In recent decades, Parkinson's disease has become an increasingly common diagnosis. Increasingly, a severe neurological incurable verdict is given to fairly young people. The advantage of modern therapy is the successful treatment of Parkinson's disease. With the correct selection of drugs and methods, most patients have the opportunity to maintain the usual lifestyle of a practically healthy person for many years.
Causes of Parkinson's disease
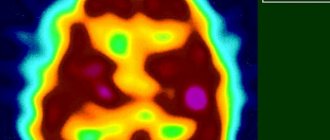
As with most neurological diagnoses, the causes of Parkinson’s disease are currently unknown to specialists. It has been established that the basis for the occurrence of disorders is the occurrence of changes occurring in the so-called substantia nigra of the brain.
The main task of this area is the production of a special chemical, dopamine, whose task is to conduct a signal that must pass between the substantia nigra and the striatum. Violation of the conductivity of this signal leads to impaired coordination of movements. The trigger for the appearance of violations is considered to be:
- hereditary predisposition;
- a lot of stress;
- damage to the meninges due to poisoning due to the release of internal toxins from the liver;
- elevated cholesterol levels, which can provoke sclerotic changes;
- cerebral circulatory disorders, provoking degenerative processes;
- inflammation caused by a viral or bacterial infection, encephalitis;
- damage to the substantia nigra by high doses of free radicals and other causes;
- tumor processes in the brain, severe head injuries;
- natural aging of the body, during which neurons die.
Most patients experience a combination of several provoking factors. At the same time, even the full complex of presence of all these causes does not always lead to the onset of a severe and incurable neurological disease.
At a young age, the main cause is congenital predisposition. The onset of the disease in middle and old age is associated in most cases with the influence of external influences on the body.
The exact reasons are unknown. Over the years of struggle with this terrible diagnosis, effective methods of treating Parkinson's disease have been developed.
Vascular parkinsonism
However, it should be noted that these clinical differences between vascular parkinsonism
and
Parkinson's disease
are not absolute. Thus, in pathomorphologically confirmed PD, a poor response to levodopa was detected in 6% of cases, absence of rest tremor in 23%, symmetrical onset in 29%, 10-20% of patients develop gait disturbances and postural instability with frequent falls relatively early ( Hudhes AJ et al., 1992).
On the other hand, RW Murrow et al. (1990) presented a case of pathomorphologically confirmed vascular parkinsonism
, which was caused by multiple lacunar infarcts in the basal ganglia and substantia nigra and ideally imitated all the clinical features of PD: the patient had a long-term slowly progressive course, unilateral onset, rest tremor, a good response to levodopa drugs and no strokes (although there was long-term arterial hypertension).
Other cases of morphologically confirmed vascular parkinsonism
with a good response to levodopa, the presence of rest tremor or hemiparkinsonism. Thus, despite the fact that the phenomenology of neurological disorders in SP has certain features, the symptoms of SP and PD partially overlap, and it is sometimes difficult to differentiate the two diseases in a particular patient.
Associated neurological syndromes. Among the neurological syndromes that often accompany vascular parkinsonism
, but not characteristic
of Parkinson's disease
, pyramidal syndrome and cerebellar ataxia can be attributed. Pyramid signs (bilateral, but usually asymmetrical revival of tendon reflexes, mainly from the lower extremities in combination with clonus of the feet or pathological foot signs, less often spasticity) are observed in 60-70% of patients and, as a rule, are moderate.
Signs of cerebellar ataxia are observed relatively rarely - in 5-15% of patients with vascular parkinsonism
, however, they can be difficult to identify against the background of severe postural instability.
Some syndromes are possible in both diseases, but develop in vascular parkinsonism
more often and at an earlier stage than in
Parkinson's disease
. These include pseudobulbar syndrome, observed in 75% of patients with SP, dementia (50%), and pelvic disorders (40%).
The presence of some of the above concomitant neurological syndromes excludes Parkinson's disease
, but does not always allow one to differentiate
vascular parkinsonism
from other neurodegenerative diseases, primarily those belonging to the parkinsonism-plus group. Thus, the combination of parkinsonism with cerebellar and moderate pyramidal syndrome is possible with multiple system atrophy, and the combination of parkinsonism with rapidly increasing postural instability, severe pseudobulbar syndrome and dementia is possible with progressive supranuclear palsy.
Features of the course of vascular parkinsonism.
Course of vascular parkinsonism
much more variable than in Parkinson's disease.
The disease usually begins after 60 years of age. The average age of patients with vascular parkinsonism
is usually higher than that of patients with PD, which indicates a later onset of the disease. However, SP is not so rare at a young age; most often it occurs in the presence of severe arterial hypertension.
The onset can be acute, but more often it is subacute or chronic. Sometimes the development of vascular parkinsonism
is preceded by one or more strokes, while extrapyramidal symptoms can develop in the acute period or several months after the stroke, sometimes against the background of regression of pyramidal or cerebellar disorders that have the ability to “mask” parkinsonian symptoms. A variant of delayed development of parkinsonism after hemorrhage in the midbrain has been described, which may indicate the role of secondary de- or reinnervation changes in the basal ganglia.
The subsequent course is continuously progressive, stationary and regressive. Most typical for vascular parkinsonism
two variants of the course: 1) acute or subacute onset followed by stabilization and (or) partial regression of symptoms; 2) progressive step-like (fluctuating) course (with alternating periods of progression, stabilization and partial regression). A steadily progressive course is also possible, and in this case, progression in SP usually occurs faster than in PD.
Gradual or step-like development of motor disorders in a significant proportion of patients with lesions of the basal ganglia
and adjacent white matter is explained by the distributed (delocalized) nature of the cortical-subcortical systems. At the same time, limited lesions in the “silent” areas of the brain remain asymptomatic, and only as they cumulate—increasing the volume of the affected tissue—do corresponding clinical manifestations arise. Normalization of blood pressure may be accompanied by stabilization and reversal of symptoms.
According to CMChang et al. (1992), the course also depends on the morphological substrate of vascular parkinsonism
: spontaneous improvement is more often observed in lacunar status; with frontal lobe infarctions, the severity of symptoms does not change, whereas with diffuse damage to the white matter, steady progression is more typical. Similar conclusions were reached by JCZijlmans et al. (1995), who identified two types of SP: one of them was characterized by an acute onset and damage to the subcortical nuclei (striatum, pallidum, thalamus), the other was characterized by a gradual onset and diffuse damage to the white matter in watershed zones.
– Return to section table of contents “
neurology"
Parkinson's disease - what is it?
When the substantia nigra of the brain is damaged and signal conduction is disrupted, degenerative disorders begin to occur in the central nervous system. The progression of the disease is very slow. Often, only a highly qualified neurologist can diagnose the initial stage for decades. The symptoms of the disease were first described in 1877 by the doctor D. Parkinson, who called the disease “continuous paralysis.” This name is associated with the main manifestation options:
- trembling of the limbs starting from the fingertips;
- slowness of movements;
- muscle rigidity.
The manifestation is associated with the onset of disturbances in the production of dopamine. Deprived of this chemical, areas of the brain gradually begin to die. The ability to conduct nerve impulses is impaired. This provokes the appearance of tremor in the early stages. Over the years, rigidity develops, leading to impaired ability to move independently.
Pathogenesis
The pathogenesis of neuroleptic parkinsonism is not entirely clear, but appears to be associated with blockade of dopamine D2 receptors in the nigrostriatal system of the brain by antipsychotics, inhibition of dopaminergic transmission and changes in the sensitivity of dopamine receptors. Neurochemical imbalance in neuroleptic parkinsonism is manifested by increased activity of the cholinergic, serotonergic systems, as well as increased activity of glutamatergic subthalamic neurons, leading to increased release of glutamate and activation of oxidative stress, which is one of the main factors contributing to damage to basal ganglia neurons. Due to their lipophilicity, neuroleptics are able to integrate into cell membranes and disrupt the energy metabolism of neurons [1].
However, often a delayed neuroleptic side effect indicates that it is not due solely to direct blockade of D2 receptors. According to research, when postsynaptic D2 receptors are blocked, dopaminergic neurons of the substantia nigra, as well as neurons of the ventral part of the midbrain tegmentum, gradually stop discharging over several weeks due to a depolarization block, which coincides with the development of parkinsonism [1].
A hidden degenerative process affecting the substantia nigra may also predispose some patients to the development of drug-induced parkinsonism. In such patients, even after complete withdrawal of antipsychotics, symptoms may subsequently progress. Neuroleptics are able to inhibit the activity of complex I of the electron transport chain of mitochondria and thereby, increasing oxidative stress, possibly “spur” the development of the degenerative process. However, we cannot exclude the possibility of so-called “late parkinsonism” - an analogue of tardive dyskinesia, which occurs as a result of irreversible damage (under the influence of neuroleptics) to neurons of the substantia nigra.[6]
Parkinsonism and Parkinson's disease, differences
These two CNS lesions are often mistakenly considered to be the same diagnosis. Actual parkinsonism refers to a wide range of neurological disorders. Including Parkinson's disease itself and secondary parkinsonism caused by mechanical or other brain damage.
However, only Parkinson's disease itself is incurable. Parkinsonism associated with brain lesions can be cured when the triggering factors are eliminated.
The neurologist's task is to determine an accurate diagnosis. Depending on the exact setting, the course of therapy is determined. These two diagnoses have different treatment options.
Parkinson's disease:
- more common in patients over 50 years of age; after 70 years of age, the primary diagnosis is observed in almost every person;
- tremor on both limbs is not symmetrical;
- speech impairment occurs, coordination of movements is impaired;
- symptoms develop very slowly.
Secondary parkinsonism:
- in the presence of provoking brain damage, it is diagnosed at any age;
- often accompanies brain injuries;
- characterized by an acute onset;
- manifestations are symmetrical;
- the clinical picture is more pronounced in the lower extremities;
- there are vegetative disorders;
- we will cure.
Secondary parkinsonism is a concomitant complication of taking many psychotropic drugs. Especially taken in unlimited quantities and without a doctor’s prescription. In drug-induced parkinsonism, tremor and rigidity manifest themselves especially strongly and acutely. Most often occurs in older women. Parkinson's disease mostly affects men.
How to treat drug-induced parkinsonism?
Drug-induced parkinsonism is a neurological syndrome. It is characterized by the manifestation of certain symptoms. This condition develops while taking certain medications.
Information about the disease
Parkinsonism caused by certain medications is a common disease. Drug-induced parkinsonism is considered a secondary form of this disease. It occurs quite often: in almost 10% of all cases of disease.
The disease is recorded mainly in elderly people. Most often, the disease is associated with taking antipsychotics. Therefore, parkinsonism is the most common diagnosis among patients in psychiatric clinics, where the treatment algorithm includes taking antipsychotics.
Neuroleptic extrapyramidal disorders were noticed as early as 1952. At that time there was no definitive data regarding this condition. The assumption of a relationship between neuroleptics and parkinsonism was made much later. When the fact was confirmed, many experts began to think about the effectiveness and safety of treatment with certain groups of drugs.
In 50% of cases, drug-induced parkinsonism is not associated with the use of antipsychotics. Other groups of medications can affect the condition, in particular:
- means that help reduce dopamine metabolism;
- centrally acting sympatholytics;
- serotonergic agents.
All of them influence the human condition in a certain way. Parkinsonism is a serious disease, unfortunately, it is irreversible.
Return to zmistCauses of drug-induced parkinsonism
As mentioned above, in most cases the disease occurs due to the use of antipsychotics. The dosage form of the disease develops against the background of the use of potent drugs. Their main action is aimed at weakening anticholinergic activity and reducing affinity for serotonin receptors.
There have also been cases where the disease developed through the use of mild antipsychotics.
Most often, the disease is observed in people over 40 years of age. Men suffer from parkinsonism much less often than women. The main symptoms of the disease may manifest themselves within 12 days after starting treatment with antipsychotics. Symptoms are especially pronounced with a sharp increase in dose.
The main symptoms are the following:
- hypokinesia;
- tension and stiffness in the muscles;
- pronounced tremor;
- instability – a person is unable to maintain balance and has difficulty moving.
In addition to the signs described above, the development of cognitive impairment is possible.
They manifest themselves in decreased memory, attention and performance.
In extremely severe cases, a person is unable to speak, and severe impairments in the functionality of the speech apparatus are recorded.
Cases of parkinsonism also occurred after taking tricyclic antidepressants. Such patients experienced severe tremors, intermittent and rhythmic movements. In general, the symptoms are similar to ordinary parkinsonism, which does not occur as a result of taking medications.
Return to zmystPrinciples of treatment of parkinsonism
Each case of disease manifestation is unique. The clinical picture can be varied, and the disease appears for various reasons. As a result, difficulties arise both with the diagnosis of parkinsonism and with its treatment.
In 36% of cases, special antiparkinsonian drugs are prescribed. However, it is more advisable to stop taking the medication that provoked the disease, since cases have been recorded when people returned to their normal lives.
A distinctive feature of drug-induced parkinsonism is the possibility of regression. This happens within a few weeks after stopping the drug. But in some cases the process may take longer. It is affected by the duration of taking medications that provoked parkinsonism.
All this indicates that in order to normalize the patient’s general condition it is necessary to discontinue the provoking drug. It can be replaced with a drug with less detectable side effects. It is important that the drug does not have a pronounced effect on the patient’s brain.
Treatment of some diseases requires the use of antiparkinsonian drugs, in particular, this is necessary for the treatment of movement disorders. The most commonly prescribed medication is Levodopa. However, recently it has not been used due to the high risk of developing hallucinations and delusional disorders. In this regard, anticholinergics and amantadine are used.
The best treatment for parkinsonism is prevention. It is necessary to abandon provoking drugs and strictly monitor the prescribed doses.
Symptoms and signs of Parkinson's disease
A severe neurological disorder is detected when the following symptoms are present:
When walking, a person loses the ability to successfully maintain balance, walking itself becomes difficult due to impaired ability to move;
- the level of muscle tone (rigidity) increases;
- frequent constipation occurs;
- one of the reasons to be tested for Parkinson's disease is a violation of the sense of smell;
- due to hypokinesia, muscle activity decreases;
- tremor (shaking) is clearly visible;
- mental and vegetative disorders appear.
In the initial stages, the disease can be identified by impaired facial expressions, movements become inhibited. Next, the patient himself draws attention to the appearance of difficulty with certain movements. At first, it is difficult to perform fine movements, and there is a problem with overcoming obstacles while moving. As brain damage progresses, the changes progress. Handwriting changes. Problems arise with performing hygiene procedures. Such as brushing your teeth, combing your hair, shaving.
Over the years, as it progresses, facial expressions completely disappear. The face becomes mask-like. Speech is noticeably impaired, it becomes difficult for the patient to chew food, retain saliva in the mouth, and drooling begins.
In young people
Parkinson's disease can appear at a young age. An example is the actor who played the main role in the once cult film “Back to the Future” Michael J. Fox. His pathology started at the age of thirty. Boxer Muhammad Ali developed Parkinson's disease in his early years. The disease also occurs in children.
Doctors believe that the onset of a complex neurological disease in young years is associated with a combination of family history and provoking external factors. These can be head injuries, acute and chronic diseases of the central nervous system. The cause of accelerated decline of the central nervous system is encephalitis. Poisoning with manganese or carbon monoxide also leads to the onset of the disease.
Separately, it is worth paying attention to the provocation of the start due to the abuse of narcotic substances, alcohol, tobacco, which provoke the death of neurons.
In young years, Parkinson's disease progresses especially slowly and has a milder course for a long period. Accurate diagnosis is often made only after typical late-stage symptoms have appeared. The patient’s gait acquires characteristic features: the arms are pressed at the elbows to the body, the spinal column is curved back, forming a “suppliant pose.” An inadequate facial reaction appears. It becomes difficult for the patient to perform many physical activities.
In the treatment of young patients, anticholinergic drugs are effective, but due to the presence of concomitant diseases, they are not prescribed in older patients. Levodopa may be prescribed in the early stages of the disease. Additionally, psychotherapy courses are provided. This helps patients accept the diagnosis and learn to live with it. Young patients are prescribed surgical treatment, which is dangerous in older age due to the presence of concomitant diagnoses.
Among women
This neurological disease is one of the few that are less common in women than in men. In the case of women with the disease, the remoral-dominant phenotype predominates. Motor symptoms appear later.
As the diagnosis progresses, women lose the ability to recognize other people's emotions such as surprise and anger. Men stop recognizing fear first. Representatives of the fair sex also:
- are more likely to become depressed and require treatment with antidepressants;
- note dissatisfaction with the quality of life;
- begin to suffer from urinary incontinence.
Timely diagnosis helps to develop an effective treatment option that prolongs the development of symptoms for a long time.
In men
Men suffer from this diagnosis more often. Among the first signs are insomnia and depression. There are problems when swallowing. To a greater extent than in women, rigidity and lack of coordination are observed. When rising from a lying position, a drop in pressure is noted.
In the elderly
Primary Parkinson's disease affects almost every person who has reached 70-75 years of age. The disease develops due to age-related death of neurons in the brain. Therapy for older patients is complicated by the presence of numerous concomitant diagnoses. Due to this, it is not possible to prescribe many drugs. Including one of the most effective - Levodopa. In the older age group, this drug is prescribed with caution, as it requires a constant increase in dosage. Cancellation leads to a sharp deterioration in health.
In elderly patients, mental and vegetative-vascular disorders begin more quickly. The patient becomes demanding and capricious, the sense of smell and taste is impaired.
Similar ailments
What else is Parkinson's disease different from? Other diseases similar to Parkinson's disease also require a diagnostic search from a doctor:
- Essential tremor . Similar to the trembling form, but the tremor is often bilateral from the first days of symptoms, involves the head and vocal cords, there is no impoverishment of movements and no effect from levodopa. Essential tremor proceeds more favorably and does not lead to significant limitations in the patient’s life for a long time.
- Dementia with Lewy bodies. A distinctive feature is the predominance of signs of dementia in the presence of movement disorders. Visual hallucinations and early depression may appear.
- Multiple system atrophy. It is characterized by severe motor and autonomic disorders in the absence of mental disorders.
- Hepatolenticular degeneration or Wilson-Konovalov disease , in which copper accumulates in the brain, liver and cornea. Because of this, patients can see a pigment ring on the cornea (Kayser-Fleischer), increased copper in blood and urine tests, and decreased blood ceruloplasmin.
If symptoms similar to parkinsonism appear, do not rush to diagnose and treat yourself.
Contact a neurologist who will help you distinguish Parkinson's disease as an independent nosological entity from secondary parkinsonism syndrome and other neurological pathologies.
The importance of this is explained by differences in the treatment of diseases and in the prognosis for the patient.
Differences between Parkinson's disease and parkinsonism:
Diagnostics
Early diagnosis of Parkinson's disease helps to identify the pathology at the earliest stages. Preventive tests and checks are recommended for people whose family history includes a large number of cases of neurological diseases. In medical practice this is called a neurological history.”
Early diagnosis will save the patient from contacting a specialist only at the stage of pronounced external disorders. Additional examinations at a later stage are no longer required.
The list of early diagnosis options includes:
- carrying out an inspection;
- performing an olfactory test, a violation of the sense of smell becomes one of the first pronounced manifestations;
- migraines;
- During a personal conversation, the doctor clarifies the quality of sleep and the level of irritability.
Tests are unable to detect the presence of this neurological disorder. In the situation of a neurological history in the family, it is necessary to carefully monitor the presence or absence of the first manifestations in the form of minimal tremor and pain between the shoulder blades.
Confirmation of the diagnosis is carried out using CT or MRI. Often, it is precisely such studies, for example, after a head injury or when examining the maxillary sinuses, that make it possible to determine pathological disorders even before the first external manifestations.
Stages of development of Parkinson's disease
Insomnia, unreasonable fatigue, constipation, and impaired sense of smell may be suspected signs of the potential development of Parkinson's disease. But experts diagnose the onset of pathology only if precise signs are present. The disease then goes through the following stages:
- Unilateral onset of motor symptoms, neck rigidity is evident, and tremor is observed only on one side. The duration of the first stage ranges from 6 months to three years.
- At the second stage, bilateral but asymmetrical manifestations are observed. Duration for mature patients is up to three years, for young patients up to 10 years.
- The third stage is characterized by the addition of instability to bilateral movement disorders. With properly selected therapy, the duration can be “stretched” to 15 years or more.
- At the fourth stage, it becomes difficult for the patient to turn in bed, noticeable axial apraxia develops when standing, the patient loses balance, problems arise when moving from a sitting position to a standing position, or getting out of bed after a lying position. The patient begins to need constant outside help. He is no longer able to take walks on his own and often even just walk on his own. Maximum duration 5 years.
- At the fifth stage, the patient is completely confined to a bed or wheelchair. He practically loses the ability to move and cannot swallow. The disease enters the thermal stage. One of the common causes of death is congestive or aspiration pneumonia.
The use of modern drugs makes it possible to maximize the duration of each stage, extending the thermal period as far as possible.
Treatment of Parkinson's disease
The duration and quality of life of the patient directly depends on the chosen therapy and the timely start of taking medications. Constant monitoring of health status by the treating neurologist is required.
In the early stages, drug treatment with drugs that activate the production and synthesis of dopamine is used. Additionally, drugs are used that reduce the breakdown of this neurotransmitter. Dopamine receptor antagonists are prescribed. They will be based on pramipexole, ropinirole, rotigotine. MAO inhibitors type B, based on rezalgin, are prescribed. By the third stage, the administration of Levodopa begins. In patients over 70 years of age, the use of this drug is recommended from the moment of diagnosis. The disadvantage of Levodopa is its rapid addiction with the need for a stable increase in dosage. In the older age group, Levodopa is prescribed taking into account concomitant age-related diagnoses.
Additionally, it is recommended to take vitamins that include magnesium. Vitamins A and D. The diet includes spinach, carrots, tomatoes, green onions and other vegetables.
In the absence of contraindications, surgical intervention may be recommended:
- deep electrical stimulation of the brain;
- stereotaxy;
- the use of stem cells capable of replacing dead neurons when transplanted.
Surgery often significantly improves the patient's condition.
Treatment of parkinsonism, drugs
There are two types of medications used in the treatment of parkinsonism:
- antiparkinsonian anticholinergic drugs, which include dynesin, bellazone, cyclodol, etpenal, tropacin, norakin;
- antiparkinsonian dopaminergic drugs levopa, glutantan, midantan, deprenyl.
Medicines have contraindications. Many are capable of provoking negative reactions. Including provoking hallucinations.
Treatment methods
The basis of conservative therapy is the use of drugs that improve blood flow to the brain. Antihypertensive drugs, drugs that lower LDL and cholesterol levels, anticoagulants and antiplatelet agents are prescribed.
For the symptomatic treatment of vascular parkinsonism, drugs that affect dopamine metabolism (levodopa), nootropics and neuroprotectors are used.
Parkinson's disease and life expectancy
Even a very experienced doctor cannot indicate the exact life expectancy when diagnosing the disease. In this neurophysiological disease, brain cells gradually die. What is the prognosis for the long-term development of the disease to severe stages with constant treatment and monitoring by a specialist? Many patients go through the stages of the disease over several decades.
The worst prognosis is given to elderly patients. In this case, Parkinson's disease can reach the thermal stage in just one and a half to two years. The akinetic-rheid type of the disease is also distinguished by its rapid development and progression through all stages. Many young patients, with adequate therapy, are able to live a full life and pass on to another world simply from old age for natural reasons.
The duration of the flow is influenced by many additional factors. Including constant contact with the attending physician, correlating the course of therapy. On average, the duration of development of all stages of the disease lasts 20-25 years. If the pathology begins at a young age, this period can increase to 40-50 years.
The reduction in time is associated with late diagnosis or refusal of treatment. In this option, the patient may die within 2-8 years after diagnosis.
Causes and types
Parkinsonism is divided into primary and secondary; the most common primary is Parkinson's disease.
The primary cause is damage or destruction of nerve cells or neurons located in the substantia nigra of the central nervous system. One of the main functions of neurons is the production of dopamine, which decreases during illness. Dopamine is a specific neurotransmitter, the deficiency of which can cause the following phenomena:
- muscle rigidity;
- tremor;
- decreased physical activity;
- unstable condition.
The exact cause of the disorder and the loss of dopamine has not yet been fully established.
Secondary parkinsonism is a more general clinical unified concept. It includes all types of Parkinson's disease that occur due to any disorder of the nerve cells of the basal ganglia of the brain, under the influence of any endogenous or exogenous factors. About 30% of all patients with this disease are affected by this type. There are several types of them: drug-induced, toxic, infectious, post-hypoxic and vascular parkinsonism. The most common of them is medicinal and often occurs against the background of long-term or improper use of antipsychotic drugs. Secondary causes also include head injuries, often called post-traumatic. It is observed in professional boxers.
In the post-infectious form, infectious diseases such as encephalitis, HIV, herpes, and mumps are to blame. Poisoning with gases or toxic substances causes a toxic type of disease, hypoxia of any origin also causes this disease. Vascular parkinsonism occurs due to damage or disease of the cardiovascular system. A distinctive feature of this type is a constant, non-stop tremor. It is characterized by constant twitching of blood vessels, which provokes impaired blood circulation in the brain. The danger is that vascular parkinsonis provokes a stroke. However, this form is quite rare.
Pathogenesis may be aggravated by heredity. A decrease in dopamine production leads to a failure in the transmission of nerve impulses to the anterior horns of the nerve column.
Prognosis and prevention of Parkinson's disease
Today, this disease remains incurable. Today doctors cannot offer drugs that can restore the structure of the brain. The prognosis of development is related to the age of the patient and the presence of concomitant diagnoses.
The severity of symptoms makes it possible to reduce timely diagnosis and prescribe effective therapy. The development forecast depends on:
- age of first manifestations, the younger, the more strength the body has to resist rapid development with frequent attacks leading to the death of neurons;
- prospects for the use of modern drugs, including Levodopa. Today in the Russian Federation this drug is included in the list of medications prescribed to federal beneficiaries under SNILS;
- the possibility of using innovative surgical methods, most often offered to young and middle-aged patients who are able to withstand surgery.
Due to the lack of accurate data on the causes of the onset of Parkinson's disease, exact methods of prevention are also unknown. But to reduce risks, it is recommended to lead a healthy lifestyle and stop taking drugs and alcohol. Regular medical examinations become an important prevention option.