Temporary loss of consciousness, which is caused by vascular dystonia by a temporary spasm or sudden dilatation of the cerebral arteries, is called fainting or syncope. The clinical picture consists of three stages: precursors, the actual fainting state and recovery.
When a vascular crisis approaches, its development can be prevented. For treatment, sedatives are used, vasoactive drugs are prescribed after determining the mechanism of the attack.
Causes of fainting with vegetative-vascular dystonia
If the flow of blood to the brain decreases by 3-5 times, then fainting occurs with loss of consciousness and a sharp decrease in muscle strength. This leads to a fall if the patient fails to sit or lie down in time. Various factors can influence arterial tone:
- stress;
- attack of pain;
- type of blood or dental, diagnostic procedures;
- staying in stuffy rooms;
- standing for a long time;
- physical or mental fatigue;
- insufficient duration or depth of sleep;
- exposure to heat or sunlight;
- drinking alcoholic beverages;
- infectious diseases.

Of particular importance in the development of fainting conditions are: low blood pressure, hyperventilation of the lungs in response to external or internal stimuli, orthostatic drop in pressure during a sharp change from horizontal to vertical position.
We recommend reading the article about neurocirculatory dystonia. From it you will learn about the causes, types and symptoms of pathology, diagnosis and treatment.
And here is more about vascular tone.
Why does fainting occur?
Loss of consciousness associated with disruption of the adequate functioning of the autonomic nervous and vascular systems is a common symptom of dystonia.
A sudden change in body position causes disruption of blood circulation in the vessels of the brain. There is a short-term oxygen deficiency and loss of consciousness. Deterioration in well-being is provoked by:
- staying inside an unventilated room;
- severe stress;
- hunger, hypoglycemia - nutritional deficiency for the brain;
- fear.
Fainting with vegetative-vascular dystonia is safe for life, but falling is associated with the risk of injury.
Paroxysms are characteristic of the hypotonic type of the disease. It is with it that a sharp decrease in blood pressure often occurs, causing fainting. Less commonly, a similar condition occurs with a mixed form of vascular dystonia in people suffering from the cardiac, hypertensive variant.
Presyncope and immediate loss of consciousness appear following the precursors - a complex of predominantly similar symptoms:
- sudden deterioration in health;
- severe weakness;
- the appearance of a dark veil in the eyes, flickering of flies;
- tinnitus;
- heavy sweating;
- numbness of hands, feet;
- nausea.
Paroxysm occurs a few seconds or minutes after the listed unpleasant sensations. Therefore, you need to urgently take action if you feel these symptoms approaching.
Symptoms of approaching loss of consciousness
The fainting state can last from 1 - 2 seconds to 3 minutes. At this time, there is a feeling of rolling weakness, a sudden loss of strength in the muscles (“legs give way”), lack of air, darkening in the eyes or flashing dots, noise or ringing in the head. If during this time the patient managed to lower his head, sit down or lie down, then the attack stops.
When syncope occurs, consciousness may be flickering (periods of loss and clarity alternate) or partial; with complete loss, the pupils are dilated, slow to respond to light, the pulse is thready, and blood pressure is low.
With deep fainting, convulsive muscle twitching and involuntary release of urine are noted.
At the end of the attack, patients complain of instability when walking, a general feeling of weakness, sweating and dry mouth. At the same time, tendon reflexes are not impaired, memory of previous events is preserved, speech is clear, slightly slow. These signs can help distinguish syncope during vegetative-vascular dystonia from acute disturbance of cerebral blood flow and traumatic brain injury.
Watch the video about vegetative-vascular dystonia, its manifestations and treatment:
Prevention of fainting
Self-help when fainting occurs due to VSD consists primarily of taking preventive measures.
- Active walks in the fresh air. Light jogging is a great option.
- Performing simple physical exercises. Excessive loads must be avoided.
- Inclusion in the diet of foods rich in potassium and magnesium (buckwheat and oatmeal, carrots, soybeans, eggplants). In the morning, freshly squeezed juice will be useful, and at night you can drink soothing teas. It should be noted that the breakfast of patients suffering from fainting must be complete. Under no circumstances should you skip your morning meal.
- Avoiding situations of stress, mental and physical fatigue.
- Performing breathing exercises, autogenic training and relaxation techniques.
- Healthy sleep (at least 8 hours long).
- Refusal of bad habits, exhausting diets and self-medication.
We recommend that you read: What can hurt in the left side?
What is the danger
The longer the pre-fainting state lasts, the more chances the patient has to hold on to a stationary object and protect himself from falling to the ground or floor. The rapid development of an attack leads to injury. The consequences of syncope can be:
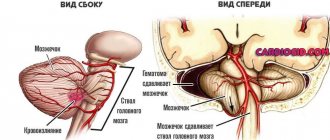
- traumatic brain injury,
- fractures and dislocations of limbs,
- spinal injury,
- soft tissue injuries,
- bleeding,
- injury.
In an unsuccessful scenario, a fatal outcome cannot be ruled out; such conditions pose a particular danger when operating complex mechanisms.
Signs and symptoms of presyncope: dizziness, nausea
Symptoms of presyncope are characterized by sudden development, which is usually provoked by certain factors. A stuffy room, tight clothing, stressful situations, excessive physical activity, eating - all this can contribute to the onset of an attack.
The most characteristic symptom of presyncope is dizziness, which may be accompanied by nausea. This indicates disturbances in the functioning of the human autonomic system.
There is a certain risk group of people for whom the presyncope may be permanent. These are people suffering from hypotension (low blood pressure), chronic anemia (low hemoglobin level in the blood, less than 100 units), bradycardia (low heart rate, less than 40 beats).
Any of the described signs is a serious reason to see a doctor. But, since an attack of pre-fainting can occur at any time and in any place, it is necessary to have at least a general understanding of how to provide first aid to the victim or yourself at home.
First aid for yourself when fainting approaches
The most important thing is to take a sitting or lying position. In summer it is better to go into the shade, and in winter to sit on a bench. If this is not possible, then you should lean your elbows on any close, stable object (wall, fence, tree), while trying to tense your body muscles as much as possible. Some people find that bending their torso down helps, but you also need to hold on to something.
When fainting approaches, you can sit down on one knee, as when tying shoelaces, in order to protect yourself from head injuries in the event of a fall.
Then you need to concentrate on breathing slowly (this is very important) and deeply into your belly. At the same time, rub your ears well with your hands, pressing until it hurts on the area under the nasal septum (in the dimple of the upper lip). If you are prone to syncope, you need to have ammonia or a piece of fresh ginger with you. They are sniffed when you feel faint.

Preventing Fainting
If a patient with vegetative-vascular dystonia feels the approach of a fainting paroxysm, and there are no loved ones nearby, then a number of actions can be taken to help prevent loss of consciousness. So, you need to do the following:
- Free your neck from suffocating clothing.
- Sit down urgently.
- If you have the strength, then open the window or go outside.
- Try to inhale the aroma of any substance with a pungent odor.
- Do breathing exercises using a paper or plastic bag. That is, just breathe into it. This will saturate the blood with carbon dioxide and thereby stabilize the condition.
- Lie down and elevate your legs slightly to improve blood flow to the brain.
Important: in order to prevent fainting, it is advisable to constantly train the blood vessels. Jogging, walking, swimming, and contrast showers are suitable for this. Regularity of exercise is very important.
Help for someone who has fallen
When providing first aid, the patient must be laid on the ground or floor, with the head at the level of the body, and it is better to raise the legs, placing the victim’s bag or things under them. Then the collar of the clothing is unbuttoned to ensure air flow. You must open a window indoors.
If a person is unconscious for more than 2 - 3 minutes, then you need to urgently call an ambulance, as this is life-threatening. You should seek medical help in any doubtful situations, but do not try to treat yourself by giving nitroglycerin or heart drops, as they can further lower blood pressure and aggravate cerebral ischemia.
Help for someone who has fainted
Causes and features of the condition
It is known that with vegetative-vascular dystonia, jumps in blood pressure often occur. Poor blood circulation and improper functioning of blood vessels provoke oxygen deficiency, which leads to fainting.
Most often, a prefainting state is observed in patients with VSD of the hypotonic type. With the mixed type, the likelihood of fainting is not so high. Pre-fainting in the morning in most cases is observed precisely with arterial hypotension.
In addition, dystonics often suffer from various phobias and panic attacks, which, in turn, provokes the release of adrenaline into the blood. The patient begins to breathe more often, tries to absorb more and more air, as a result of which the balance of oxygen and carbon dioxide levels is disrupted.
It is worth noting that in this case, fainting will only benefit the patient, since with “turned off” consciousness the required level of oxygen in the blood will be restored. A pre-fainting state with VSD can last up to about three minutes.
Presyncopal condition with VSD what to do
Vegetative-vascular dystonia is characterized by various signs and symptoms from different systems. The patient has cardiac, neurological, respiratory, etc. disorders. But one of the most unpleasant signs of pathology is fainting with vegetative-vascular dystonia. How to deal with them and what first aid looks like in case of loss of consciousness is discussed below in the material.
As a rule, fainting with vegetative-vascular dystonia is observed due to disruption (dysfunction) of the autonomic nervous system. In particular, loss of consciousness is observed in young people and girls who are tall and have an asthenic physique. At the same time, in patients with frequent fainting, it is the hypotonic or hypertensive type of dystonia that is identified. That is, there are problems with blood vessels.
If we consider the fainting state from the point of view of the process occurring in the body, then the picture looks like this:
- A person with vegetative-vascular dystonia, with a sudden change in body position or in other predisposing conditions, experiences vascular, namely venous insufficiency. That is, blood enriched with oxygen does not reach the brain cells so quickly.
- With a sudden change in body position, the heart cannot cope with the movement of blood. The pressure in the lumen of the vessels drops.
- As a result of this phenomenon, the brain experiences hypoxia.
- In turn, oxygen starvation provokes fainting. The patient loses consciousness.
Important: It is worth understanding that brain cells do not tend to accumulate oxygen and glucose. Neurons need a constant flow of blood to be properly nourished. If the brain does not receive important microelements, a person faints. As a rule, loss of consciousness is short-lived and lasts from a few seconds to several minutes. For a short duration of fainting, the brain cells are not affected in any way.

Vascular pathologies, and subsequently fainting, can occur in the following cases:
- sudden change in body position (sharp rise from a sitting or lying position);
- severe and sudden stress;
- prolonged physical fatigue;
- long stay in a stuffy room or car;
- sudden change in temperature (staying in a sauna/swimming in a cold pool);
- drinking alcoholic beverages.
Patients with hypertensive or hypotonic type of dystonia are advised not to make sudden movements when changing body position. The position needs to be changed slowly. At the same time, fainting conditions are more common in young people during adolescence than in older patients.
In most cases, patients who are prone to fainting feel a pre-fainting (half-fainting) state before the attack begins. It is characterized by the following symptoms:
- darkening of the eyes;
- feeling of weakness throughout the body and slight dizziness;
- coldness of the extremities and a feeling of numbness;
- sticky cold sweat on the palms and face;
- lack of air;
- feeling of panic and fear;
- tinnitus;
- mild convulsive syndrome;
- loss of coordination of movements.
If the patient feels a fainting state during VSD, it is advisable to have time to inform others about this before losing consciousness. If you sit down in time or lean your back on a hard surface, you can protect yourself and not fall with possible subsequent injury.

If a patient with vegetative-vascular dystonia feels the approach of a fainting paroxysm, and there are no loved ones nearby, then a number of actions can be taken to help prevent loss of consciousness. So, you need to do the following:
- Free your neck from suffocating clothing.
- Sit down urgently.
- If you have the strength, then open the window or go outside.
- Try to inhale the aroma of any substance with a pungent odor.
- Do breathing exercises using a paper or plastic bag. That is, just breathe into it. This will saturate the blood with carbon dioxide and thereby stabilize the condition.
- Lie down and elevate your legs slightly to improve blood flow to the brain.
Important: in order to prevent fainting, it is advisable to constantly train the blood vessels. Jogging, walking, swimming, and contrast showers are suitable for this. Regularity of exercise is very important.
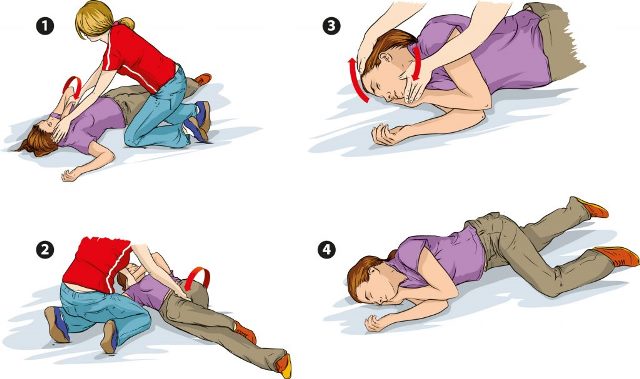
If you witness your neighbor or just a passer-by losing consciousness, then you need to help the person regain consciousness. You need to do the following:
- Place the person so that their legs are approximately 30 degrees above heart level.
- Open the clothes that are squeezing your chest and neck.
- Slap your cheeks.
- Give ammonia a whiff.
- As soon as the person regains consciousness, it is advisable to offer him sweet warm tea or other sweet drink.
It is worth understanding that dystonia is a whole symptom complex. And to get rid of it, it is important to lead a healthy lifestyle and maintain an optimistic attitude. Additionally, self-control during moments of paroxysms is beneficial to the patient.

Fainting with VSD is a typical symptom of a disorder in the functioning of the autonomic nervous system. This condition is not necessarily a sign that a person has dystonia; it may indicate other pathologies in the functioning of the body. However, fainting with vegetative-vascular dystonia has characteristic features, which can be found below.

Dysfunctions of the central nervous system, an invariable sign of vegetative-vascular dystonia, contribute to the development of fainting conditions. Under the influence of any of the factors, a sudden failure may occur, which will provoke the occurrence of fainting.
Causes of fainting during VSD:
- overstrain of body, mind and emotions;
- increased fatigue;
- constant or sudden stress exposure;
- sudden changes in air temperature, atmospheric pressure or weather patterns;
- prolonged presence in a room with a lack of oxygen and elevated air temperature;
- a sudden change in body position (for example, quickly rising from a lying position);
- consumption of alcoholic beverages.

After the body of a person with dystonia has felt the impact of at least one of the factors listed above, the following changes occur in it, manifested in a state of fainting:
- disturbances occur in the vascular links, leading to relaxation of smooth muscles and an increase in the lumens in the vessels;
- there is a decrease in blood pressure;
- the amount of blood supplied to the arteries of the brain decreases;
- brain tissue begins to experience an acute lack of oxygen;
- A protective reaction of the brain manifests itself in the form of a short-term shutdown of its basic functions.
Due to the fact that the tissues and vessels of the brain are incredibly sensitive to the amount of oxygen entering them, fainting occurs as a protective reaction of this organ to a sharp deficiency of the corresponding element.
The pre-fainting state does not last for an hour or two, it comes on suddenly and lasts from 3 seconds to 3 minutes. During this period of time, a person experiences the following changes in his own state:
- heart rhythm disturbances occur;
- sudden emptiness and lethargy sets in, accompanied by a drop in blood pressure;
- the outflow of blood from the brain causes darkness before the eyes;
- a sharp decrease in consciousness is accompanied by weakness;
- dizziness and fainting are interspersed with symptoms such as the appearance of black spots before the eyes and tinnitus.
From a medical point of view, the human body in a state of fainting shows the following:
- consciousness is lost or fleetingly clears up;
- pupils dilate;
- eyes react to light slowly and reluctantly;
- the pulse becomes weak, thread-like;
- blood pressure becomes extremely low;
- There may be tremors in the legs and some urine leakage.
After a person returns to consciousness, he may feel weak, have difficulty standing, sweat profusely, and complain of dry mouth mucous membranes. The speech of such a person will be clear, understandable, but somewhat slow. All these signs make it possible to distinguish fainting in a person with dystonia from the consequences of cerebrovascular accidents or TBI.
The main danger of a situation where fainting occurs is that the sudden development of such a situation can provoke the occurrence of injury in the person who has lost consciousness.
If the pre-fainting state lasted no more than 10 seconds, the patient falls to the floor without having time to react, sit down or lie down on anything.
Consequences of sudden fainting:
- receiving a traumatic brain injury;
- fracture;
- dislocation;
- damage to the spinal column;
- soft tissue injury;
- bruises;
- bleeding from damaged body surfaces.
Fainting during VSD is especially dangerous for people who work with complex machinery or drive vehicles. The rapid onset of fainting can lead to serious injury at work or an accident that can be fatal.
If you have vegetative-vascular dystonia, you can always prevent fainting and loss of consciousness - to do this, you should sit down or take a horizontal position.
A pre-fainting state with VSD can most often be felt, this means that the person understands that something is wrong with him and can try to go to a safe place, sitting down on the floor if possible.
First aid for fainting and its approach is as follows:
- sit or lie down, lean on a stable object;
- if you manage to lie down, place your legs a little higher than the entire surface of the body; hide in the shadows;
- provide a flow of fresh air;
- unfasten buttons or fasteners on clothing that interfere with the flow of oxygen to the respiratory organs;
- tense all muscles;
- tilt your head to the floor so that the blood rushes to your head;
- to squat;
- rub the ear area with your fingers;
- influence the surface located under the nose, at the level of the middle of the upper lip; try to breathe slowly, involving your stomach in every inhalation and exhalation;
- hold cotton wool moistened with ammonia near the nose;
- Sprinkle your face with water or another warm liquid.
When a person’s condition has stabilized, he should be offered a glass of sweet tea and not allowed to stand on his feet for some time, waiting for the blood vessels to stabilize.

If a person with dystonia has lost consciousness, they should be placed on a hard, flat surface with their feet elevated. After this, a set of measures should be carried out to return him to consciousness:
- Open a window or disperse the crowd to provide fresh air to the patient.
- Unfasten clothing that may interfere with his free breathing.
- Apply a cloth or heating pad soaked in warm water to the patient’s heels.
- Bring ammonia applied to a cloth or cotton wool to your nose. Under no circumstances should you insert these objects into the nasal passages, just gently move the cotton around the patient’s nose.
- In case of prolonged loss of consciousness (more than 3 minutes), call a doctor.
- Do not give the person heart drops or nitroglycerin tablets.
- After the person returns to consciousness, give him sweet, not hot tea.
- Prevention of fainting during VSD
To prevent fainting from becoming a frequent companion for a person with dystonia, he should seek help from a neurologist and therapist after the first such incident.
Specialists will prescribe therapy in the form of taking the following medications:
- improving blood circulation processes;
- normalizing the metabolism of neurons in the brain (nootropics);
- sedatives (sedatives);
- stimulating (in the presence of low blood pressure numbers).
It is very important to change your usual diet by including the following foods:
- buckwheat and oats;
- peas and beans;
- fresh vegetables (eggplant, parsley, onions, carrots);
- fruits (citrus fruits, plums, apricots);
- green tea.
Experts recommend changing your lifestyle towards a healthy one, which will certainly reduce the frequency of fainting:
- Give up bad habits, including smoking, sitting at the computer late and drinking alcohol.
- Maintain a bedtime and make your sleeping area comfortable.
- Be sure to alternate mental work with physical exercise.
- Walk more often.
- Do yoga.
- Carry out hardening procedures.
- Take a contrast shower to train the vascular system.
- Occasionally be in the sun, only at safe hours.
- Take vitamin supplements.
- Learn and apply breathing exercises.
In order to get rid of fainting, the effect of dystonia on the nervous system should be weakened. For this purpose, experts recommend taking teas with sedative herbs (mint or lemon balm) before going to bed, and fresh juices in the morning, with the addition of lemongrass (if you have low blood pressure).
With timely prevention of VSD, arrhythmia, hypertension, migraines, which includes maintaining a healthy lifestyle and proper nutrition, fainting will gradually disappear and will no longer bother the person.
Kuban State Medical University (KubSMU, KubSMA, KubGMI)
Level of education - Specialist
Research Institute of Cardiology named after. A.L. Myasnikova
NTsSSKh them. A. N. Bakuleva
Russian Medical Academy of Postgraduate Education
Cantonal Hospital of Geneva, Geneva (Switzerland)
Russian State Medical Institute of Roszdrav
Vegetative-vascular dystonia is divided into four types - hypotonic, hypertensive, cardiac and mixed. Neurosis, one of the varieties of which is VSD, causes an imbalance in the functioning of two types of the autonomic nervous system - sympathetic and parasympathetic. In case of increased activity of the parasympathetic nervous system, the syndrome develops according to the hypotonic type. It is characterized by weakness and fainting.
Fainting is a short-term loss of consciousness, lasting from a few seconds to 2 - 3 minutes. Usually a person comes to his senses without outside help. Fainting is not dangerous to life or health, except that you can get injured if you fall.
Under the influence of unfavorable external factors, the following pathophysiological processes are triggered in the body:

Thus, short-term fainting is a protective function of the brain from irreversible processes associated with a lack of oxygen.
Most often, the cause of fainting is severe emotional stress - stress, anxiety, overwork. In addition, fainting can be caused by:
- climate change or weather change;
- stuffiness in the room;
- sudden rise to the feet;
- motion sickness in transport;
- drinking alcohol.
A feeling of fear can also be a cause of fainting with vegetative-vascular dystonia.
Approaching fainting can be determined by several signs. Weakness with VSD is one of the first. Presyncope is also determined by symptoms:
- darkening or ripples before the eyes;
- ringing in the ears;
- dizziness and loss of coordination;
- anxiety, fear, panic;
- tremor of fingers;
- numbness of the limbs;
- pallor.

Knowing the signs of an impending vegetative-vascular paroxysm, you can take measures to prevent it. Presyncope with VSD can be relieved in the following ways:
- the first thing to do is sit down; people faint while on their feet and very rarely from a sitting position;
- go out into the fresh air or ventilate the room;
- sniff a substance with a pungent odor (ammonia or perfume);
- take a few breaths and exhales into a paper bag - this will help restore the required amount of carbon dioxide in the blood;
- while sitting, tilt your head down to increase blood flow to it.
The person needs to be reassured so that the panic attack does not lead to more severe manifestations of VSD syndrome - tachycardia or arrhythmia. Intellectual tension also helps to overcome the onset of fainting. You can count or read poetry out loud.
If loss of consciousness occurs, the person should be laid down with their legs slightly elevated. Unbutton a tight collar or blouse to allow free breathing. Light slaps on the cheeks will bring you back to consciousness, or you can sprinkle your face with cold water. The smell of ammonia brings you well.
After vegetative-vascular paroxysm, a feeling of weakness and severe weakness sets in. Hot sweet tea will help cope with it. Medical attention is not required for short-term fainting.

If paroxysm occurs for the first time, you should definitely consult a doctor to find out its cause. Fainting can be a symptom of other serious illnesses. With autonomic dysfunction, examination usually does not reveal any pathologies - neither cardiac nor cerebral. But this does not mean that VSD does not need to be treated.
Constantly being in an anxious state, imbalance of the autonomic nervous system, fainting, weakness in the legs with VSD over time have a negative effect on the heart and blood vessels.
As the main treatment, medicine suggests changing your lifestyle and taking sedatives. They will help relieve anxiety and normalize your emotional state.
For VSD of the hypotonic type, it is useful to take stimulating tinctures of ginseng, Rhodiola rosea (golden root), and Eleutherococcus. They will tone the blood vessels and prevent a drop in blood pressure, leading to fainting.
No wonder they say that movement is life. For patients with vegetative-vascular dystonia, physical activity is the main medicine. Physical exercise is mandatory to prevent weakness due to VSD, which leads to weakening of the heart muscle. The best effect in physical and emotional terms is provided by swimming, aerobics, and yoga.
The loads should be feasible and enjoyable. In addition to the swimming pool and gym, daily walking will be of great benefit. Mental stress is no less important than physical stress. Intellectual games, learning a foreign language, solving crosswords not only allows you to take your mind off dark thoughts, but also makes your brain work.
With vegetative-vascular dystonia, the normal conduction of nerve impulses is disrupted. Therefore, patients are recommended to include in their diet more foods rich in microelements such as potassium, phosphorus and magnesium - greens, legumes, buckwheat, eggplant, oranges, bananas, dried apricots or fresh apricots.
The hypotonic type of autonomic dysfunction may be accompanied by anemia. Therefore, the menu must include nuts, meat, liver and other offal. Hypotonic people can afford salty foods - marinades, herring, cheeses. Spices will raise the blood pressure - mustard, cinnamon, ginger, black pepper. It is healthy to eat chocolate, drink cocoa and coffee with sugar.
VSD is treated by a neurologist in collaboration with a psychotherapist and psychiatrist. You should not take prescriptions in the form of therapeutic exercises, aromatherapy or balneological procedures lightly. These types of treatments will help get rid of the syndrome faster than numerous pills.
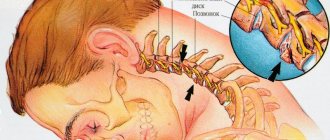
VSD and osteochondrosis
Cervical (as well as cervicothoracic osteochondrosis) and VSD are closely interrelated. Experts say that in almost 90-100% of cases, cervical osteochondrosis leads to vegetative dystonia. Let's figure out why this happens.
Cervical osteochondrosis is a degenerative disease in which the intervertebral discs in the cervical spine become thinner and destroyed, which leads to pathological changes in the spine: compression of blood vessels and nerves occurs, as well as the vertebral arteries through which blood flows to the brain. Due to compression of the arteries, blood circulation is impaired. The brain becomes vulnerable to stress; in addition, due to compression of the nerves and irritation of the nerve fibers, it begins to perceive the signals entering it worse. All these factors lead to the development of autonomic disorders. Thus, VSD in cervical osteochondrosis is a very common phenomenon. Osteochondrosis can be the cause of vegetative dystonia, and if it is treated, the symptoms of VSD will also disappear.
However, it also happens that a patient has both diseases, but osteochondrosis is not the cause of VSD, and the symptoms of dystonia are caused by some other organic disease. In this case, treating osteochondrosis will not be enough; in this case, additional identification of the causes of disorders and additional treatment of VSD is necessary.
Causes of development of osteochondrosis of the cervical spine
The exact reasons causing changes in the intervertebral discs are unclear. Most doctors believe that factors that can cause the disease are:
- Insufficient physical activity. As a result of a sedentary lifestyle, the back muscles become weak and cannot hold the spine in a straight position, which leads to deformation of the intervertebral discs.
- Incorrect posture. Often, osteochondrosis of the cervical spine develops in people who, due to their occupation, spend a lot of time in an uncomfortable position.
- Metabolic disorders resulting from a lack of vitamins and poor nutrition.
- Neck injuries.
- Some chronic infections.
VSD and cervical osteochondrosis: symptoms

With VSD and cervical osteochondrosis, symptoms indicating the disease may be as follows:
- headaches;
- rapid pulse;
- dizziness;
- drowsiness, weakness, loss of strength, fatigue;
- panic attacks (panic attacks with osteochondrosis and VSD are accompanied by extrasystole, sweating, shortness of breath, feelings of fear and anxiety, confusion, etc.);
- nausea (nausea with VSD and osteochondrosis usually occurs in the morning);
- sleep disorders.