Types of disorder
An experienced doctor should diagnose the condition and make a diagnosis.
There are the following degrees of depression:
- Easy. Appears sporadically. The person leads a normal life. Only a few symptoms are present.
- Average. The presence of a disorder becomes obvious. It begins to interfere with the usual routine.
- Severe depression is the most difficult. The person stops coping with everyday activities. Without treatment, irreversible consequences occur.
Having at least a few symptoms of severe depression should be a reason to see a doctor.
They are not difficult to detect. The attentive attitude of loved ones plays a decisive role, since the patient himself is not able to ask for help.
How does severe depression manifest?
Timely consultation with a doctor is the key to successful treatment.
Knowing the symptoms of severe depression can help you recognize them in a loved one:
- Insomnia, sleep disturbance.
- Lack of appetite.
- Memory problems.
- Loss of activity, fatigue.
- Inability to concentrate for a long time on one object, work, or important conversation.
- Feelings of guilt, hopelessness.
- A sharp decrease in self-esteem.
- Loss of interest in life and the world around you.
- The desire for loneliness.
- Phobias and fears that a person was previously unaware of are clearly manifested.
- Thoughts about suicide.
- Pain in the heart, digestive organs, migraine.
It is important to know that severe depression does not appear suddenly. Its signs may be faintly noticeable to others. It is for this reason that trusting communication with loved ones is vital.
Depression
When the realization comes that all actions performed by a person, all efforts are in vain, apathy and depressive moods come.
Depression itself marks the fourth stage. Here comes the realization that it is impossible to change what happened. A person is overcome by apathy, he is indifferent, and loses interest in existence. It seems to him that, coupled with the unpleasant incident, everything has come to an end. Nothing can bring him joy anymore. Previously significant things lose their meaning.
At the same time, some people experiencing despondency and apathy go through this stage at home, endlessly watching TV shows, constantly chewing something, eliminating all social contacts, while others continue to work, lead their usual lives, communicate with relatives, friends, and perform various social duties.
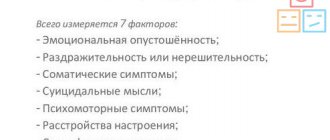
The fourth stage of depression is characterized by the following manifestations:
– lack of appetite;
– decreased self-esteem (people feel like complete nonentities);
– invariably present drowsiness or other sleep disorders;
– decrease in concentration;
– lack of desire for social interaction, communication, sharing one’s own experiences with others;
– obsessive suicidal thoughts;
– awareness of the futility of the efforts made;
– regret about the past, disappointment in one’s own person;
– immersion in the world of sadness and regrets.
The described stage of depression is considered the most protracted phase. Therefore, the support of relatives, the help of the environment, and sometimes even a psychologist are very significant here.
Causes of severe depression
Depression often occurs after severe shocks and emotional experiences. These include the death of a loved one, physical violence, and job loss. In these cases, significant symptoms appear immediately. The patient needs urgent help. Recovery may take up to three months.
It is much more difficult to recognize the problem when there is no obvious reason for severe depression. What to do in this case? First of all, watch the person carefully.
There are hidden reasons that provoke the disorder:
- frequent quarrels in the family;
- noisy neighbors;
- a relationship with a person who is frightening, annoying or simply unpleasant;
- repeated failures in personal life;
- problems at work.
It may seem to an outsider that these are all trifles unworthy of attention. But it is precisely because of such circumstances that anger, rage, and irritation accumulate. Subsequently, any trifle can provoke a nervous breakdown and prolonged depression.
In addition to psychological reasons, there are also physiological ones:
- severe intoxication of the body;
- traumatic brain injury;
- hormonal imbalance;
- diseases of the cardiovascular system;
- sedentary lifestyle, unhealthy diet;
- identity crisis;
- inability to satisfy one's needs;
- experiences associated with man-made and natural disasters.
Treatment for severe depression should begin as soon as symptoms are noticed. In a critical situation, when there is no way to see a doctor or no one to talk to, the emergency service will help.
All you have to do is dial the phone number. The person on the other end of the line will listen carefully and give advice. Simple words of comfort can have a powerful positive effect in some cases.
Why depression needs a new definition
According to many psychiatrists, advances in the research, diagnosis and treatment of depression require a new approach that links individual symptoms to underlying mechanisms.
In Hippocrates' Aphorisms, melancholy (as depression was called in ancient times) is defined as “a prolonged feeling of fear and despondency.” The reason, according to the author, is an excess of bile in the body (translated from the ancient Greek “melancholy” - “black bile”).
Since then, doctors have repeatedly made attempts to define this still not very understood disease more accurately and clearly. In the 1920s, German psychiatrist Kurt Schneider stated that there were two types of depression, each requiring a different form of treatment: “endogenous depression,” caused by mood swings, and “reactive depression,” caused by the experience of external events. In 1926, British psychologist Edward Mapother criticized this theory, writing in the British Medical Journal
that the existence of two types of depression has not been proven and that the obvious differences observed in depressed patients are simply differences in the severity of their condition.
Today Schneider's typology is out of fashion. Instead of his definition of depression, others were proposed to be used, and from the twenties to our time there were many such proposals. In 1969, American existentialist psychologist Rollo May wrote in his book Love and Will that “depression is the inability to construct a future,” and in 1987, cognitive psychologist Albert Ellis ) stated that depression, unlike “normal sadness,” is caused by “irrational belief”—“absolutist, dogmatic ideas about what is desirable and what should be”—and that this deprives sufferers of the ability to effectively deal with even minor setbacks.
In 1952, the American Psychiatric Association attempted to standardize definitions of mental illness, including depression, by classifying these illnesses. In the first edition of the Diagnostic and Statistical Manual (DSM), depression was classified under the broad category of “disorders without a clearly defined physical cause.” Schizophrenia, paranoia and mania also fell there. DSR-III, published in 1980, was the APA's first attempt to make definitions of specific diseases clearer by specifying symptoms; The new edition provides guidance on distinguishing depression from other disorders such as schizophrenia, dementia and uncomplicated grief, and outlines eight symptoms of depression, including “poor appetite or significant weight loss” and “complaints of decreased ability to think or concentrate, or severe the presence of such a malaise.”
According to the authors of these guidelines, if an adult patient has at least four of the eight symptoms they specified, his condition meets the criteria for clinical depression.
The DEM-V, published in 2013, finally devoted an entire chapter to depressive disorders. The diagnostic criteria remained largely the same, but an additional symptom emerged: “Almost every day, a predominantly depressed mood while awake, as evidenced by either a subjective report (eg, feeling sad or empty) or observation made by others (eg, being tearful). )".
Some scientists believe the definition of DSR-V is still too vague. In 2011 in the journal World Psychiatry
psychiatrist Daniel Goldberg noted that many of the symptoms outlined in the DSD are contradictory, which can complicate the work of researchers seeking to come to a more precise understanding of depression. “A patient with psychomotor retardation, hypersomnia, and increasing weight is assessed as having the same symptoms as one who is agitated, sleeping poorly, and losing weight,” Goldberg wrote.
Many studies conducted in recent years support the validity of Goldberg's concerns. For example, in 2000, a group of researchers from Johns Hopkins University, studying the symptoms of almost 2,000 patients, tried to identify types of depression. However, scientists have not been able to integrate gender, family history, symptoms and severity of the disease into a single picture. “Depression is heterogeneous,” the researchers concluded, adding that “the severity of a given illness appears to be more informative than the nature of symptoms.” And in 2010, German scientists, testing the validity of the DSR-IV definition of depression, found that a huge number of patients with “a wide variety of combinations of comorbidity, personality traits, features of a depressive episode and demographic characteristics” fall under its criteria. These results, they said, “challenge our understanding of major depression as a homogeneous entity with a strictly defined place in the classification of diseases.”
According to Scott Monroe, a psychology professor at the University of Notre Dame du Lac, part of the problem is that depression is considered a syndrome rather than a disease.
A disease is a specific condition characterized by the presence of a specific cause and corresponding physical manifestations, while a syndrome is a collection of signs and symptoms that are known to often appear together, but are not reducible to any one known cause.
In a paper published in June in the journal Current Directions in Psychological Science
, Monroe called on scientists to develop a more precise definition of depression.
“Problems arise from the prevalence of vagueness and imprecision,” he writes, “and vague ideas based on dubious similarities and differences may ultimately turn out to be clearly erroneous.”
Part of the reason scientists are still working under a “dominance of vagueness and imprecision” is that there is no clear answer to the question of what causes depression. The dominant hypothesis in the 1960s is that it is caused by a chemical imbalance in the brain, namely low levels of the neurotransmitter serotonin. As a result, pharmaceutical companies have spent enormous amounts of money developing “selective serotonin reuptake inhibitors” (SSRIs), drugs that increase serotonin levels in the brain.
Until now, these drugs (in particular, Paxil
,
Zoloft
and
Prozac
) are the type of antidepressant that is most often prescribed, even though research has shown that low serotonin levels do not necessarily cause depression.
And in 2010, the results of a review of three decades of research on antidepressants were published. According to this review, SSRIs may provide significant benefit for severe depression, but their effectiveness for mild to moderate depression “may be minimal or non-existent.”
Part of the problem, says Bruce Cuthbert, director of development of translational testing and treatment for adults at the National Institute of Mental Health (NIMH), is that researchers tend to focus on finding a universal treatment method that cannot be found.
“When you do a clinical trial, you diagnose a lot of people with depression, but they're all very different,” says Cuthbert. - It's like comparing apples, pears and tangerines. Don't expect any significant effect. Don’t expect to be able to say, “This treatment works for all fruits.”
In Cuthbert's opinion, efforts to develop a single treatment for depression are akin to similar efforts by oncologists: the approach is too broad to be really useful.
“To those treating depression, DMR has been touted as the ‘Bible,’ when at best it is a dictionary with a set of terms and an explanation for each term,” NIMH Director Tom Insel said in 2013. ). “Unlike our definitions of coronary artery disease, lymphoma or AIDS, DSD definitions are based on consensus regarding clusters of clinical symptoms rather than any objective laboratory findings.”
In 2010, Insel asked Cuthbert, then a psychology professor at the University of Minnesota, to help NIMH develop a new system for defining mental illness. As a result, the Research Domain Criteria (RDoC) was born in 2013, a system designed to change the way researchers think about mental disorders. Unlike DSD, disorder is not the core concept of RDoC; Instead, the classification is based on certain symptoms, such as fear, anhedonia (inability to feel pleasure), and desire or reluctance to work. In addition, the system lists the genes, neural circuits, physical responses, and self-reported behaviors associated with each symptom.
The theoretical foundation of the RDoC system is the idea that treating a specific symptom produces better results than treating a broad category of diseases. For example, some patients with depression experience anhedonia, while others do not. If researchers take a group of patients in which all suffer from anhedonia, but not all have a diagnosis of depression (anhedonia is common in schizophrenics), and treat this very specific symptom, they will get the best results.
The current definition of depression, Cuthbert explains, is dictated by scientists who observe patients and then create lists of symptoms based on their observations. “The logic here is: if you describe the disease in detail, you can define it,” he notes. However, according to him, it is becoming increasingly clear that, relying on the description of the disease, scientists, without going deeper into its understanding, are just skimming the surface. Cuthbert hopes the RDoC system will force them to take a closer look at the mechanics of each symptom. By doing this, they will be able to come up with more informed ideas about how to diagnose mental illness.
“We're starting to think differently about mental illness,” says Cuthbert. “The current diagnostic system is no longer suitable for research.”
“The current understanding of depression comes from a time when it was not very well understood,” he adds. “Now we know a lot more about it—thanks to physics, genetics, neurochemistry—and we need to use it.”
How is severe depression treated?
Helping yourself in difficult situations can be difficult. A depressed person is rarely able to adequately assess his condition.
If you manage to recognize anxiety symptoms in yourself or a loved one, do the following:
- Eliminate everyday problems, put an end to difficult relationships, change your least favorite job.
- Get examined by a therapist to identify other diseases. Get treatment if necessary.
- Contact a neurologist. It will determine the presence and type of pathology of the brain or central nervous system.
- Get treatment from a psychiatrist. He will explain how to get out of severe depression in your case.
Having discovered psychological problems, many are embarrassed to seek help and withdraw into themselves. In this case, only attentive loved ones can save the person. A timely visit to a doctor will prevent a tragic outcome and guide the patient along the path of healing.