Parkinson's syndrome significantly shortens life expectancy. Ten years from the moment of manifestation, about 65% of patients die or become disabled, and after fifteen years this number increases to 80%. In the absence of a rehabilitation and treatment program, the mortality rate among Parkinson's patients is three times higher than the mortality rate in the population.
Development of the disease
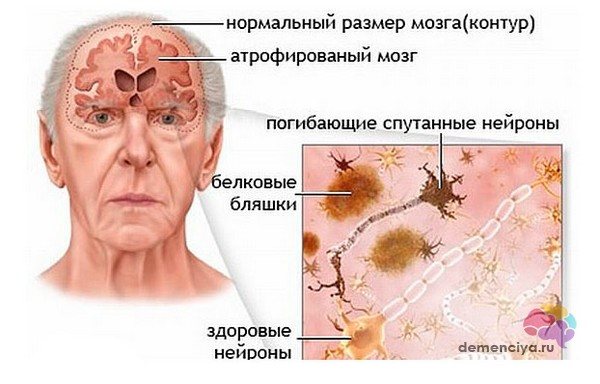
Parkinson's pathogenesis develops over years. Neurons are being destroyed in the anterior sections of the substantia nigra. The first changes appear when 60-80% of nerve cells die in this zone.
| Stages of pathogenesis | Changes in functional anatomy and cell physiology |
| First phase | The cells of the anterior sections of the substantia nigra die, alpha-synuclein accumulates in the cytoplasm, microglia are activated, and astrocytes die. |
| Second phase | The functioning of neurons is disrupted. Therefore, the connection between neurons of the basal ganglia and peripheral cells suffers. Due to this, the normal functioning of agonist and antagonist muscles is disrupted. |
| Third phase | Degenerative changes lead to atrophic changes in the muscles, the formation of joint immobility, and problems with maintaining balance. These changes paralyze the patient. |
Symptoms
Knowing the first signs of the disease can help in early diagnosis and treatment, which increases the chances of recovery and life expectancy.
In the table we consider the main symptoms and the nature of their occurrence: Clinical picture of Parkinson’s disease
| Sign | Characteristic |
| Tremor (shaking) | Occurs in the limbs, lower jaw, eyelids, and head. Manifests itself in the form of uncontrollable trembling, which is explained by excessive contraction of muscle tissue |
| Rigidity | A decrease in dopamine leads to a lack of inhibition of muscle contractions, which leads to tone. As a result, the muscles become hard and lose elasticity and mobility. Feels like stiffness of movement |
| Hypokinesia | Disturbances in the structure of the basal ganglia lead to a decrease in motor activity. Actions will be performed slowly and with difficulty |
| Bradyphrenia | Decreased thought processes, slow and quiet speech. Occurs due to damage to nerve cells and lack of dopamine |
| Unsteady movements | Destruction of the basal ganglia leads to difficulty maintaining balance, as a result of which gait is disrupted: steps become short and slow |
| Mental disorders | The development of the disease leads to a decrease in mental abilities, disturbances of consciousness, insomnia, depression, and general weakness |
Patients with Parkinson's disease are restricted in their movements. A typical picture of the appearance of such a person is: the arms are bent at the elbows and pressed to the body, the body is slightly bent and the weight is shifted forward, the head is slightly elongated. Periodic trembling of the limbs is noticeable, the face is calm and does not express any emotions.
Hen-Yar classification

English doctors Margaret Hen and Melvin Yahr developed a classification of Parkinson's disease in the mid-20th century. It is still used in clinical practice today. After all, the stages are described in detail. They help the treating doctor navigate the prescription of therapy. In addition, the Hoehn-Yahr scale accurately describes the patient's signs of disability. This means that in the final stages a person needs help and cannot care for himself.
Important! The classification has been slightly modified. Later, stages 0, 1.5 and 2.5 were added to it.
Classification criteria
- Presence of symptoms of Parkinson's disease;
- Manifestation of the clinic on one side or both sides. Is the torso involved?
- Presence of postural instability;
- Ability to overcome inertia of movement;
- Self-care ability;
- Ability to stand and walk with assistance.
Quality of life cannot be assessed using the Hen-Yar classification. There is a Unified Rating Scale (UPDRS) for this purpose. It covers a wide range of criteria from sleep disorders to speech problems and depression. However, general practitioners and neurologists rarely use it. After all, such testing is labor-intensive and requires special training of a specialist.
Hen-Yar scale
| Stage | Manifestations |
| Zero | There is no clinic. At the same time, processes of neurodegeneration may already be actively occurring in the brain. |
| First | There is a clinic on one of the limbs. |
| Stage 1.5 | There are symptoms on the trunk and limbs. |
| Second | Bilateral body involvement. |
| Stage 2.5 | In addition to symmetrical symptoms, postural instability appears. But the ability to overcome the inertia of movement remains. |
| Third | Pronounced clinical picture of the disease. But the patient takes care of himself. |
| Fourth | Need help at home. The ability to walk and stand without support remains. |
| Fifth | Severe disability. Inability to walk or stand up. |
Late stage Parkinson's disease and dementia
Good evening, Zoya. Sorry for the delay in answering, I was working... Yes, everything is on my intuition... EVERYTHING!!! I came gradually to our menu. No fresh berries, nothing from greens (except for dill in the soup), all the food was overcooked , frayed. All my attempts to somehow improve the menu, to diversify it with vitamins ended with either constipation or diarrhea. I consulted with a gastroenologist once, she told me, you managed to stabilize your mother, you left the constant enemas, so stick with it. All the vitamins come out anyway of them, nothing is digested, they only irritate their intestines and their already weak digestion. I can write to you what I feed my mother. The menu is always the same. I only change soups, yogurts, and juices. Or rather, I even buy weak juices and spoil them water (apple, multivitamins, grape, I don’t take others). Breakfast is grated cottage cheese, seasoned with yogurt - half a bowl, kefir or a drink made from kefir (all sorts of berry flavors are sold). Lunch is soup, with a piece of black bread crumbled into it, ground in a blender. Any soup, with the exception of pickle soup, kharcho, etc., spicy soups, a full bowl, diluted juice. Afternoon snack, dessert yogurt, dessert cottage cheese, any milk dessert that you have in stores, activity, for example. Drink tea or yogurt, or fruit drink (diluted). Dinner is oatmeal porridge. I buy Nordic. When the nurse is working, I buy disposable packs, dilute with water and milk and microwave, 1 minute and ready, with various dried fruits. Add a spoonful of butter, almost full bowl, let's do it thinner, not with milk alone, because whatever makes it strong, dilute it with 2/3 water, 1/3 milk. Drink tea. Between feedings, be sure to give clean plain water to drink, an hour after feeding a cup of water. This is a must, if she doesn’t drink it all, then in half an hour more. To at least somehow support her desiccated body. This is our menu. I don’t give jelly to my mother, it strengthens her. Jelly too, I used to give it to her and my mother liked them , alas...now she doesn’t swallow the jelly...holds it in her mouth, doesn’t understand what needs to be swallowed...then it all pours out. Now it’s hot here, sometimes I give my mom ice cream...))) the only thing I can do to please her...but only ice cream .Slightly melted, she likes it. Also, Zoya, I started buying protein mixtures again, I put a spoonful of the mixture everywhere, it’s pure protein, to support my mother’s strength. They are tasteless, so they’re very convenient. How are you doing? Write. To everyone envious of your mother, her condition, weight, housing and communal services.
How does the disease manifest itself?
The early stages are the hardest to recognize. Clinic zero is not expressed. The development of neurodegeneration can only be indicated by diagnostic studies of the brain. And the first symptoms (tremor or spasm) are often mistaken for a variant of the “senile norm”. In any case, you need to be attentive to your loved ones and consult a doctor in a timely manner. The earlier treatment is started, the slower the disease progresses.
Zero stage
It is known that the first changes characteristic of Parkinson’s begin to occur in the patient’s brain at the age of 50-65. However, the patient has no idea about them. After all, the etiological factor of the disease has not been established. And the clinic appears when more than half of the neurons die. But if a person without symptoms has changes in the anterior part of the substantia nigra, then the likelihood of illness in the future is high. However, to set the zero stage, a more thorough and in-depth examination should be performed.

First stage
It also goes unnoticed. Patients with the trembling form develop tremors at this stage. In this case, the disease is easier to diagnose. Trembling occurs at rest and affects only one part of the body (head, finger, arm, hand, leg). Other clinical signs may occur.
- Decreased sense of smell;
- Depression and other mood disorders;
- Insomnia;
- Decreased resistance to physical activity;
- Problems with potency.
Stage 1.5
New symptoms progress slowly and unnoticeably. However, the patient may indicate the following manifestations of the disease:
- Tremor from one area spreads to the entire limb. For example, if a finger trembles, the tremor spreads to the hand or arm;
- Rigidity or stiffness of the muscles appears. Patients are especially concerned about the back and neck muscles;
- In women, the manifestations of the disease at this stage look like cervical osteochondrosis.
Stage 2
- Symmetrical lesion on both sides;
- Tremor of the lips, lower jaw, tongue, head;
- Increased salivation;
- Bradykinesia develops. Habitual actions take more time;
- Walking pace slows down;
- Amymia appears. The face stops displaying emotions;
- There are problems with sweating;
- The skin becomes dry. They require constant hydration.
Stage 2.5
At this stage, postural instability develops. This is the inability to maintain an upright body position in certain situations. The patient loses stability when walking with turns. During this period, it is still possible to independently overcome the inertia of rest or the inertia of movement.
Patients often develop an inability to begin walking or, once started, to recover in time. Sometimes the patient begins to move as if the torso is ahead of the legs. This often leads to loss of stability and falls.
Third stage
It is characterized by impaired postural stability and further progression of syndromes. The following clinical signs are available:
- Muscle stiffness;
- Spastic muscle tone;
- The “gear wheel” symptom is formed;
- "Doll walk" This clinical sign is characterized by small mincing steps;
- Clumsiness. Muscle spasm makes movements awkward and gait unsteady;
- Sudden loss of facial expressions;
- Petitioner pose;
- Muffled speech.
At the same time, you still have the opportunity to take care of yourself. Some patients even retain work skills if they do not involve physical labor.
The third stage is characterized by retropulsion. The doctor and assistant stand on either side of the patient. The doctor pushes the man in the chest. At the same time, he loses stability. Then the test is repeated with a push in the back.
Fourth stage
- Tremor progresses in this phase. He worries the patient constantly. It significantly disrupts his life and makes self-care difficult;
- The patient's quiet, nasal voice appears. The speech does not have a pronounced emotional coloring. The clarity of pronunciation of phrases is lost;
- Muscular rigidity significantly impairs patient care. Stiffness prevents you from performing your usual everyday activities;
- Difficulty getting out of bed on your own;
- When walking, falls often occur and cause serious injury.
Fifth stage
The terminal stage of the disease, in which the patient requires constant care.
- The patient does not move independently. In the early stages, movements are possible only within the bed;
- To move, a wheelchair is used or the patient moves with the support of relatives;
- Swallowing is impaired, making it difficult to eat independently;
- Disturbance in urination.
Acute decompensation
This is a reversible, serious condition that develops in patients with Parkinson's disease. Causes of acute decompensation:
- Complication of dopaminergic therapy;
- Exacerbation of somatic pathology;
- Injuries;
- Psychogenic disorders.
Clinical picture of decompensation:
- Development of dyskinesias;
- Increased tremor, despite adequate therapy;
- Lack of effect from taking levadopa;
- Increased body temperature (without pronounced inflammatory changes in the main organs and tissues);
- Severe muscle rigidity with complete impairment of mobility;
- Loss of speech;
- Impaired consciousness up to stupor and coma.
With such clinical manifestations, the patient should be urgently hospitalized in the intensive care unit. Against the background of decompensation, breathing and swallowing disorders rapidly progress.
Survival time and mortality in Parkinson's
The prognosis for life with Parkinson's disease is unfavorable. PD relatively quickly leads to permanent disability. After 10-20 years, about 40-75% of patients die from the onset of the disease, and half of the survivors require constant outside help.
Death in Parkinson's often occurs from concomitant diseases - coronary heart disease, pneumonia, cerebral circulatory disorders, thrombosis, etc.
The highest risk of death is observed in patients with parkinsonism plus multiple system atrophy syndrome. In second place is mortality in patients with dementia with Lewy bodies, and in third place is parkinsonism as a symptom of another neurodegenerative disease (including Alzheimer's disease).
Features of the course of the disease in different groups

| Average age of onset of symptoms after 60 years | Average age of onset of symptoms after 45 years | |
| Duration of illness | About 10 years | More than 15 years |
| Severity of clinical symptoms | Rapid progression, large number of patients with stages above 2.5 | Slow course of the disease with adequate therapy, a large number of patients with mild stages |
| Levadopa dosage | Large doses are required to correct the disorder | Levadopa is not prescribed for initial therapy, only in severe cases |
| Side effects from treatment | Often expressed | Occurs in the treatment of resistant forms |
| Severity of motor and psychoemotional disorders | Movement disorders are more pronounced in this group; decompensations occur, requiring psychiatric help. | Emotional disturbances are expressed, the help of a psychotherapist is required |
Course of Parkinson's disease: men and women
| Men | Women |
| Frequency of occurrence | Get sick 2 times more often |
| Mortality rate | Women have higher |
| Progression of symptoms | Progresses faster |
| Difference in clinical signs: | |
| "Begging Pose" | More often in men |
| Depression | More often in women |
| Cognitive decline | More often in men |
| Depression, anxiety | More often in women |
Characteristic
Parkinson's disease is a degenerative disorder of the central nervous system, primarily affecting the functioning of the musculoskeletal system. It mainly occurs in old age (after 70–80 years), but there are also cases of the disease developing after 40 years. Statistics show that every 500 people on the planet suffer from this disease.

Many people consider Parkinson's and Alzheimer's diseases to be similar. In both cases, the central nervous system is affected to one degree or another, but the mechanism of development itself is very different. Alzheimer's disease is characterized by cognitive impairment, while Parkinson's disease primarily affects the musculoskeletal system.
Life expectancy by stage
| Stage | Lifespan | What to do to prolong life? |
| First stage | Symptoms are minimal, so life expectancy is difficult to predict. It will be equal to a healthy person from the population. Without treatment, the transition to progression occurs after 3 years. | Early diagnosis and treatment of the disease, giving up bad habits and following a sleep and rest schedule will allow you to stay in the first stage longer. |
| Second stage | Symptoms are progressive. This is the time for clinical diagnosis and initiation of therapy. Without it, the patient will progress to loss of self-care after 3 years. With adequate therapy, symptoms progress slowly. The patient may linger at this stage for a decade. | Control of therapy, competent selection of drugs, treatment of concomitant diseases, maintaining a healthy lifestyle |
| Third stage | Requires assistance from an outsider to perform complex actions. He copes with everyday tasks independently, but there are limitations. Progression over 15 years with adequate therapy and constant care. | Compliance with doctor’s recommendations, selection of medication dosage, regular social activity, monitoring of somatic pathology. |
| Fourth stage | Irreversible changes lead the patient to complete dependence on outside help. With proper care, the stage lasts 2-5 years. | Patient care, drug control. |
| Fifth stage | On average it lasts about a year. | Care, prevention of bedsores and congestive pneumonia |
The influence of therapy and rehabilitation on the prognosis of Parkinson's
Without any treatment, a Parkinson's patient becomes disabled on average after 10 years. Patients who adhere to pharmacotherapy retain social and everyday skills and physical activity much longer. A well-designed rehabilitation program allows 90% of such patients to live more than 15 years from the onset of Parkinson’s without any outside help. Great importance is attached to psychotherapy, which allows you to correctly configure the patient for treatment, thereby reducing the severity of psychotic symptoms and cognitive disorders, which, in turn, helps to slow down the course of the disease. Physiotherapy and exercise therapy improve the patient’s quality of life and have a favorable effect on the overall prognosis.

Modern medicine can improve the prognosis even if the disease is resistant to therapy. For this purpose, surgery with electrical stimulation of the brain is used. Special electrodes are implanted into the brain, the generator from which is implanted next to the collarbone. Thanks to regular stimulation of neurons, the severity of the clinic decreases. The settings are adjusted depending on the patient's condition.
Important! Such surgery is associated with risks (stroke, infection, blood clots). Therefore, before the operation, you should weigh the pros and cons, conduct a full examination of the patient and warn him about the possible consequences.
Therapeutic approaches at different stages
| Early stages From 0 to 2.5 | Late stages 3 to 5 | |
| Approach to therapy for young people | Monotherapy (amantadines, anticholinergics, dopamine receptor agonists (DRA)) | Combination therapy (levadopa + amantadines, anticholinergics, ADR) |
| Therapy for the Elderly | Minimum effective doses of levadopa (amantadines, anticholinergics with caution) | Levadopa + dyskinesia correctors (clonazepam, muscle relaxants) + therapy for mental disorders (olanzapine) + combating orthostatic hypotension (midodrine, glucocorticosteroids) |
| Diet | Balanced diet, no alcohol, moderate protein intake | Low Protein Diet |
| Non-drug methods | Exercise therapy complex daily, sports, dancing, oriental gymnastics | Exercise therapy, application of biological feedback methods using a stabilogram |
| Surgery | Used in young patients. Functional neurosurgery methods are used: stereotactic destruction of individual zones, deep brain stimulation. At the development stage, intracerebral implantation of embryonic dopamine-producing stem cells. |
Patient care
At the fourth and fifth stages, the patient loses the ability to care for himself. He requires daily care and help at home. It can be provided by relatives or a caregiver.

- Prevention of bedsores. For this, positioning or a special anti-decubitus system is used. In the first case, the patient needs to be turned frequently, ensuring a comfortable position. In the second case, an automatic mattress is used, which deflates and inflates independently. Hygiene procedures are carried out daily, the skin is moisturized with cream. A medicinal ointment is applied to diaper rash and maceration;
- Breathing exercises. Carried out to prevent congestive pneumonia;
- Stimulation of independent activity (minimum maintenance while maintaining skills);
- Daily exercise therapy complex (in active and passive mode);
- Monitoring medication intake (for older people, transdermal options, a patch on the skin may be suitable);
- Psychological support (joint conversation, talking about new events, memories, viewing photos and videos).
Parkinson's disease is a progressive disease. It inevitably moves from stage to stage. And medicine cannot prevent it. However, it takes courage and patience to slow down the progression of the disease.











