Epilepsy - modern methods of treatment
Epilepsy is the most common neurological disorder, with an incidence of 0.5-1% in the general population. For most patients, the prognosis remains positive with long-term control of seizures in the amount of 65%-70% of cases from the first or second dose of an antiepileptic drug (AED). However, approximately 30-40% of all patients suffering from epilepsy do not achieve remission, despite regular use of the drug. In such cases, it is imperative to conduct a full assessment of the patient's condition to determine the reasons for the lack of response to the drug and to find alternative ways to treat refractory epilepsy. Over the past 20 years, significant advances and important events have been recorded in the field of epilepsy treatment, such as the introduction of:
- High resolution magnetic resonance imaging of the brain
- Antiepileptic drugs of the second and third generation
- Neurostimulation systems
- Widespread use of dietary treatments
- ketogenic diet
New generation antiepileptic drugs
Antiepileptic drugs are the main form of therapy used in most cases of epilepsy. Until 1993, the only antiepileptic drugs available were Phenobarbital, Primidone, Hydantoins, Ethosuximide, Carbamazepine and Valproate are currently used for long-term treatment, while Phenobarbital and Hydantoins have good results in the treatment of acute status epilepticus. However, recent decades have seen the addition of a large number of new antiepileptic drugs that are now widely available and tested in clinical settings, giving the physician greater choice in personalizing treatment and the ability to control seizures with fewer side effects for the patient. The most common in modern clinical practice are Levetiracetam, Lamotrigine, Oxcarbazepine, Topiramate and Zonisamide, although even newer drugs such as Rufinamide, Lacosamide and Perampanel are increasingly being used.
Dietary treatment.
Dietary treatment, primarily a ketogenic diet, has proven to be an effective alternative for the treatment of many patients with drug-resistant or epileptic encephalopathy. In the 1990s, this procedure returned to clinical practice and has now been shown to be effective in numerous studies, although the mechanism by which seizure control is achieved remains unknown. This is a diet that is high in fat, normal in protein, and very low in carbohydrates, which forces the body to work in starvation conditions by processing fat instead of carbohydrates. Achieving these goals requires greater strictness in limiting carbohydrates, as even small amounts of sugar can divert the metabolism from producing and burning glucose, which the body prefers over ketones for energy. Implementation of ketogenic diet treatment requires a highly trained and experienced nutritionist in close collaboration with the neurologist and the patient's family.
Surgical treatment of epilepsy
In the past, surgery was considered a last resort in the treatment of intractable epilepsy only after all medical and non-medical options had been tried and had failed to result in seizure remission. Nowadays, surgery is a very successful and effective way to combat epilepsy if the appropriate indicators are present or it is the only therapy that can lead to recovery. Any patient with refractory focal seizures is evaluated for surgical treatment after failure of at least two AEDs. Additional criteria to determine whether surgery can be performed are: serious impact of the frequency and severity of seizures on daily life, the presence of well-localized damage to the cerebral cortex, and the ability to eliminate eliptogenic activity without causing neurological complications. The option of surgical treatment of epilepsy should be considered without delay in the presence of the above conditions, especially in children with known anatomical lesions. Particularly important is a detailed preoperative examination of the patient, including high-resolution neuroimaging of the brain, video electroencephalography and examination by a Neuropsychologist and Psychiatrist. Surgical treatment of epilepsy may include partial resection of the epileptogenic focus by removing the entire lobe of the cerebral cortex (lobectomy) or even resection of one hemisphere of the brain (hemispherotomy).
The most successful is resection of the temporal lobe and intervention in the frontal lobe. In some cases of refractory epilepsy in which resection is not possible, other methods may be used. The most widely used today is an incision of the corpus callosum, either partially (two thirds) or a full incision, with positive results in generalized tonic and atonic attacks and in Lennox-Gastaut syndrome.
Neurostimulation and neuromodulation
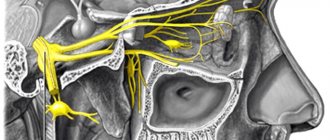
Neurostimulation is gaining momentum in the treatment of many neurological diseases and has already established itself as a treatment option in cases such as Parkinson's disease. With regard to epilepsy, three neurostimulation methods have gained clinical use: electrical stimulation of the vagus nerve (VNS), deep stimulation of the hypothalamic medial nuclei.
The use of a vagus nerve stimulator has been approved as an adjunctive therapy in children over 12 years of age and in adults with persistent focal seizures and has been shown to, in addition to seizure control, significantly improve the quality of life of patients with epilepsy. A number of new techniques are currently in development, such as transcranial magnetic stimulation, with promising results. However, all Neurostimulation methods are used extremely rarely, only when the possibility of surgical treatment has been tested and has been unsuccessful or is not possible for the patient.
SURVEY
BASIC CHECK UP (Complete blood count, ESR, creatinine, urea, glucose, cholesterol, triglycerides, AST transaminases, ALT transaminases, Australian antigen HBsAg, urinalysis, Pediatrician examination )
Causes
Genetic predisposition and inheritance play a significant role in the development of epilepsy. So, if parents suffer from a disease, the child is more likely to develop the disease. The incidence of epilepsy in families with sick parents is from 5% to 45%.
In addition to heredity, acquired factors play a role in the formation of the lesion. Lifetime and intrauterine causes of epilepsy:
- disruption of brain development during fetal formation;
- hippocampal sclerosis;
- vascular pathologies of the brain: atherosclerosis, arteriovenous malformations;
- traumatic brain injuries;
- brain tumors and cysts;
- neurodegenerative diseases;
- past infectious diseases;
- the impact of acute intoxication: alcoholics and drug addicts are more susceptible to seizures than healthy people.
Research methods
Electroencephalography is the “gold” standard in the diagnosis of epilepsy. The brain produces electrical activity that is expressed in different rhythms. During epilepsy and during remission, brain wave activity changes, and this is visible on the electroencephalogram. EEG in epilepsy is characterized by such phenomena, which are called epileptiform:
- spike discharges;
- complexes of spike waves and polyspike waves;
- sharp waves;
- hypsarrhythmia;
- sharpened potentials during sleep;
- wicket spikes;
- rhythmic midtemporal waves.
In addition to electroencephalography, magnetic resonance and computed tomography have diagnostic value.
A general clinical examination includes an examination and interview with a doctor. The epileptologist or neurologist is asked to describe the psychological state before and after the attack and when it begins. The responses of relatives play a role, since they are the ones who see what happens to the patient during an attack: the patient himself loses consciousness at this time.
Psychodiagnostics includes the study of cognitive functions. With epilepsy, personality changes: a person becomes vindictive, sarcastic and ironic. In the emotional sphere, dysphoria often appears. Thinking becomes rigid, sedentary, and detailed. Epileptics find it difficult to separate the important from the unimportant. Slowly attention shifts. Patients tend to concentrate for a long time on emotionally significant things. For example, epileptics remember insults for a long time.
The following types of attacks are distinguished:
- Generalized convulsive seizures consist of sudden muscle tension and short-term cessation of breathing. Then convulsions begin, lasting from 10 seconds to 20 minutes. The attack stops on its own, after which the child falls asleep.
- Nonconvulsive generalized seizures (absences) are less pronounced. They consist of sudden freezing, the patient’s gaze becomes absent. Sometimes the child's eyelids may tremble and his eyes may close. Duration is about 5-20 seconds; in the acute period, the child does not react to external stimuli. Once finished, he can continue to do his own thing. Typically, childhood epilepsy of this type begins at the age of 5-7 years and is more common in girls. After puberty, a child may “outgrow” the disease. But you shouldn’t wait for this, since the absence form can develop into a more complex one.
- Atonic attacks are characterized by sudden loss of consciousness with muscle relaxation. They are easily confused with fainting. If seizures occur frequently, this is a serious reason to contact a neurologist and pediatric epileptologist.
- Infantile spasm is an involuntary tilt of the head or torso forward with hands pressed to the chest. Seizures can occur after waking up, especially abruptly, and are typical for children under 3 years of age. By the age of five, childhood epilepsy of this type can either go away completely or change into another form.
In addition to the types described, there are other forms. If there is something alarming about your child’s condition, you should seek advice from a pediatric epileptologist.
Treatment methods
Principles of treatment of epilepsy:
- Prescription of antiepileptic drugs.
- Determining the need for a diet.
- Neurosurgical correction of the disease.
- Social and psychological rehabilitation of patients and families.
Doctors in the treatment of epilepsy have the following goals:
- relieve pain from cramps;
- prevent recurrence of a new attack;
- reduce the duration of attacks;
- reduce the number of side effects from taking medications;
- restore mental functions or prevent their degradation.
Medication
Drug treatment of epilepsy has the following principles:
- Individuality. The dose and regimen are selected individually for each patient.
- Complexity. It is advisable to use drugs with a combined effect that have a complex effect on the patient’s seizures and mental health. Metabolic agents, absorption therapy and dehydration drugs are also prescribed with anticonvulsants.
- Continuity. For successful treatment of epilepsy, monotherapy is usually prescribed - lifelong use of one drug. It should be taken constantly, according to the regimen. When the drug is discontinued, the risk of epileptic seizures increases. However, 70% of patients receive monotherapy, 25% receive bitherapy (two drugs), and 5% receive tritherapy (three drugs).
- Timeliness. One seizure without a specific cause (stress, mental tension) does not require antiepileptic therapy.
- Gradualism. Treatment begins with a minimum dose of anticonvulsants. Over time, the dose is increased until the seizures are completely eliminated. The dose is calculated based on the weight and age of the patient.
However, the main principle of epilepsy treatment is maximum effectiveness with a minimum of side effects.
Treatment of epilepsy in adults involves taking the following anticonvulsants:
- valproates;
- carbamazepines;
- benzodiazepines;
- Barbiturates;
- Succinimides.
Absorbable therapy: hyaluronidase, bijoquinol. Dehydration therapy: magnesium sulfate, dextrose solution 40%, furosemide. Metabolic therapy: nootropics, vitamins, herbal medicine, folic acid.
Diet
The ketogenic diet is used to treat epilepsy. Doctors have found that eating this diet reduces the risk of epileptic seizures in children and some adults. The main point of the ketogenic diet is low carbohydrate content and high fat content.
The ketogenic diet includes the following foods:
- butter;
- bacon;
- high fat cream;
- vegetable oil;
- mayonnaise.
The diet is only used when drug therapy has no effect - the body has developed resistance to anticonvulsants.
Operational
Surgical treatment is used only in the following cases:
- Symptomatic epilepsy appeared against the background of a structural lesion in the brain.
- The frequency of epileptic seizures is more than twice a month. Seizures lead to maladjustment of the patient and worsen his mental abilities.
- Resistance to antiepileptic therapy has developed when taking at least four drugs.
- Epileptic foci occur in areas of the brain that do not carry vital functions.
The goal of the operation is to reduce the frequency of seizures and improve the patient's quality of life.
Socio-psychological
This treatment item consists of the following items:
- Social and pedagogical aspects. They are aimed at adapting the patient to society, developing personal qualities and developing a life position.
- Psychological rehabilitation. Aimed at restoring reduced mental functions and developing emotional-volitional stability.
Prevention of consequences of epilepsy:
- getting enough sleep;
- abolition of bad habits, physical and emotional overload;
- avoiding overheating in the sun, hyperventilation and high-temperature rooms;
- reducing the amount of time spent in front of the TV.
Signs and symptoms
The term “epilepsy” covers more than 60 pathologies of the nervous system. There are several characteristic signs in which you should contact an epileptologist as soon as possible:
- Sharp intense headaches accompanied by vomiting, confusion, speech disorders;
- Sudden convulsions lasting from a few seconds to 10-20 minutes;
- Loss of consciousness;
- Sudden tension or relaxation of muscles, accompanied by cessation of breathing, involuntary urination;
- Freezing in unusual positions, with strange facial expressions and/or a complete lack of reactions to external stimuli.
Epilepsy in children (especially newborns) can occur with vague symptoms, which causes difficulties in diagnosis.
Modern diagnostic methods and approaches to the treatment of epilepsy in children
Epilepsy is a chronic brain disease characterized by repeated attacks of disturbances in motor, sensory, autonomic or mental functions resulting from excessive neural discharges. The frequency in the population reaches 0.5-0.8%, and among children – up to 1%. In 85% of patients, epilepsy debuts in childhood and adolescence. The disease is based on pathological paroxysmal excitation of brain neurons, prone to discharges that clinically manifest themselves in the form of epileptic seizures. In the community, the most commonly known type of seizure is generalized seizures, but these constitute only a small portion of all seizures known today. There are more than 30 different types of epileptic seizures, which, according to their clinical manifestations, can be grouped into groups of “convulsive” seizures (tonic, clonic, myoclonic, hypermotor, myatonic, etc.) and “non-convulsive” (absences, dialeptic with automatisms, temporal syncope). According to the mechanism of occurrence, seizures are divided into focal, that is, arising as a result of irritation of a certain focus (part) of the brain, and generalized, in which the epileptic discharge instantly spreads to both hemispheres of the brain. It should be noted that epilepsy is a heterogeneous disease, that is, epileptic seizures can be caused by various reasons. In this regard, it is customary to subdivide epilepsy into forms and syndromes. In total, more than 40 forms of epilepsy have been described, which are characterized by various syndrome-specific causes of occurrence, age of onset, set of attacks, course, prognosis, as well as approaches to therapy.
According to the modern classification, symptomatic, cryptogenic and idiopathic forms of epilepsy are distinguished. Symptomatic refers to epileptic syndromes with a known cause. As the name implies, symptomatic epilepsy is one of the symptoms of another disease of the nervous system, for example, oxygen starvation during pregnancy, pathology of childbirth, intrauterine infection (perinatal encephalopathy), brain tumors, meningoencephalitis, rare hereditary diseases, etc. Symptomatic forms of epilepsy, often combined with mental retardation and cerebral palsy; more difficult to treat.
Cryptogenic (from the Greek criptos - hidden) forms of epilepsy are syndromes with an unrefined, unclear cause. It is understood that cryptogenic forms are symptomatic, but at the present stage, using all diagnostic methods, it is not possible to identify their cause. Today, most neurologists are inclined to believe that it is more correct to interpret cryptogenic forms of epilepsy as “probably symptomatic.” Separately, idiopathic forms of epilepsy are distinguished - the most favorable. The concept of idiopathic epilepsy comes from the Greek words “idios” (own) and “patos” (painful) and means that this form of epilepsy is caused by dysfunction of the brain itself. According to Delasiauve, one of the first to propose the term idiopathic epilepsy at the beginning of the 19th century, cases with no signs of organic brain damage should be included in this group. Tissot in 1770 suggested that in idiopathic epilepsy “there is a predisposition of the brain to convulsions.” As a rule, with idiopathic forms there is normal intelligence, there is no paralysis, and epilepsy responds well to treatment. In the structure of forms of epilepsy there is also a division into focal and generalized, depending on the types of epileptic seizures.
Epileptologist in Moscow: address
Stepanishchev I.L. - epileptologist, neurologist. This doctor works with both children and adults. He has been working in this field for 29 years, has the highest category, and has the highest rating among patients. Works at the Institute of Child and Adult Neurology named after. Saint Luke.
Baeva E. Yu. – neurologist, functional diagnostics doctor, epileptologist. Reviews are predominantly positive. She has been working with patients with epilepsy for 18 years. You can consult and examine her at two addresses: st. Priorova, 36 Water Stadium; st. Kosmonavta Volkova, 9/2 Airport.
Kremenchugskaya M.R. is a neurologist and epileptologist of the highest category, working with people of all ages for 37 years. He treats at the Institute of Pediatric and Adult Neurology named after. Saint Luke.
Gadzhiev G.I. - ultrasound doctor, neurologist, pediatric epileptologist, works with adults. 15 years of experience, awarded the highest category. The consultation takes place at: medical; Children's clinic No.117.
Voronkova K.V. is a pediatric neurologist and also an epileptologist. She has 16 years of experience, has the highest category, and was awarded the title of professor. Academic clinic "Cecile+".