 days before the start of the study. All patients were examined to exclude other types of headache before inclusion in the study. Patients with severe liver and kidney failure, the presence of cholestasis, pregnant and nursing mothers, patients with myasthenia gravis, and patients with hypersensitivity to flupirtine were excluded from the study. Patients were examined and interviewed before treatment, 7 days after starting the drug, and after treatment. Monotherapy with Katadolon was administered at a dose of 300 mg/day. within 8 weeks. Additional intake of analgesics if the analgesic effect of the drug is insufficient is recorded in the headache diary. Before treatment, the clinical characteristics of the patients corresponded to the characteristics of patients with CHF (Table 1). The average age of the patients was 39±5 years; in the study group there were 28 women and 2 men. Patients had 21.6±6.3 attacks of headache per month, on average 5.4±6.3 attacks per week, attacks lasted 5.3±3.7 hours per day, pain intensity according to VAS was 6.47± 0.89 points, all patients had significant tension in the pericranial muscles - 23.4±4.9 points, while 28 patients abused analgesic drugs, the average number of which was 18.6±10.3. The disease was quite severe before treatment: there was a significant decrease in quality of life and was 42.75±14.17, autonomic disorders were pronounced - 36.69±13.19, self-assessment of anxiety and depression HADS was 16.15±5.9, which corresponded to severe anxiety and depression, sleep disturbances were pronounced 17.9±2.38, according to a comprehensive pain questionnaire, pain intensity was 3.97±1.8, pain interference was 3.25±0.74, support from a loved one was 4, 99±1.19, life control 3.54±0.7, degree of emotional suffering 3.85±0.7 (Table 2). Indicators of the nociceptive flexor reflex (NFR) before treatment were reduced: pain threshold – 6.19±2.1, reflex threshold 7.2±2.57, coefficient 0.85±0.1 (Table 3). During 7 days of treatment with the drug, patients had an average of 2.86±1.5 headache attacks, which was significantly (p<0.05) less than before treatment - 5.4±6.3, the duration of the attack was significant (p <0.05) did not change, and pain intensity according to VAS changed significantly (p<0.05) from 6.47±0.89 before treatment to 5.5±1.3 after 7 days. Patients took significantly (p<0.05) fewer analgesic drugs (3.33±1.5) than before treatment (5±1.0). Thus, with the help of taking Katadolon, already in the first week of treatment it was possible to significantly reduce the number of headache attacks and its intensity, as well as reduce the number of analgesic drugs used to relieve attacks. After the end of the course of treatment, all clinical indicators improved significantly (p<0.05), namely, the number of attacks per month decreased, the number of analgesic drugs taken decreased, the intensity of pain according to VAS decreased, tension in the pericranial and cervical muscles decreased, no significant changes were obtained in influencing the duration of the attack, the indicators of the comprehensive pain questionnaire also improved, in addition to influencing the support of a loved one, the indicators of SVD and anxiety-depression improved, there was no effect on the quality of sleep and the NFR coefficient. Thus, the effectiveness of the drug Katadolon is undeniable; the results obtained indicate the analgesic and muscle relaxant effect of Katadolon. To determine the properties of Katadolon, we calculated the Δ% degree of severity of its muscle relaxant and analgesic properties. In our patients with CHF, the effect on the severity of muscular-tonic syndrome was 56 Δ%, the effect on the severity of pain according to VAS was 25 Δ% and 12 Δ% was the effect on the pain threshold and reflex threshold (Fig. 1). Thus, our study revealed a greater severity of muscle relaxant properties, which makes it possible to recommend the use of Katadolon for all conditions accompanied by muscle tension. The drug was well tolerated by patients. Only 2 patients noted the occurrence of side effects, such as mild, intermittent weakness at the beginning of taking the drug for 1 day, and 1 patient had stool upset, also during the 1st day of taking the drug. According to subjective assessment, 80% of patients indicated good tolerability and effectiveness of the drug, 20% satisfactory. Conclusion 1. As a result of the use of Katadolon in treatment
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Drugs for drug therapy
Treatment is prescribed by a doctor in the form of the complex use of various means (medicinal, relaxation, etc.). The main place in it is given to bringing the patient’s psycho-emotional state back to normal. Antidepressants are prescribed for the treatment of depression, phobias, and anxiety. Muscle relaxants are used to relieve muscle tension and spasms. Rapid-acting NSAIDs help cope with illnesses that develop under the influence of stress. There is no single recipe for getting rid of the disease; each patient requires a personal selection of medications.
To stop an attack and relieve acute symptoms of the disease, the following are most often used:
- ibuprofen;
- paracetamol;
- diclofenac;
- acetylsalicylic acid (aspirin);
- flupirtine.
To prevent an attack, take:
- amitriptyline;
- tizanidine;
- nortiptyline;
- baclofen.
You should be careful when taking medications when treating TTH. Using a painkiller for too long can have the opposite effect and cause another headache - a headache.
Symptoms of tension headaches
You can talk about HDN if:
- Her attack goes away within half an hour to several days. This is due to the physiological characteristics of the body;
- Pain regularly appears in the form of a pressing, pulling sensation in the forehead, moving to the temporal and occipital parts of the head;
- Tensor headache is expressed by constancy, absence of pulsations and stabbing sensations;
- The urge to vomit and nausea are not observed, but nervousness, irritability, loss of strength, painful sensitivity to sounds and bright light are pronounced.
A sure sign of tension-type headache is the appearance of a headache, of mild or moderate intensity, which does not interfere with the usual course of life and is relatively easily tolerated. In this case, the pain is not severe and the person soon gets used to it, postponing examination by a doctor.
Prevention of tension-type headache
For prevention purposes, it is proposed to use non-medicinal methods:
- Sleep at least 7-8 hours.
- Eat well and often (3-6 times a day), drink 2 liters of water.
- Avoid coffee, which contains caffeine, which dilates blood vessels and causes an increase in blood pressure.
- Reduce consumption or completely eliminate alcohol, after which oxygen starvation occurs, which has a destructive effect on brain cells.
- Choose the most optimal rest and work regime for your health.
- Organize breaks at work more often, during which it is recommended to perform exercises for the eye muscles and do physical warm-up.
- Move actively, take long walks in the air every day.
- Do exercise therapy, water procedures, use massage, acupuncture, manual therapy.
- Follow your doctor's instructions.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist. Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences. Experience: 22 years.
Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 22 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 23 years.
Palagin Maxim Anatolievich
Ask a question The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 5 years.
Felbush Anton Alexandrovich
Head of the Center for Extrapyramidal Diseases.
The doctor is a neurologist. Parkinsonologist. Physiotherapist. Experience: 9 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 7 years.
Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 16 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 15 years.
Read also
Headache treatment
Tarasova Svetlana Vitalievna.
Expert No. 1 in the treatment of headaches and migraines. Head of the Multiple Sclerosis Center. Neurologist of the highest category. Doctor of Medical Sciences Migraine is one... Read more
Temporomandibular joint dysfunction
Symptoms of dysfunction of the temporomandibular joint Among all the lesions of the mandibular joint, one can note myofascial pain click syndrome of the masticatory muscles, which characteristically translates ...
More details
Migraine
Migraine or headache seriously worsens a person's condition, especially with frequent attacks - chronic migraine. At the same time, people often do not take migraine seriously, not even thinking about seeing a doctor.…
More details
Overuse headache (Headache caused by excessive medication)
Frequent headaches are a good reason to immediately contact a neurologist. Otherwise, you can miss the onset of a serious illness or lead yourself to the formation of an abusive headache...
More details
Headache due to neuralgia of the greater occipital nerve
Headache caused by neuralgia of the greater occipital nerve occurs in 40% of patients. This is a signal from the body about the presence and development of serious problems. Unpleasant sensations are often confused by sufferers...
More details
"Tension headache: what to do?"
Home / Blogosphere
Alexander Ivanov 2019-07-27 08:00
Every person has experienced a tension headache at least once. This is a dull, constant pain that presses or squeezes the head like a hoop, which can last for days or even weeks, reducing a person’s quality of life. One of the main causes of such headaches is stress and prolonged work at the computer. It most often affects mental workers. How to stop feeling the “iron cap” on your head? Osteopathic doctor Alexander Ivanov spoke about this in a new article for BUSINESS Online.
“Headache is a common complaint when visiting an osteopathic neurologist” Photo: pixabay.com
THE MOST COMMON TYPE OF HEADACHE
Headache is a common complaint when visiting an osteopathic neurologist. Lately, parents often come to me with school-age children who have headaches. Drug treatment of such pain does not suit anyone, because there are many side effects, as they say, we treat one, and cripple another. Therefore, people are looking for effective and non-drug ways to get rid of headaches. Previously, in my publications, I have already talked in general terms about tension headaches. Today I will give practical recommendations and exercises to get rid of headaches.
The person experiences pain all over the head, as if it were being squeezed with a hoop or a helmet was put on it. The pain appears more often in the afternoon, late in the evening, after work or school. The trigger for pain is stress and muscle tension. Occasionally it is accompanied by nausea. This pain lasts from several hours to days. The intensity is usually low, and the attack is relieved with the help of painkillers.
CAUSES OF TENSION HEADACHES
Reason #1: Stress during the day. Psycho-emotional stress during the day leads to a malfunction of the anti-pain system, and ordinary nerve impulses from receptors turn into a source of pain. In addition, stress leads to excessive muscle tension in the neck and head, which also causes pain.
Reason No. 2. Violation of work ergonomics. For example, an uncomfortable work position, a high table or a low chair leads to overstrain of the muscles of the shoulder girdle and neck.
Reason No. 3. Abuse of gadgets and long hours of work at the computer. This is a common cause of headaches among office workers, students and schoolchildren. Previously, I already had an article about the dangers of using gadgets.
Reason No. 4. Uncomfortable pillow and incorrect sleeping position. Overexertion of the neck muscles during sleep can cause tension pain. It usually appears in the morning after waking up. Previously, I also wrote about how to choose a pillow and what position is best to sleep in.
Reason No. 5. Physical inactivity, or lack of movement. Impaired blood circulation due to lack of movement during the day can also cause tension headaches. This often occurs in office workers during prolonged sitting. Therefore, it is important to do industrial exercises and take a break from work every 40 minutes.
PREVENTION AND TREATMENT OF TENSION HEADACHES
Prevention of headache follows from an analysis of its causes. Think about what might most often be the cause of your headaches. The cause must be eliminated first. Next, work goes on with the muscles of the neck and head - this is the elimination of trigger (trigger) muscles. Gentle manual therapy (osteopathy) and physical therapy are important in this work.
However, to identify the cause and make a diagnosis, in any case you need to consult a doctor. This could be a neurologist or an osteopathic neurologist. To treat tension headaches, it is advisable to use non-drug methods: osteopathy, therapeutic massage, acupuncture, physical therapy.
GYMNASTICS FOR TENSION HEADACHES ACCORDING TO IVANOV
1. Place both hands on the sides of the scalp (temples, crown). The fingers are spread out like a rake. Make light rocking movements with your head back and forth so that your hands slide over your head and massage the scalp. Exercises relax the fronto-occipital aponeurosis. Do it for one minute.
Photo courtesy of Alexander Ivanov
2. You can use a wooden comb to massage your head. Comb your hair in all directions with a comb. This will improve blood flow and relax the aponeurosis of the head. Do it for one minute.
Photo courtesy of Alexander Ivanov
3. Exercise "slider". Place one hand on your forehead and the other on the back of your head. Move your hands first in different directions up and down, and then in one direction up or down. Do it for one minute.
Photo courtesy of Alexander Ivanov
4. Grab your head tightly from the sides with your hands. Next, having “glued” to the scalp, shift it in different directions left and right, back and forth, clockwise and counterclockwise, along an oblique line. Do it for one minute.
Photo courtesy of Alexander Ivanov
5. Tapping the head. Using the phalanges of our fingers, we lightly tap the head along the sagittal suture (strictly in the middle), then along the entire head from the forehead to the back of the head. Do it for one minute.
Photo courtesy of Alexander Ivanov
Exercises may have contraindications. Consult your doctor before doing this.
Be healthy!
Yours sincerely,
Ivanov Alexander Alexandrovich - Candidate of Medical Sciences, osteopathic doctor, neurologist, naturopath, member of the Russian Osteopathic Association, popularizer of a healthy lifestyle and a conscious approach to health.
Personal website www.osteopat-ivanov.ru