In young children, the phenomenon of affective respiratory attacks is not so uncommon. ARP is a sudden stop in breathing, in other words, apnea. But if in adults apnea manifests itself mainly at night and has completely different reasons, then in children breath-holding can occur against the background of any emotions.
For example, many mothers have probably noticed that if a child screams and cries a lot, sometimes he can involuntarily hold his breath. The same applies to experienced fear, experienced hysteria, sudden fright, etc. Also, respiratory attacks can also appear during strong impacts, for example, during a fall.
Usually there is no cause for concern even with frequent manifestations of ARP.
Affective respiratory attacks are observed in children aged 1-3 years; after 3 years, they most often disappear due to age-related changes that occur in the body quite quickly.
If ARP continues to manifest itself in middle childhood, you should immediately contact a neurologist and psychologist. The problem may be hidden both in the respiratory tract itself and in the psychological component of the child.
Kinds
Apnea is classified according to its etiology. There are three types of syndrome:
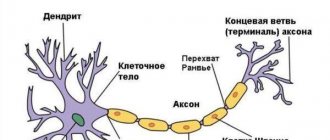
- Central. It is provoked by primary and secondary disorders of the central nervous system (less commonly, the spinal cord). Most often, this type of pathology affects children who have suffered brain injuries, have genetic diseases and were born before 34 weeks (due to underdevelopment of the nervous system).
- Obstructive. Stopping breathing in obstructive apnea syndrome is caused by obstacles to the passage of air through the nasopharynx. The cause of narrowing of the airways may be the specific anatomy of the jaw or nasal passages, neoplasia, macroglossia (large tongue size), hypertrophy of the palatal tissues, inflammation of the tonsils and adenoids, and an increase in fat in the laryngopharynx area. Obstructive syndrome is more common in adult patients.
- Mixed. Occurs in the presence of several predisposing factors. Disorders of the nervous system in this case are usually secondary and associated with pathologies and defects of internal organs or systemic infections.
The most favorable prognosis is typical for obstructive apnea. When mechanical obstacles to the passage of air are removed, breathing stops stop.
Types of paroxysms and their characteristic symptoms
Affective-respiratory paroxysms can manifest themselves in different ways. Based on this, they are classified into types.
Depending on the clinical picture and the nature of the spasm of the respiratory muscles, the following types of breath-holding attacks in children are distinguished:
- complicated by ARP. Manifested by severe hypoxia of the brain. Holding your breath lasts longer than a minute. The child experiences involuntary urination, cramps in the arms and legs;
- simple ARP. Characterized by short-term breath holding. The attack lasts no more than 20 seconds. There are no signs of hypoxia and hypercapnia;
- white ARP. Manifested by shortness of breath and fainting. It develops quite quickly. The baby's skin in the chest, neck and face turns pale;
- blue ARP. The attack begins with hysterics. The child takes a sharp and deep breath, then holds his breath. Hyperemia of the epidermal covers is replaced by their cyanosis. Muscle tone decreases, the baby becomes weak. Possible loss of consciousness.
With a simple type of ARP, breathing is restored on its own. If the course is complicated, medical attention may be required. The clinical picture of affective-respiratory paroxysms is similar to the manifestations of epilepsy.
Therefore, it is necessary to conduct a full differential examination. The doctor may prescribe a blood test, ultrasound, ECG, EEG. The diagnosis of ARP is made if no organic disorders are identified.
For ease of classification, all affective-respiratory attacks are usually divided into two types - “blue attacks” and “pale attacks” (based on the color of the skin at the time of paroxysm). But in medicine there is a more detailed classification that describes as many as four types of ARP.
- Simple - an attack is accompanied by holding your breath at the very end of exhalation. Blood circulation does not change, breathing is restored on its own.
- Blue - usually associated with emotions such as anger, anger, pain. When crying or hysterical, the child exhales quickly and forcefully, the muscles weaken, loss of consciousness may occur, and cyanosis occurs—blue discoloration of the skin. After returning to consciousness, the child wants to sleep and can sleep for a couple of hours. The electroencephalogram was not changed, everything was normal.
- Pale - paroxysm is accompanied by loss of consciousness and turns pale, but the episode of crying itself almost does not take place or the baby’s crying is insignificant. The electroencephalogram is also within normal limits, no pathological changes are recorded.
- Complicated - proceeds either according to the “pale” or “blue” scenario, but in a severe form, reminiscent of an epileptic seizure. The electroencephalogram is pathological at the time of the attack, but outside the paroxysm it remains normal for the most part.
Features of parasomnias
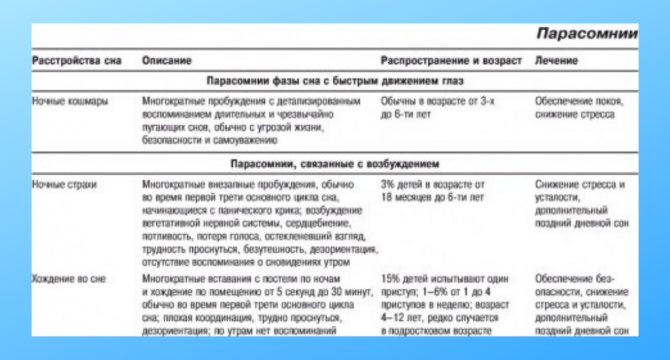
Parasomnias are expressed in a variety of behavioral attacks that occur at night.
- Night terrors. Characterized by sudden awakening, accompanied by screaming or crying.
The episodic manifestation of an attack is crowned with frequent contractions of the heart muscles, sometimes rapid breathing or stopping is noted.The disorders have an amnesic form and a tendency to self-liquidation. Treatment is usually not required unless there is persistent relapse and progression of the disorder.
- Nocturnal myoclonus. A sleep disorder characterized by increased motor activity at night. This disorder primarily includes restless legs syndrome, seizures and rhythmic movement disorders. In mild forms, the patient may not even suspect that he has abnormalities. Differential diagnosis is carried out using a polysomnographic study.
- Sleepwalking.
The disorder is characterized by uncharacteristic behavioral acts during sleep - walking without waking up, slurred conversation, and in the most rare cases, eating without waking up. The patient may sit up in bed, perform pathological motor acts, and make strange sounds. The disorder often occurs in children, but can also begin in old age. Somnambulism is a rather dangerous phenomenon. In medical practice, there have been cases of death and mechanical injuries during involuntary sleep walking. In this case, awakening the patient becomes more difficult, and the attacks themselves become amnesic. - Sleep epilepsy. Epileptic seizures occurring at night. Often accompanied by apnea and enuresis.
- Bruxism.
Loud, intense grinding of teeth that occurs during sleep. Previously, people mistakenly considered night bruxism to be a manifestation of the presence of parasitic worms, but this has nothing to do with helminthic infestation. The patient himself does not notice the manifestations of the disease, but loved ones often wake up from characteristic sounds. It is observed mainly in the second phase of sleep. It tends to progress and even destroy the integrity of the teeth. The disorder is associated not only with neurological, but also with the patient’s dental problems. - Hereditary sleep paralysis. This disorder is characterized by sudden awakening, accompanied by a sharp numbness of the limbs. Often the disease has a hereditary etiology and is difficult to treat.
- Urinary incontinence. Often observed at night in children, but may persist into adulthood. The disorder is associated with psychosomatic and nervous disorders, can be hereditary and acquired as a result of severe mechanical trauma, severe shock or psycho-emotional shock.
Are seizures dangerous?
The danger for the baby is epileptic seizures, accompanied by loss of consciousness and impacts on hard surfaces. First aid during an attack consists of the following points:
- at the beginning of an attack, the baby must be laid on a wide surface, blocking access to corners and furniture;
- turn your head to the side, preventing asphyxia (no need to hold your tongue);
- after the attack ends, check your breathing (if not, start artificial breathing).
It is necessary to record the time of the onset of the epileptic seizure and its end. If one attack ends and then a second one begins, call emergency help immediately.
The attacks themselves, which develop against the background of emotional stress, are not dangerous. However, parents need to consult a pediatric neurologist to exclude the epileptic nature of seizures.
It is imperative to consult a pediatrician, since in some cases seizures may indicate a deficiency of certain microelements and vitamins.
Nightmares
Children often have very unpleasant and vivid dreams. Nightmares usually appear during REM sleep, closer to the morning. The child screams or utters individual phrases and words when sleeping. Sometimes during a nightmare it can be very difficult to wake up.
Dreams are vivid and very disturbing. They contain scenes of chases, attacks, violence and other dangers. The next morning the child can tell in detail about what he saw in his dream. Children who suffer from nightmares appear very frightened when they wake up. They often cry while recounting the contents of their nightmares.
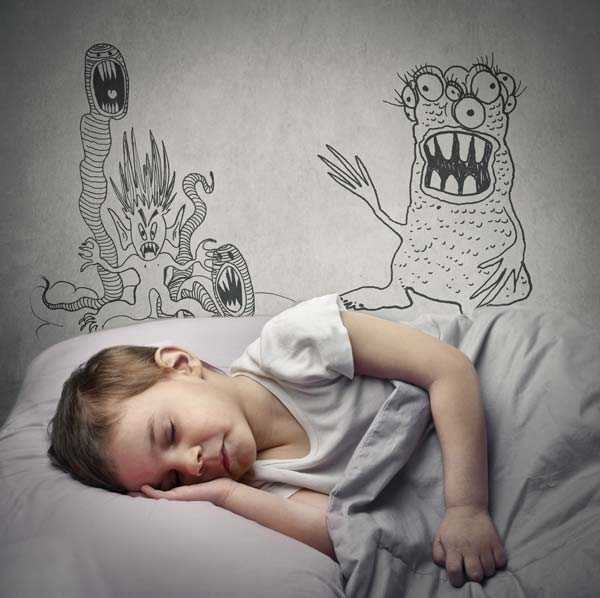
Parents can sometimes find it difficult to distinguish night terrors from nightmares. In the video below you can see the opinion of Dr. Evgeniy Olegovich Komarovsky about parasomnia in childhood. A renowned pediatrician explains in detail the difference between night terrors and unpleasant dreams.

Therapy
To successfully treat parasomnia, it is necessary to normalize your daily routine. In the second half of the day, the child should be given only light food. Sleep should be at least 9-10 hours at night, and about 1-2 hours during the day. Children with sleep disorders need high physical activity in the morning and afternoon, and quiet time in the evenings.
Using diary entries, you can track: at what time your child most often experiences sleep disturbances. Doctors recommend waking up the child 10-15 minutes before the expected episode of parasomnia, and then putting him back to sleep. This is especially necessary for nocturnal enuresis.
Behavioral correction is also used. The child needs to visit a child psychotherapist. The doctor will conduct classes with the child or teenager aimed at relieving emotional stress. At home, parents can use special evening rituals. This could be a relaxing bath, drinking tea made from soothing herbs, or slow-paced gymnastics. Such activities enhance inhibition processes in the central nervous system before bedtime.
In many cases, drug treatment for parasomnia in children is necessary. Typically, a child is prescribed plant-based sedatives:
- "Persen";
- valerian extract (tablets);
- herbal remedies with mint or motherwort.

Tranquilizers are prescribed to children extremely rarely. The body quickly gets used to such medications. For severe sleep disorders, the drugs Phenibut and Phezam are used. They are not classic tranquilizers, but are nootropic drugs with an additional sedative effect. These are prescription drugs that can only be given to a child on the recommendation of a doctor.
Physiotherapeutic methods for treating parasomnia in children are also used: electric sleep, massage, baths with decoctions of sedative herbs. It is especially useful to carry out such procedures in the afternoon.
Symptoms
Each affective-respiratory paroxysm is necessarily preceded by some strong emotion. Just like that, being in a familiar and calm state, the child does not fall into an attack. Each attack develops in strict accordance with the order of changing stages; each attack is exactly similar to the previous one.
Trying to cope with the emotion, the baby begins to breathe unevenly, cry, and then suddenly becomes silent, freezes and remains in this state for some time, his mouth is usually open. Parents may hear wheezing and clicking sounds. The baby cannot control holding his breath and interrupt it of his own free will. Apnea does not obey the will of the child.
With a simple attack, breathing is restored in about 15 seconds. The baby looks normal and has no other symptoms. With other forms of ARP, the baby may fall, lose consciousness, and his skin and mucous membranes become pale or bluish. During an attack, the pulse is almost not palpable or it is very weak.
The body may arch (Dr. Komarovsky calls this a “hysterical bridge”) if the muscles are very tense, or go limp, like a rag doll, if they are relaxed. Convulsions, if present, most often manifest themselves in the form of involuntary twitching, for example, of the limbs.
Recovery always begins with normalization of breathing. Then the skin and mucous membranes acquire a normal color, and the muscles come into order. Recovery from a normal attack is quick, the child may immediately ask for food or start playing. The longer the attack lasts, the more time it takes to fully recover. When a complicated attack occurs, the child continues to quietly cry and whine for some time, and with this he usually falls asleep for a couple of hours.
An episode of a “blue” affective-respiratory attack usually begins with uncontrollable crying for several seconds (no more than 10-15), after which a sudden stop in breathing occurs on exhalation, which is characterized by the following symptoms:
- the mouth is open, there is no inhalation;
- crying stops;
- cyanosis rapidly increases;
- within a few seconds (up to several minutes, usually no more than 0.5-1 minute) there is no breathing (apnea develops).
If apnea lasts more than 1 minute, loss of consciousness, “limpness”, followed by tension in the muscles of the body, stretching or arching are possible. If oxygen access is not restored, the phase of clonic convulsions begins (twitching of the child’s limbs and torso).
Prolonged holding of breath and, as a consequence, oxygen intake provokes hypercapnia (excessive accumulation of carbon dioxide in the blood), which causes a reflex relief of spasm of the laryngeal muscles: the child takes a breath and begins to breathe, regaining consciousness.
After such a prolonged attack with tonic or clonic convulsions, deep sleep usually occurs for 1-2 hours.
Although holding their breath may seem deliberate, children do not do it on purpose; the reflex occurs when a crying child forcefully exhales air from the lungs while crying.
“Pale” attacks are most often provoked by fear, a sudden painful stimulus (injection, hitting the head, falling, etc.) or a combination of these factors. The child may cry, but more often he simply calms down, loses consciousness and suddenly turns pale. Characterized by weakness and heavy sweating, the pulse cannot be felt for several seconds. In the most severe episodes, clonic contractions of the muscles of the limbs and involuntary urination are possible.
ICD code
Most types of parasomnia according to ICD-10 are included in the group of diseases grouped under the code F51 (“Sleep disorders of non-organic etiology”). Thus, sleep disorders are classified that are not a symptom of any disease, but exist independently.
Here are the codes for the most common types of parasomnia in childhood:
- somnambulism - F51.3;
- night terrors - F51.4;
- nightmares - F.51.5;
- confusion after waking up - F51.8.
You may be interested in: I want to sleep, but I can’t sleep. Possible causes of insomnia, treatment options, reviews
The exceptions are bruxism and nocturnal enuresis. Grinding of teeth during sleep is considered a somatoform disorder. This is the name for disorders of psychogenic etiology that occur with somatic manifestations. Bruxism code is F45.8.
As for bedwetting, ICD-10 defines this disorder as an emotional disorder. The code for enuresis of inorganic origin is F98.0.
What does it look like?
Pediatricians conditionally divide affective-respiratory syndrome into 4 types. The classification is as follows:
- A simple option, or holding your breath at the end of the exhalation. Most often develops after a child’s dissatisfaction or trauma. Breathing is restored on its own, and blood oxygen saturation does not decrease.
- The “blue” option, which most often occurs after a pain reaction. After crying, a forced exhalation occurs, the mouth is open, the child does not make any sounds - “rolled”. Rolling of the eyes and cessation of breathing are visible. The baby first turns bright red, then turns blue, then goes limp, and sometimes loses consciousness. Some regain consciousness after regaining their breathing, while others immediately fall asleep for an hour or two. If you record an EEG (encephalography) during an attack, there are no changes in it.
- “White” type, in which the child almost does not cry, but turns sharply pale and immediately loses consciousness. Then comes sleep, after which there are no consequences. No seizure focus is detected on the EEG.
- Complicated - begins as one of the previous ones, but then paroxysms are added, similar to an epileptic attack, which can even be accompanied by urinary incontinence. However, subsequent examination does not reveal any changes. This condition can pose a danger to all tissues due to severe oxygen starvation, or brain hypoxia.
Such convulsions do not pose a threat to life, but consultation with a neurologist is required in order to distinguish them from more severe cases. Breathing stops for a period of time from several seconds to 7 minutes, and it is very difficult for parents to maintain composure. The average time to stop breathing is 60 seconds.
Symptoms and methods of eliminating parasomnia in children
Parasomnia includes a number of sleep dysfunctions. These include enuresis, sleep paralysis, nightmares, and somnambulism.
The nature of the origin of these deviations is associated with dissociative disorders. The diagnosis is made after polysomnography using video monitoring.
Parasomnia is more common in children than in adults. This is explained by their fragile nervous system.
What kind of disorder is this
Parasomnia is a condition in which there is a violation of autonomic functions and coordination of movements. It manifests itself at night, when a person loses control over himself.
Parasomnia in adults often develops against the background of serious pathologies. Over time, the problem tends to progress under the influence of age-related changes. In a child it appears as an independent disease.
In some cases, the problem is resolved without intervention, after stabilization of the nervous system.
Symptoms
Clinical manifestations of the pathological process relate to the quality of sleep. During the night, the child may wake up several times due to irritating factors. The awakening process is accompanied by twitching and convulsions. The main symptoms of parasomnia include:
- Nightmares. The baby wakes up in the middle of the night as a result of a strong fright. This is accompanied by a jump in blood pressure, rapid heartbeat and shortness of breath.
- Sleep paralysis. This condition is characterized by incomplete recovery from sleep. The body is completely stiff, but the eyes open and close. At the same time, the child continues to see the dream, mistaking it for reality.
- Sleepy enuresis. Its appearance is associated with disorders of the nervous system. When the bladder is full, the brain does not receive a signal that it needs to be emptied. The baby wakes up due to discomfort. Sometimes the disease develops against the background of anemia, diabetes mellitus or pathologies of the genitourinary system.
- Snore. It is provoked by respiratory dysfunction or uncomfortable body position.
- Epilepsy attacks. They arise as a result of serious disorders of the nervous system. Characterized by cyclic jerks, atypical muscle contractions and arching of the body.
- Sleepwalking. A person suffering from parasomnia is able to move and talk in their sleep. His movements and speech have no logical basis. Manifestations of sleepwalking include vivid displays of emotions, speech activity, walking around the apartment and moaning.
The main feature of the symptoms of parasomnia is the lack of awareness of what is happening. In the morning the child does not remember what happened. Pathology can manifest itself both on a regular basis and occasionally.
Complications
The danger of the disease lies in the increased likelihood of developing sleep apnea. It is accompanied by respiratory arrest, which in some cases leads to death.
When sleepwalking, moving around the apartment, the child can get hurt. The most common types of injuries include falling from a height and hitting furniture.
Waking up from pain provokes additional emotional stress.
Parasomnia in childhood can affect the psychological state of the child during the daytime. Due to lack of sleep, he becomes irritable and his performance decreases. This causes memory problems.
Diagnostics
To determine the cause of the violations, consultations with pediatric specialists are required. First of all, parents should contact a somnologist or neurologist. The next step will be polysomnography, which will allow us to determine failures during the transition from one phase to another. During the procedure, the nature of the respiratory system and heart is recorded.
If necessary, MRI, CT and ultrasound examination of blood vessels are prescribed.
What's happening?
Since young children do not yet know how to evaluate and perceive their own emotions, do not know how to cope with them, or control their manifestations, very vivid affective reactions develop. A strong emotion gives rise to convulsive contraction of muscles in the larynx area.
What happens next is reminiscent of laryngospasm - the baby is additionally frightened by the new sensation of being unable to take the usual breath due to the narrowing of the glottis, the new fear contributes to an even tighter closure.
At the same time, cramps can develop; they are involuntary and are also associated with muscle emotional tension. The attack lasts no more than a minute, most often from 15 to 25 seconds, then the muscles begin to relax and the child begins to breathe normally.
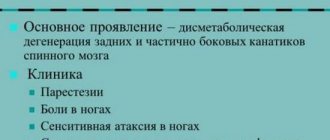
Due to the child’s underdeveloped respiratory and muscular systems, when he exhales too much, his lungs may be deprived of oxygen, and a spasm of the larynx will not allow him to take a breath in a timely manner. The likelihood of laryngeal spasm increases with a deficiency of calcium and vitamin D in the body, as well as with low hemoglobin in the child’s blood.
Since the need for calcium in a child is quite high - it is very actively consumed during the construction of bone and dental tissue, to one degree or another, deficiency of this mineral occurs quite often.
Doctors divide attacks according to the color of the skin changes into “pale” and “blue”:
- Pale paroxysm occurs after a child falls, a sudden blow, an injection, or severe fright, while the child may just start crying, but more often breathing stops even before screaming. The child cannot breathe, his mouth is open, but there is no crying. The heartbeat is delayed and the pulse is almost not palpable, the child’s skin turns pale, and in future life children prone to pale ARP are more likely to faint.
- A blue attack is usually a reaction to an emotional storm, dissatisfaction and anger that the child cannot cope with.
Such a reaction can develop when a child refuses to satisfy a momentary desire - to buy a toy, give daddy’s phone number, or a chocolate bar. Starting to cry, the child increases the degree of emotional stress; at one point he cannot breathe in air due to a spasm of the larynx, and the skin acquires a bluish tint. In this state, the child may lose consciousness, a loss of muscle tone is possible - he “goes limp”, or vice versa - he arches from their overexertion.

Burda Media
Treatment Options
Treatment of parasomnia is carried out in two directions: psychotherapy and drug treatment. Most often, medications are prescribed for an indefinite period, sometimes for life. Sleeping pills, sedatives, anxiolytics, antidepressants, and benzodiazepines are used. In some cases, phenobarbital-based drugs are prescribed, but they cause dependence and are therefore not recommended for long-term use.
For mild sleep phenomena, traditional medicine can be used, for example, tinctures and tea based on valerian, mint, etc. Doctors prescribe bromine-based sedatives. It has a beneficial effect on the functioning of the nervous system, therefore it actively works against parasomnias of neurological and somatic etiology.
Psychotherapy and cognitive behavioral treatment play an equally important role as medications. Psychotherapeutic treatment works well on patients whose sleep phenomena arise due to psychological trauma, etc. Violations lead to the fact that the patient is constantly lethargic, so he tries to lie in bed more and moves less. This leads to even more harm because it triggers other sleep problems, such as insomnia. In this case, cognitive behavioral therapy is recommended. Patients are advised to keep sleep diaries and establish a daily routine, especially in the evening and at night.
For parasomnia in adults, doctors recommend avoiding stress, nervous work, etc. not only during the treatment period, but also after. This will help reduce symptoms.
What should you do during attacks?
First of all, parents should not panic. The emotional state of others is always transmitted to the baby, and if confusion is fueled with fear, it will only get worse. It would be a good idea to hold your breath for a while. This will make you feel that nothing bad will happen to your baby due to a temporary delay in respiratory functions. You can also blow on your baby's nose, pat him on the cheeks and tickle him. Any such action will help the child come to his senses much faster in order to breathe again.
During prolonged attacks, especially those accompanied by convulsions, you should put the baby on a flat bed, and then turn his head to the side. This will prevent him from choking on vomit if he vomits. It is recommended to splash cold water on the baby, then wipe his face and gently tickle him.

It should be noted that when mothers and fathers tear out their hair during attacks, they further aggravate the condition of the children. After attacks, the baby should be allowed to rest. You can't wake him up if he suddenly falls asleep. It is important to remain calm after attacks and speak quietly. The main thing is not to make noise. In the presence of a nervous environment, attacks may recur.
For any attacks accompanied by convulsions, you should definitely consult a neurologist. Only a doctor can distinguish an affective-respiratory attack from epilepsy or other neurological disorders. Thus, you need to arrange a consultation with your doctor if something like this happens for the first time. The doctor must determine whether the child has a disease or is it an affective reaction. In the event that an attack occurs not for the first time, and there is no illness as such, measures must be taken regarding the upbringing of the child.
When something like this happens to a child for the first time, you need to call a doctor. This is especially necessary against the background of seizures. The pediatrician will be able to assess the severity of the condition and tell you whether the child needs hospitalization. After all, parents are not always able to fully monitor their baby. In addition, this is how the consequences of brain injuries, various poisonings and all kinds of acute diseases manifest themselves.
What should parents do during an affective-respiratory attack? Komarovsky advises the following.
Which doctor should I contact?
If you experience symptoms of a sleep disorder, you should make an appointment with a therapist. The doctor will interview the patient, conduct an examination and refer him to specialists.
To establish a diagnosis, a consultation with a neurologist is required. At the appointment, you need to tell in detail how long the episodes of sleepwalking last, describe the usual rhythm of the child’s life, without hiding possible emotional overloads and conflict situations
Before visiting, it is important to find out the situation in the kindergarten or school and provide a complete list of medications that the child has taken recently.
To diagnose violations, the following is carried out:
- electroencephalography;
- Magnetic resonance imaging;
- Ultrasound of cerebral vessels.
It is necessary to take blood and urine tests, and take an x-ray of the spine. After the results of the examination, treatment with a psychiatrist or somnologist - a doctor specializing in sleep disorders - is sometimes recommended. The doctor may prescribe polysomnography, a procedure that identifies the causes of disorders.
Is this dangerous for the child?
Affective-respiratory paroxysms in themselves do not pose a danger to the child’s life. But if attacks occur frequently, this can cause a disruption in social adaptation.
ARP also increases the likelihood of a decrease in the level of mental and intellectual development of the child. A child with breath-holding spells may have poor performance in school.
Sometimes somatic disorders are observed: hypoxia of brain structures, decreased activity of alveoli in lung tissue, increased aggregation of red blood cells. It is imperative to consult with a pediatrician, cardiologist, or neurologist.
Sometimes attacks of breath holding are caused by a deficiency of certain vitamins and microelements in the child’s body. It is important to start treatment of affective-respiratory paroxysms on time. Parents should do everything necessary to prevent the occurrence of such attacks.
In most cases, affective-respiratory paroxysms do not negatively affect the life and health of the child. Children outgrow these attacks. Much depends on the attitude of the parents.
Only a qualified specialist can confirm a preliminary diagnosis of epilepsy based on a special study - electroencephalography. This study allows us to identify pathological activity in brain structures.
The difficulty of diagnosis lies in the fact that it is difficult to keep a baby under 1 year of age in one place. In addition, a specialist can obtain the most accurate results during daytime or night sleep. Diagnostic measures are carried out not only before diagnosis, but also during therapy to monitor the healing process.
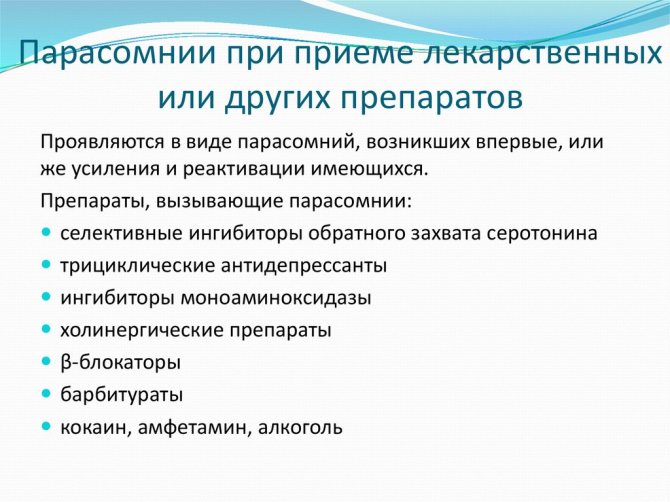
Why does parasomnia develop?
The causes of parasomnia are closely related to functional pathologies of the nervous system. It is logical to assume that the nature of sleep disorders may be psychosomatic, i.e. “bad sleep” occurs “due to nervousness.” This is supported by scientific evidence. Parasomnia often develops as a result of a stressful situation. It is not for nothing that they say about a person in difficult circumstances: “He sleeps poorly.” Parasomnia is one of the characteristic symptoms of depression or neurosis. In addition, diseases of the heart and blood vessels, digestive organs, and nervous system can lead to sleep disorders. Pathology can also manifest itself as a side effect of potent medications.
Drinking coffee and heavy food can also disrupt the process of falling asleep and staying asleep. People with alcoholism or drug addiction also experience functional disorders of varying severity
It is important to understand that the development of parasomnia is somewhat influenced by a hereditary factor, but its significance should not be exaggerated
Factors contributing to sleep disturbance:
- taking antidepressants;
- nervous excitement, excitement, worries;
- heartburn;
- abuse of caffeine, alcohol, drugs (some studies classify all these substances as narcotic);
- increased motor activity of the limbs;
- stress;
- chronic lack of sleep;
- improper diet and regimen;
- background diseases of internal organs: heart and blood vessels, brain, nervous system, stomach and intestines, etc.
Remember that only a doctor can identify the causes of pathology, stop its manifestations and cure diseases. This will be discussed below.

In adults
Parasomnia in an adult is more often of a pathological nature than in a child. If the disorder is not associated with a mental condition, it may be a manifestation of an underlying disease
It is important to diagnose it and begin treatment in a timely manner. The older the patient, the more the disease can progress due to the age-related characteristics of the body.
Nightmares with panic fear upon awakening can occur in people at any age, but night terrors (when a person continues to sleep) are observed much less frequently in adults than in children. In this case, adults experience so-called sleep paralysis - a short-term lack of movement in the limbs, accompanied by fear, sometimes fear of death. Restless legs syndrome is also typical for adults - a feeling of “pins and needles” and cramps, tingling that interferes with normal sleep.

In children
Parasomnia is observed much more often in children than in adults. Its most common manifestation (especially in preschool age) is enuresis. Due to the immaturity of the nervous system, the child is not always able to control urination during sleep. Enuresis is directly related to hyperactivity in children.
At the age of 4-8 years, children may develop sleepwalking, a type of awakening disorder. The range of manifestations of sleepwalking is wide: from simply sitting on the bed to attempts to leave the house, after which the child falls asleep, and the next morning does not remember the events that happened to him. Night terror attacks occur in children aged 2-4 years. Children wake up screaming or crying for a short time, but after further falling asleep and waking up they have no memory of them.
Unlike fears, with nightmares the child wakes up and is able to answer the question about the cause of his fear. As a rule, this is some kind of dream that frightens him. Sleepy intoxication, or confused awakening, is quite common in children under 5 years of age - difficult awakening, characterized by disorientation. Children under 10 years of age are much more likely than adolescents and adults to experience sleep talking, which is usually not a dangerous phenomenon unless accompanied by other pathologies. Most types of parasomnia in children resolve by adolescence.
Affective-respiratory attacks in children: causes, symptoms and treatment
These are attacks in which, after exposure to an emotional or physical stimulus that is excessive for the nervous system, the child holds his breath, short-term apnea (stopping breathing) occurs, and sometimes convulsions and loss of consciousness occur.
Such attacks usually pass without consequences, but require observation by a neurologist and cardiologist.
Affective-respiratory attacks occur in children aged 6 months to one and a half years. Sometimes they appear in a 2-3 year old child.
Newborns do not suffer, up to 6 months of age there are practically no attacks due to the pronounced immaturity of the nervous system, and with age the child “outgrows” them. The frequency of attacks is up to 5% of all children.
Such a child requires special attention when raising, because children's seizures are equivalent to hysterical fits in adults.
What is ARP
Affective-respiratory attacks, from the point of view of doctors, are the earliest manifestation of fainting or hysterical attacks.
To better understand what exactly is happening to your baby, it’s worth first deciphering the name of the concept we are considering.
The word “affect” denotes a very strong uncontrollable emotion, and everything related to the concept of “respiratory” is associated with the respiratory organs.
This means that ARP is a violation of the breathing process, somehow combined with the emotional sphere of the child. And, as researchers have proven, they are more susceptible to excitable, spoiled and capricious children.
The first affective-respiratory attacks begin, as a rule, after the baby is six months old and last until about 4-6 years.
By the way, I would like to draw the attention of parents that holding their breath in children occurs involuntarily and not on purpose, although from the outside it looks as if the baby is pretending. The described paroxysm is rather a manifestation of a pathological reflex that is triggered during crying, at the moment when the baby exhales most of the air from the lungs at once.
Apnea in infants
Apnea is a sudden stop in breathing that is not associated with emotional stress. Infants and newborns are susceptible to the disease. In adults, apnea may occur during severe skin irritation.
A particular danger is the sudden cessation of breathing during sleep apnea. In this case, breathing stops for more than 25 seconds, which can have negative consequences for the child. The disorder should be treated, otherwise a number of neurological pathologies may develop, including disruption of the baby’s development.
Sudden breathing problems during sleep are a cause for concern. In infants, the disorder may develop for the following reasons:
- trauma during childbirth;
- congenital anomalies of the structure of the nose;
- swelling of the mucous membrane of the nasopharynx due to colds and viral diseases;
- severe obesity.
At older ages, such disorders are rarely observed. Stopping breathing in children over 8 months of age is directly related to the emotional state of the child and, according to many experts, is the first harbinger of neurosis and hysteria in the future.
What does it look like to hold your breath in a crying baby?
Affective-respiratory paroxysm most often occurs when the child is crying a lot. So to speak, at the peak of his indignation at the current situation.
During such a noisy display of emotions, the child may suddenly suddenly become quiet and, opening his mouth, not utter a sound. In this case, breathing may stop for 30-45 seconds, the baby’s face becomes pale or blue, depending on the circumstances, and at this time the parents themselves are ready to lose consciousness.
By the way, it is how the child looks when he cries that determines what type of seizure you observe. They are conventionally divided into the so-called “pale” and “blue”.
ARP types: white and blue version
Many experts divide the type of skin color at the time of an attack of ARP into two groups - white (pale) and blue (cyanotic):
- For the group of pale ARP, triggering factors for the development of an attack can be reactions to pain from falls and bruises, injections, and cuts. If you try to count your pulse during an attack of apnea (lack of breathing), it will completely disappear for a few seconds. In terms of their mechanism of development, white (pale) ARPs can be very similar to fainting states. As these children grow older, such hysterical attacks turn into fainting states.
- More often attacks of ARP occur as cyanosis ; they can manifest themselves with pronounced discontent and hysteria, when expressing one’s own character, anger or unfulfilled desires. Children can fall into this type of ARP when their parents refuse to fulfill their demands, if they do not get their way, and attract attention by screaming, hysterics and crying.
Usually it all starts with intermittent and deep breathing, typical of prolonged crying, and then when inhaling, breathing stops completely for a few seconds, but then the children’s condition returns to normal.
Externally, such attacks of cyanotic ARP can imitate laryngospasm (twitch of the laryngeal muscles).
- In some cases, the attack may be prolonged, and muscle tone may suffer, which weakens due to hypoxia. Then the baby in the arms of adults can go limp, like a “rag doll.”
- A second variant of a protracted attack is also possible - a tonic, close to convulsive, muscle contraction, which is why the baby can bend in an arc.
Types of breath-holding seizures
“Pale” affective-respiratory attacks in a child occur as a painful reaction at the time of a fall, bruise, or injection, while the baby sometimes does not even have time to cry. At this time, the child may not have a palpable pulse, and this type of attack is similar to fainting in adults. By the way, often this condition later develops into fainting.
And “blue” attacks are the “highest point” of the expression of anger, rage and discontent. In children, paroxysms develop in most cases of this type. If it is impossible to get what is required or achieve what is desired, the child begins to scream and cry. As he inhales, his intermittent but deep breathing stops, and a slight blueness appears on his face.
Most often, the condition normalizes on its own, but sometimes the baby may experience tonic muscle tension or, conversely, a decrease in their tone. Outwardly, this manifests itself in the fact that the child suddenly tenses up and arches or goes limp, which, by the way, also does not last long and goes away on its own.
Causes and risk factors
There is no consensus on the causes of this condition, although the main theory is the psychogenic onset of affective-respiratory attacks.
There is a point of view that attacks are usually observed in emotionally mobile, irritable, capricious children and are some kind of hysterical attacks. In response to painful or negative psycho-emotional effects, the child develops corresponding symptoms.
Some authors note the importance of the problem of interpersonal relationships within families or the phenomena of overprotection. Research conducted in 2008 showed that children prone to affective-respiratory attacks have higher levels of emotionality, activity, emotional intensity and distractibility.
Despite the obvious influence of the psychological component, most experts still believe that this phenomenon occurs not only in emotionally complex children; The following factors play an important role:
- hereditary predisposition (25–30% of children have a family history of affective-respiratory attacks, when at least one of the parents suffered from them;
- cardiovascular pathology;
- deficiency of iron, necessary for the metabolism of catecholamines and adequate transmission of nerve impulses;
- epileptic nature of the condition.
Emotional factors that can trigger an attack:
- irritation;
- discontent;
- feeling of dissatisfaction;
- fear, fright.
Seizures develop more often if the child is overtired or overexcited, hungry or in an unusual environment.
Are seizures dangerous for a child?
Concerned parents should be immediately warned that the described paroxysms do not pose any serious danger to the health and life of a crying baby.
You should call an ambulance only if the child’s breathing has stopped for more than a minute. And you should consult a doctor in case of frequent (more than once a week) attacks, as well as in cases when they change: they begin differently, end differently, or if unusual symptoms are detected at the time of the paroxysm.
If you observe affective-respiratory attacks in a child, the main thing is not to be nervous, try to help him restore his breathing by lightly patting his cheeks, blowing in his face, sprinkling some water on him or tickling his body. This is usually successful, and the baby begins to breathe normally. After an attack, hug the baby, reassure her and continue to do your job without showing concern.
What to do with apnea
Sleep apnea in a newborn poses a serious health risk. If parents notice symptoms of sudden respiratory arrest in an infant, they should immediately call emergency medical help.
First of all, you need to wake up the baby. Parents should then lightly massage the limbs and earlobes to restore normal blood circulation.
If, 20 seconds after stopping breathing, the child is still unable to take a breath, several exhalations of artificial respiration should be carefully performed.
It is imperative to remember that the baby’s lungs are small, and exhalations during artificial respiration should be very small.
In addition, you need to make sure that the cause of respiratory arrest is not foreign objects in the baby’s larynx. To do this, you should pick up the baby, carefully tilt his head back and carefully examine his throat.
Apnea, unlike ARP, is a very dangerous disorder that requires careful diagnosis by a neurologist and treatment. When faced with a sudden stop in breathing during sleep, you must urgently call an ambulance and then undergo all the necessary examinations.
Source: https://neuro-orto.ru/bolezni/affektivno-respiratornye-pristupy.html
Causes of the disease
Scientists have identified a number of negative factors that are common causes of sleep disturbances. The main ones include:
- Prolonged depression;
- Severe or prolonged stress;
- Emotional shock (usually associated with the death of a loved one);
- Problems with hormone balance;
- Detection of thyroid dysfunction;
- Parkinson's disease;
- Poor nutrition;
- Having bad habits;
- A side effect from long-term use of certain categories of medications;
- Chronic pathologies of the respiratory tract;
- Problems in the functioning of the gastrointestinal tract;
- Fever.
A separate group of patients consists of pregnant women and young children. In the first case, the disease manifests itself against the background of general changes in the body and natural sleep disturbances. As a rule, such parasomnia goes away on its own after delivery.
In the case of children, the disease is caused by the formation of the nervous system, accompanied by hyperexcitability, impressionability and a special reaction to various external stimuli. Immediate treatment is required only when sleep disturbances occur very often, preventing the baby from developing normally.
It is obvious that the occurrence of parasomnia is influenced by psychological, physiological and hereditary factors. To treat a disease, it is necessary to establish the cause and act on it.
How to distinguish epilepsy in a newborn from physiological changes
A child under one year of age is seriously different in behavior from older children - 2-3 years old. He often makes unconscious movements with his arms and legs. And distinguishing normal development from an epileptic seizure can be difficult. But there are universal signs indicating the onset of a seizure.
| Main features | Additional signs |
| Sudden immobilization - the child seems to freeze. | Problems with breathing, until it stops. |
| The gaze is focused in one direction. | Temperature increase |
| The eyes begin to roll behind the upper eyelids. | Frequent urination and defecation. |
| There is no reaction to stimuli - light, sound, movement. | Convulsions |
| Loss of consciousness |
After the attack, the child’s normal functioning resumes.
Causes
The following conditions can cause sleep apnea:
- injuries and tissue damage to the brain and spinal cord;
- primary failure of the respiratory center;
- structural features of the bones of the skull and jaw (short neck, small lower jaw, narrow nasal passages);
- hypertrophy of the soft tissues of the palate (increase in the size of the tonsils, palatine tongue);
- underdevelopment of the laryngeal muscles;
- disorders of the upper respiratory tract caused by inflammatory and tumor processes;
- obesity;
- diseases of the endocrine and cardiovascular systems;
- metabolic disorders (primarily glucose, calcium, magnesium and amino acids);
- systemic infections (meningitis, septicemia, pneumonia);
- autoimmune pathologies;
- overheating, hypothermia.
Those at risk for the syndrome include:
- people with a hereditary predisposition to sleep apnea;
- premature babies;
- children with congenital abnormalities that are accompanied by changes in the nervous system and maxillofacial anatomy (Down syndrome, “cleft lip”);
- infants suffering from gastrointestinal diseases and reflux;
- crumbs that appeared during complicated childbirth, triggered by injury or prolonged hypoxia.
Treatment
If parasomnias impair quality of life, it is recommended to initiate therapy. Methods depend on developing symptoms and the results of the diagnosis performed.
Drug therapy
It is carried out using the following medicines:
- Benzodiazepines (Gidazepam, Clobazam, Midazolam). They produce a sedative and anticonvulsant effect, which has a positive effect on the quality of sleep.
- Antidepressants (Paroxetine, Sertraline, Escitalopram). They allow you to normalize a person’s psycho-emotional state, which has a positive effect on his rest.
- Sedatives (valerian, motherwort) help relieve anxiety.
- Tranquilizers (Valium, Mebikar, Spitomin). Used in extreme cases when other means are ineffective.
Physiotherapy
Physiotherapy helps many patients cope with this problem. Depending on the diagnosis, the patient is prescribed acupuncture, photo or magnetic therapy, and massage.
Psychotherapy
If sleep pathologies are caused by psychological problems, treatment with a psychotherapist is indicated. The doctor helps the patient understand himself and find solutions to the current situation. Sometimes they resort to hypnosis.
Traditional treatment
To improve the quality of sleep and get rid of parasomnias, you can use the following folk remedies:
- Mint tea. Pour a tablespoon of herb into 240 ml of boiling water and wait 15 minutes. The finished drink is drunk before bedtime.
- Linden and lemon balm tea. Each herbal component is used in the amount of a teaspoon. The resulting mixture is poured into 210 ml of boiling water, after cooling, taken instead of tea, before bed.
- Infusion of hop cones. A tablespoon of plant material is poured with 220 ml of boiling water. The resulting drink is taken before bedtime.
Sleepwalking
Sleepwalking is the strangest and most complex form of parasomnia; it is not for nothing that it has acquired so many myths. Usually somnambulism occurs in the deep sleep phase in the first half of the night, but sometimes it also happens during REM sleep in the morning.
A sleeping person sits up in bed, mumbles about something, walks around the room or goes outside. In rare cases, even eating is possible. During an episode of sleepwalking, a person can be either excited or calm.
The length and complexity of the attack may also vary. The events occurring at this time are amnesic, that is, the person in the morning does not remember what happened to him at night.
Sleepwalking is a fairly common phenomenon among children. Statistics say that about 17% of 8-13 year olds are susceptible to somnambulism.
Adults also suffer from it, and in some of them it begins in old age. It has been established that sleepwalking can be inherited.
There is still no cure for sleepwalking. The only thing that loved ones of a person prone to sleepwalking should do is to take care of his safety, since while in a state of sleep, he is not able to control his behavior.
For example, it may fall from a height and cut itself on glass. Medical practice knows cases of serious injuries and even death of people during sleepwalking.
From the room in which the somnambulist sleeps, you need to remove all dangerous, breakable objects, close the doors and windows at night, and eliminate access to the stairs.
Contrary to the popular belief that a person who is in a state of somnambulism cannot be woken up so as not to harm his psyche, in reality this is not the case. The only thing that awakening in such a case can lead to is the natural embarrassment of a person awakened in an unusual situation.
That is why it is recommended not to wake him up, but to carefully bring him to bed and put him to sleep
Possible dangers
Of course, the main question that interests all parents who are faced with this phenomenon is whether a respiratory attack is dangerous for the child’s health.
Doctors loudly claim that both pale and blue attacks do not pose any danger to the body. However, decreased muscle tone and lack of oxygen entering the brain can affect the body if the frequency of attacks is very high.
Medical experts also say that you may need to call a doctor if your child holds their breath for more than one minute. But the question remains unclear about what to do then for parents who experience and see this danger.
Therefore, the best recommendation in this case may be the only advice - parents, having noticed at least once the manifestation of an affective respiratory attack in their child, should not postpone a visit to a neurologist. Firstly, it is the doctor’s words about the safety of attacks that can reassure and reassure mom and dad.
Secondly, if necessary, the doctor can prescribe certain effective treatment, which consists of taking certain medications. The doctor can also give instructions to parents about paying more attention to the child, his proper upbringing specifically in terms of controlling his emotions, and it doesn’t matter whether they are positive or negative.
In other words, it is not the child who will fight ARP, but his parents, who are obliged to create a positive atmosphere around him, not to indulge his weaknesses and desires in order to force him to remain silent.
We must remember that a child is also a person, even if he is still small, and therefore he must learn to endure and admit his mistakes.
Infliction of physical pain, constant guardianship, and then attempts to make amends by buying gifts fundamentally harm the child, shaping his future character.

Treatment of parasomnias in children
Parasomnias often disappear on their own as the child grows and the central nervous system matures. If the symptoms of the disorder do not significantly affect the quality of life, therapy is not required. If the clinical picture is severe, treatment is carried out by a neurologist, psychiatrist, or psychologist. Methods used:
- Normalization of the daily routine. To prevent subsequent episodes of disturbed sleep, it is necessary to exclude provoking factors: strictly adhere to the regime, allocate 9-10 hours for sleep at night and 1-3 hours during the day, eat light food in the afternoon, avoid the influence of stress factors.
- Behavioral therapy. The programmed wake-up method is used. Parents, using observation diary data, wake the child 15 minutes before the parasomnia episode, and then put them back to sleep. This method also includes evening rituals that help the child relax, triggering processes of central nervous system inhibition: herbal teas, special gymnastics, a warm bath.
- Drug treatment. Pharmacotherapy is aimed at accelerating the maturation of mechanisms that regulate sleep cycles, as well as increasing inhibition. Nootropics, herbal sedatives, and, less commonly, tranquilizers are prescribed.
- Physiotherapy. Treatment methods are selected individually. Massage, electrosleep, herbal baths, exercise therapy, and swimming can be used.
What are nightmares in children?
Nightmares in children cannot be called the imagination of a child or the speculation of overly caring parents. This is a physiological phenomenon of a hallucinatory nature, when the child’s overexcited brain cannot go into the inhibition stage. As a result, increased mental excitability occurs in the first stage of deep sleep.
Approximately 1/3 of children suffering from nightmares exhibit increased motor activity. They may kick their legs and wave their arms in a panic, try to get up and run, without leaving the deep stage of sleep. Subsequently, they may develop sleepwalking or parasomnia.
This condition is characterized by the baby’s desire to move around and are in a state of sleep. At the same time, his eyes may be wide open. But the pupils are usually dilated and do not respond to movements in front of them. It is not easy to wake up a child; he does not recognize the people around him, does not orient himself in space, and does not understand where he is.
Primary night terrors in children usually last 15-20 minutes. At this time, the pulse quickens, blood pressure rises, and sweating increases. The child breathes quickly and abruptly. Rapid eye movements occur. Then the stage of arousal passes into deep sleep. Uncomplicated childhood nightmares do not repeat twice during the night. After waking up, the baby may not remember what happened to him at night.
Children's nightmares are not hereditary diseases and are not caused by genetic factors. They can be triggered by a mismatch of physical and mental development, the presence of severe functional diseases of some organs and systems. Sometimes nightmares precede the development of mental illness.
Manifestations of nightmares occur in children of all ages. However, the largest number of cases is recorded in the age group from 3 to 5 years. Boys suffer more often. Complete relief from night terrors occurs at the age of 12 years.
Prevention and causes (ARP) of an affective-respiratory attack in a child, advice to parents
These are attacks in which, after exposure to an emotional or physical stimulus that is excessive for the nervous system, the child holds his breath, short-term apnea (stopping breathing) occurs, and sometimes convulsions and loss of consciousness occur. Such attacks usually pass without consequences, but require observation by a neurologist and cardiologist.
Affective-respiratory attacks occur in children aged 6 months to one and a half years. Sometimes they appear in a 2-3 year old child.
Newborns do not suffer, up to 6 months of age there are practically no attacks due to the pronounced immaturity of the nervous system, and with age the child “outgrows” them. The frequency of attacks is up to 5% of all children.
Such a child requires special attention when raising, because children's seizures are equivalent to hysterical fits in adults.
Why do seizures occur?
The leading causes are hereditary. There are children who are excitable from birth, and there are character traits of their parents that involuntarily provoke these attacks. The parents of such children also experienced bouts of “rolling down” in childhood . In children, affective-respiratory paroxysms can occur in response to the following situations and stimuli:
- adults ignoring the child’s demands;
- lack of parental attention;
- fright;
- excitation;
- fatigue;
- stress;
- overload with impressions;
- falls;
- injuries and burns;
- family scandal;
- communication with an unpleasant (from the child’s point of view) relative.
Adults must understand that the child reacts this way unconsciously, and not at all intentionally. This is a temporary and abnormal physiological reaction that is not under the child's control.
The fact that a child has such a reaction is “to blame” for the characteristics of his nervous system, which cannot be changed. A child was born this way, early age is the beginning of all manifestations.
This needs to be corrected by pedagogical measures in order to avoid character problems at an older age.
What does it look like?
Pediatricians conditionally divide affective-respiratory syndrome into 4 types. The classification is as follows:
- A simple option, or holding your breath at the end of the exhalation. Most often develops after a child’s dissatisfaction or trauma. Breathing is restored on its own, and blood oxygen saturation does not decrease.
- The “blue” option, which most often occurs after a pain reaction. After crying, a forced exhalation occurs, the mouth is open, the child does not make any sounds - “rolled”. Rolling of the eyes and cessation of breathing are visible. The baby first turns bright red, then turns blue, then goes limp, and sometimes loses consciousness. Some regain consciousness after regaining their breathing, while others immediately fall asleep for an hour or two. If you record an EEG (encephalography) during an attack, there are no changes in it.
- “White” type, in which the child almost does not cry, but turns sharply pale and immediately loses consciousness. Then comes sleep, after which there are no consequences. No seizure focus is detected on the EEG.
- Complicated - begins as one of the previous ones, but then paroxysms are added, similar to an epileptic attack, which can even be accompanied by urinary incontinence. However, subsequent examination does not reveal any changes. This condition can pose a danger to all tissues due to severe oxygen starvation, or brain hypoxia.
Such convulsions do not pose a threat to life, but consultation with a neurologist is required in order to distinguish them from more severe cases. Breathing stops for a period of time from several seconds to 7 minutes, and it is very difficult for parents to maintain composure. The average time to stop breathing is 60 seconds.
Mechanism of development and clinical picture
Seizures look scary, especially in infants. When a child stops breathing, the supply of oxygen to the body stops. If you hold your breath for a long time, muscle tone reflexively drops - the baby “goes limp.”
This is a reaction to acute oxygen deficiency to which the brain is exposed. A protective inhibition occurs in the brain, its work is restructured to consume as little oxygen as possible.
Eye rolling ensues, which greatly frightens parents.
With continued holding of breath, the muscles sharply increase tone, the child’s body tenses, arches, and clonic convulsions may occur - rhythmic twitching of the torso and limbs.
All this leads to the accumulation of carbon dioxide in the body - hypercapnia. This reflexively stops the spasm of the laryngeal muscles, and the baby takes a breath. Inhalation is usually done while crying, then the child breathes well and calmly.
In practice, seizures rarely occur. After apnea, the child usually immediately stops rolling; in some, breathing is restored after “going limp.”
Breathing and emotions
It’s not for nothing that the attack is called an affective-respiratory attack, or ARP for short. This is how a small child expresses his anger and dissatisfaction if something is done “not according to him.” This is a real affect, an emotional attack. Such a child is initially characterized by increased emotional excitability and capriciousness.
If we leave character traits without attention, then at an older age the child gives real hysterical reactions if he is denied something: he falls to the floor, yells at the entire store or kindergarten, stomps his feet and calms down only when he gets what he wants.
The reasons for this are twofold: on the one hand, the child has hereditary characteristics of the nervous system, on the other, the parents do not know how to treat him in such a way as to smooth out all the “corners” of his character.
What to do during an attack?
First of all, don’t panic yourself. The emotional state of the surrounding adults is transmitted to the baby, and if confusion and fear are “stirred up,” it will only get worse. Hold your breath yourself.
Feel that nothing bad happened to you and your baby due to the temporary delay in breathing movements. Blow on the baby's nose, pat his cheeks, tickle him.
Any such impact will help him quickly recover and breathe.
During a prolonged attack, especially with convulsions, place the baby on a flat bed and turn his head to the side. This will prevent him from choking on vomit if he vomits. Spray him with cold water, wipe his face, and gently tickle him.
If during an attack parents “tear out their hair,” then the baby’s condition becomes more serious. After an attack, even if there were convulsions, give the baby a rest. Don't wake him if he's asleep. It is important to remain calm after an attack, speak quietly, and not make noise. In a nervous environment, the attack may recur.
For any attack with convulsions, you should consult a neurologist. Only a doctor can distinguish ARP from epilepsy or other neurological disorders.
Make an appointment with your doctor if this happens for the first time. It is necessary to distinguish between illness and affective reaction. If the attack has happened more than once, but there is no illness, you need to think about raising the baby.
If this happens to your baby for the first time, you should call a pediatric ambulance, especially if convulsions occur. The pediatrician will assess the severity of the condition and decide whether hospitalization is required. After all, parents are not always able to fully monitor their baby, and this is how the consequences of a traumatic brain injury, poisoning or acute illness can manifest themselves.
Simple rules for parents
The task of parents is to teach the child to manage his anger and rage so that it does not interfere with the lives of the rest of the family members.
Discontent, anger and rage are natural human emotions; no one is immune from them. However, boundaries must be created for the baby, which he has no right to cross. To do this you need this:
- Parents and all adults living with the child must be united in their requirements. There is nothing more harmful for a child when one allows and the other forbids. The child grows up to be a desperate manipulator, from whom everyone then suffers.
- Place in a children's team. There, the hierarchy is built naturally, the child learns to “know his place in the pack.” If attacks occur on the way to the garden, you need to consult a child psychologist, who will specifically indicate what needs to be done.
- Avoid situations where an attack is likely to occur. The morning rush, a queue at the supermarket, a long walk on an empty stomach - all these are provoking moments. It is necessary to plan the day so that the baby is well-fed, has sufficient rest and free time.
- Switch attention. If a child bursts into tears and the crying intensifies, you need to try to distract him with something - a passing car, a flower, a butterfly, snowfall - whatever. It is necessary not to let the emotional reaction “flare up” .
- Clearly define boundaries. If a child knows for sure that he will not receive a toy (candy, gadget) from either his grandmother or aunt, if his father or mother forbade it, then after the most desperate crying he will still calm down. Everything that happens needs to be spoken in a calm tone. Explain why crying is useless. “Look, no one in the store is crying or screaming. It’s impossible - it means it’s impossible.” Sensitive children need to add that mom or dad loves him very much, he is good, but there are rules that no one is allowed to break.
- Call a spade a spade and pronounce the consequences of whims. “You're angry and I can see it. But if you continue to cry, you will have to calm down alone in your room.” You need to be honest with children.
How is the diagnosis made?
First, the doctor comprehensively examines the child. If necessary, ultrasound of the head (neurosonography) and EEG, sometimes a heart examination (ECG, ultrasound), are prescribed. The diagnosis of ARP is made only when no organic disorders are found.
Treatment begins with the proper organization of the child’s life. The recommendations are simple - regimen, diet, walks, activities according to age. But without following these recommendations, no treatment will help, because a measured, orderly lifestyle is the main thing a child needs.
Some parents need sessions with a family psychologist so that they can learn to understand their own children. Drug treatment is rarely required, and in this case it is most often limited to neuroprotectors and nootropic drugs, as well as vitamins.
The best prevention is a calm, friendly atmosphere in the family without quarrels and lengthy showdowns.
Pogrebnoy Stanislav Leonidovich, neurologist
Rate this article:
Total: 129
4.39 129
Source: https://mozgius.ru/bolezni/nevrologiya/affektivno-respiratornyj-pristup.html
Therapy
Treatment uses methods that influence the physiological causes of incontinence (diuretics, antispasmodics, physiotherapy, special nutrition) and the state of the patient’s nervous system (sedatives, psychotherapy).
Medicines
The following groups of drugs are used in the treatment of urinary incontinence:
- M-anticholinergics. The drugs relax smooth muscles, relieve spasms that lead to urination, and increase the reservoir capacity of the bladder. The most effective anticholinergics are Oxybutin and Driptan. Atropine can be used to relieve bedwetting.
- Synthetic analogues of vasopressin. The substance is a natural diuretic that regulates the excretion and reabsorption of water. Its substitutes (Desmopressin, Adiucretin) are used to reduce the volume of urine that is excreted during sleep (with nocturnal enuresis).
- Nootropics. Drugs (Piracetam, Picamilon, Glycine, Pantogam) are prescribed to improve cerebral microcirculation, correct the regimen (when using drugs with a stimulating and sedative effect) and treat sleep disorders associated with rapid falling asleep and profundosomnia.
- Herbal medicines with a sedative effect. For neurotic urinary incontinence, natural sedatives based on valerian, motherwort, and lemon balm are prescribed. Herbal infusions are accepted for 6-12 months.
- Vitamin and mineral complexes.
To treat enuresis in neurosis, tranquilizers (Radedorm, Rudotel, Eunoctine) and antidepressants (Melipramine, Amitriptyline) are also used.
When diagnosing the cause of incontinence, it is important to exclude inflammatory processes in the genitourinary system. If the results of urine microscopy, bacterial culture or PCR tests show signs of infection, the patient is also prescribed antimicrobial agents
The most preferred ones include fluoroquinolones, nitrofurans, macrolides and cephalosporins. In case of viral etiology of inflammation, immunomodulatory (Genferon, Viferon) and antiviral agents are prescribed.
Psychotherapy
Patients who suffer from neurosis-like enuresis are advised to undergo psychotherapy. It allows you to identify the root cause of a neurotic disorder or chronic stress and correct the condition.
Alternative Methods
In addition to psychotherapy and medication, the following methods of treating enuresis are used:
- Monitoring urination using an enuresis alarm. This device detects the humidity of linen or bed and wakes up the patient with a sound and vibration signal, forming a wake-up reflex when the urge occurs. For neurosis-like enuresis, the alarm clock should be used only in combination with psychotherapy and sedatives.
- Diet. A decrease in the volume of fluid consumed and an increase in salt content in the evening causes fluid retention in the body. Dietary therapy is a narrowly applicable practice (helps only symptomatically and only with nocturnal enuresis) and can cause inconvenience to the patient.
- Physiotherapy. Exercise therapy serves to strengthen the pelvic floor muscles and improve urinary sphincter control. Therapeutic exercises can be used for polyetiological enuresis and as an additional therapy for incontinence in girls and women.
- Physiotherapy. The list of the most effective physiotherapeutic methods for enuresis includes electrophoresis, high-frequency current therapy (darsonvalization), magnetic therapy, acupuncture, restorative massage, and electrosleep.
Adult patients are able to independently develop self-control, attend psychotherapy sessions and correct the condition with medications, but treatment of neurological enuresis in children depends entirely on the parents. They should be patient and not express negative emotions directly towards the child, as this may only prolong the therapy. On average, treatment of enuresis takes up to several months.
Advertising:
Causes and mechanisms of development of ARP
During an attack, there is always a provoking factor that causes the child to cry. The question immediately arises: “But all the children cry, and only a few cry?” Of course it is. Crying alone is not enough for ARP to develop. A necessary condition is also increased neuro-reflex excitability, sometimes even hysteria of the child, which leads to a reflex spasm of the respiratory tract (larynx, trachea) when crying in response to an emotional or painful stimulus. In addition, the softness of the cartilaginous tissues of the larynx and trachea in young children predisposes to spasm, especially if the child has rickets. When the cartilage becomes denser, even with strong crying, respiratory spasm and respiratory arrest (apnea) no longer occur.
Apnea leads to a decrease in oxygen content in the blood (hypoxia), resulting in cyanosis and/or pallor and loss of consciousness. If the hypoxia is sufficiently great, convulsions may occur (the child tenses, stretches out, perhaps twitching of the limbs, facial muscles), with a deeper loss of consciousness - involuntary urination. The presence of seizures and involuntary urination does not mean that the baby has epilepsy; these symptoms may be a consequence of hypoxia (“lack of oxygen”) of the brain due to apnea. EEG and video-EEG monitoring help with diagnosis here (see section “Diagnostics”).
With the “pale type” of ARP, in addition to stopping breathing, the child may experience a short-term slowdown or even stoppage of the heart, which stops beating for seconds (synonymous with asystole). Studies have shown that asystole during an attack can reach 2-3 seconds, so the clinical picture is dominated not by cyanosis, but by pale skin due to a short-term decrease in blood flow to the brain, probably aggravated by a decrease in blood pressure. In this regard, the “pale type” in its manifestations is more similar to a fainting (syncope) state.
Factors that aggravate brain hypoxia in ARP and increase the severity of symptoms are anemia (decrease in hemoglobin and red blood cells, iron in the blood), rickets, heart disease (congenital heart defects, arrhythmia, etc.), chronic diseases of the respiratory system (bronchial asthma, bronchiectasis, illness, chronic bronchitis, etc.). As a rule, children with such concomitant diseases suffer from ARP with more severe clinical manifestations.
Violations of the educational and pedagogical approach to the child are of great importance in the development of ARP. Parenting as a “star”, “family idol”, with overprotection often leads to aggravation of hysterical traits in the child, which in turn contributes to a higher frequency of attacks.
Features of the disease
As a medical term, enuresis means any systematic involuntary urination in patients over 5 years of age. In children younger than this age, the nervous system is not mature enough to fully control physiological functions. The urinary disorder becomes clinically significant no earlier than 5-6 years.
In ICD-10, enuresis is listed under the number F98.0 and refers to a group of emotional and behavioral disorders that usually begin in childhood and adolescence.
At the age of 5, enuresis is diagnosed in 15-20% of children. Children one year older suffer from this disease less often - in 7-12% of cases. In the age group of 6-12 years, involuntary urination is observed in 3 children out of 100, and in 12-18 years - in one. In adults, the pathology is even less common - in about 1 person in 200. If enuresis was diagnosed in childhood, the risk of developing pathology in adulthood increases.
A number of specialists in urology and psychiatry also classify pathology by the nature of the patient’s attitude towards episodes of urinary incontinence. Neurosis-like enuresis is characterized by long-term indifference of patients to their condition (mainly pre-pubertal children) and increased experiences afterwards. Neurotic enuresis is characterized by initial psychological discomfort and stress.
Regardless of the type of pathology, neurologists, psychiatrists, psychologists, urologists, physiotherapists, pediatricians or general practitioners should take part in the diagnosis of urinary incontinence. Treatment tactics depend on the etiology of the disease.
Prevention
ARP and paroxysms during an attack are one of the first manifestations of hysteria in a child. Parents must remember that no one is born hysterical; children become like this because of the emotional atmosphere in the family.
To avoid the development of attacks it is necessary:
- clearly outline the boundaries of what is permitted for the child;
- do not shout or punish the baby;
- give the child enough attention, but avoid overprotection;
- treat the child like an adult.
If love and mutual understanding reign in the family, children do not throw tantrums at the slightest provocation. The main task of parents is to do everything so that the child in the family feels loved and protected.
To prevent affective-respiratory paroxysms in a child, experts give parents the following recommendations:
- do not shout or punish the baby. It is better to try to calmly explain to the baby what he is wrong about;
- treat the child like an adult. It is important to take into account the baby’s opinion, his interests, preferences;
- provide rational, balanced nutrition. It is necessary to ensure that the child is not hungry;
- If the baby is capricious and crying, then you need to switch his attention from the problem that worries him and calm him down. This will prevent an emotional reaction from developing.
Diagnosis of parasomnias
To establish a diagnosis and determine the cause of sleep disorders, patients are examined by a neurologist, and, if indicated, by a psychotherapist or somnologist. The main task when diagnosing parasomnia is to exclude or confirm the organic nature of the sleep disorder. Diagnosis of the disorder of this condition includes the following types of laboratory and instrumental studies:
- general examination of the patient with examination of the neurological status;
- analysis of the patient’s complaints and objective data of sleep disorders from the words of relatives;
- polysomnography – sleep phases are studied with their analysis, that is, in which phase changes are observed. At the same time, indicators of the respiratory system, heart function, and blood pressure are taken into account;
- electroencephalography /EEG/ of the brain - to identify epileptic activity of certain parts of the central nervous system;
- MRI of the brain - to exclude organic lesions of the central nervous system;
- computed tomography – to exclude a space-occupying process in the brain;
- consultation with an ophthalmologist - examination of the fundus and determination of visual fields to exclude vascular, traumatic, brain lesions and space-occupying processes;
- laboratory examination of a general blood test - for hemoglobin content, ESR in order to identify an inflammatory process or anemia;
- biochemical blood test for sugar, cholesterol - to exclude diabetes mellitus and atherosclerosis.
How to help your child
Problems of maintaining and strengthening the health of children should be considered from the moment of birth. Prevention is the best way to avoid many diseases in later life.
Affective-respiratory attacks in children, only at first glance, are an ordinary problem, to which the less attention you pay, the faster it goes away. You shouldn't think like that. In fact, it is important to know that nervous disorders only get worse over time.
Dangerous consequences can manifest themselves in the form of poor performance at school, mental and physical development delays.
Somatic disorders may also occur, for example, increased aggregation of erythrocytes, decreased activity of the alveoli in the lung tissue, hypoxia of brain structures, etc.
Understanding what breath-holding spells or an affective-respiratory attack is in a child helps to cope with this common problem. The situation is as follows. In common parlance, this condition is called “rolling up.”
Roughly speaking, the baby, against the background of strong nervous overexcitation, loses control over his autonomic nervous system. A full-blown hysterical attack develops with all the accompanying symptoms.
Affective-respiratory attacks are especially dangerous in infants or newborns, since in the first weeks and months of life there is no clear control over the work of all structures of the central and autonomic nervous system.
At the moment when the baby experiences strong negative emotions, he experiences the effect of a primary convulsive reaction. Moreover, it mainly affects the intercostal muscles and the diaphragm. There is a feeling that he cannot breathe air.
This causes severe fear, which, against the background of hypercapnia, forms the preconditions for respiratory arrest.
The development of an attack of affective breath-holding can be preceded by aggression or hysteria: the child begins to stomp his feet, scream, demand something, try to hit a parent or others, etc.
This is the so-called primary hysterical reaction, which subsequently triggers the mechanism of blocking the respiratory muscles.
It is worth understanding that children really cannot inhale and exhale air for completely physiological reasons. And they need help.
The most important thing that modern guardians of a child prone to affective-respiratory breath-holding and convulsive syndrome should know are options and ways to prevent such paroxysms.
Let's start by understanding the definition of APR as a manifestation of insufficient development of the child's autonomic nervous system. By its pathological nature, an affective-respiratory attack in children is a cessation of respiratory movements of the chest due to the lack of innervation (paralysis) of the intercostal muscles and diaphragm.
Overexcitation of the nervous system can also turn off the child’s consciousness. This is necessary to quickly restore the reserve of the central nervous system. The lack of oxygen supply to the brain structures makes the baby temporarily forget about the emotional background that led him to such a state.
After an attack, the child experiences severe drowsiness and relaxation of the muscular frame of the body. It's best to let him sleep. After awakening, there will be no trace left of the hysterical paroxysm.
Many pediatricians still recognize only one cause of affective-respiratory attack in children, and this is typical hysteria. However, in reality everything is much more complicated.
There are multiple or complex causes of an affective-respiratory attack, and among them there is indeed an excessive or hysterical reaction of the autonomic and central nervous system to the influence of a negative traumatic factor.
But this is far from the only factor that provokes ARP.
So, pathogenetic influence factors include:
- weakness of the autonomic nervous system, such children will suffer from vegetative-vascular dystonia in the future;
- consequences of severe birth trauma (cerebral hypoxia, low assessment of the condition of the non-born on the Apgar scale);
- violation of the daily routine and regular lack of sleep (often found in children attending kindergarten and parents going to bed late);
- insufficient amounts of B vitamins and some important amino acids in the diet;
- the presence of serious chronic somatic pathologies;
- increased convulsive readiness;
- increased muscle tone;
- disruption of the development of cerebral blood vessels of the neck;
- thyroid diseases;
- adenoiditis, tonsillitis and other chronic pathologies of the upper respiratory tract that complicate the process of physiological breathing.
The modern classification of attacks of affective-respiratory arrest with convulsive syndrome implies subdividing them into 4 distinct types.
Depending on the clinical manifestations of pathological spasm of the respiratory muscles, the following types of attacks are distinguished:
- blue ARP begins with hysteria, followed by a sharp deep breath and then asphyxia (lack of breathing) sets in, hyperemia of the skin quickly gives way to cyanosis, the child loses muscle tone and becomes limp, and may lose consciousness;
- white ARP is more complicated, with obligatory loss of consciousness and the rapid onset of characteristic pallor of the skin of the face, neck and chest;
- a simple type of ARP occurs without hypercapnia and hypoxia, the breath holding is short-term and does not exceed 20 seconds;
- a complicated type of ARP occurs with severe hypoxia of the brain (if there is no breathing for more than 60 seconds), accompanied by involuntary urination and convulsions in the lower and upper extremities.
It is important to understand that the clinical picture of ARP may resemble an epileptic attack. Therefore, it is important to conduct a full examination to exclude epilepsy. Symptoms may include the following:
- the increase in hysterical reaction to external negative influence occurs within 2-4 minutes;
- with a gradual deepening of hysteria, the child experiences overexcitation of the cerebral cortex;
- control over the muscles is lost - at this moment you can see stopping breathing and loss of tone of the whole body;
- the baby seems to go limp, stops breathing and slowly slides to the floor;
- the skin of the face, neck and chest begins to change color - at first they turn sharply red, then, depending on the type of attack, they turn white or blue;
- a short-term loss of consciousness may occur;
- After a few seconds, the child comes to his senses, abruptly stops crying and begins to breathe fully.
It is important to understand that affective-respiratory convulsions are only superficially similar to the manifestation of epilepsy. However, to exclude such a condition, it is not enough to know the main differences.
Diagnosis necessarily includes an EEG (electroencephalogram of the brain). This examination shows the absence of a focus of excitation in the cortex and brain structures in ARP and its presence in epilepsy.
Therefore, this examination is definitely worthwhile. At least to calm myself down. And treat the baby more correctly.
Under no circumstances should a child be allowed to achieve his goals with such hysterical attacks. Otherwise, such a style of behavior will be fixed at a reflex level.
You will receive regular affective-respiratory attacks at the slightest reason for the child’s negative perception of reality.
The distinctive features of epileptic seizures and affective-respiratory attacks are as follows:
- Various circumstances lead to ARP, and epilepsy manifests itself without external causes;
- ARP always develops differently, but epileptic seizures are always the same;
- In children under 4 years of age, epileptic seizures account for no more than 2% of the total number of such disorders;
- in children over 5 years of age, attacks of affective-respiratory disorder are diagnosed only in 1% of the total number of cases;
- with ARP, valerian, motherwort and nootropic treatment help;
- in case of a true epileptic seizure, it is useless to give sedatives;
- There are significant pathological changes in the EEG only in epilepsy.
If the baby has an attack, then it is necessary to show him to the doctor within the next 1.5 hours. These manifestations can be the result of very dangerous diseases.
Only in a medical institution can an ECG of the heart and an ultrasound of internal organs be done to exclude heart defects, pulmonary vein embolism and other dangerous conditions; spirography, an X-ray of the lungs, and examination of the trachea for the presence of foreign bodies may also be required.
You need to know what to do when such symptoms appear, and what you should avoid categorically. Providing first aid to a child when symptoms of ARP appear should begin with clearing the airways. You can take the baby out into the fresh air. You need to unfasten the top buttons and remove the pressure on your neck.
It is important not to get confused or panic. Try to maintain your composure and smile. This will help the baby recover faster. Try patting him on the cheeks or lightly tickling him. If you have ammonia on hand, give it a sniff. Just don't bring it too close to the baby's face.
In case of loss of consciousness, it is important to create conditions to prevent tongue retraction. To do this, place the child on a flat surface and turn his head to the side. And here you should call an ambulance.
Therapy begins with behavior correction and psychological work with parents. Such conditions most often occur in children raised in families where parents do not follow the rules of communication with them.
Treatment of affective-respiratory attacks begins with a consultation with a neurologist. A specialist can give a referral to a psychologist to correct the mental state of both the baby and his parents. Drug therapy may then be prescribed. But, as a rule, it does not give any special results. It is much more important to take the following steps:
- normalize the child’s daily routine:
- develop a special diet containing all vitamins, minerals and amino acids;
- exclude, if possible, traumatic factors;
- teach your child to listen to his parents and compromise with them.