Epilepsy is a serious chronic disease, the distinctive feature of which is repeated unprovoked epileptic seizures, characterized by disruption of almost all brain functions.
↯
More articles in the magazine
“Deputy Chief Physician”
Activate access
In the article we will talk about what epilepsy is, what symptoms are typical for it, what indicators to pay attention to when filling out an emergency hospital call card, and also give an example of filling out a call card during an epileptic seizure.
Symptoms of an epileptic attack:
- The appearance of an “aura” (flashes before the eyes, auditory or olfactory hallucinations, numbness of the limbs, blurred vision or complete loss of the ability to see, dizziness, loss of consciousness and other phenomena).
- Cramps of all muscles or individual groups of them.
Cheat sheet when applying for a calling card for a patient with epilepsy
The call card for epilepsy indicates the patient's complaints at the time of examination.
The documentation reflects the following points:
- the nature of the convulsions (if they are conscious);
- the patient’s feelings before the attack;
- the presence of a bite injury on the tongue;
- presence of involuntary urination;
- presence of headache;
- the presence of dyspeptic symptoms (nausea, vomiting);
- the presence of sensitivity disorders and paresis;
- the presence of general weakness;
- presence of speech, vision, and cognitive impairments.
Clinical recommendations can be deployed in the Consilium System: available for doctors only!
Anamnesis
The medical history in the emergency call card for epilepsy includes items such as:
Time of seizure onset (how many hours/minutes ago).- Nature of seizures (partial, generalized).
- The sequence of appearance and dynamics of symptoms or complaints that became the reason for calling the emergency medical team or identified during a medical examination.
- Did the patient fall during the attack? If you fell, did you hit your head?
- Events that triggered the seizure.
- Frequency of seizures.
- Anticonvulsant medications taken by the patient.
- Concomitant pathologies (if any).
Also, the call card for epistatus indicates the source of the information received - from the words of the patient, eyewitnesses, from the outpatient card, discharge summary from the hospital. If the source of information cannot be established, it is necessary to indicate that a reliable history is unknown.
Additionally, the call card for convulsive syndrome indicates whether the allergy history is aggravated, and in women - if there is additional information regarding the gynecological history (diseases, surgical interventions, etc.). If the patient has an elevated body temperature, his epidemiological history should be clarified.
Objectively
The emergency physician should pay special attention to such indicators as:
- severity of condition;
- level of consciousness (according to the Glasgow school);
- position;
- condition of the skin and mucous membranes;
- Body temperature;
- condition of the tongue - localization, whether there is a bite;
- characteristics of behavior, psycho-emotional state;
- contact: describe whether the patient is oriented in time and space, whether he remembers who he is, whether he follows the instructions of the emergency doctor;
- impairment of cognitive functions (memory, attention, perception);
- features of sensitivity (it is necessary to indicate the type of sensitivity being tested (temperature, tactile, pain, etc.), as well as the identified disorders and their localization;
- speech features (normal, aphasia, dysarthria, etc.);
- pupils (dilated, constricted, normal size);
- features of the pupillary reaction - friendly or not;
- presence or absence of nystagmus (if present, indicate its side and nature);
- the presence or absence of facial asymmetry (if present, indicate the side, central or peripheral paresis of the facial nerve);
- the presence or absence of meningeal symptoms (stiffness of the neck muscles, Brudzinski’s, Kernig’s symptoms, etc.);
- the presence or absence of focal symptoms (paresis, plegia, their severity and type);
- the presence or absence of pathological foot symptoms (Babinsky, etc.);
- tendon reflexes D=S;
- coordination tests - finger-nose, knee-heel, etc.;
- whether the patient controls urination and defecation.
If the patient is injured due to a fall, this should also be described in detail in the call card for an epileptic attack.
What information should be in the patient's outpatient medical record?
The worksheet provides information about what information needs to be recorded on the card, how to fill it out and when it needs to be entered.
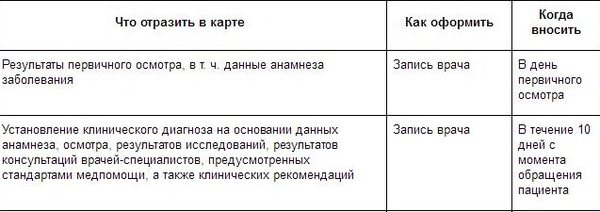
The material is available in the Chief Physician Help System for subscribers and demo access clients. Download table
For reference: epistatus
Status epilepticus is a pathological condition in which epileptic seizures follow each other (they can last for half an hour or more), and in the intervals between attacks the patient does not regain consciousness. Epistatus can develop as a complication of epilepsy or become its manifest manifestation.
A repeated attack develops even before the impaired functions of the central nervous system, which resulted from the previous attack, have been restored.
Thus, violations from various systems and organs of the human body progressively accumulate.
If, in the intervals between attacks, the patient’s condition is relatively normalized, consciousness is restored and no progressive impairment of body functions is observed, then this condition is called serial epileptic seizures and is qualitatively different from status epilepticus.
The pathophysiology of all types of status epilepticus is the same - it differs only in the degree of involvement of the brain in the epileptic activity.
The basis of this condition is continuous (or intermittent, but repeating) paroxysmal collective electrical activity of brain neurons.
Then pathological excitation occurs in neural circles, which, in turn, leads to the maintenance of the status of epileptic seizures according to the principle of a vicious circle.
Depending on how strongly different parts of the brain are involved in this pathological activity, the nature of the epistatus also differs.
Unlike a single epileptic seizure, the body is not able to independently stop status epilepticus. In addition, with this condition it is not necessary to fall into a coma, and in some cases the patient may even retain formal consciousness.
- In this article you will find only a few ready-made samples and templates. In the Consilium System they more than 5000
.
You will have time to download everything you need using demo access in 3 days
?
Activate
Epilepsy, unspecified - example of writing a call card
Male, 36 years old. The reason for the call is that he is unconscious on the street, the reason has not been established (passers-by call).
Complaints, medical history
At the time of inspection, he makes no complaints about what happened and doesn’t remember. He is located on the street near the store, sitting on the porch.
According to others, about 10-15 minutes ago there was an attack of tonic-clonic seizures with loss of consciousness and foam at the mouth. No treatment was undertaken. This is not the first time this has happened; I previously went to the emergency room for epileptic seizures.
Anamnesis of life
Epilepsy, the patient is registered as an outpatient with a neurologist. Regularly takes anticonvulsant medications. Comfortable blood pressure cannot be explained.
Physical examination
- moderate condition;
- level of consciousness - stunned (13 according to Glasgow school), behavior is inhibited;
- pupils are normal, D=S, reaction to light is lively, gaze paresis is absent, horizontal nystagmus;
- the skin is dry, clean, physiologically colored, the mucous membranes are not inflamed;
- heart sounds are clear, rhythmic, there are no noises, the pulse in the peripheral arteries is rhythmic, of satisfactory quality;
- from the central nervous system – there are no meningeal symptoms, muscle tone is increased, there are no focal symptoms;
- the pharynx is calm, the tonsils are of normal size;
- chest excursion is normal, breathing is normal, percussion – pulmonary sound, auscultation – vesicular breathing, no wheezing;
- no peripheral edema;
- the tongue is moist, clean;
- the abdomen is soft, painless, regular in shape, takes part in the act of breathing, there are no symptoms of peritoneal irritation;
- the liver does not extend beyond the edge of the costal arch;
- chair – 1 time per day, decorated;
- diuresis is normal, SSPO is negative.
Main pathology
The patient is stunned, inhibited, inadequate, lost orientation in time and space. There are marks of teeth on the tongue, and there are also signs of involuntary urination. Consciousness gradually recovered during the examination. No signs of head injuries were found.
| time | 17-30 | 17-50 | 18-10 | Etc. peace |
| NPV | 16 | 16 | 16 | 16 |
| Pulse | 86 | 84 | 76 | 72 |
| Heart rate | 86 | 84 | 76 | 72 |
| HELL | 150/90 | 130/80 | 130/80 | 130/80 |
| Pace. ºС | 36,6 | |||
| SpO2 | 97 | 97 | 97 | 97 |
Blood glucose – 6.9 mmol/l;
ECG data: sinus rhythm, 83 beats/min, no signs of acute pathology of the heart and blood vessels. There is no ECG archive.
Diagnosis by the EMS team
Epilepsy of unknown origin, condition after an attack.
Therapeutic measures
17-39 – Sol. MgSO4 25% – 10 ml i.v.
The patient was hospitalized in the neurological department of the city hospital.
Single convulsive epileptic seizures
As a rule, seizures develop against the background of a satisfactory condition of patients and are characterized by loss of consciousness, short-term cessation of breathing, cyanosis, tongue biting, and involuntary urination. During an attack, mydriasis is observed, the reaction of the pupils to light is absent. There is a moderate increase in blood pressure and increased heart rate.
After the attack, stunning is observed for 10-15 minutes; patients have difficulty making contact and quickly become exhausted. Less commonly, an epileptic coma occurs that turns into sleep; sometimes a twilight state of consciousness is observed. In some patients with short-term (20-30 sec) generalized tonic seizures, a rapid clearing of consciousness occurs, they are active, adequate, easily come into contact, and sometimes euphoric.
In the neurological status after a seizure, many patients experience: decreased corneal reflexes, muscle hypotonia, decreased or absent deep reflexes. Focal neurological symptoms include asymmetry of facial muscles, horizontal nystagmus, mild symptoms of pyramidal insufficiency (increased reflexes, Babinski's symptom), etc.
Severe postictal paresis is unusual in adult patients with epilepsy with generalized or unilateral seizures, and their presence should always raise suspicion of the existence of an ongoing cerebral organic process. Only in isolated cases does epileptic hemiplegia (Todd's palsy) develop, which makes diagnosing the underlying disease difficult. In these cases, in elderly patients it is necessary to exclude, first of all, acute cerebrovascular accidents, as illustrated by the following example:
Patient S., 76 years old. From the anamnesis it is known that since the age of 23, after a cerebral contusion, he has suffered from epileptic seizures with a frequency of up to 5-6 times a year. He is registered at a psychoneurological dispensary. He takes anticonvulsants irregularly. Suffering from hypertension. Today, a convulsive epileptic seizure developed with the appearance of tonic-clonic convulsions in the right half of the body and in the right limbs, accompanied by loss of consciousness, vomiting, and involuntary urination. Upon examination, the patient's condition is moderate, the skin is hyperemic and slightly cyanotic. The number of breaths is 24 per minute. In the lungs there is vesicular breathing, scattered dry rales. The heart sounds are muffled, the accent of the second tone is on the aorta. Pulse 92 per minute, arrhythmic. Blood pressure 200/100 mm Hg. Art. The patient is stunned, opens his eyes when called, and tries to follow the instructions. There are no meningeal pupils. The movements of the eyeballs are somewhat limited, the pupils are of medium width, D = S, their reaction to light is preserved.
Convergence is weakened. The right nasolabial fold is smoothed. There are no spontaneous movements in the right limbs. Muscle tone is low, D
A feature of this observation is the difficulty of diagnosing the underlying disease that caused the seizures. The patient's vascular history, increased blood pressure, and the appearance of focal neurological symptoms with rapid subsequent regression suggested a transient cerebrovascular accident with convulsive seizures.
However, indications of seizures in the past and negative data from an echoencephalographic study rather pointed to the possibility of developing Todd's palsy in a patient with epilepsy, which was confirmed by data from the patient's objective condition upon recovery from a seizure, as well as additional anamnestic information.