What is ophthalmoplegia, its types and treatment methods
The optic nerve belongs to the cranial peripheral nerves, but essentially it is not a peripheral nerve either in origin, or in structure, or in function.
This is the white matter of the cerebrum, the pathways that connect and transmit visual sensations from the retina to the cerebral cortex. The optic nerve delivers nerve messages to the area of the brain responsible for processing and perceiving light information. It is the most important part of the entire process of converting light information.
Its first and most significant function is the delivery of visual messages from the retina to the areas of the brain responsible for vision. Even the smallest injuries to this area can have serious complications and consequences.
Optic atrophy according to the ICD has ICD code 10
Causes
The development of optic nerve atrophy is caused by various pathological processes in the optic nerve and retina (inflammation, dystrophy, edema, circulatory disorders, toxins, compression and damage to the optic nerve), diseases of the central nervous system, general diseases of the body, hereditary causes.
The following types of disease are distinguished:
- Congenital atrophy - manifests itself at birth or a short period of time after the birth of the child.
- Acquired atrophy is a consequence of adult diseases.
Factors leading to optic nerve atrophy may include eye diseases, central nervous system lesions, mechanical damage, intoxication, general, infectious, autoimmune diseases, etc. Optic nerve atrophy appears as a result of obstruction of the central and peripheral retinal arteries that supply the optic nerve, as well as is the main symptom of glaucoma.
Characteristics[edit | edit code]
Limitation of abduction of the right eye. This person tries to look to the right, but the right eye refuses to turn in that direction.
Nerve dysfunction is caused by esotropia, a convergent strabismus at the fixation distance. At near fixation, the affected individual may have only latent deviation and be able to maintain binocularity or have less esotropia. Patients sometimes rotate their face toward the affected eye, moving the eye away from the affected lateral rectus muscle to control diplopia and maintain binocular vision.
Clinical picture
The clinical picture of abducens nerve paresis is characterized by the following signs.
- Limited mobility of the eyeball.
- Secondary deviation of the eye.
- Double vision.
- The position of the head is involuntary and forced.
- Dizziness.
- Orientation disorder.
- Uneven, uncertain gait.
With a mild form of paresis, the symptoms are mild and practically do not cause concern to the patient. While with paralysis the same symptoms are severe and cause significant discomfort.
- sharp deterioration of vision;
- unnatural protrusion of the eyeball;
- constant headaches;
- redness of the whites of the eyes;
- double vision;
- painful sensations in the eye;
- discomfort in the forehead;
- possible manifestation of conjunctivitis.
In severe forms of the disease, there may be a lack of activity and mobility of the eyeball, a deterioration in the reaction of the pupil to light and its immobility. If ophthalmoplegia develops against the background of other diseases, the clinical picture also includes additional symptoms.
Types of disease
In this case, the eye shifts to the zone of action of a healthy or less affected muscle. The patient has difficulty moving the eyes towards the paralyzed muscles, resulting in double vision.
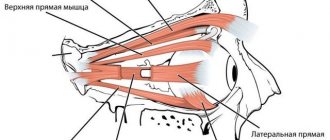
Based on the degree of damage to the optic nerves, partial and complete ophthalmoplegia are distinguished. Partial can be external, in which the work of the extraocular muscle of the eyelid is disrupted, and internal, if only the nerve columns are affected by paralysis.
In the full form of the disorder, there is immobility of the eyeball and drooping of the upper eyelid, and the inability of the pupil to respond to light.
Atrophy of the optic nerve of the eye occurs:
Partial optic atrophy
A characteristic feature of the partial form of optic nerve atrophy (or initial atrophy, as it is also defined) is the incomplete preservation of visual function (vision itself), which is important when visual acuity is reduced (due to which the use of lenses or glasses does not improve the quality of vision).
Although residual vision can be preserved in this case, there are disturbances in color perception. Preserved areas within sight remain accessible.
Complete atrophy
Any self-diagnosis is excluded - only specialists with the proper equipment can make an accurate diagnosis. This is also due to the fact that the symptoms of atrophy have much in common with amblyopia and cataracts.
In addition, optic nerve atrophy can manifest itself in a stationary form (that is, in a complete form or a non-progressive form), which indicates a stable state of actual visual functions, as well as in the opposite, progressive form, in which a decrease in the quality of visual acuity inevitably occurs.
Horizontal paresis
Horizontal disorders, accompanied by the inability to move both eyes in the same direction, are much more common than vertical ones. With horizontal control, a complex system is used, consisting of impulses from:
- cerebellar center;
- hemispheres;
- vestibular system, represented by the nuclei of the neck.
In the reticular formation of the bridge, the received signals are transmitted to the 4th cranial nerve, which, through a bundle of nerves, transmits them to the rectus and internal muscles on different sides of the skull. Acute brain injuries often develop due to circulatory disorders.

Provoking pathologies
The key reasons for the development of ophthalmoplegia are pathologies of nerve tissue. The disease can be congenital or acquired.
The congenital form in most cases occurs with other pathologies in the structure of the eye and is part of a complex of symptoms of various genetic anomalies. There is a hereditary cause of the disease.
The disease can develop against the background of other infectious diseases - tuberculosis or syphilis, as well as tetanus, botulism and diphtheria.
Ophthalmoplegia can be an accompanying symptom of ophthalmoplegic migraine, a rare disease that causes severe headache attacks.
82)Ticket
Polyemylit(installation sp-brain steam)
Etiology: poliovirus (coxsackievirus, enterovirus, ECHO?, RNA-soda)
Clinic:
forms:
- spinal
- bulbar
- pontic
- combined
Symptoms:
- fever
- cat.phenomena
- upset stool
- sweating
- rash
- urination disorder
- paresthesia
- mening.symptoms
- hemodin.violation
- AR oscillations
- dyspnea
- paresis
- impaired swallowing and phonation
- pairs of facial muscles
- por.per.horns SM
D-ka:
Treatment:
- constant mode
- painkillers
- warm
- san-kur.treatment
39) Medial longitudinal fasciculus and internuclear ophthalmoplegia
medial (posterior) rectus fasciculus - paired formation, complex in composition and function, starting from the nucleus of Darkshevich and the intermediate nucleus of Cajal at the level of the metathalamus. passes through the entire brainstem near the midline, ventral to the central peripontal gray thing, and under the bottom of the 4th ventricle of the brain, penetrates the anterior cords of the spinal cord, and ends at the cells of its anterior horns at the cervical level.
In general, thanks to him, the movements of the eyes of the apple are synchronous))
Defeat:
- DIFFERENT VIEW FORMS,
- strabismus
- nystagmus
It’s more annoying when:
- severe TBI
- Circulatory disorders in the brain stem
- when the brainstem is compressed by a tumor
- etc.
Possible following syndromes:
- paresis of gaze (vertical, horizontal)
- floating eye symptom
- Hertwig-Magendie sign
- Internuclear ophthalmoplegia
- Lutz syndrome
- sesquicentral syndrome
- oculocephalic reflex (phenomenon of the doll's head and eyes, doll eye test, Cantelli's symptom)
- convergent nystagmus
- vestibulo-ocular reflex
Internuclear ophthalmoplegia is a violation of the concomitant deviation of the eyeballs to the sides as a result of rupture of the connections of the medial longitudinal fasciculus between the nuclei of the abducens (VI) and oculomotor (III) nerves. On the affected side, there is a restriction of inward movement of the eye, while monocular (in one eye) nystagmus occurs in the other eye.
Internuclear ophthalmoplegia is more often observed with multiple sclerosis, stroke, less often with brain tumors, encephalitis, drug intoxication (diphenin, tricyclic antidepressants), Wernicke encephalopathy, traumatic brain injury, Lyme disease.
40) Damage due to herpetic infection. Herpetic encephalitis
- General intoxication
- people's psyche
- people's consciousness
- Nar.cortical functions (alexia, apraxia, acalculia)
Primyeloencephalic form of added mening.syndrome
Panecephalic syndrome: sudden onset coma, clonic-tonic seizures and general symptoms
+ brainstem syndromes (horizontal nystagmus, dynamic ataxia on the side of paresis
Encephalomyelitis form of the optic nerve + lower paraplegia + meningomyelitis syndromes (dissemal myelitis picture)
Symptoms of atrophy
Drug treatment
In order to reduce pain, relieve spasms and strengthen muscles, acupuncture, electrophoresis and phonophoresis with medications are prescribed.
Since the optic nerve carries visual images, the most common signs of its inflammation are the following:
- sudden deterioration of vision in one or both eyes;
- the appearance of black and white vision. Color vision, being more perfect, suffers first;
- Pain appears when moving the eyes. An optional symptom that may be absent if there are no signs of classic inflammation and swelling of the retrobulbar tissue;

The main sign of optic nerve atrophy is a decrease in visual acuity that cannot be corrected with glasses and lenses.
- With progressive atrophy, a decrease in visual function develops over a period of several days to several months and can result in complete blindness.
- In the case of partial atrophy of the optic nerve, pathological changes reach a certain point and do not develop further, and therefore vision is partially lost.
With partial atrophy, the process of vision deterioration stops at some stage, and vision stabilizes. Thus, it is possible to distinguish between progressive and complete atrophy.
Diagnostics
Despite the presence of pronounced external signs, the following hardware tests are prescribed;
Therapy consists of eliminating the causes of the disease, alleviating pain and restoring, if possible, nervous and muscle activity.
Physiotherapeutic methods
Diagnosis of the type of disease and the causes that cause it is necessary to select a treatment method.

The disease is diagnosed by initial examination. It has pronounced external manifestations. To establish the nature of the disease and its causes, consultation with a neurologist and ophthalmologist is necessary.
If neoplasms are detected, additional consultation with an oncologist may be required.
After receiving all the necessary data about the disease and determining the causes, treatment is prescribed. It is aimed at eliminating the factors that resulted in the development of ophthalmoplegia, relieving pain and maximizing the restoration of nervous and muscular activity.
Optic nerve atrophy is a fairly serious disease. In case of even the slightest decrease in vision, it is necessary to visit an ophthalmologist so as not to miss precious time to treat the disease.
Any self-diagnosis is excluded - only specialists with the proper equipment can make an accurate diagnosis. This is also due to the fact that the symptoms of atrophy have much in common with amblyopia and cataracts.
An examination by an ophthalmologist should include:
- visual acuity test;
- examination through the pupil (diluted with special drops) of the entire fundus of the eye;
- spheroperimetry (precise determination of the boundaries of the field of view);
- laser dopplerography;
- assessment of color perception;
- craniography with an image of the sella turcica;
- computer perimetry (allows you to identify which part of the nerve is damaged);
- video-ophthalmography (allows us to identify the nature of damage to the optic nerve);
- computed tomography, as well as magnetic nuclear resonance (clarifies the cause of optic nerve disease).
Also, a certain information content is achieved to compile a general picture of the disease through laboratory research methods, such as blood tests (general and biochemical), testing for borreliosis or syphilis.
Diagnosis and treatment
Treatment of ophthalmoplegia consists of eliminating the causes of the disease, relieving pain and restoring, as far as possible, muscle and nervous activity.
- anti-inflammatory drugs;
The earlier the disease is detected, the more likely it is to successfully get rid of it. Do not ignore visits to the doctor and try to cure yourself.
Treatment of optic atrophy is a very difficult task for doctors. You need to know that destroyed nerve fibers cannot be restored.
One can hope for some effect from treatment only by restoring the functioning of nerve fibers that are in the process of destruction, which still retain their vital functions. If this moment is missed, then vision in the affected eye can be lost forever.
When treating optic nerve atrophy, the following actions are performed:
- Biogenic stimulants (vitreous body, aloe extract, etc.), amino acids (glutamic acid), immunostimulants (Eleutherococcus), vitamins (B1, B2, B6, ascorutin) are prescribed to stimulate the restoration of altered tissue, and are also prescribed to improve metabolic processes
- Vasodilators are prescribed (no-spa, diabazole, papaverine, sermion, trental, zufillin) to improve blood circulation in the vessels supplying the nerve
- To maintain the functioning of the central nervous system, Fezam, Emoxipin, Nootropil, Cavinton are prescribed
- To accelerate the resorption of pathological processes - pyrogenal, preductal
- Hormonal drugs are prescribed to stop the inflammatory process - dexamethasone, prednisolone.
Medicines are taken only as prescribed by a doctor and after an accurate diagnosis has been established. Only a specialist can choose the optimal treatment, taking into account concomitant diseases.
D. Monocular double vision (double vision when looking with one eye)
Symptoms depend on which nerve is affected. Such injuries cause paralysis that is easily recognized. With paresis of the oculomotor nerve, in addition to strabismus, mild exophthalmos may be observed, caused by hypotonia of the rectus muscle with preserved tone of the oblique muscles, which contribute to the protrusion of the eyeball outward.
We invite you to familiarize yourself with Pilocarpine eye drops - instructions, price, reviews and analogues
Trauma (history is helpful) sometimes results in bilateral orbital hematomas or, in extreme cases, rupture of the oculomotor nerve.
Compression by a tumor (or giant aneurysm), especially a parasellar one, causes slowly increasing paresis of the extraocular muscles and is often accompanied by involvement of the optic nerve, as well as the first branch of the trigeminal nerve.
Other space-occupying lesions, such as supraclinoid or infraclinoid aneurysms of the carotid artery (all of the above are typical, slowly increasing involvement of the oculomotor nerve, pain and sensory loss in the area of the first branch of the trigeminal nerve, rarely calcification of the aneurysm, which is visible on a simple x-ray of the skull; later - acute subarachnoid hemorrhages).
An arteriovenous fistula in the cavernous sinus (a consequence of repeated trauma) ultimately leads to pulsating exophthalmos, a pulse-synchronous noise that is always heard, congestion in the conjunctival veins and in the fundus. When the oculomotor nerve is compressed, the early symptom is mydriasis, which often appears before paralysis of eye movements.
General increase in intracranial pressure (usually the abducens nerve is involved first, later the oculomotor nerve).
After lumbar puncture (after it, a picture of damage to the abducens nerve is sometimes noted, but with spontaneous recovery).
Infections and parainfectious processes (spontaneous recovery is also noted here).
Tolosa-Hunt syndrome (and paratrigeminal Roeder syndrome) are very painful conditions that present with incomplete external ophthalmoplegia and sometimes involvement of the first branch of the trigeminal nerve; characterized by spontaneous regression within a few days or weeks; steroid therapy is effective; relapses are possible.
Meningitis (includes symptoms such as fever, meningism, general malaise, damage to other cranial nerves; it can be bilateral; cerebrospinal fluid syndrome).
Neoplastic and leukemic infiltration of the meningeal membranes is one of the known causes of damage to the oculomotor nerves at the base of the brain.
Cranial polyneuropathies as part of spinal polyradiculopathies of the Guillain-Barre type; isolated cranial polyneuropathy: Miller Fisher syndrome (often manifests itself only in bilateral incomplete external ophthalmoplegia; ataxia, areflexia, paralysis of the facial muscles, protein-cell dissociation in the cerebrospinal fluid are also noted), idiopathic cranial polyneuropathy.
Diabetes mellitus (an uncommon complication of diabetes, observed even in its mild form, the oculomotor and abducens nerves are usually involved, without pupillary disorders; this syndrome is accompanied by pain and ends with spontaneous recovery within 3 months. It is based on microvascular ischemia of the nerve.
Ophthalmoplegic migraine (a rare manifestation of migraine; a history of migraine helps the diagnosis, but other possible causes must always be excluded).
Multiple sclerosis. Damage to the oculomotor nerves is often the first symptom of the disease. Recognition is based on generally accepted diagnostic criteria for multiple sclerosis.
Idiopathic and completely reversible isolated lesion of the abducens nerve (most often found in children) or oculomotor nerve.
Infectious diseases such as diphtheria and intoxication due to botulism (swallowing paralysis and impaired accommodation are noted).
Such disorders are almost always accompanied by other symptoms of central nervous system damage and are usually bilateral.
We invite you to read Azarga instructions for use, Azarga price, Azarga description, Azarga buy
In nuclear oculomotor palsy, the different muscles innervated by the oculomotor nerve rarely exhibit the same degree of weakness. Ptosis usually appears only after paralysis of the external eye muscles (“the curtain falls last”). The intrinsic eye muscles are often spared.
CVA in the brainstem (sudden onset, accompanied by other brainstem symptoms, mainly cross-symptoms and dizziness. Brainstem symptoms, usually including nuclear oculomotor disorders, are manifested by well-known alternating syndromes.
Tumors, especially stem gliomas and metastases.
Traumatic brain injury with hematoma in the brain stem area.
Syringobulbia (does not progress for a long period, there are symptoms of damage along the length, dissociated sensitivity disorders on the face).
Double vision can also be observed in some other lesions, such as chronic progressive ophthalmoplegia, toxic ophthalmoplegia due to botulism or diphtheria, Guillain-Barré syndrome, Wernicke encephalopathy, Lambert-Eaton syndrome, myotonic dystrophy.
Finally, diplopia has been described in cases of clouding of the lens, incorrect correction of refraction, and diseases of the cornea.
Monocular diplopia is always intriguing to the neurologist. This condition can often be either psychogenic or caused by a refractive error in the eye (astigmatism, impaired transparency of the cornea or lens, dystrophic changes in the cornea, changes in the iris, a foreign body in the media of the eye, a defect in the retina, a cyst in it, defective contact lenses).
This situation doesn't happen often. Its main causes are: fracture of the orbital base involving the inferior rectus muscle; thyroid orbitopathy involving the inferior rectus muscle, ocular myasthenia, damage to the third (oculomotor) cranial nerve, damage to the fourth (trochlear) cranial nerve, skew deviation, myasthenia.
More rare causes: orbital pseudotumor; myositis of the oculomotor muscles; primary orbital tumor; entrapment of the inferior rectus muscle; third nerve neuropathy; aberranetic reinnervation in case of damage to the third nerve; Brown's syndrome (strongrown) is a form of strabismus caused by fibrosis and shortening of the tendon of the superior oblique muscle of the eye;
double elevator paralysis; chronic progressive external ophthalmoplegia; Miller Fisher syndrome; botulism; monocular supranuclear gaze palsy; vertical nystagmus (oscillopsia); myokymia of the superior oblique muscle of the eye; dissociated vertical deviation; Wernicke's encephalopathy; vertical one and a half syndrome; monocular vertical diplopia.
Course of therapy
Treatment methods for paresis of the eye muscles in children are not particularly different from those in adults. However, it must be borne in mind that most congenital anomalies are corrected through surgery.
If the operation is successfully performed, the extraocular muscles are partially or completely restored. If the problem is compression of the nerve pathway, then the main task is to eliminate the cause.
After eliminating the factor influencing the development of muscle paresis, treatment is adjusted towards restoring blood flow and damaged nerve fibers. For this purpose, exercises that strengthen the oculomotor muscles are often used.
They serve as the basis for the treatment of minor injuries and are a good preventive measure. In severe cases of the disease, therapeutic exercises well complement the main course of therapy.
Drug therapy for paresis may include the following:
- Vitamin complexes;
- Preparations for strengthening the extraocular muscles and restoring their innervation;
- Eye drops;
- Medicines that improve blood circulation;
- Corrective glasses and bandages.
The pathology can be treated with medications only according to the regimen prescribed by the doctor, so as not to aggravate its course and not to impair vision, especially if the child is sick. It is recommended to combine drug therapy with other methods, namely:
- Steriopictures. By watching them, the extraocular muscles are trained and blood flow improves. The nerve tissues that innervate the muscles of the eye are extremely tense during the procedure, due to this the lost innervation is restored. The procedure must be carried out under the supervision of a specialist so as not to cause complications;
- Electropheresis. This physiotherapeutic procedure is carried out with a 1.5% solution of Neuromidin. The duration of one session of electropheresis usually does not exceed 20 minutes, and it acts directly on the synapses (junctions) of the muscle and nervous tissue of the eyeball. After a course of such therapy, the patient’s severity of paresis decreases and the innervation of the eye muscles improves.
It is impossible to eliminate some causes of paresis in children, for example, congenital anomalies, without surgical intervention. Their duration and degree of risk depend on the type of operation and the factor that influenced the development of the pathology. In the case of severe damage to the optic nerves, it will not be possible to completely eliminate the problem, but there will be a chance to save the child’s vision.
Due to paresis of the extraocular muscles, many complications develop, such as strabismus, ptosis, etc. In children, this pathological process is often a consequence of congenital anomalies. It may not appear immediately, but only over time. This is why it is important to see an ophthalmologist and other doctors, especially in the first years of a child’s life.
It is impossible to eliminate some causes of paresis of the eye muscles in children, for example, congenital anomalies, without surgical intervention. Their duration and degree of risk depend on the type of operation and the factor that influenced the development of the pathology. In the case of severe damage to the optic nerves, it will not be possible to completely eliminate the problem, but there will be a chance to save the child’s vision.
≫ More information on the topic: https://nashinervy.ru/perifericheskaya-nervnaya-sistema/prichiny-pareza-glaznyh-myshts-u-detej.html
Notes[edit | edit code]
- ↑ Disease Ontology release 2019-05-13 - 2019-05-13 - 2020.
- ↑ Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2020.
- ↑ Ehrenhaus, MP. Abducens Nerve Palsy.
eMedicine.com. October 9, 2003. - ↑ The meaning of this term can be found, for example, https://en.wikipedia.org/wiki/Suppression_(eye)
- ↑ Harley RD. Paralytic strabismus in children. Etiologic incidence and management of the third, fourth, and sixth nerve palsies.Ophthalmology. 1980 Jan;87(1):24-43.
- ↑ Vallée L, Guilbert F, Lemaitre JF, Nuyts JPAnn Pediatr (Paris). 1990 May;37(5):303-5. Benign paralysis of the 6th cranial nerve in children,
- ↑ False localizing signs - Larner 74 (4): 415 - Journal of Neurology, Neurosurgery & Psychiatry
- ↑ AM Gubler: De l'hémiplégie alterne envisagée comme signe de lésion de la protubérance annulaire et comme preuve de la décussation des nerfs faciaux. Gazette hebdomadaire de médecine et de chirurgie, Paris, 1856; 3: 749–754, 789–792, 811–816. English translation in Wolf, The classical brain stem syndromes. Springfield, Thomas, 1971.
- ↑ Halo Orthosis Immobilization - Spine - Orthobullets.com
- ↑ Bansal S, Khan J, Marsh IB. Unaugmented vertical muscle transposition surgery for chronic sixth nerve paralysis. Strabismus. 2006 Dec;14(4):177-81
- ↑ Britt MT, Velez FG, Thacker N, Alcorn D, Foster RS, Rosenbaum AL.Partial rectus muscle-augmented transpositions in abduction deficiency.J AAPOS. 2003 Oct;7(5):325-32.
- ↑ Neugebauer A, Fricke J, Kirsch A, Rüssmann W. Modified transposition procedure of the vertical recti in sixth nerve palsy. Am J Ophthalmol. 2001 Mar;131(3):359-63
Preventive measures
Ophthalmoplegia can develop against the background of other neurological diseases. A complete preventive examination should be completed 2 times a year in order to identify them in time and begin treatment.
Optic atrophy is a serious disease. To prevent it, you need to follow some rules:
- Consultation with a specialist if there is the slightest doubt about the patient’s visual acuity;
- Prevention of various types of intoxication
- promptly treat infectious diseases;
- do not abuse alcohol;
- monitor blood pressure;
- prevent eye and traumatic brain injuries;
- repeated blood transfusion for profuse bleeding.
Timely diagnosis and treatment can restore vision in some cases, and slow or stop the progression of atrophy in others.
Disorders with similar symptoms
Symptoms of the following conditions may be similar to those of progressive supranuclear palsy (PSP). Comparisons may be useful for differential diagnosis.
- Corticobasal degeneration (CBD) is a rare, progressive neurological disorder characterized by the loss and shrinkage (atrophy) of cells in certain areas of the brain (cerebral cortex and basal ganglia). The symptoms and signs of this disease resemble some patients with PSP, and some experts believe that CBD and PSP are variations of the same disease. Both are tauopathies.
- Multiple system atrophy (MSA) is a rare progressive neurological disease characterized by a variable combination of parkinsonism and cerebellar ataxia (poorly coordinated limb movement, unsteady gait and dysarthria). Many patients with MSA also develop dysfunction of the autonomic nervous system, which controls blood pressure, heart rate, sweating, bowel movements, and bladder. The exact cause of multiple system atrophy is unknown.
- Shy-Drager syndrome is a subtype of multiple system atrophy with autonomic failure. Most experts no longer use this term.
- Parkinson's disease is a slowly progressive neurological condition characterized by involuntary shaking (resting tremor), muscle rigidity or inflexibility, slowness of movement (bradykinesia), and difficulty making voluntary movements (akinesia). Degenerative changes occur in areas deep inside the brain (substantia nigra and other pigmented areas of the brain), causing a decrease in dopamine levels in the brain. Dopamine is a neurotransmitter, a chemical that sends a signal from one nerve cell to another in the brain. Parkinson's disease progresses much more slowly than PSP and usually does not cause disability for ten years or more.