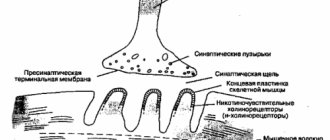
The work of all muscles in the body of a healthy person is innervated by nerve endings, that is, the nervous system sends a certain impulse that acts directly on the muscle fiber, as a result of which it contracts or relaxes.
When there is a failure in the transmission of these impulses, various diseases occur, one of which is myasthenia gravis.
- Causes of myasthenia gravis
- Symptoms of myasthenia gravis, characteristic signs
- Diagnosis of myasthenia gravis
- Myasthenia gravis treatment, drugs
What is myasthenia gravis, causes of development
Few people know what myasthenia gravis is. This disease is studied by neurology; the exact causes of its occurrence are still unknown. But it is clear that it is caused by a violation of impulse transmission between nerves and muscles.
The transmission of impulses from nerve endings to muscle fibers is accompanied by the release of neurotransmitters (hormones in the brain that carry out neuromuscular transmission). In Erb-Goldflam disease, antibodies block or eliminate large numbers of muscle receptors for acetylcholine (a neurotransmitter). As a result, fewer impulses are sent to the muscles, causing them to weaken over time.
One theory is that the thymus (a gland in the upper chest), which is part of the immune system, may help produce antibodies that destroy muscle acetylcholine receptors.
Reference. In children, the thymus is large; in adult patients it is small. However, in patients who suffer from myasthenia gravis, this gland is greatly enlarged. Often the pathology is combined with a thymus tumor.
The course of asthenic bulbar palsy (ABP) is aggravated under the influence of negative factors:
- chronic fatigue;
- infectious diseases;
- stress;
- pregnancy;
- immunity disorders;
- certain medications, for example, beta-blockers, calcium antagonists, quinine, some antibacterial agents;
- excessive heat, etc.
Under the influence of these factors, antibodies actively destroy the postsynaptic membrane, which is responsible for transmitting nerve signals between neurons. Then the transmission of impulse slows down and eventually stops completely.
Forms
Myasthenia gravis, or myasthenia gravis, as doctors call the disease, can develop at different periods of life. The disease can be congenital or acquired.
Depending on the age at which the first symptoms of the pathology appear, the following forms are distinguished:
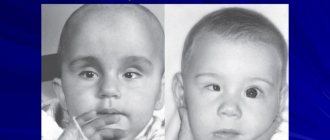
- Congenital is a rare form of the disease that develops during fetal development. The pathology is transmitted from the mother, who also suffers from it. The newborn is weak, inactive, and has difficulty breathing. Often the child dies immediately after birth, although in some cases it is possible to put myasthenia gravis into remission after proper therapy.
- Early – muscle weakness manifests itself in children from 3 to 5 years old.
- Youthful – signs of increased muscle fatigue are observed from 12 to 16 years.
- Adults – symptoms of myasthenia gravis occur in patients aged 20–30 years.
And there is also a difference between myasthenia gravis and muscle groups in which weakness is more pronounced:
- The generalized (pseudoparalytic or malignant) form is characterized by uniform weakening of muscles throughout the body. This is a serious illness that may or may not be accompanied by weakness of the respiratory muscles.
- Local forms. This group includes ophthalmic (eye) myasthenia gravis, which causes drooping eyelids and visual disturbances. The bulbar form of the pathology is accompanied by difficulty swallowing and speech disorders. With musculoskeletal myasthenia, a specific group of muscles is weakened, for example, in the upper or lower extremities.
Local forms of the disease may or may not be accompanied by breathing problems.
Manifestations of the disease
The symptoms of myasthenia gravis are specific, so they are difficult to confuse with signs of any other disease. They begin to manifest themselves in stages, and here is what usually happens and in what order:
- Weakness of the facial, pharyngeal and masticatory muscles.
- Fast fatiguability. A person gets tired even after the simplest manipulations with his hands or walking.
- Low mobility.
- Weight loss and physical exhaustion.
- Swallowing problems (dysphagia).
- Changes in facial expressions and gait.
- Weakness of the neck and respiratory muscles.
- Impaired sensitivity of the tongue, pharynx and lips.
- Weightening of the eyelids and deterioration of vision.
During the day, the severity of symptoms changes, and a person’s well-being after prolonged muscle tension worsens significantly. In the morning a person may feel healthy and energetic, but after a few hours he begins to feel tired, which progresses very quickly.
Symptoms
The disease is manifested by the main syndrome – pathological muscle fatigue. The symptoms of generalized and local myasthenia gravis are different.
At first, the pathology has a gradual course, so it is often detected when it has already become an advanced form. Therefore, it is important for anyone to know what symptoms it manifests at an early stage:
Huntington's disease and its symptoms
- the voice fades towards the end of the speech;
- difficulty chewing solid food;
- the swallowing process is disrupted;
- Fatigue sets in faster when walking, climbing stairs, or doing activities in which your arms are raised up;
- a shuffling gait appears;
- eyelids droop.
The muscles most often affected are those responsible for eye movement, facial expressions, chewing, and swallowing.
If desired, anyone can perform tests that will help detect early myasthenia gravis:
- Open and close your mouth quickly for 30 seconds. If a person is healthy, he will do this 100 times, and a sick person will do it less.
- Lie on your back, raise your head, fixate for 60 seconds, looking at your stomach.
- Stretch your arms out in front of you and stand there for 3 minutes.
- Do deep squats 15–20 times.
- Quickly clench and unclench your hand. The patient's eyelids droop after such actions.
With ocular myasthenia, the patient experiences eyelid ptosis, visible objects become bifurcated, and eye mobility is limited. The pharyngeal-facial (bulbar) form of the pathology is manifested by weakening of the muscles of the soft palate, pharynx, and larynx. Then the patient's voice weakens during conversation or it becomes nasal. It becomes difficult for him to chew, swallow solid and then soft food, and over time he switches to tube feeding. The patient's speech becomes slurred, and the pronunciation of sounds is distorted.
With myasthenia gravis, the patient has difficulty chewing and swallowing food
Over time, the chewing and facial muscles weaken. Then facial expressions become less active, wrinkles are smoothed out, and when smiling, the lower lip remains motionless. Chewing food becomes difficult, the mouth is constantly slightly open, and the pronunciation of labial sounds is distorted.
Important. With local myasthenia, there is a risk of immobilization of the muscles of the vocal cords, which leads to suffocation.
Myasthenia gravis initially manifests itself as muscle weakness after physical activity. Over time, this symptom becomes more pronounced. All groups of striated muscles (face, neck, torso, limbs) are affected. In advanced cases, breathing becomes difficult. In addition, the sphincter muscles weaken, which results in involuntary urination and defecation. As the pathology develops, the patient loses the ability to care for himself.
Important. If untreated, pseudoparalytic myasthenia gravis is complicated by myasthenic crisis. This condition is life-threatening for the patient.
It is important to be attentive to your health in order to notice the first signs of myasthenia gravis in time and carry out treatment.
Diagnostics
If suspicious signs appear, the patient should contact a neurologist. First, the specialist conducts a survey, he is interested in information about the symptoms present, their connection with physical activity, taking medications, and the presence of myasthenia gravis in relatives. Next, a neurological examination is performed to identify reflex activity, muscle strength, muscle tone, coordination, and vision assessment. For this purpose, tests are performed with repetitive movements; if weakness increases during the procedure, this indicates myasthenia gravis.
And they also conduct a proserine test to assess the strength of muscles that get tired faster. Then the doctor gives an injection of Proserin, which strengthens the impulse between the nerve endings and muscles. Then the test is repeated, if muscle strength increases, then the patient has myasthenia gravis.
Laboratory blood tests will help identify antibodies that destroy acetylcholine receptors. In some cases, antibodies may be absent in Erb-Goldflam disease.
Electromyography is used to evaluate nerve conduction. During the procedure, electrodes are fixed on the body, through which a weak current is supplied to the muscles for a long time. If, as the muscles get tired, the impulse weakens, then this indicates pathology.
Needle myography is used to measure the electrical activity of a specific muscle fiber. To do this, a thin electrode is inserted into the muscle, which resembles an injection needle.
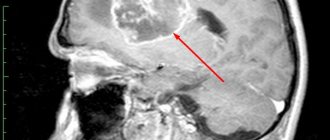
For a layer-by-layer study of the structure of the chest, namely the anterior mediastinum, CT or MRI is prescribed. These tests help identify thymic tumors.
And differential diagnostics are also carried out, which will distinguish myasthenia gravis from meningitis, polymyositis (inflammation of muscle tissue), ocular myopathy, etc.
List of abbreviations
AChR - acetylcholine receptors
CT – computed tomography
MRI – magnetic resonance imaging
QMGS - quantitative myasthenia gravis severity scale
MGFA - Myasthenia Gravis Association of America
RIA – radioimmunoassay
ELISA – enzyme immunoassay
BP - blood pressure
RR – respiratory rate
AOS – acid-base state
GHB – gamma-hydroxy-butyric acid
VC – vital capacity of the lungs
MOV – minimum inspiratory volume
DO – tidal volume
ALS – amyotrophic lateral sclerosis
IVL - artificial lung ventilation
M – myasthenia gravis
EMG – electromyography
Ig – immunoglobulin
MuSK – muscle specific kinase
RyR – ryanodine receptors
- Vetshev P.S., Ippolitov L.I., Merkulova D.M., Zhivotov V.A. Surgical treatment of thymomas in patients with generalized myasthenia // Surgery. – 2003. – No. 10. – P.15-20.
- Vetshev P.S., Sanadze A.G., Sidnev D.V. Zhivotov V.A. Antibodies to titin in patients with myasthenic and non-myasthenic thymoma // Surgery. – 2007. – No. 6. – P.42-48.
- Gekht B.M. Syndromes of pathological muscle fatigue. M. Med. 1974. – 164 p.
- Lantsova V.B., Sepp E.K. Immunobiochemical features of IgG antibodies in myasthenia gravis // Bulletin. Let's experiment. biol. and honey – 2002. – T. 133. – No. 6. – P.678-680.
- Kuzin M.I., Gekht B.M. Myasthenia. - M.; Medicine, 1996. – 224 p.
- Sanadze A.G., Sidnev D.V., Gekht B.M., Khlebnikova N.N., Chugunova N.A., Shcherbakova N.I. Antibodies to the acetylcholine receptor in the diagnosis of myasthenia gravis and other forms associated with the pathology of neuromuscular transmission. Neurological Journal. – M.: Medicine. – 2003. – T.8. - Annex 1. – P.19-20.
- Sanadze A.G., Sidnev D.V., Davydova T.V., Shcherbakova N.I., Kapitonova Yu.A., Kasatkina L.F., Semyatitskaya R.N., Gilvanova O.V., Menenkova E. .YU. Antibodies to muscles (anti-titin antibodies) in patients with late onset myasthenia gravis: clinical and electrophysiological correlations // Neurological Journal. – T.8. – Appendix 1. – 2003. – pp. 23-26.
- Sanadze A.G. Myasthenia and myasthenic syndromes. M. Litera, 2012. –250 p.
- Sanadze A.G., Sidnev D.V., Vetshev P.S., Ippolitov L.I. Titin, thymoma and myasthenia // Journal of Neuroimmunology. – 2006. – T.5. – No. 3-4. – P.23-26
- Sidnev D.V., Sanadze A.G., Shcherbakova N.I., Davydova T.V., Gilvanova O.V., Galkina O.I., Kononenko Yu.V. Antibodies to muscles (anti-titin antibodies) in the diagnosis of myasthenia gravis combined with thymoma // Neurological Journal. – T.8. – Appendix 1. – 2003. – P.21-23.
- Sidnev D.V., Karganov M.Yu., Shcherbakova N.I., Alchinova I.B., Sanadze A.G. Antibodies to the acetylcholine receptor in patients with various clinical forms of myasthenia gravis and Lambert-Eaton myasthenic syndrome // Journal of Neurology and Psychiatry named after S.S. Korsakov. – 2006. – T.106. – No. 1. – P.55-58.
- Kharchenko V.P., Sarkisov D.S., Vetshev P.S., Galil-Ogly G.A., Zayratiants O.V. Diseases of the thymus gland. – M.: Triada-X. – 1998. – 232 p.
- Aarli JA, Stefansson K., Marton L., Wollmann RL Patient with myasthenia gravis and thymoma have in their sera IgG autoantibodies against titin // Clin. Exp. Immunol. – 1990. – V.82. – No.2. – P.284-288.
- Aarli J., Skeie G., Mygland A., Gilhus N. Muscle striation antibodies in myasthenia gravis. Diagnostic and functional significance // Ann. NY Acad. Sci. – 1998. – V. 841. – P.505-515.
- Aarli JA Titin, thymoma, and myasthenia gravis. //Arch. Neurol. – 2001. – Jun. – V.8. – No.6. – P.869-870.
Treatment methods
Treatment of myasthenia gravis should be comprehensive: lifestyle changes, medication, physical therapy, physiotherapy, diet, etc. The choice of methods is made by the doctor, taking into account the type of disease, the rate of its development, and the patient’s age.
Drug treatment is the basis of therapy. Medicines improve neuromuscular patency, reduce the production of antibodies, improve metabolic processes and muscle condition.
List of medications used in the treatment of myasthenia gravis:
- Acetylcholinesterase inhibitors: Prozerin, Oksazil, Kalimin, Mestinon. These drugs prevent the breakdown of acetylcholine, then the substance accumulates at the junction of nerves with muscles, and muscle fatigue is reduced. Anticholinesterase drugs are the mainstay of symptomatic treatment.
- Corticosteroids, such as Prednisolone, suppress the activity of the immune system by reducing the production of antibodies that destroy acetylcholine receptors.
- Immunosuppressants: Azathioprine, Cyclosporine, Mycophenolate, Methotrexate. These medications may be used by older patients if anticholinesterase drugs and corticosteroids are ineffective. Immunosuppressants suppress the immune system.
Carefully. Long-term use of corticosteroids during treatment of myasthenia gravis increases the risk of bone destruction, weight gain, diabetes, infectious diseases, etc.
Anticholinesterase medications are recommended to be combined with potassium supplements, which improve muscle contraction and neuromuscular transmission. Antioxidants improve metabolic processes and nutrition of tissues throughout the body.
Reference. In Israel, they have developed a new medicine for the treatment of myasthenia gravis called Monarsen, the action of which is associated with the inhibition of anticholinesterase (an enzyme that destroys acetylcholine). The drug is at the research stage. Many patients who experienced the effect of Monarsen improved their general condition and neurological status. Side effects after its use have not yet been noticed.
One of the methods of treating myasthenia gravis is plasmapheresis.
Myasthenia gravis can be treated using plasmapheresis. This is a procedure during which the patient's blood is filtered in a special apparatus, while the plasma with antibodies is separated, but the blood cells are preserved. The blood cells are then injected back into the bloodstream along with rheopolyglucin (a plasma substitute). However, the therapeutic effect after the procedure lasts for several weeks. The disadvantages of plasmapheresis include the likelihood of difficulty accessing the vein, decreased pressure, and bleeding due to the use of anticoagulants.
To normalize the functionality of the immune system and provide the body with normal antibodies, human immunoglobulin is used. The mixture is administered intravenously, after which the severity of the autoimmune process decreases. This procedure has fewer side effects than plasmapheresis, although the therapeutic effect appears after a few weeks and lasts 4-8 weeks.
If the pathology progresses rapidly, a tumor of the thymus is present and weakening of the pharyngeal muscles is observed, then the patient is prescribed a thymectomy. This is an operation to remove the thymus gland, during which anesthesia is used. Thymectomy is indicated for a disease that lasts no longer than 10 years in patients under 60 years of age.
Reference. If surgery for myasthenia gravis is contraindicated, then radiation therapy is performed to suppress thymus function.
Nutrition for myasthenia gravis must be correct, it is important to replenish the diet with foods rich in potassium, calcium, phosphorus: fresh fruits (bananas, avocado, melon), vegetables (legumes, potatoes, pumpkin), dried fruits, dairy products, egg yolks, fish, cereals (buckwheat, pearl barley, oatmeal), etc. You need to eat food during the period of highest muscle strength, take breaks while chewing. It is recommended to eat soft foods; it is better to avoid hard foods. Foods with magnesium (spinach, broccoli, flounder, carp, mackerel, etc.) and those that have a diuretic effect (green tea, cucumbers, tomatoes, watermelons, Brussels sprouts, etc.) should be excluded from the diet.
Complex therapy can be supplemented with folk remedies. However, use them only after consulting your doctor.
Exercise therapy increases the body's nonspecific resistance, prevents the development of muscle atrophy, and improves the functionality of the respiratory and cardiovascular systems. The complex is compiled by a doctor, taking into account the form of the pathology, its severity and general condition. It is recommended to perform simple gymnastic and breathing exercises with measured load. It is important to alternate activity with periods of relaxation and breathing exercises to avoid excessive fatigue. In severe myasthenia gravis, physical training is carried out only at the stage of remission.
Treatment can be supplemented with physiotherapeutic procedures, for example, electrophoresis, myoelectrostimulation, diadynamophoresis, darsonvalization, therapeutic massage. Physical treatment methods help improve the functions of the neuromuscular system, improve the condition of the nervous system, and relieve dystrophic disorders.
How to treat the disease
Improvement in the patient’s well-being with myasthenia gravis is achieved only against the background of correction of neuromuscular impulses. To restore disrupted processes, acetylcholine and drugs that suppress anticholinesterase are prescribed. And glucocorticoids are used to regulate immunological disorders.
If the treatment effect is insufficient, additional therapeutic measures are used - intravenous administration of a large dosage of methylprednisolone.
In addition, an important stage in the treatment of myasthenia gravis is the prescription of potassium-sparing agents, including a diet high in dried apricots, bananas and raisins.
When treating a generalized form of pathology, it is permissible to use surgical intervention in the area of the thymus gland.
To restore the health of elderly patients, cytostatic therapy and blood purification are used.
Complications
The main complication of Erb-Goldflam disease is myasthenic crisis. This condition is accompanied by the following symptoms:
- Frequent shallow breathing, which becomes rare and intermittent. The face first turns red, then turns blue. In the absence of help, the person dies from respiratory arrest.
- The heart rate increases (up to 180 beats/min), blood pressure rises (up to 200 mm Hg). Then the pulse slows down.
- Saliva is produced abundantly and sweat production increases.
If the patient is not helped, brain damage occurs due to hypoxia.
If the muscles are severely weakened, disability may occur.
Contraindications for myasthenia gravis
There are contraindications for myasthenia gravis that the patient should take into account to avoid complications:
- Alcoholic drinks.
- Prolonged exposure to the sun.
- Excessive physical activity.
Some patients are interested in what antibiotics can be taken for illness. These drugs are contraindicated as they impair neuromuscular transmission. For the same reason, it is prohibited to take antipsychotics, antiepileptic drugs, calcium antagonists, neuromuscular blockers, etc.
Reviews
Many patients have learned to control myasthenia gravis and undergo regular treatment to maintain good health. Some of them decided to undergo thymectomy, after which most of them improved their condition. However, cases of death of patients from myasthenic crisis are not uncommon.
Reviews from patients:
Maria, 56 years old: “I was diagnosed with myasthenia gravis at the age of 45. Doctors prescribed surgery to remove the thymus. Then I took Kalimin and Metipred. After completing the course, weakness and ptosis disappeared. Of course, I have to periodically take medications, go on a diet, and do special exercises, but now I remember the illness as a bad dream.”
Svetlana, 48 years old: “I suffered for a long time from muscle weakness: I could not climb stairs, dry my hair with a hairdryer, swallow food, and I felt short of breath. I went to the hospital, where I was diagnosed with myasthenia gravis. Doctors prescribed me Prednisolone, Kalimin, Potassium orotate. And they also performed plasmapheresis and physiotherapy. At home I did therapeutic exercises and went for a massage. After some time, the symptoms slowly began to disappear. It’s been 1.5 years now, I’m regularly undergoing treatment and there are no symptoms yet.”
Veronica, 33 years old: “My sister died of myasthenic crisis at 30 years old. She felt sick at work, fell and began to choke. Colleagues called an ambulance and she was hospitalized. She was in intensive care for about a week, but the doctors were unable to save her.”
Folk remedies
Along with drug therapy, it is possible to treat myasthenia gravis at home with folk remedies in order to speed up recovery and alleviate the condition. However, any traditional treatment methods must be agreed with the observing specialist.
Effective means:
- Oats. The grains are thoroughly washed and filled with water in a volume of 0.5 liters. Next, the container is placed on the fire, the composition is brought to a boil, and steamed for at least half an hour. Next, to prepare the infusion, wait another 2 hours, removing the oats from the heat. The resulting decoction is taken an hour before meals, at least 4 times a day. The duration of therapy is 3 months with a break of 1 month and another course of treatment.
- Onion. The product in a volume of 200 grams (purified) is mixed with 200 grams of sugar and filled with water in a volume of 0.5 liters. The composition is placed on low heat and cooked for 1.5 hours. Next, cool the mass, add two tablespoons of honey and take two teaspoons three times a day.
- Three heads of garlic are crushed and mixed with four lemons, a liter of honey and linseed oil (200 g). All ingredients must be thoroughly mixed and taken daily, one teaspoon three times a day.
The most important
Myasthenia gravis is an incurable, dangerous disease that requires regular or continuous courses of treatment. In the absence of proper therapy, it can lead to disability and death from myasthenic crisis. To avoid dangerous complications, it is important to seek medical help when the first signs appear, then the chances of long-term remission increase. Pathology needs to be treated comprehensively: taking medications, following a diet, attending physiotherapy and massage sessions, and not forgetting about contraindications. In some cases, doctors may insist on surgery. By following the recommendations of a qualified doctor, the patient can avoid complications and improve the quality of life.
Appendix B: Patient Information
Is it possible to live normally while suffering from myasthenia gravis?
The answer to this question is definitely YES! Because myasthenia gravis is a disease that can be treated, and not just sympathize with a sick person. The complex of therapeutic drugs and measures currently used makes it possible to achieve stable remission of the disease and return more than 70% of patients to a normal, fulfilling life.
Myasthenia gravis is characterized by remissions that occur during basic therapy, after thymectomy, or spontaneously - without any treatment at all. Good compensation for the disease is possible with small or moderate doses of anticholinesterase drugs, which does not interfere with the work and active rest of patients.
Even in cases where patients are forced to undergo treatment with maintenance doses of glucocorticoid and immunosuppressive drugs, life does not stop for them. Families with myasthenia gravis have healthy children. A woman can carry a child herself and be sure that he will be healthy.