Facial hemispasm is a pathological condition that is characterized by the occurrence of involuntary tonic and clonic spasms of facial muscles on one half of the face.
Facial hemispasm, or Brissot's spasm, was first described in detail in the 19th century by the French neurologist E. Brissaud. The disease is extremely rare in the population (5-7 people per 100 thousand population). Brissot's cramp is more often diagnosed in people over 30 years of age. Women are slightly more susceptible to this disease.
History of discovery
Facial hemispasm was first described by Gowers in 1884.
This pathology occurs after 50-60 years and mainly on one side of the face. There is also a severe form of the lesion, when muscle spasms occur on both sides. The disease begins with short pulsations of the orbicularis oculi muscle.
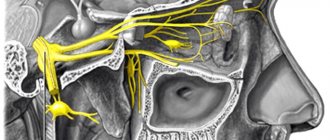
All facial muscles are gradually involved: zygomatic, frontal, subcutaneous and others. Clinical movements progress over time and become persistent spasms of all muscles. Chronic nerve irritation in the face occurs due to various reasons.
Causes of primary and secondary nature
Experts have divided the causes of hemifacial spasm into primary and secondary. The primary causes include compression of the nerve as it exits the brain stem by a small blood vessel - such spasms are called idiopathic.
Secondary causes include compression of the facial nerve by a vascular malformation, tumor, and so on.
Primary causes, that is, contact of the facial nerve with an adjacent vessel, most often occur in hypertensive patients, the elderly and women during menopause.
For the occurrence of facial hemispasm, the following factors are sufficient:
- damage to the cerebral cortex;
- multiple sclerosis;
- impaired blood circulation;
- cyst and tumor of the brain;
- genetic predisposition;
- toxic poisoning by harmful substances;
- long-term use of antibiotics or hormonal drugs.
Gradually, the sensitivity of the affected nerve increases and spasms are provoked by minor environmental influences: cold, blinding light or strong sound.
The spasm resumes when eating, talking, laughing, which leads to irritation, sleep disturbance, fatigue and stress, which further aggravate the course of the disease. At the same time, the pressure on the vascular walls increases, neighboring tissues swell and oppress areas in the area of the nerve, as a result it again torments the patient.
Clinical signs
To diagnose the pathology, a thorough examination of the patient by a neurologist is required.
As a rule, the manifestation of the disease begins with twitching of the orbicularis oculi muscle, which occurs rarely. Gradually, neighboring muscles are involved in spasm and move to half of the face, and the frequency of attacks increases and reaches the point that the patient cannot see one side with his eye. Atypical and secondary spasms begin with contractions of the cheek muscles, spreading up the face. The attacks begin without cause and may persist during sleep.
After a long period of time, the patient may develop moderate paresis (muscle weakness) of the facial muscles on the affected side. Bilateral hemispasm develops extremely rarely.
Facial spasms
Cramps are involuntary paroxysmal contractions of muscles, their twitching. Convulsions of the face, legs and any parts of the body can be tonic or clonic. Tonic cramps are muscle tension called spasms. The clonic variant of seizures is considered an involuntary muscle twitching. A combination of them is possible. We are talking about tonic-clonic seizures.
Also, seizures are divided into partial and general . Partial cramps are cramps that occur in a specific muscle group. Their appearance may be associated with stereotypical movements and muscle strain, as well as hypothermia, etc. Local cramps that occur in the muscles of the hand, foot, trunk and face can occur due to serious damage to the area of the brain that is responsible for the innervation of this muscle group. In this case, the occurrence of seizures will be observed on the side opposite to the lesion. General convulsions (generalized) are a consequence of epileptic syndrome, as well as a complication of intoxication, traumatic brain injury and an infectious process.
Establishing diagnosis
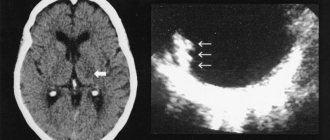
Diagnosis of hemaspasm is based on analysis of the patient’s clinical picture. An examination by a neurologist is also carried out. Computed tomography and magnetic resonance imaging can help make the correct diagnosis.
MRI helps to identify the cause of facial nerve spasm: tumor, aneurysm, vascular malformation, focus of lacunar infarction, and others. MRI can determine whether primary or secondary spasm is present.
This pathology has symptoms similar to some diseases, which should be excluded when examining the patient. To do this, it is necessary to make a differential diagnosis. The list of diseases and syndromes for differential diagnosis is presented as follows:
- essential blepharospasm;
- facial myokymia;
- teak;
- cortical seizures;
- tardive dyskinesia;
- postparalytic hemispasm.
Urinary incontinence due to neurogenic detrusor overactivity
Before injection, in accordance with the clinical approach, intravesical administration of a diluted anesthetic (with or without sedatives) or general anesthesia is used. In the case of local injection of an anesthetic into the bladder, it is necessary to catheterize the bladder and rinse it with a sterile 0.9% sodium chloride solution before the next stages of the Botox® injection.
The recommended dose of Botox® is 200 units, with 1 ml (about 6.7 units) administered into 30 detrusor points.
Diluted Botox® (200 units/30 ml) is injected into the detrusor muscle using a rigid or flexible cystoscope, avoiding the vesical triangle and the bottom of the bladder. The bladder should be filled with a sufficient amount of 0.9% sodium chloride solution to adequately visualize the injection points; however, bladder overdistension should be avoided.
Before starting injections, the injection needle should be filled (flushed) with approximately 1 ml of solution (depending on the length of the needle) to remove air.
The needle should be inserted approximately 2 mm deep into the detrusor, making 30 injections of 1 ml (total volume 30 ml) at points located approximately 1 cm apart (see figure). As a final injection, approximately 1 ml of sterile 0.9% sodium chloride solution is administered until the full dose is reached. After completing the injections, the 0.9% sodium chloride solution that filled the bladder is withdrawn for better visualization. The patient should be observed for at least 30 minutes after injections.
Clinical improvement is usually observed within 2 weeks. Repeat injections should be considered after the effect of the previous injection has subsided (in clinical studies, the average duration was 256-295 days (36-42 weeks) based on patient request for re-treatment), but not earlier than 3 months after the previous bladder injections.
The safety and effectiveness of Botox® in the treatment of urinary incontinence due to neurogenic detrusor overactivity in children (under 18 years of age) have not been demonstrated.
Therapy methods
Treatment of hemifacial spasm is carried out using various methods in a comprehensive manner, after which the disease disappears completely or is blocked. The method of therapy is chosen by the doctor after a thorough examination of the patient.
Methods to combat facial hemispasm include drug treatment, botulinum toxin injections, microvascular decompression, and treatment with traditional recipes.
Conservative - medicinal method
The treatment program is aimed at the use of drugs from various pharmacological lists: Baclofen, Gabapentin, Levetracem, Cponazepam.
- But this method has disadvantages: long-term use is impossible because:
- the effect of exposure decreases and the dosage has to be increased;
- there are no indicative statistics, since large-scale studies have not been conducted;
- There are side effects leading to drowsiness, loss of concentration, and decreased quality of life.
But in the early stages of the disease, conservative treatment is sufficient, which can completely eliminate the pathology.
Botulinum toxin
This method involves injecting a drug into the affected nerve. Botulinum toxin type A is used. The drug helps well in the early stages and in advanced forms of the disease.
But this method also has disadvantages:
- the high cost of treatment, in addition, repeated injections are required after 3-4 months, the drug requires responsible storage;
- Treatment is contraindicated for patients with eye diseases or poor vision; the drug may cause deterioration.
Therefore, before treatment, the doctor prescribes an examination of the patient by an allergist and ophthalmologist.
The absence of contraindications facilitates botulinum toxin injections, which has a positive effect on the cure of patients in 75% of cases.
Microvascular decompression
Hemispasm is considered a “conflict” between the facial nerve and the vessel, so they are separated by a Teflon protector as a result of a neurosurgical operation.
The protector dampens painful pulsations that form facial spasms. Neurosurgical interventions are used very widely and have been practiced for more than 40 years. Statistics show that in 90% of cases hemispasm disappears forever.
ethnoscience
To treat facial hemispasm with folk remedies, compresses are applied to the area of the face affected by the spasm.
You can make an onion compress: to do this, one head of white onion should be chopped in a meat grinder, placed between layers of gauze and applied to the affected area. A garlic-lemon compress is made in a similar way, for which you need to chop a few cloves of garlic and moisten them with lemon juice.
Apply both compresses carefully so as not to harm the eyes. These methods do not cure the disease, but relieve pain and soften the attack of spasm.
All treatment is carried out in conjunction with a special diet. The diet includes foods containing B vitamins, potassium and magnesium. These elements reduce the risk of hemispasm. It is necessary to exclude fatty foods and coffee from the diet.
Idiopathic overactive bladder
Before administering the drug, intravesical instillation of a diluted solution of a local anesthetic with or without a sedative effect is possible. Before intravesical instillation of local anesthetic, it is necessary to empty the bladder and rinse it with a sterile 0.9% sodium chloride solution.
The recommended dose of Botox® is 100 units in the form of 0.5 ml (5 units) injections into 20 detrusor points.
Diluted Botox® (100 units/10 ml) is injected into the detrusor muscle using a rigid or flexible cystoscope, avoiding the area of the bladder triangle and the bottom of the bladder. The bladder should be sufficiently filled with 0.9% sodium chloride to achieve proper visualization of the injections, but excessive distension of the bladder should be avoided.
Before starting injections, the injection needle should be filled (flushed) with approximately 1 ml of solution (depending on the length of the needle) to remove air.
The needle should be inserted approximately 2 mm deep into the detrusor, making 20 injections of 0.5 ml (total volume 10 ml) at a distance of approximately 1 cm from each other (see figure below). The last injection is approximately 1 ml of sterile 0.9 % sodium chloride solution so that the total dose is administered completely. After completing the injections, the 0.9% sodium chloride solution that filled the bladder is withdrawn for better visualization. The patient should be observed for at least 30 minutes after injections until spontaneous urination occurs.
Clinical improvement is usually observed within 2 weeks. Repeat injections should be considered after the effect of the previous injection has subsided (median duration of effect in phase 3 clinical studies was 166 days (approximately 24 weeks) based on patient request for retreatment), but not earlier than 3 months after the previous bladder injections.