Symptoms
According to the ICD, epilepsy is a chronic neurological disorder that manifests itself in the form of short-term or prolonged convulsive attacks called seizures.
The etymology of the disease dates back to ancient Greek times, when in the 4th century BC. Hippocrates, in one of his first greatest treatises, described the “Sacred Disease”, which at that time manifested itself mainly in clergy and high-ranking officials. Epilepsy has since remained an unknown, frightening disease. Only in the mid-twentieth century did scientists establish the true cause of epileptic seizures. It is associated with the sudden appearance of electrical impulses in the neurons of the brain, which provoke convulsions, a state of passion, a person performing unusual actions, etc.
The reasons for the development of epilepsy can be either inherent in the genetic nature of people or acquired. The first signs of the disease usually appear in childhood or adolescence, or in adults over sixty years of age. Epilepsy in its standard manifestation is secondary or symptomatic.
- disorders of brain development during puberty, subsequently characterized by hypoxia, birth injuries, and low birth weight of the newborn;
- genetically determined development of brain defects;
- congenital abnormalities in the psycho-emotional structure;
- the presence of genetic syndromes in the body;
- metabolic and endocrine disorders.
Among the acquired factors of the disease, infectious diseases of the brain (encephalitis, meningitis, neurocysticercosis), a stroke, the occurrence of a brain tumor, traumatic brain injury with subsequent mental and neurotic disorders, and multiple sclerosis should be highlighted. Signs of epilepsy can also arise in connection with the resulting intoxication, clearly expressed by various forms of addiction, especially alcoholism and drug addiction. According to the World Health Organization, every tenth alcohol-dependent person suffers from epileptic seizures.
Signs of epilepsy must be distinguished depending on the stage of development of the disease and the frequency of seizure recurrences. The initial stage is characterized by a short-term loss of connection with the outside world, imperceptible twitching of the eyes and facial muscles. The person seems to fall into a state of numbness or thoughtfulness for a few minutes, after which he continues to behave as usual.
Mild epilepsy is rarely diagnosed because the patient himself most often does not realize that he has symptoms of an attack. However, symptoms usually occur before the onset of an epileptic seizure, forming a special aura state. Experts call aura the sudden appearance of a feeling of bliss, a feeling of déjà vu (“already seen”) or jamavu (“never seen”), dizziness, and fever.
Epilepsy most often progresses until the age of eighteen and is accompanied by a gradual increase in the intensity and frequency of seizures. At first, attacks occur only once every few years or months, forming primary symptoms, then they are observed in the patient more and more often, occurring once or twice a month, or even a week. At a later stage of disease progression, epileptic seizures occur several times a day.
The primary signs of epilepsy are a grand mal seizure. The peculiarity of this seizure is that it appears suddenly and does not depend on any external stimuli. Primary symptoms appear a day or two before the onset of the attack and are expressed in lack of appetite, dizziness, fever, insomnia, and excessive irritability.
Then, just before the onset of the attack, an aura state is formed, after which the patient abruptly loses consciousness. During a fall, the patient emits an unusual loud cry, which is formed due to spasm of the glottis and the appearance of convulsive contractions in the diaphragm and chest. Further, the symptoms of epilepsy are expressed in the occurrence of tonic convulsions - tense stretching of the limbs and torso, unnatural throwing back of the head, holding the breath, convulsive clenching of the jaws.
There is also a circulatory disorder, manifested in a “white” complexion and swollen veins in the neck. Tonic convulsions last up to 20 seconds, after which they develop into jerky muscle contractions, accompanied by the appearance of foam from the mouth, often stained with blood due to the fact that the patient bites his tongue or cheeks during an attack.
Diagnosis of epilepsy begins with a family history. Information about the illness of close relatives is important.
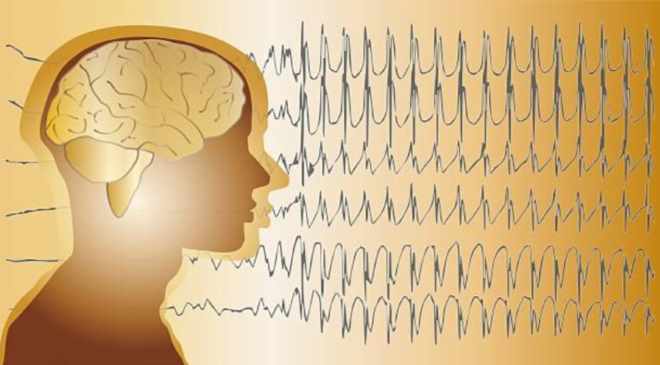
The leading and reliable diagnostic method is the electroencephalogram. Electrodes are attached to the patient's head to record brain activity.
The study is often carried out during sleep, since many patients have attacks that begin at night.
MRI is performed to identify structural changes in the brain. Magnetic resonance imaging can detect tumors, hematomas, and the consequences of a head injury.
MRI is also used to differentiate epilepsy from other diseases. A biochemical blood test helps identify hypoglycemia, sodium and potassium deficiency, which can cause seizures.
Hormone levels are also examined if endocrine disorders are suspected.
Dysphoria is characterized by a sudden change in a person’s emotional background in a negative direction. An attack of bad mood, melancholy, or depression can occur without any apparent reason and last several hours, less than a day.
A mild form of the disorder is often mistaken for special character traits of a person - the appearance of excessive grumpiness, touchiness, tearfulness, pickiness, or caustic causticity. In general, such a person has a dislike for society and its representatives and a tendency to conflict. This is most often observed in people suffering from epileptoid psychopathy.
However, the symptoms of dysphoria can vary significantly - some people experience psychomotor agitation, while others experience severe retardation. People with dysphoria, as a rule, cannot concentrate on surrounding events during an attack or answer questions asked of them.
If a dysphoric disorder goes from a mild form to a more protracted course - for several days, weeks, a person develops somatic as well as vegetative disorders:
- loss of appetite;
- change in sleep quality;
- sharp fluctuations in pressure parameters;
- dryness of mucous and integumentary tissues;
- tachycardia.
In severe cases, dysphoria will be characterized by the most pronounced anger, melancholy, apathy, and despair. In this case, the patient will have outbursts of anger, sometimes with semi-delusional shouting, which the person subsequently does not even remember. At the peak of negative emotions, dissatisfaction with oneself and others increases. To stop it, some people resort to alcoholic beverages, drugs, or try to die.
Clinical manifestations of epilepsy
The main symptom of epilepsy is epileptic seizures, or seizures. As a rule, they are short-lived (15 seconds - 5 minutes) and begin suddenly. Possible types of manifestation:
- Grand mal seizure: a person loses consciousness, falls, the muscles of the whole body involuntarily contract, foam comes out of the mouth.
- Minor epileptic seizure (absence): the patient loses consciousness for a few seconds. The face twitches convulsively. A person performs illogical actions.
Correct and timely treatment of the disease in 75% of cases can stop attacks or get rid of them forever (for more details, see epilepsy - symptoms and treatment).
What types of epilepsy are there?
When does epilepsy appear?
Epileptic seizures occur in people:
- up to 20 years in 75% of cases;
- after 20 years in 16%;
- in older age - about 2-5%.
The official side of the issue
Epilepsy attack. Tonic and clonic phases.
Despite numerous discoveries in the field of this disease, many countries today do not adequately recognize a disease such as epilepsy. For example, in China and India, patients suffering from epileptic seizures are legally prohibited from marrying or officially obtaining employment.
A strict law banning marriage also existed in the UK until 1970, and in the USA an epileptic could legally be denied entry to various public places, be it a theatre, cafe or concert. Negative attitudes towards people suffering from epileptic seizures are also evident in the Russian Federation.
The World Health Organization, along with the International League Against Epilepsy and the International Bureau of Epilepsy, annually conduct a number of awareness-raising and charitable events to raise awareness and further change people's attitudes towards this neurological disease. Such activities are aimed at studying how the symptoms of the disease manifest themselves, aspects of providing first aid during an epileptic attack, providing patients with all necessary medications at the state and regional levels, as well as expanding treatment options for all patients with epilepsy.
Official statistics state that around the world there are about 50 million people with recurrent attacks of epilepsy. Ten percent of people have experienced an epileptic attack at least once in their lives that is not associated with brain disorders. Symptoms similar to an epileptic seizure can occur after experiencing a sudden shock, a nervous breakdown, or post-traumatic stress disorder.

The person experiences sudden spasms throughout the body, numbness, trembling, panic attacks, or complete apathy. Also, epilepsy symptomatically overlaps with some mental illnesses, and therefore, when the first symptoms of an attack occur, it is necessary to consult a doctor and carry out a differential diagnosis, and then receive appropriate treatment.
Epileptic dementia
One of the most serious disorders in epilepsy is epileptic dementia. Its cause is a change in the cerebral cortex, which occurs due to frequent seizures. Sometimes intelligence is reduced due to traumatic brain injuries that the patient could receive during an attack, for example, by falling and hitting his head on the floor. Scientists note that children's brains are more susceptible to changes that provoke dementia.
Epileptic dementia is directly related to personality and character disorders. Slowness and fluidity of actions leads to a slowdown in gaining new experience, a person’s combinatorial function weakens, memory deteriorates, and intellectual abilities decline. Over time, dementia provokes the formation of straightforwardness, the horizons narrow, many are unable to distinguish trifles from worthwhile matters, jokes from serious words. Speech becomes intermittent, many people use a lot of words with diminutive connotations, for example, “crib”, “water”, “pillow”.
Over time, many patients focus exclusively on their health and symptoms and can only talk about topics related to the disease. Because of this, epileptic dementia is often called concentric.
Sometimes dementia develops against the background of twilight seizures and the use of certain potent medications. Once these symptoms and side effects are eliminated, the dementia is eliminated.
Treatment
Treatment of the disease is aimed at reducing the frequency of attacks and preventing complications.
Drugs to treat the disease:
- Anticonvulsants (Carbamazepine, valproic acid). Reduce pathological brain activity.
- Nootropics (Vinpocetine, Mexidol) improve cerebral circulation.
- Psychotropic drugs are prescribed when epilepsy is combined with mental disorders.
Surgery is used in cases of drug resistance and in the absence of effect from other methods.
The following types of operations are performed:
- Lobectomy (temporal lobe resection).
- Lesinectomy (removal of a damaged area of the brain).
- Callosotomy (dissection of the corpus callosum).
- Vagus nerve stimulation.
- Hemispherectomy (removal of the hemisphere).
- Neurostimulator implantation.
Non-traditional methods of therapy include:
- Breathing exercises by Strelnikova. It is based on alternating inhalations and exhalations, as a result the patient’s tension is relieved.
- Massage of the collar area, back. The purpose of the massage is to reduce muscle spasms and calm the nervous system. The movements of the massage therapist should bring relaxation.
- Diet. The ketogenic diet has been shown to be effective in reducing the number of seizures. When carbohydrates are reduced in the diet, the body begins to use fats as an energy source. In most patients, such nutrition leads to remission.
- Starvation. This is a radical method that can be used under the supervision of a doctor. Fasting may help patients who are resistant to anticonvulsants. During fasting, metabolism changes, which leads to a reduction in the number of attacks.
- Folk remedies. Decoctions of medicinal herbs that have a calming effect (valerian, lemon balm, mint, angelica root) are used.

The above symptoms disappear after a few minutes, and the patient enters the stage of muscle relaxation. Immediately after the attack, he does not react to external stimuli and has dilated pupils. The absence of protective reflexes and the appearance of involuntary urination are also noted. The patient fully regains consciousness only after some time and then falls into a deep sleep.
The consequences of an epileptic attack occur almost immediately after the shock experienced by the body. Patients complain of a general state of drowsiness, fatigue, exhaustion, but perceive an attack of epilepsy as if experienced in a dream.
Diagnosis of the disease is accompanied by identifying diseases similar in symptoms to epilepsy and conducting an electroencephalographic examination (EEG). Epilepsy appears on photographs in the form of sharp waves and peaks that form pathological brain activity. During diagnosis, medications are also used that activate areas of the brain that cause seizures, functional tests are taken, the fundus of the eye is examined, and CT and MRI are performed.
Treatment of the disease in both adults and children is based on taking special anticonvulsants, eliminating risk factors for the progression of epilepsy, psychological work with the patient and his adaptation to the conditions of social life. As preventive measures, it is necessary to consider giving up tonic drinks, smoking, alcohol, also maintaining a sleep schedule, having a balanced diet and avoiding the active influence of external factors on the body.
Epilepsy is one of the neurological diseases that are chronic in nature. It is possible to completely eliminate the symptoms of epilepsy and repeated relapses only in two-thirds of cases of the disease, therefore, when the first suspicion of epilepsy appears, it is necessary to urgently consult a neurologist and receive appropriate treatment.
Rating: (Votes: 1, 5.00 out of 5)
Personality and mental disorders in epilepsy require careful diagnosis and careful treatment. Sometimes for rehabilitation it is necessary to involve several specialists (neurologist, psychotherapist, psychiatrist), since any drug for the treatment of epilepsy can worsen the severity of psychosis, and vice versa.
For the medicinal treatment of personality disorders, antipsychotics and antidepressants are used, and therapy is always carried out under the strict supervision of doctors; an electroencephalogram is often necessary to monitor brain activity in the treatment of psychosis. Depending on the severity of mental symptoms, inpatient treatment under the close supervision of doctors may be required.
The first stage of any treatment is a thorough examination and accurate diagnosis. The Comprehensive Mental State Assessment Scale (CMS) test helps identify dysphoria. There are also several methods for diagnosing gender identity, one of which is the S. Bem questionnaire.
At the second stage, the doctor selects an individual treatment plan. It may include drugs for the treatment of the underlying disease (anti-epileptics, neuroleptics, barbiturates), relief of symptoms of dysphoria (treatment of depressive episodes with antidepressants, suppression of outbursts of aggression with sedatives).
Group or individual psychotherapy helps to cope with a severe psychological condition.
Dysphoria is a pathological change in the emotional sphere that can signal serious problems. Lack of proper treatment can lead to serious irreparable consequences. If you notice symptoms of dysphoria, do not delay your visit to the doctor.
Diagnosis of epilepsy
Which doctor should you contact if you suspect epilepsy? Conversation with the patient.
People at particular risk of developing epilepsy should undergo regular examinations by a neurologist after injury. If severe attacks occur, the patient should consult a doctor.
First, the specialist conducts a general examination and performs tests to identify neurological disorders. When making a diagnosis, the doctor takes into account the clinical picture, data obtained from EEG and neuroimaging.
Clinical picture
The diagnosis of epilepsy is often made when a doctor visits a patient during an emergency attack. If a person seeks medical attention because they suspect a seizure, the doctor will ask for their medical history, including seizure history.
— Electroencephalography (EEG). The most important diagnostic tool for detecting epilepsy is the EEG, which records and measures brain waves. Long-term monitoring may be required when patients do not respond to medications. EEG is not an absolutely reliable method. Repeated EEGs are often necessary to confirm the diagnosis, especially for some partial seizures.
— Videoelectroencephalography (videoEEG). For this test, patients are admitted to a special department of the hospital where they are monitored with an EEG and also monitored with a video camera.
Patients, especially those with difficult-to-treat epilepsy, may need to undergo video EEG monitoring for a variety of reasons, including seizures or drug additions before surgery for anything, or if non-epileptic seizures are suspected.
— Computed tomography (CT). A CT scan is usually the initial test with a brain scan for most adults and children with their first seizures.
This is a fairly sensitive imaging method and is suitable for most purposes. In children: even if the test results in everything being normal, the doctor must be sure that there are no other problems.
CT scanning is a much more sensitive method than x-rays, it provides high video resolution when viewing bone structures and soft tissues.
— Magnetic resonance imaging (MRI). Doctors strongly recommend an MRI for children with their first seizures who are younger than 1 year or who have seizures associated with any unexplained significant mental or motor problems. MRI can help determine whether a disease can be treated with surgery, and MRI can be used to guide surgeons.
Symptoms
Epilepsy is a serious disease of the human brain that is accompanied by characteristic symptoms. Let's take a closer look at the causes of epilepsy in adults and the consequences of this disease.
When seeing an epileptic attack, many people wonder how epilepsy is transmitted and whether it can be contracted from a sick person. In fact, this disease is not infectious, for example, such as influenza, chickenpox or acute respiratory infections. It can only arise due to the influence of the following factors:
- hereditary predisposition;
- acquired predisposition of an adult.
Epilepsy can be inherited. This fact can be explained by the predisposition of the brain or its appendages to hyperreactivity, as well as the special state of neurons and their tendency to excite. This rare feature is contained in the human genetic code and can be transmitted from sick parents to children. Additional causes of epilepsy attacks may include:
- meningitis;
- traumatic brain injuries;
- encephalitis;
- severe damage to brain structures due to taking drugs or alcohol;
- cyst.
What causes epilepsy after the above diseases? The fact is that such severe brain damage leads to the emergence of special neurons in it that have a low excitation threshold.
Groups of these neurons form the so-called epileptic focus, which contributes to the “capture” of nerve impulses. They spread to all the cells surrounding them, thus attracting all new neurons. Depending on the functions that these connections performed, during a seizure a person may have autonomic, mental, motor or sensory disorders.
Another reason why epilepsy occurs is cancer in the brain. With this disease, brain tissue changes and is damaged greatly, which can give some impetus to the development of epilepsy.
Epilepsy most often manifests itself with its characteristic seizures. They are classified depending on the damage to neuronal functions:
- A motor attack is the most common. With it, muscle cramps are observed in the hands, feet and face of the patient. There may also be involuntary shouting of individual words or sounds. Usually an attack occurs for no reason and spreads first to one part of the body and then to the second.
- A sensitive attack is accompanied by a sensation of pain and tingling in different parts of the body. It is as if a person conducts an electric current through himself. In addition, he may experience ringing in the ears and suffer from dizziness. In more severe cases, the patient may lose consciousness.
- Vegetative attacks are characterized by an unpleasant sensation in the stomach of displacement of internal organs and increased salivation. In this condition, a person’s blood pressure rises sharply. Thirst and changes in complexion may also occur.
- A mental attack causes a sharp deterioration in memory, changes in behavior and mood. A person may suddenly experience an inexplicable feeling of fear or panic. There is also a feeling of déjà vu, hallucinations and mental seizures.
In addition, epileptic seizures are divided into the following subcategories:
- absence seizures are a type of seizure in which a person loses consciousness for 10-20 seconds. At the same time, the brain seems to switch off from work, and the patient may freeze in mid-sentence. Additional symptoms of this condition include eyelid twitching, increased heart rate, and gesticulation. After the attack ends, the person returns to his normal state;
- myclonic seizures are accompanied by severe muscle spasms, tremors and jerking of the body. In this case, the patient may also throw back his head, tuck his legs and fall to his knees.
The consequences of an epileptic attack cannot always be predicted, so it is very important to properly provide first aid to such a person. Despite the fact that epilepsy is still considered an incurable disease, its diagnosis does not mean a death sentence for a person. Moreover, with the right therapy and taking special medications, seizures can be stopped.
The bigger problem with epilepsy is the psychological part of the disease, since a person with such a disease often faces misunderstanding and even fear from people around him who are afraid of seizures. Because of this, the patient has to change his job and lifestyle.
Also, due to the death of neurons, people with epilepsy may experience frequent mood swings, depression and even changes in personality, so you need to be extremely patient and intelligently perceive such psychological reactions in the patient’s nervous system.
Doctors have not yet been able to find out the general causes of this disease. The disease is not directly related to heredity, however, the risk of its occurrence increases significantly if one of the family members is sick. Approximately 40% of people with this diagnosis have close relatives who also have epilepsy.
Another group of patients are people who have suffered a traumatic brain injury, concussion, or stroke. A brain tumor and various cerebral circulation disorders due to past infectious diseases or congenital weakness of cerebral vessels can also give impetus to the development of epilepsy.
Epilepsy can appear at any age, but it is most often experienced by adolescents and young people under 20 years of age. Another risk category is old people over 60 years of age. According to WHO, approximately 5–7 people out of a thousand suffer from this disease.
In 70% of cases, the cause of the disease remains unclear.
Epilepsy is characterized by the occurrence of short-term seizures, accompanied by muscle twitching and loss of consciousness. It can be hereditary and acquired.
A major convulsive seizure begins suddenly, sometimes precursors of an attack occur several days before its development:
- headache;
- insomnia;
- excessive irritability;
- lack of appetite.
The main cause of the disease is considered to be the formation of foci in the brain that generate paroxysmal discharges in the structures of nerve cells.
In addition, the development of pathology can be facilitated by:
- severe concussions;
- neuroinfections;
- intrauterine infections;
- birth injuries;
- malformations of the brain;
- chromosomal diseases;
- oncology;
- metabolic disorders.
The pathological condition begins suddenly without warning, and the condition itself is unstable and short-term. Its duration is about several hours. The patient's consciousness is gripped by fear, rage, anger, and melancholy. The patient is disoriented, cannot understand where he is, who he is, what year it is.
Epilepsy: first aid
The main thing is to remain calm. How to identify epilepsy? If a person has convulsions and the pupils are dilated, then this is an epileptic seizure. First aid for an epileptic seizure includes ensuring safety: the epileptic’s head is placed on a soft surface, sharp and cutting objects are removed. Do not restrain convulsive movements. It is forbidden to put any objects into the patient’s mouth or unclench his teeth.
When vomiting occurs, the person is turned over on his side so that the vomit does not end up in the respiratory tract.
The duration of convulsions is a couple of minutes. If the duration lasts more than 5 minutes or there are injuries, call an ambulance. Afterwards the patient is placed on his side.
Minor attacks do not require outside intervention.
Epilepsy, the first symptoms of which can frighten an unprepared person, requires certain protection of the patient from possible injury during a seizure. For this reason, for epilepsy, first aid involves providing the patient with a soft and flat surface under him, for which soft things or clothing are placed under the body.
It is important to free the patient’s body from constricting objects (primarily this concerns the chest, neck and waist). The head should be turned to the side, giving the most comfortable position for exhaling vomit and saliva.
The legs and arms should be held slightly until the seizure is over, without resisting the convulsions. To protect the tongue from bites, as well as teeth from possible fractures, something soft (napkin, scarf) is placed in the mouth. When the jaws are closed, they should not be opened. Water should not be given during an attack. When falling asleep after a seizure, you should not wake the patient.
Types of epilepsy
There are several types of epileptic seizures of varying severity: from short-term loss of consciousness to uncontrolled muscle contraction with the appearance of foam at the mouth. The last attacks are the most dangerous; they can result in death due to tongue retraction or spasm of the pectoral muscles.
If a small part of the brain is responsible for the seizure, then the seizure is called partial or focal. When the entire brain is affected, we can talk about the onset of a generalized seizure. There are also mixed attacks; they start from a small area and quickly spread over the entire surface of the brain, involving more and more new areas.
In the most severe cases, when medications do not help, the doctor may suggest surgically removing the lesion. During this operation, the part of the brain that is responsible for seizures is cut out, after which epileptic seizures stop. However, this method of treatment is used only in extreme cases and for its successful implementation it requires a very experienced doctor and the most modern equipment.
Forms of epilepsy
Its division is based on the genesis and category of attacks:
- Local (partial, focal) - epileptic disease of the frontal, temporal, parietal or occipital zone.
- Generalized:
- idiopathic – the root cause remains unidentified in 70-80% of cases;
- symptomatic – due to organic brain damage;
- cryptogenic - the etiology of epileptic syndromes is unknown, the form is considered intermediate between the previous two.
Memory problems with epilepsy
elena757575, writes July 16, 2020, 1:26 pm Borisoglebsk, 44 years old
Gender: Female Required: neurologist, vertebroneurologist
Hello. I have been suffering from epilepsy for 3.5 years. Previously, the attacks were frequent, 10 times a month, now 2 times. After the attacks there was a very severe loss of memory, I don’t remember the names of people I knew, many events fell out of my memory, my thinking became very inhibited. I took bilobil forte, ciraxon, and now pantogam, but it was of little use. Memory worsens every day, but attacks become less frequent. After the attack, the temperature rises significantly (38 degrees) for 2 days and has a strong craving for sweets. Before the attacks there is weakness, dizziness, objects blur, and you also really want sweets. On normal days I measured my glucose level – 5.9, but after the attacks it didn’t work. Is it necessary to do this? How to get memory back and is it possible? Doctors say that this is normal for epilepsy, but I can’t work because I’m lost in the situation. An accountant by profession.
Hello, Elena! With such memory loss, it is necessary to raise the question of disability with doctors. What treatment are you currently receiving?
I have group 3. Depakine Chrono 500, 1 tablet morning and evening. Finlepsin 200 - 1 tablet in the morning and 2 in the evening, Seizar 100, 1 tablet in the morning and evening, Pantogam 250, 1 tablet in the morning, afternoon and evening. I just want my memory to be restored.
Are you being seen by a doctor? 3 antiepileptic drugs is too much.
Of course, every 3-4 months
Simple memory training techniques
Memorization. It has long been known that cramming does not develop memory. And 80-year-old scientists remember specialized information better than their young students. It's all about the structure of the perception of information, and not about its chaotic swallowing.
Epilepsy in pregnant women
Many antiepileptic drugs inhibit the effectiveness of contraceptives, which increases the risk of unwanted pregnancy. If a woman wants to be a mother, then she should not be persuaded - it is not the disease itself that is inherited, but only a genetic predisposition to it.
In some cases, the first attacks of epilepsy appeared in women while bearing children. An emergency treatment plan was developed for such women.
If you have epilepsy, it is possible to give birth to a healthy child. If the patient is registered with an epileptologist, then when planning a pregnancy, scenarios for its development are prepared in advance. The expectant mother should know the effect of anticonvulsants on the fetus and undergo timely examinations to identify pathologies in the child’s development.
6 months before the expected pregnancy, drug therapy is reviewed. Often, doctors completely stop anticonvulsants if there have been no seizures in the last 2 years and there are no neurological abnormalities. Then there is a high probability of pregnancy occurring without seizures in the presence of epilepsy.
Experienced doctors recommend monotherapy, when one drug is selected with a minimum dosage to control attacks.
Buy online
Problems of qualification of anxiety disorders in epilepsy
The classification of both mental and anxiety disorders in epilepsy is the subject of ongoing debate [11, 36, 37].
Authors studying mental disorders in epilepsy use 2 different approaches or a combination of them when assessing anxiety disorders. The first approach is to use established classifiers (DSM and ICD) in these cases, i.e., different categories of anxiety disorders. Within this approach, numerous studies have demonstrated an increased risk of comorbidity between epilepsy and specific anxiety disorders. Thus, a study conducted in Germany [13] using a structured clinical interview to identify Axis I disorders according to DSM-IV showed an increase in the prevalence of social phobia (7.2%), specific phobia (6.2%), and panic disorder (5. 1%), GAD (3.2%) compared with rates in the general population (1.24, 4.8, 1.1 and 1.2%, respectively). Similar data were reported in a population-based study of the prevalence of anxiety disorders in England [18], showing significantly increased odds of GAD, social phobia and agoraphobia in epilepsy compared with the general population (adjusted risks 2.6, 5.2 and 3.2, respectively). . In several studies, the incidence of obsessive-compulsive symptoms/disorders was higher in epilepsy compared with the general population, but varied widely depending on the patient population studied and the method of assessment. Thus, in patients with temporal lobe epilepsy, the incidence of obsessive-compulsive disorder was estimated at 10-22%, while patients with idiopathic generalized epilepsy did not differ in this indicator from the control group [38]. A study of the prevalence of mental disorders in adolescents 13-14 years old with epilepsy compared with the control group revealed, along with a high level of attention deficit hyperactivity disorder (21.6 and 4.3%, respectively), an increased prevalence of specific phobias (32.4 and 13.8 %), obsessions (31.1 and 9.1%), panic attacks (36.5 and 9.9%) and post-traumatic stress disorder (44.6 and 12.5%) [39].
It is worth noting that direct use of classification system criteria may have a negative impact on the diagnosis of epilepsy itself. For example, the classic manifestations of a partial seizure in mesotemporal epilepsy easily fit into the criteria for a panic attack (a short, circumscribed episode of intense fear or discomfort, reaching a maximum intensity within minutes and associated with autonomic manifestations, somatic and mental symptoms). Muscle tension, butterflies in the stomach, fear of losing control or going crazy, and other symptoms can occur during any phase of epilepsy. If the diagnosis of epilepsy is not considered at all at a medical appointment, for example if there is insufficient history of seizures, this can lead to erroneous diagnosis and treatment. Even if the same drug is used for both cohorts of patients (for example, mood stabilizers), secondary improvement in mental symptoms may, according to V. Beletsky and S. Mirsattari [40], “deflect” the diagnosis even further from neurological
Another approach to the qualification of anxiety disorders is their assessment as a consequence of the epileptic process itself and further differentiation depending on the time of occurrence relative to the epileptic attack. The level of anxiety is assessed, as a rule, using self-questionnaires (for example, HADS) without describing its features or attempts at classification [41]. With this approach, anxiety manifestations in epilepsy should belong to the category of organic mental disorders, or more precisely, to the section “anxiety disorders due to a general somatic condition” (or “due to other diseases,” i.e., epilepsy). Proponents of this approach draw attention to the fact that mental disorders (including anxiety disorders) are clinically different from those observed in psychiatric practice. For example, attention is drawn to the main "source" of anxiety in PE - fear of injury or death during an attack, which cannot be classified into any known DSM-IV category, including the diagnosis of GAD, which requires symptoms disproportionate to the actual source of anxiety. The legitimacy and validity of this approach, which assumes the independence of an organic anxiety disorder that does not have a strictly specific set of characteristics characteristic only of these categories, according to V.V. Kalinin [42], seems controversial and even speculative. Indeed, when diagnosing an organic anxiety disorder, the authors do not indicate its diagnostic criteria or specifications, but focus on the differences between anxiety states in epilepsy and anxiety-phobic disorders. Thus, the diagnosis of organic anxiety disorder is based not on positive (diagnostic) characteristics, but on negative (differential) characteristics.
Within this approach, it has been shown that periictal anxiety occurs in a significant number of PEs, some of whom may experience either exclusively preictal, ictal, or postictal anxiety, while others experience a combination of both [34]. A seizure prediction study [43] found an association between increased self-reported anxiety and next-day risk of seizures.
It is the periictal manifestations that are most difficult to attribute to any specific anxiety disorder. Moreover, manifestations such as ictal fear, postictal panic, or a panic attack in general may be a manifestation of an epileptic seizure, even despite the difficulty of differentiating them based on electroencephalographic (EEG) characteristics [44].
Ictal anxiety is the most common emotion accompanying seizures and occurs in 20% of PE [45], more often in temporal lobe and focal epilepsy compared to the generalized form [46]. Such anxiety is often a sudden onset of intense fear that clinically resembles panic attacks [47], but according to D. Chong et al. [48], is a clinical reflection of the activity of the convulsive focus and the manifestation of an aura, which allows us to consider it as a paroxysmal (epileptic) phenomenon. The literature describes several cases of intractable temporal lobe epilepsy previously misdiagnosed as panic disorder. Compared to ictal fear, panic attacks last longer and also almost never occur during sleep [11]. In addition, ictal attacks of fear are more stereotypical and are more often accompanied by deja vu
, automatisms, are less often associated with depressive symptoms and anticipatory anxiety [48].
According to the views of some authors [49], the level of perception (perceptual system) and apperception (perception based on previous experience, subjective interests, etc.) of attacks in PE is the most important predictor of anxiety. At the same time, according to other researchers [50], the psychological well-being of patients is in no way related to the occurrence of epileptic paroxysm, including its type (generalized or focal). Another difference between PE of different localization is the fact that patients with left-sided temporal lobe epilepsy tend to exaggerate their depressive and anxiety symptoms when filling out self-questionnaires, while patients with right-sided temporal lobe epilepsy tend to underestimate them [51].
In a recent study [48], which included 512 patients with focal epilepsy, 36 (7%) experienced ictal fear. Such fear was associated with auras, accompanied by olfactory and visceral complaints, deja vu
and
jamais vu
, derealization, cardiac symptoms, shortness of breath and a feeling of constriction in the chest. Fear did not correlate with gender or age, but epileptic foci were most often found in the right temporal lobe.
Anxiety symptoms may be postictal, occurring 12 to 72 hours after an attack, or may represent an increase in interictal anxiety. In a large prospective study of postictal psychiatric symptoms52 in patients with intractable partial epilepsy, anxiety was the most common symptom: 45% of patients reported significant anxiety for an average duration of 6–24 hours after more than 50% of attacks. Using a questionnaire assessing psychopathology, and cognitive symptoms, it was possible to find that more than 90% of patients with interictal psychiatric symptoms reported their post-ictal exacerbation - worsening fear of an attack, increased persistent anxiety and symptoms of agoraphobia, which were largely associated with the fear of a second attack.
The third approach, a compromise and pathogenetically more justified, assumes the presence of both anxiety disorders due to epilepsy and comorbid anxiety disorders, classified under the headings of the ICD or DSM and fully complying with the proposed criteria. This approach assumes that PE may suffer, in addition to anxiety as part of epilepsy, from comorbid anxiety-phobic disorders, like any other patient, for example, with somatic pathology. Most often, such disorders include interictal anxiety states that manifest themselves during the interictal period. As part of this approach, in 2007, the ILAE Commission on the Psychobiology of Epilepsy proposed a new classification of mental disorders in epilepsy [53], which does not compete with the known classification systems in psychiatry, but rather establishes boundaries between disorders that meet the DSM criteria (anxious, depressive, somatoform, dissociative disorders), and specific for epilepsy. The latter authors include psychopathological symptoms that are the main manifestation of attacks (anxiety, confusion, disorientation, memory disorders, dysphoria, hallucinations) and special categories of interictal disorders that are specific to epilepsy and have characteristic features - psychoses in epilepsy, affective somatoform (dysphoric) disorders. As for anxiety and phobias specific to epilepsy, the authors identify only “fear of an attack” as a separate category, noting its maladaptive nature. At the same time, the authors emphasize that when qualifying any symptoms, it is necessary to determine their relationship with the appointment or withdrawal of AEDs and with changes in the EEG.
Bidirectional relationships of anxiety and epilepsy and common biological substrates
The bidirectionality of the relationship between anxiety and epilepsy, described back in the 80s of the 20th century [54], is confirmed in modern epidemiological and clinical works. Data from a long-term cohort study in the UK [55] showed that anxiety is more common in patients in whom epilepsy manifests in the next 3 years than in the control group (18.5 and 13.8%, respectively), and the likelihood of anxiety disorders in epilepsy is also higher. for at least 3 years higher than in the control group. Another comparative epidemiological study [56], including US veterans over 65 years of age with and without epilepsy, found that anxiety preceding the first epileptic seizure was significantly more common in PE than in the control group (11.7 vs. 8). .5% respectively). Children assessed immediately after their first unprovoked seizure showed significantly higher levels of anxiety compared to established norms [57]. A Swedish demographic study [58] found that patients hospitalized for anxiety disorders were 2.6 times more likely to develop epilepsy than those without a history of hospitalization.
The high prevalence of anxiety disorders in epilepsy and the bidirectionality of their relationship to the underlying disease suggests not only joint mechanisms for the implementation of these conditions, but also common biological substrates [7, 59].
The genetic link between anxiety and epilepsy is supported not only by familial clustering studies, but also by genotyping results. A longitudinal study [60] of childhood epilepsy found that among first-degree relatives, the likelihood of an unprovoked seizure was significantly associated with the presence of an anxiety disorder. In a Brazilian study [61], genotyping of serotonin transporter gene polymorphisms was carried out in 155 patients with temporal lobe epilepsy, and the presence of a specific allele (C allele of the 5-HT1A C-1019G polymorphism) was an independent risk factor for the development of anxiety diagnosed on the basis of a structured clinical interview .
Data from experimental and clinical studies [62, 63], establishing a pathogenetic link between epilepsy and anxiety, confirm neurobiological theories indicating abnormalities in the neurotransmitter systems (serotonin, norepinephrine, dopamine and GABA), especially in the limbic system (in particular, the amygdala) . Previous studies suggested the role of the dopaminergic system in “igniting” subictal activity and the formation of affective disorders, including anxiety disorders [54]. More recently, serotonin imbalances have been repeatedly linked to both epilepsy and anxiety disorders. Thus, a positron emission study in patients with severe mesiotemporal epilepsy and panic disorder showed similar results, namely a decrease in the binding potential of serotonin type 1A receptors (5-HT1A) in epilepsy in hyperexcitable neurons and in the limbic system compared to the control [64 ], and in panic disorder - in the anterior and posterior cingulate gyrus and in the raphe region [65]. It was found that the genetically prone to epilepsy rat (GEPR) strain, which serves as an experimental model for it, has congenital pre- and postsynaptic deficiencies in serotonin and norepinephrine transmission [66].
GABA also plays a role in the pathophysiology of anxiety and epilepsy. This hypothesis is supported by the simultaneous antiepileptic and anxiolytic effects of benzodiazepines, which act as GABA agonists, as well as the provocation of panic symptoms in patients with panic disorder by the benzodiazepine agonist, flumazenil [63]. In addition, drugs related to ligands of the α2δ subunit of voltage-gated calcium channels, such as pregabalin, also have both anti-anxiety and anticonvulsant potential [67]. Some studies report evidence of non-drug approaches to reduce stress and anxiety (eg, progressive muscle relaxation) and have anticonvulsant potential, even in patients with drug-resistant forms of epilepsy [68].
Neuroimaging studies [69] have demonstrated that decreased amygdala volume is associated with ictal fear, and changes in left amygdala volume are associated with subclinical anxiety symptoms in a sample of healthy adults. However, data on amygdala volume in anxiety disorders and epilepsy remain controversial. On the one hand, patients with temporal lobe epilepsy and concomitant depression or anxiety showed an increase in amygdala volume compared to PE, but without affective disorders [70, 71]. On the other hand, L. Elst et al. [72] when studying interictal dysphoric disorder, found an inverse correlation - the smaller the volume of the amygdala, the greater the likelihood of the manifestation of certain psychopathological phenomena, including anxiety. In the same study, the authors proposed a dimensional approach to the problem of amygdala volume, based on the assumption that its volume reflects the dominant way of processing emotional information. According to this hypothesis, a “hyperstable” mode of emotional processing, such as phobic anxiety, is associated with increased amygdala volume, whereas emotional instability, expressed by psychotic anxiety, irritability, and aggression, is correlated with decreased amygdala volume.
Thus, recognizing the importance of the comorbidity of epilepsy with mental disorders, including anxiety disorders, is a priority of modern epileptology. Anxiety in PE is a multifaceted problem and its management requires an interdisciplinary approach. Clarifying the nature of anxiety in epilepsy allows clinicians to develop appropriate plans for optimal treatment of both epilepsy and comorbidities. Due to the fact that routine EEG is not a sensitive enough test to solve the complex differential diagnostic problems of epilepsy with comorbid anxiety disorders, clinicians must rely on their knowledge of the various variations of this symptomatology, taking into account the various forms of epilepsy, the time of onset of anxiety symptoms and its characteristics .
The authors declare no conflict of interest.
Causes of alcoholic epilepsy
Seizures can occur in two cases: when blood alcohol levels drop or some time after stopping drinking alcohol. This is due to the fact that long-term consumption of large amounts of alcohol leads to an increase in the seizure threshold in the body. And interrupting the supply of alcohol to the body leads to a sharp decrease in the threshold, as a result, epileptic seizures occur.
In addition, epilepsy may result from electrolyte and neurotransmitter imbalances (decreased inhibitory gamma-aminobutyric acid), which are common in patients with alcohol dependence.
Post-traumatic epilepsy

Post-traumatic epilepsy (PTE) occurs in most cases some time after a brain injury. The appearance of such a disorder is due to the healing processes of existing damaged structures. After an injury, regeneration processes begin. Functional nerve fibers, neurons, cannot recover. At the site of their death, foci of gliosis form.
Glia are additional cells that normally contribute to the normal course of metabolic processes, the transmission of nerve impulses and perform a number of other functions. The proliferation of glial cells allows one to compensate for damage and restore the conduction of nerve impulses between surviving neurons.
The restoration of nerve endings causes abnormal electrical activity to appear in the affected areas of the brain.
The first symptoms of epilepsy may appear as early as 5-7 days after TBI. However, in most cases, pronounced signs of pathology appear 1-2 weeks after a brain accident. In some cases, seizures appear several months and sometimes years after the injury.
Symptoms
The most characteristic manifestation of epilepsy that occurs after brain injury is seizures. Patients have specific triggers that can trigger a seizure. Often attacks occur after drinking alcohol, stress, physical overload, etc.
Often, several hours or days before a seizure, patients experience an aura, that is, a premonition or physical symptoms that may indicate an imminent seizure. This period manifests itself in different forms in different patients.
The most characteristic manifestations of the “aura” before an attack include:
- causeless anxiety;
- nausea;
- stomach ache;
- appetite disorders;
- insomnia;
- increased irritability;
- headache.
Seizures can be either convulsive or non-convulsive. In the first case, the patient may lose consciousness. Often there is a throwing back of the head and twitching of the muscles. Involuntary loud screams and foam at the mouth may occur. Sometimes involuntary urination or bowel movements occur.
After an attack, patients often experience spatial disorientation and short-term amnesia. In milder cases, the pathology does not lead to seizures accompanied by convulsive syndrome.
However, this does not mean that pathological epileptiform activity does not harm the brain. Often, against the background of epilepsy that occurs after a skull injury, mental and neurological disorders begin to increase.
Thus, epilepsy can cause the following changes:
- frequently changing mood;
- memory impairment;
- loss of ability to think soberly;
- personality change;
- the appearance of mania.
Dementia often develops against the background of a pathological condition such as epilepsy. This disorder gradually leads to the patient losing the ability to think sensibly, decreased cognitive abilities, impaired spatial orientation, etc.
Complications and consequences
It is important to understand the dangers of epilepsy. The main complication is status epilepticus, when the patient does not return consciousness between frequent seizures. Severe epileptic activity leads to cerebral edema, from which the patient can die.
Another complication of epilepsy is injuries due to a person falling on a hard surface, when any parts of the body get into moving objects, or loss of consciousness while driving. The most common types are biting the tongue and cheeks. When bone mineralization is low, strong muscle contraction causes fractures.
In the last century, it was believed that this disease provoked a mental disorder, and epileptics were sent for treatment to psychiatrists. Today, the fight against the disease is led by neurologists. However, it has been established that some mental changes do occur.