Astrocytoma is a malignant tumor that develops from neuroglia. These types of neoplasms originate from astrocytes, which are small star-shaped cells in the central nervous system. The main function of these cellular elements is to support nerve cells, however, with the development of pathological mutations, they can give rise to the growth of a tumor such as astrocytoma. The reasons for the development of this neoplasm remain unclear. It is assumed that factors such as hereditary predisposition, exposure to ionizing radiation, toxic chemicals and highly oncogenic viruses may play a role in the etiopathogenesis of the disease. Depending on the location, the following types of tumors are distinguished:
- cerebral astrocytoma;
- spinal cord astrocytoma;
- cerebellar astrocytoma.
Features of the histological structure allow us to distinguish the following types of astrocytoma:
- pilocytic astrocytoma (piloid astrocytoma) are highly differentiated tumors classified as neoplasms of the first degree of malignancy;
- fibrillary astrocytoma is the most common type of tumor, characterized by grade II malignancy;
- anaplastic astrocytoma – characterized by rapid growth and rapid progression of the tumor process and belongs to the group of tumors of the III degree of malignancy;
- protoplasmic astrocytoma is a rare type of tumor, characterized by a special structure of cells with processes;
- fibrillary protoplasmic astrocytoma - includes plasmatic and fibrous astrocytes;
- glioblastoma is the most aggressive variant of the tumor, characterized by grade IV malignancy.
Etiology of the disease
The exact occurrence of neoplasms has not been studied, but experts name risk groups based on statistical data. For example, it is known that oligoastrocytomas are more common in young people aged 25 to 30 years. But there are also known cases of the disease in children and the elderly.
Experts still have not reached a consensus on whether the use of mobile phones and other sources of electromagnetic radiation increases the likelihood of developing tumors. But in general, there are two main groups of reasons for the development of neoplasms.
The first is disruptions in the process of tissue formation in the fetus during intrauterine development. In medical terms, this group is called dysembryogenetic factors and this is the main cause of the development of brain tumors in children. The second is DNA errors accumulated over the course of life that interfere with the normal functioning of cells. An unhealthy lifestyle, stress, and external influences of various unfavorable factors lead to the fact that some cells of the human body begin to mutate. Once the number of mutations exceeds a certain critical threshold, a neoplasm appears in the body.
The main factors that increase the likelihood of a neoplasm are the following:
- Chemotherapy or exposure to ionizing radiation in the treatment of tumors of other locations;
- Genetic predisposition or hereditary diseases, for example, Turcotte syndrome, neurofibromatosis and more;
- Wrong diet. For example, addiction to smoked meats, canned food, fried foods and foods containing carcinogens;
- Work in hazardous industries or in difficult conditions for the body. Thus, according to statistics, representatives of such professions as doctors, firefighters, farmers, and workers of petrochemical enterprises get sick more often. Working with plastic, mercury, arsenic, rubber, and petroleum products is especially harmful;
- Presence of cancer;
- Poor environmental situation in the region of residence.
Poor nutrition is a possible cause of oligoastrocytoma.
By the way, it is believed that smoking does not have any effect on the risk of brain tumors. Although it may well contribute to the development of neoplasms in other localizations, primarily lung cancer.
Causes
The exact causes of anaplastic astrocytoma are largely unknown. Scientists have concluded that hereditary factors play a significant role. Also, a tumor in the brain can begin to form under the influence of radiation and chemicals.
Other factors that may contribute to the development of an astrocytic tumor include:
- history of traumatic brain injury;
- alcoholism, smoking, drug addiction;
- immunodeficiency states;
- congenital abnormalities in the structure of DNA.
Most often, a combination of factors leads to the occurrence of astrocytic oncopathology.
Tumor classification
According to the World Health Organization, there are now more than one hundred types of different brain tumors. They differ in the origin and genetic characteristics of the cellular mutations that have arisen. The type of mutation is identified using a special histochemical analysis. It is one of the key factors in selecting effective therapy.
There are five large groups of brain tumors: meningeal, primary lymphomas, neuroepithelial, germ cell, ependymal.
Neuroepithelial include: astrociatric, oligodendroglial, mixed. In particular, oligoastrocytoma belongs to mixed neuroepithelial neoplasms, as it is formed from astrocyte and oligocyte cells simultaneously.
In addition, tumors are divided according to the degree of malignancy, each of which has its own name. The first degree is pilocytic oligoastrocytoma, the second is fibrillary, the third is anaplastic, the fourth is glioblastoma. The fourth degree is considered the most dangerous.
Brain astrocytoma
Astrocytes are a type of neuroglial cell. They are shaped like small stars. Normally, these cells perform a number of important functions. They ensure metabolic processes in nerve fibers, regulate the volume of fluid present in cells, blood microcirculation and help eliminate waste from functional neurons.
Due to the influence of external or internal unfavorable factors, a mutation occurs in the structure of stellate cells. They begin to multiply rapidly and at the same time lose the ability to perform their functions. Gradually degenerated astrocytes form tumor formations that have an irregular shape and penetrate healthy brain tissue with their processes.
Damage to the cerebellum, white matter, optic nerves, brain stem and other parts of the brain may occur. This pathological condition can be either benign or malignant.
Depending on the structure, such neoplasms can be simple or complex. The first category includes fibrillary, gemistocytic and protoplasmic astrocytoma of the brain. Complex ones include subependymal, microcystic, cerebral and piloid astrocytoma.
Based on the degree of malignancy, tumors are divided into 4 grades. Astrocytomas can develop into extremely dangerous glioblastomas. With such an unfavorable course, the life expectancy of patients can be significantly reduced.
Symptoms of manifestation
Clinical symptoms depend more on the location and size of the tumor rather than on its type. At the initial stage, the disease may not manifest itself in any way and may not cause discomfort to the person. At this moment, the tumor is still small and can only be detected by chance.
All manifestations of the disease can be divided into two main types: those that arise due to the size of the tumor due to the fact that this increases intracranial pressure and those that appear depending on which brain centers suffer from the tumor that appears.
Most often you can observe such signs as:
- Headache;
- Nausea and vomiting;
- Epileptic seizures, convulsions;
- Failures in the symmetry of reflexes;
- Aphasia – loss of the ability to speak and even write;
- The sense of balance in space is lost;
- Nystagmus - the eyeballs begin to move involuntarily;
- Systemic dizziness;
- Personality changes. Lethargy and apathy are observed, the person loses the desire to take care of himself. But it can also be the other way around – a manifestation of excessive activity and aggression.

Headache is a symptom of oligoastrocytoma
Diagnostics
In order to select adequate therapy, a thorough diagnosis is necessary. The patient is sent for studies such as:
- MRI with contrast. This allows you to determine the size, boundaries and structure of the tumor;
- CT both with and without contrast enhancement;
- PET/CT of the brain with amino acids;
- Electroencephalography;
- Study of tumor markers.
In preparation for surgery, the patient may additionally be referred for blood tests, including biochemistry. During surgery, part of the affected tissue is taken for further histological examination.
Therapy methods
Specialists such as neurosurgeons, oncologists, and radiologists take part in the treatment. As a rule, therapy is carried out comprehensively - the tumor is removed, and then chemotherapy or radiotherapy is carried out. The proposed treatment will directly depend on the main characteristics of the tumor. Additionally, symptomatic therapy is provided.
Surgery
As a rule, benign tumors are completely removed. Malignant ones - whenever possible. In this case, the surgeon tries to remove as many affected cells as possible without damaging healthy tissue. It is often impossible to completely remove mutated cells, so additional radiation and chemotherapy are given after surgery.
Chemotherapy and radiation therapy
In radiation therapy, ionizing radiation is directed at the tumor, which is harmful not only to malignant cells, but also to healthy tissue. However, the body's cells are restored after such treatment, and the tumor slows down or disappears altogether (although rarely).
Chemotherapy is safer than ionizing radiation. Therefore, it is more often used in the treatment of children. It also negatively affects healthy cells, but increases the patient’s chances of a favorable prognosis.
Treatment
Therapy for this pathological condition depends on many factors, including the location and volume of the formation, the histological type of astrocytoma, the severity of clinical manifestations, the degree of malignancy and the age of the patient.
If the tumor does not cause severe symptomatic manifestations, doctors can take a wait-and-see approach and recommend routine examinations every 3 months.
If the tumor does not grow, surgery may not be necessary. For rapidly growing and malignant astrocytomas, therapy should be selected by an oncologist and a neurosurgeon. To improve the prognosis, complex treatment is often prescribed, including chemotherapy, radiation and surgery.
Pathology cannot be treated exclusively with folk remedies. Various medicinal herbs can be used exclusively as auxiliary methods of therapy.
Surgical intervention
The main treatment method for astrocytomas is surgical removal. The types of tumors that have clear outlines are most amenable to surgical elimination. Malignant neoplasms that do not have clear boundaries and penetrate healthy brain structures are almost impossible to completely eliminate during surgery. This increases the risk of relapse.

Approximately 3-5 hours before surgery, patients are given special medications to achieve better visualization of the tumor. Preliminary preparation of the patient is mandatory. The operation is performed under general anesthesia. A neurosurgeon performs manipulations to eliminate a tumor under an electron microscope. This allows for maximum removal of tumor tissue.
Radiation therapy
Radiation can be given either after or before surgery. This treatment method affects astrocytoma cells without damaging healthy ones. Radiation therapy can be carried out either externally or internally.
In the first case, the source of ionizing radiation is located outside the human body. This option is associated with a high risk of developing a number of pathologies resulting from the influence of radiation on healthy tissue.
The internal effect is more gentle. In this case, radioactive substances are injected directly into the tumor tissue using a catheter. This reduces the risk of developing complications in the future.
Chemotherapy
Chemotherapy for astrocytomas is used as an adjunct to radiation and surgery. These drugs are extremely toxic and at the same time have a low effect on such tumors.
Drugs used in chemotherapy for astrocytoma include:
- Lomustin.
- Carmustine.
- Vincristine.
- Temozolomide.
The use of these drugs has a toxic effect not only on tumor cells, but also on the entire body. Because of this, severe signs of intoxication occur, worsening the general condition of the patient.
Radiosurgery
Stereotactic radiosurgery is often used to treat astrocytoma. This manipulation involves exposing the affected area to a powerful stream of radiation. Radiosurgery is performed using a special “gamma knife” installation. A similar treatment method is used to eliminate malignant infiltrating formations whose size does not exceed 3.5 cm.
Complications
Brain damage does not have the best effect on future quality of life. The presence of tumors often leads to the development of complications such as:
- Deterioration of vision;
- Loss of speech clarity;
- Impaired sense of balance and functions of the musculoskeletal system;
- Loss of ability to distinguish tastes and smells.

In some cases, the patient may lose the ability to move independently. Complications may develop together or separately, or may not appear at all. It all depends on the individual characteristics of each patient.
Forecast
Brain tumors are not divided into stages like other malignant neoplasms. They have their own classification. In this case, the prognosis of patient survival is directly related to the location of the tumor and the degree of its malignancy.
In the first degree of malignancy, the growth of the tumor is slow, it does not penetrate other tissues, and the cells themselves are similar to normal ones. In the second degree, growth is still slow, but mutated cells can penetrate into neighboring tissues, and there is a risk of relapse. Neoplasms of the first and second degrees are considered benign and in this case the prognosis for the patient is favorable. But formations can mutate, acquiring a higher degree of malignancy.
The third and fourth degrees of malignancy are more dangerous. Thus, at the third stage, tumor cells are noticeably different from healthy ones; they quickly divide, which leads to significant tumor growth. In addition, these cells penetrate into neighboring tissues. In the fourth degree, cells divide extremely quickly. Nuclei of different sizes and shapes are observed in them, new vessels appear, designed to nourish the growing tumor; often such formations are accompanied by the appearance of cysts and necrosis.
The prognosis is based on the degree of malignancy and the genetic nature of the tumor. The structure of the cells in this case is less important.
Detection of the disease at an early stage and timely adequate treatment increases the chances of survival, but overgrown tumors are more difficult to fight, especially if they have a high degree of malignancy.
Epidemiology
Hemocytic astrocytomas account for approximately 10% of all WHO grade II disseminated astrocytomas. The average reported patient age at diagnosis is 40 years, the median age is 42 years, and the male to female ratio is 2:1.
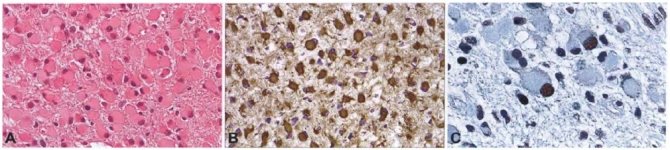
Hemocytic astrocytoma. Tumor cells have enlarged, glassy, eosinophilic cytoplasm and eccentric nuclei. B Immunostaining shows marked and persistent accumulation of GFAP in the cytoplasm of neoplastic hemocytes. Interspersed - small tumor cells with little cytoplasm; Spread is largely limited to this inconspicuous cell population. Accumulation of C p53 is present in the nuclei of small and hemocytic tumor cells.
Localization
Gemistocytic astrocytomas can develop in any region of the central nervous system, but they most often develop in the frontal and temporal lobes.
Macroscopic examination
Macroscopically, hemocytic astrocytomas do not differ significantly from other low-grade diffuse gliomas. They are often characterized by expansion of infiltrated areas of the brain without clear delineation of neoplasms. The involved areas may have a grayish discoloration, granularity, firmer or softer consistency, and microcystic change.
Microscopy
The histopathologic hallmark of gemistocytic astrocytoma is the presence of a prominent proportion of gemistocytic neoplastic astrocytes. Hemocytes should make up more than 20% of all tumor cells; The presence of random hemocytes in a diffuse astrocytoma does not justify the diagnosis of gemistocytic astrocytoma. The average proportion of gemistocytes is approximately 35%. The 20% cut-off point is somewhat arbitrary, but a useful criterion in borderline cases.
Hemestocytes are characterized by plump, glassy, eosinophilic cell bodies with an angular shape. Stout, randomly oriented processes form a rough fibrillar network. These processes are often useful for isolating tumor cells from mini-hemocytocytes found in oligodendroglioma. Hemostocytic neoplastic astrocytes consistently express GFAP in their perikarya and cellular processes. The nuclei are typically eccentric, with small, distinct nucleoli and tightly folded chromatin. Frequent perivascular lymphocytes. Electron microscopy confirms the presence of abundant compact glial filaments in the cytoplasm and cellular processes. Enlarged mitochondria were also noted.
Prevention measures
As preventive measures, we can recommend maintaining a healthy lifestyle, giving up bad habits, moderate physical activity, and frequent walks in the fresh air. Maintaining a proper diet. It is advisable to avoid products containing carcinogens. In addition, it is worth protecting the body from physical and psycho-emotional stress, observing sleep and wakefulness. Refuse to work in hazardous industries and not live in regions with unfavorable environmental conditions.
Compliance with all these measures is not 100% protection against the appearance of tumors, but it will reduce the risk of their occurrence and will also have a beneficial effect on your overall health.