Why does a person need two eyes?
In order to understand the causes of double vision, it is necessary to become familiar with the medical term “binocular vision.”
Double vision.
Nature has given us the opportunity to see with two eyes, because only in this case can we obtain three-dimensional vision, that is, assess the location and size of objects in space.
You can do a simple experiment. Close one eye and try to perform the usual manipulations: make tea, throw a crumpled piece of paper into the trash can, thread a thread through the eye of a needle, etc. With one eye closed, the world becomes flat: sugar spills past the cup, a lump of paper does not reach the basket, there is nothing to say about the thread and needle.
Going down the stairs becomes a real challenge due to the inability to determine the height of the steps. This is because only when using both eyes at the same time, a person receives a three-dimensional image and is able to assess how close or far this or that object is. So, binocular vision is the three-dimensional vision that a person has when using both eyes.
There are several important conditions for binocular vision to “work”: approximately the same visual acuity of both eyes, symmetrical location and normal mobility of the eyeballs, preservation of the visual nerve pathways that carry information from the eyes to the brain, absence of diseases in those areas of the brain responsible for vision , in particular, they merge images from both eyes into a single picture. If one of these conditions is violated, binocular vision is lost and various symptoms appear. One of them is double vision.
Rules of application
Correct use is the key to the effectiveness and safety of each drug.
The following procedure must be followed:
- Application of the product is only possible with clean hands.
- Carefully open the cap or take a prepared clean pipette.
- Sit on a chair or lie down, tilt your head back, pull down your lower eyelid and look up.
- Place the required number of drops behind the lower eyelid from the inside of the eye, without touching the eyelids and eyelashes.
- Release the lower eyelid and close your eyes to better distribute the drops.
- Collect excess product using a pre-prepared cotton ball.
- Keep your eyes closed for 2–3 minutes.
You also need to remember:
- eye drops are intended for individual use. Their use by other people is strictly prohibited in order to avoid the transmission of infectious eye diseases;
- the period of use and storage location of the medicine are determined by the instructions, which must be strictly followed;
- if it is necessary to use several types of drops, the break between their use should last at least 15 minutes;
- after use, the pipette is thoroughly washed;
- in some cases, patients feel the taste of the medicine after instillation. This fact is explained by the drops entering the lacrimal canal, then through the nose into the oral cavity onto the receptors of the tongue.
When using contact lenses, they are removed before instillation
Classification of double vision.
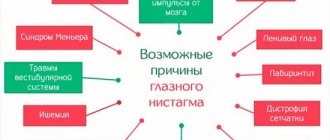
Depending on the cause, double vision can be divided into several types:
- ophthalmological (related to eye diseases and injuries)
- neurological
- endocrine
- infectious
This division is extremely arbitrary, since the reasons are often interrelated and can be combined
According to the mechanism, double vision occurs in the background:
- damage to the extraocular muscles
- lesions of the oculomotor nerves
- hematomas of retrobulbar tissue
- orbital bone fractures
- neoplasms in the paraorbital tissue
- neoplasms and other diseases of the optic nerve and visual cortex
- thyroid diseases
- infectious diseases
- alcohol and other intoxications
Symptom Definition
When a pathological condition occurs, the image that a person sees doubles.
In this case, blurred and unclear outlines are observed. With minor deviations, this condition can manifest itself only as vagueness of the contours, but severe double vision syndrome causes a feeling of incorrectness of the perceived image, which is why the patient begins to experience very strong uncertainty. Diplopia is most often the result of misalignment of the visual axes, as a result of which the brain receives not one focused image from both eyes, but from each separately. This disorder may result from a genetic predisposition or be an acquired condition. An example of a hereditary disorder of this type is strabismus.
Why does diplopia occur? Symptoms and their nature.
Most often, double vision occurs against the background of paralytic strabismus , when the mobility of one of the eyes is limited. As a rule, this is a consequence of damage (including traumatic damage) to the extraocular muscles or the nerves responsible for their work. The function of the extraocular muscles is to hold both eyes in the same position and ensure their synchronous movement.
Eye muscles and their purpose.
In this case, the brain receives exactly the same images from each eye and combines them (binocular vision). With paralytic strabismus, when looking towards the non-working muscle, the affected eye remains in the same position, so the brain “sees” two completely different images at the same time - this is double vision.
Another group of causes of double vision is the displacement of one of the two eyes . You can simulate this condition yourself by lightly pressing your finger through the eyelid into the space between the eye and the bone of the orbit. This will cause a slight shift in the eye, which you will feel as double vision.
The eye can be displaced due to injuries to the skull with a fracture of the bones of the orbit (read about the consequences of such injuries here => hematomas of the retrobulbar tissue (outflow of blood into the space behind the eye), as well as neoplasms in the cavity of the orbit (the tumor, increasing, gradually displaces the eye). In all of these In some cases, diplopia may also occur and may sometimes be accompanied by other symptoms associated with brain damage.
Neurological diseases that can cause diplopia:
- damage to the group of oculomotor nerves (3, 4 and 6 pairs of cranial nerves: oculomotor, abducens and trochlear)
- pathways
- representations of the binocular vision function (centers) in the brain (for example, the midbrain and pons of the brain stem, occipital cortex).
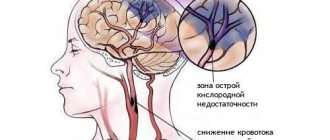
They can be damaged due to focal changes in the nervous tissue (for example, double vision after a stroke) or tumors of these or adjacent structures. In addition to double vision, these changes may be accompanied by other manifestations that will help the neurologist determine the location of the affected area.
Diseases of the thyroid gland (most often hyperthyroidism), for unknown reasons, causes an abnormal reaction in the form of immune aggression against one’s own tissues and cells. The autoimmune target is the cells of the tissue surrounding the eye (paraorbital tissue). As a result of such aggression, the fiber grows and thickens, displacing the eye anteriorly. This condition (exophthalmos) can be either unilateral or bilateral with varying degrees of severity on the right and left. Anterior displacement of the eye (exophthalmos) leads to impaired binocular vision and the appearance of double vision.
Infectious diseases (tetanus, botulism, etc.), as well as intoxication (food poisoning, alcohol poisoning, drugs and other chemical agents) have an adverse effect on nervous tissue, paralyzing the normal transmission of nerve impulses. This leads not only to double vision, but also to numerous other disruptions to the normal functioning of the human body.
Clinical picture and complaints
Symptoms will directly depend on where the violation occurs. If the oblique eye muscles are affected, then double vision occurs in the form of the location of one object above another.
If the rectus muscles are damaged, it will be parallel. Diplopia is expressed by varying degrees of deviation of the eyes in the opposite direction from the damaged muscles.
This leads to limited or complete absence of eye movement. Often patients, in order to overcome a painful condition, turn or tilt their heads.
Common symptoms of diplopia include:
- double vision;
- difficulties in the process of determining the location of objects;
- frequent dizziness.
In the case of infectious diseases, meningitis, tumors, vascular diseases, skull trauma, double vision will be combined with symptoms characteristic of these diseases. In diphtheria, diplopia occurs at the peak of the disease. In the case of botulia, double vision will be one of the primary symptoms.
- double vision;
- difficulties in the process of determining the location of objects;
- frequent dizziness.
In case of infectious diseases. meningitis. tumors, vascular diseases, skull trauma, double vision will be combined with symptoms characteristic of these diseases. In diphtheria, diplopia occurs at the peak of the disease. In the case of botulia, double vision will be one of the primary symptoms.
Diplopia in one eye and why is there double vision in one eye?
Often a person is bothered by diplopia in one eye. Unlike “classic” double vision, in this case the problem always lies in the eye itself. These may be the following conditions and diseases:
- friendly strabismus of one eye
- astigmatism of one eye (acquired)
- polycoria, traumatic injury to the iris
- lens displacement
- cataract
- retinal edema
Concomitant intermittent strabismus is a type of strabismus that is not associated with problems with the extraocular muscles and nerves; it occurs when there is insufficient vision in one eye or in the presence of uncorrected nearsightedness or farsightedness. Double vision with concomitant strabismus does not always occur; it is due to the fact that two zones of clear vision (two points of correspondence) are formed on the retina instead of one. That is, two active zones are formed on the retina, which simultaneously send information along the optic nerve to the brain, which is the cause of such a phenomenon as diplopia of one eye.
Astigmatism occurs due to acquired (after operations, injuries, inflammation and other diseases) irregular shape of the cornea - the anterior transparent membrane of the eye. A light beam passing through such a cornea is scattered, projecting a distorted image onto the retina. Congenital astigmatism causes the same defects in light refraction, but it accompanies a person from early childhood, so the brain quickly gets used to the distortions, and they are not perceived as double vision. Acquired astigmatism causes discomfort, to which, however, a person also gets used to it over time.
Problems with the iris can also cause double vision in one eye, although in these cases completely different, more significant symptoms still come to the fore. With polycoria, for example, this is a significant decrease in vision. It is unlikely that a person will complain of double vision if he sees very poorly with this eye. In case of traumatic separation of the iris from the root (attachment site), acute intense pain, profuse lacrimation, severe photophobia, and inability to open the eye due to all of the above come to the fore. It is extremely rare to notice double vision in this case. However, let’s look at these conditions and possible mechanisms of vision distortion in a little more detail.
Polycoria translated from Latin means “many pupils.” The pupil is a hole in the iris that acts as a diaphragm: by narrowing or expanding, it regulates the amount of light entering the retina. Polycoria can be congenital (developmental anomaly) or acquired (a consequence of injury or eye disease). In addition to the “main” pupil, the iris has one or more holes through which light also enters the retina, distorting the image on it.
As a result of an eye injury, the iris can be torn away from its attachment point; excess light enters through this gap, which, through the same mechanism, can give a feeling of double vision.
Displacement of the lens (including artificial) is possible due to rupture or weakness of the zonules of Zinn - the ligaments on which the lens with its capsule is fixed. Doctors call this situation “lens subluxation.” If the subluxation is of a sufficiently high degree, the lens shifts significantly, and the equator of the lens—its edge—becomes visible in the lumen of the pupil. Some of the light passes through the lens, some through its edge, and some through the area without the lens, and the retina receives a distorted image.
Cataracts (clouding of the lens) in the early stages can also sometimes produce symptoms similar to double vision due to the displacement of the light beam in the cloudy area of the lens.
Retinal edema is when it becomes saturated with fluid. The retina is not only a collection of rods and cones (receptors of the terminal branches of the optic nerve). The retina consists of 10 layers, some of which are represented directly by nervous tissue, and some are intended to ensure its normal functioning. When retinal edema occurs, fluid accumulates between the layers, the retina rises and protrudes anteriorly. All this leads to a disruption in the normal perception of images; a person sees straight lines as curved, objects as distorted, and double vision may appear in the form of a second contour of the object.
Treatment
During a thorough examination, your doctor can diagnose retinopathy. In the early stages, retinopathy is corrected by photocoagulation - laser treatment. The procedure can completely restore vision. When combined with subsequent prevention, photocoagulation reduces the risk of blindness by 90%
In later stages, with retinal detachment or large retinal hemorrhages, vitrectomy - removal of the vitreous humor - may be indicated. The surgery involves removing scar tissue, blood clots, and cloudy fluid that has accumulated in the eye. Vitrectomy can improve vision.
Diplopia: treatment. Double vision and ways to correct it.
Diplopia is a condition that should never be ignored; it is always a reason for examination.
Double vision is not a separate disease, so it is impossible to cure double vision without eliminating the original cause!
Strabismus is treated jointly by ophthalmologists and neurologists. As a rule, this is a long process; you should not expect any effect sooner than six months later. The prognosis depends entirely on the specific cause, so it should be discussed with doctors.
If the cause of diplopia is a hematoma of the retrobulbar tissue (hemorrhage in the tissue behind the eye), then as the blood is absorbed, the eyes will return to their “place”, which will be accompanied by a gradual improvement in the condition.
Fractures of the orbital bones are treated by ophthalmologists and maxillofacial surgeons. If reposition is performed in a timely manner (the edges of the fragments are compared), then after healing, after some time (again, within 6 months), the diplopia gradually goes away.
If the cause is a tumor, then only its treatment can help eliminate diplopia.
Diplopia associated with thyroid disease must be treated as soon as possible, as other changes occur quite quickly that can lead to complete blindness. The main treatment is carried out by an endocrinologist.
Treatment of diplopia due to diseases and poisoning is carried out in an infectious diseases hospital. The likelihood of recovery depends on the severity of the general condition and the timeliness of assistance provided.
If double vision is felt only when looking with one eye (diplopia of one eye), then the cause is always inside the eye. If the problem is concomitant strabismus, the doctor develops a special set of measures and exercises that will help correct strabismus and double vision. Astigmatism can be corrected with glasses, contacts, or surgery. Diseases of the iris, including after injury, can only be treated surgically.
But since such interventions have a high risk of complications, the decision is made by the ophthalmic surgeon individually in each individual case. The same applies to diseases of the lens. Retinal edema is treated conservatively or by injecting drugs into the eye cavity (intravitreal). Retinal edema does not respond well to treatment and, unfortunately, often recurs.
You see that the reasons that caused double vision are quite diverse, and it is simply impossible to figure them out on your own. Therefore, as soon as it appears, you must immediately see an ophthalmologist, he will conduct an examination and, if necessary, refer you to doctors of other specialties.
astigmatizm-club.ru
Patients often turn to ophthalmologists with complaints of double vision, the causes and treatment of which only the doctor knows. This symptom brings considerable discomfort in the perception of the environment and is often a concomitant symptom of a serious illness.
This vision pathology in medicine is called diplopia. With this disease, coherence in eye movements is disrupted, and the patient sees one object as 2 separate ones.
The effect of diabetes on vision: drops and vitamins for the eyes
Diabetes mellitus is a common disease characterized by damage to small and large blood vessels throughout the body.
In many cases, with this diagnosis, there is a violation of the structure of the visual organs.
One of the most common and severe complications of hyperglycemia is diabetic retinopathy – damage to the blood vessels of the retina, leading to loss of vision.
How does diabetes affect vision?
With hyperglycemia, the human body experiences constant surges in blood glucose levels. If the sugar concentration is increased over a long period of time, this leads to a change in the curvature of the lens and damage to the retina and optic nerve.
As a result, jumps in visual acuity are observed, causing damage to the blood vessels that supply the retina of the eye. Eye diabetes can cause temporary myopia, the symptoms of which disappear immediately when blood glucose levels normalize.
Diabetic cataract
Cataract is an eye disease that causes clouding of the lens of the eye. This pathological condition is one of the common complications of diabetes mellitus.
As a result of periodic surges in blood sugar levels, material metabolism is disrupted, the nutrition of the eyeball is significantly deteriorated, as a result of which glucose compounds accumulate in the structure of the lens, causing its hardening and darkening.
This leads to incorrect refraction of light rays and the formation of a fuzzy image.
Diabetic cataract, which can be true or senile, can develop at any age and at any stage of hyperglycemia. Most often, this complication occurs in women over 40 years of age and affects both organs of vision. With timely treatment and constant monitoring of blood sugar concentrations, diabetic cataracts can disappear within 2 weeks.
Diabetic glaucoma
With hyperglycemia, vascular damage occurs in all vital organs, including the eyes.
A high concentration of sugar in the blood causes the formation of new eye vessels, which block the normal outflow of intraocular fluid, causing an increase in ophthalmotonus (eye pressure). Thus, glaucoma of the eye develops, accompanied by the following symptoms:
- flashing halos of light before the eyes;
- photosensitivity;
- increased lacrimation;
- pain;
- eyes itch;
- discomfort.
Diabetic glaucoma is a fairly common complication of diabetes, which if not treated promptly leads to complete blindness.
Diabetic retinopathy
Diabetic retinopathy is a common eye complication in diabetes mellitus, characterized by damage to the retinal vessels. The likelihood of developing such a pathological condition increases with the course of hyperglycemia.
The longer a person is sick, the higher the risk of irreversible retinal changes and vision loss.
And if the patient additionally suffers from anemia, hyperlipidemia or obesity, then the rate of progression of diabetic retinopathy increases significantly.
You can suspect the presence of eye diabetes based on the following symptoms:
- blurred vision;
- flickering of “flies” and dark spots before the eyes;
- a veil covering the eyes;
- poor visibility up close.
The severity of symptoms and treatment depend on the stage of the disease. At the initial stage of hyperglycemia, visual impairment is minor; to restore it, it is enough to change your lifestyle, follow a diet and control your sugar levels. In more complex cases, conservative or surgical treatment is prescribed. Laser coagulation is often used for treatment.
Eye drops for diabetes
The first step in treating eye diabetes is to prescribe antihyperglycemic drugs or insulin to control blood sugar levels, as well as special exercises for the eyes.
For stage 1 diabetes, these measures are sufficient. At stage 2, eye drops are prescribed to stop the progression of diabetic retinopathy, cataracts or glaucoma.
If hyperglycemia is complicated by glaucoma, the following medications may be recommended:
- Timolol;
- Betaxolol;
- Photin.
Diabetic cataracts are treated with the following medications:
- Catalin;
- Taufon;
- Katachrom.
The following ophthalmic drops will help cope with diabetic retinopathy:
- Quinax;
- Riboflavin;
- Vitafacol.
Eye drops for diabetes should be used 1-2 drops 2-3 times a day for 2-3 weeks. Treatment for diabetic glaucoma can take much longer.
Vitamins for eyes for diabetes
In diabetes mellitus, material metabolism is disrupted, as a result of which the body does not receive enough vitamins and microelements. Therefore, patients with hyperglycemia are necessarily prescribed vitamin therapy to strengthen vision. Diabetics with eye pathologies need to take the following vitamins daily:
- B vitamins . They normalize glucose levels, ensure normal functioning of the central nervous system, and improve blood circulation.
- Ascorbic acid. Strengthens the immune system, makes blood vessels more elastic.
- Tocopherol. Cleanses the body of toxins and glucose breakdown products, strengthens blood vessels.
- Retinol. Provides good visibility at night, improves visual acuity.
- Vitamin R. Dilates blood vessels, improves microcirculation.
In addition to these vitamins, diabetic patients should take mineral complexes. For diabetic retinopathy, vitamin eye drops Quinax or Prenacid are most often prescribed. Eye vitamins for diabetes such as Blueberry-Forte, Selenium-Active and Vervag Pharma also help well.
Eye surgery
In advanced cases of diabetic retinopathy, cataracts or glaucoma, surgical intervention is performed. Most often, laser coagulation of the retina is prescribed, aimed at reducing the formation of pathological vessels. Sometimes vitrectomy is performed. Eye surgery is performed only in extreme cases when conservative therapy is ineffective.
Source: https://GlazaLik.ru/spravka/diabet/
Types of diplopia
There are different classifications of diplopia according to the cause, clinical picture, and development of the disease.
Doubles happen:
- Monocular - double vision in one eye. With this type, if the patient closes one eye, the double vision does not disappear.
- Binocular - symptoms appear when both eyes are used, and disappear when one of them is closed. With the binocular type of diplopia, the visible image spreads vertically or horizontally in the eyes.
Diagram explaining what diplopia is
Depending on the causes, binocular diplopia is divided into subtypes:
- strabogenic - occurs in patients with various types of strabismus;
- oculogenic - develops after eye surgery;
- neuroparalytic - manifests itself due to damage to the nerve endings that supply the nerves that carry out eye movement;
- restrictive - provoked by damage due to eye injuries with a shift of the eyeball or tightness of the muscles that move the eyes.
Double vision also happens:
- Paralytic - manifests itself due to paralysis of the external muscles of the eye.
- Cross – the picture is shown crosswise.
How to remove double vision?
Treatment of diplopia is usually aimed at correcting the underlying disease. Anomaly of perception is not a disease, but an indicator of problems. In some cases, medical intervention must be urgent, but if no other signs of ill health appear, then restoration of normal vision takes some time. For correction, along with drug therapy, the patient is offered:
- wear special glasses - built-in prismatic lenses help focus;
- do special gymnastics, the simplest exercise is rotating the eyeballs with the eyelids closed;
- detoxification in case of poisoning almost immediately eliminates symptoms;
- for injuries, cataracts and retinal detachment, surgery is used;
- For pathologies of the thyroid gland and other endocrine disorders, hormone therapy is prescribed.
Causes
The eye is a complex system that consists of the perception of colors, objects, optics, and sending information to the brain through the nervous system. Complications are possible in each of these components. When a patient experiences double vision, it is possible to assume the following causes of diplopia:
- Inflammation of the cornea of the eye. If the disease is not cured in time, it can lead to complications such as damage to the optic nerves and muscles. The main reason for monocular diplopia is various eye injuries.
- Aneurysm of the internal carotid artery, which compresses the optic nerve.
- Diabetic neuropathy is a complication of diabetes mellitus that occurs in patients who have been sick for a long time. This reason most often provokes the appearance of diplopia in older people (over 50 years old) with type 2 diabetes.
- Benign and malignant tumors, hematomas in the cerebral hemispheres and eye sockets affect the connections of nerve tissue and individual areas in the subcortex.
- Unilateral or bilateral diplopia often accompanies surgery for retinal detachments, cataracts, and strabismus.
- Traumatic brain injuries.
- Malfunctions in the functioning of the endocrine system and thyroid gland sometimes also act as a cause of double vision.
- Diseases of the nervous system - cerebral infarction, meningitis, stroke.
- Infectious diseases, especially mumps, tetanus, diphtheria and rubella.
- Increasing a single dose of Botox, which is administered during cosmetic procedures, can also cause double vision due to changes in neuromuscular conduction.
Botox injection - Vegetovascular dystonia. In the case of VSD, we are talking about idiopathic diplopia. The reasons that the patient has double vision in this case are not physiological, but psychological. Doctors cannot come to a common opinion which area this is: neurology, or a state of neurosis, or a psychosomatic disease.
Sometimes completely healthy people experience double vision when looking at objects due to insufficient sleep, after heavy mental or physical work, or intoxication of the body, including alcohol and medication.
Double vision in type 2 diabetes
Treatment of such a serious disease as diabetes mellitus is a priority task of modern medicine. The consequences of type 2 diabetes can lead to disability or death.
In addition, a complication may develop against the background of the disease - so-called eye diabetes. Retinopathy in diabetes mellitus is the leading cause of blindness.
As a result of this disease, the vascular system of the eyeball is affected.
What is diabetic retinopathy
In diabetes, early detection of changes in the retina of the eye helps to take measures to prevent the development of the disease.
Diabetic retinopathy is a severe complication of diabetes that occurs in 90 percent of patients affected by the endocrine disease.
Diabetes of the eye is often the result of a long course of the disease, but timely examination helps to detect changes at a very early stage.
Stages
| Stage 1 | Stage 2 | Stage 3 | Stage 4 |
| Non-proliferative (background) stage. | Preproliferative form. | Proliferative stage. | Terminal stage. |
| The fragility and permeability of capillary walls increases. Damage to the membranes of the eyes. Hemorrhages occur in the eye, and retinal edema develops. | Strong destructive processes begin. Retinal detachment. Visual acuity decreases. The eye may become very swollen. | Abnormal vessels begin to grow in the eyeball. The appearance of new capillaries, which are very fragile, leading to frequent hemorrhages. | Final changes in the retina leading to blindness. There may come a time when the lens will not focus light rays, and this will lead to complete blindness. |
- Diabetic nephropathy - causes, symptoms, classification by stages and treatment
- Retabolil - instructions for use, composition, release form, indications, side effects, analogues and price
- Gliclazide tablets - instructions for use, composition, dosage, contraindications, analogues and price
Eye treatment
At all stages of the pathogenesis of retinopathy in diabetes, treatment of the eye vessels, aimed at correcting metabolic disorders, must be carried out.
Adequate therapy for diabetes mellitus and strict control over glycemic levels should also be organized as early as possible from the onset of the disease.
A significant factor in the treatment of eye disease is the use of medications that cause a decrease in angioprotectors, cholesterol concentrations, immunostimulants, anabolic steroids, biogenic stimulants, and coenzymes.
Using laser coagulation of the retina
Treatment of hemorrhage in the eye using laser coagulation is considered to be the most effective. The essence of the method is that to stop the disease, capillaries are cauterized using a special laser. Laser eye treatment is a modern and effective method, the correct use of which stabilizes the development of the disease.
According to doctors, photocoagulation helps eliminate up to 82% of cases of the disease in the preproliferative stage, and up to 50% in the prophylactic stage.
At the last stage of retinopathy, laser coagulation allows patients to preserve their vision for 1 to 10 years. Diabetic cataracts and senile cataracts can also be treated with laser photocoagulation.
Timely photocoagulation of the retina will help avoid blindness!
Drugs
A patient with retinopathy due to diabetes mellitus should be treated jointly by an ophthalmologist and an endocrinologist. Treatment is carried out under the control of general indicators of the blood system.
In addition, the healing process must include insulin therapy, a rational individual diet, and vitamin therapy.
When treating eye diabetes, a variety of medications can be used to help improve the condition of the retinal vessels and slow down the disease.
Neurovitan is often prescribed as the main drug for retinopathy:
- This medication is safe and effective and does not cause side effects.
- It is prescribed to adults, 2 tablets per day.
- The course of treatment is 2 weeks.
- You should not drink alcohol while taking the medicine.
Among other vitamin formulations, Vitrum Vision Forte is often prescribed. The doctor may also recommend taking medications based on Ginkgo Biloba:
- These drugs are usually available in capsule form.
- They are taken like vitamins - one capsule per day.
A prick in the eye
Retinopathy in diabetes can be treated with Retinalamin:
- This medicine can reduce the intensity of local inflammatory processes.
- The drug is administered parabulbarly, i.e. into the lower eyelid area through the skin.
- It is necessary to administer 5-10 mg of the active substance per day, first diluting it in 2 ml of saline solution.
- The course of treatment is up to 10 days.
Doctors also recommend using Vasomag:
- This medicine can optimize metabolism and energy supply to tissues.
- Its timely use in eye diabetes helps slow down the pathology.
- Vasomag is administered parabulbarly.
- It is recommended to use the drug in the morning due to the likely stimulating effect.
- Contraindicated during pregnancy, with increased intracranial pressure, and in children under 18 years of age.
Eye pressure tablets
The drug "Arifon":
- Contains the active substance – indapamide.
- The drug has a vasodilator, diuretic, hypotensive effect.
- Adults are prescribed 1 tablet per day; it is advisable to take the drug in the morning.
- The drug is not used in children, during lactation, or for kidney and liver diseases.
Treatment of eye disease in diabetes mellitus can be carried out with the help of drugs that affect the capillaries of the retina. These include:
- "Troxevasin";
- "Venoruton".
The above drugs are used as follows:
- They are used in the form of capsules.
- The tablets are taken 3 times a day for two weeks.
Eye drops for pain in the eyes
Eye drops may help with diabetic retinopathy. Doctors advise drinking "Emoxipin":
- The contents of the drug are drawn up with a syringe without a needle, then the liquid is instilled into the eye.
- You should apply 2 drops 3 times a day.
- The course of treatment is 30 days.
You can also use Timolol drops:
- The active substance reduces intraocular pressure.
- The drug normally begins to act 20 minutes after use.
- It is not recommended to use the medicine for bronchial asthma, chronic pulmonary obstruction, or while breastfeeding.
Can vision recover on its own?
When a disease such as angiopathy occurs, vision itself cannot be restored.
It is imperative to undergo treatment, including the use of medications, diet, annual examination by specialists, and in the acute course of the disease, surgery.
Poor vision cannot be cured with eye drops or tablets. Therefore, the most effective treatment for diabetic retinopathy, which helps to avoid blindness, remains panretinal laser coagulation of the retina.
Diagnostics
The main goal of diagnosis is to determine the causes of diplopia. To do this, you need to find out the location of the damage: the eye, the optic nerve, the auxiliary apparatus of the eye, or the brain.
The examination includes the following procedures (their necessity and quantity is determined by a specialist) such as:
- slit lamp eye examination;
- Ultrasound of the eyeballs;
- direct and indirect ophthalmoscopy;
- viziometry;
- conjunctival analysis;
- acuity and visual fields;
- refraction of a light beam;
- electromyography;
- cordimetry;
- perception of color gamut (four-point color text);
- Edrophonium test.
Survey
An important method in identifying this disease is testing (ophthalmological cover test). During the test, the following information is revealed:
- at what point did double vision appear, during what events;
- whether there was a fall, fainting, eye or head injury;
- does the splitting intensify with fatigue or in the evening;
- what problems are there, besides double vision;
- whether or not the person being examined tilts his head to the side;
- double vision improves or worsens when tilting the head to one side or the other;
- double vision if you close 1 eye.
If necessary, the attending physician, having studied the examination results, gives a referral to the patient to other specialists: neuro-ophthalmologist, neurologist, oncologist, psychiatrist, dermatovenerologist, rheumatologist and endocrinologist.
In the presence of strabismus, the method of diploptic provocation with coordiometry is used. The specialist performs a test tracking of the patient's vision while looking at a light source that is moving. Then the data is transferred to a special coordinate map. After analyzing them, the specialist identifies damage to one of the eye muscles.
Correct diagnosis of diplopia
Examination methods
Basic: none; OAK, ESR/CRP, lipid profile, urinalysis, fasting glucose or HbAlc.
Additional: thyroid function testing, radiography, CT/MRI.
Auxiliary: edrophonium test, electromyography, cerebrospinal fluid examination, angiography.
- At the initial stage, no examination is required to identify the most common causes; referral to a specialist is the most preferable option.
- OAK, ESR/CRP, lipid profile, if cranial nerve palsy is suspected and there is no need for hospitalization, OAK and ESR/CRP will also show signs of inflammatory diseases.
- Urine glucose/fasting blood glucose or HbAlc will help detect diabetes.
- A thyroid function test may reveal hyperthyroidism.
- Other studies (possibly some of those mentioned above) will most likely be carried out at the stage of specialized care: radiography of the bones of the skull and face for injuries; CT or MRI (head injury, stroke, multiple sclerosis, intracranial space-occupying lesion); specialized neurological studies (edrophonium test, electromyography, cerebrospinal fluid analysis, angiography).
Determine whether diplopia is binocular or not. With monocular double vision, there is a much smaller list of possible causes.
Take time to clarify the symptom. Sometimes patients complain of “double vision” when what they really mean is blurred vision, and vice versa.
By covering one of the eyes, you can find out for sure which eye is affected.
IV cranial nerve palsy causes diplopia in downward and inward gaze, which is often noticed when descending stairs. The patient may try to compensate for this by tilting the head - the so-called ocular torticollis.
Intoxication combined with head trauma is often observed in isolation wards and emergency departments. Hospitalization for neurological observation is strongly recommended.
Acute onset diplopia may reflect a serious pathology and the patient should be referred for emergency care.
Intermittent diplopia should not be easily dismissed as a minor symptom—remember that myasthenia gravis and multiple sclerosis are possible diagnoses.
Anamnesis. From the anamnesis it is necessary to determine whether the image is double in one or both eyes.
Examination of other systems includes checking for cranial nerve dysfunction such as blurred vision, numbness of the forehead and cheek, facial weakness, dizziness, hearing loss, gait changes, and difficulty swallowing or speaking. The patient should be assessed for other persistent or intermittent neurological symptoms such as weakness and sensory disturbances.
Physical examination. The patient's assessment begins with examining vital signs for common symptoms of fever and toxicity (eg, prostration and confusion).
An ophthalmological examination begins with an external examination and measurement of visual acuity with correction of each eye individually and both eyes together, which makes it possible to establish the monocular and binocular nature of diplopia. It is necessary to note the presence of exophthalmos, ptosis, pupillary defects during external examination, as well as uncoupled eye movements and nystagmus during the study of eyeball mobility. During ophthalmoscopy, any abnormalities of the lens (eg, cataract, dislocation) and retina (eg, detachment) are noted.
In some cases, the affected eye can be identified by closing the eyes one at a time; The weakened eye is the one whose closure eliminates peripheral double vision.
The doctor then completes a neurological examination, checking strength, sensation, reflexes, cerebellar function, gait, and symptoms of damage to other pairs of cranial nerves.
Other important diagnostic tests include palpation of the neck for a goiter or signs of pretibial myxedema (Graves' disease).
Alarming symptoms. Worrying symptoms include:
- involvement of more than one pair of cranial nerves;
- pupil involvement;
- any neurological symptoms other than diplopia;
- pain;
- proptosis.
Interpretation of survey results. Test results often indicate involvement of a specific pair of cranial nerves:
- Third pair of cranial nerves: ptosis, deviation of the eyeball downwards and laterally, in some cases – dilation of the pupils.
- Fourth pair of cranial nerves: vertical diplopia, worse when looking down (the patient tilts the head to improve vision).
- Sixth pair of cranial nerves: deviation of the eyeball medially, worsening diplopia when looking to the side (the patient turns his head to the right to improve vision).
Other test results also help suggest the cause of diplopia.
Intermittent diplopia indicates a neurological disorder with dynamic symptoms (periods that wax and wane), such as myasthenia gravis or multiple sclerosis, or the manifestation of latent phoria (deviation of the ocular axis). Patients with latent phoria do not have other neurological symptoms.
Internuclear ophthalmoplegia (IO) occurs due to damage to the brain stem in the region of the medial longitudinal fasciculus. It can be diagnosed by examining the mobility of the eyeball. Usually in this case there is limited gaze mobility on the damaged side (no further than the central line) and contralateral nystagmus. At the same time, during convergence, eye mobility is not limited, because in this case, the medial longitudinal fasciculus is not involved.
Painful sensations suggest a pressing lesion or inflammatory disease.
Special studies. Patients with monocular diplopia should be referred to an ophthalmologist for a specialized examination without prior examination.
In the case of binocular diplopia, to identify patients with unilateral palsy of one of the pairs of cranial nerves, the reaction of the pupils to light is checked. Other symptoms in this case usually do not appear for several weeks. Often the condition resolves spontaneously on its own. To clarify the nature of the disorder and the patient's condition, an ophthalmological examination may be recommended.
Other patients may require neuroimaging (MRI) to identify lesions in the orbit, skull, or central nervous system. If there is a suspicion of a metallic foreign body in the orbit, or if MRI is unavailable or contraindicated, diagnosis can be made using computed tomography. If infection, aneurysm or acute stroke is suspected ({amp}lt;3 hours), examination should be carried out immediately.
Thyroid function tests (serum thyroxine [T4] and thyrotropin tests) are indicated in patients with signs of Graves' disease. Patients with intermittent diplopia are recommended to undergo testing for myasthenia gravis and multiple sclerosis.
If a patient begins to experience double vision for no apparent reason, then one should not delay visiting a doctor; the sooner this is done, the better.
Due to the fact that the reasons can be quite serious, the slightest delay can lead to disastrous consequences.
To determine the cause of double vision, your doctor will typically perform diagnostic tests, ranging from a general examination, blood tests, and a CT scan.
The success of treatment will directly depend on a correct diagnosis.
A general survey will help the doctor make the correct diagnosis. It may include questions about the onset of symptoms, injuries ever received, loss of consciousness, possible accidents, the dependence of the intensity of vision on the time of day, as well as the presence of other accompanying symptoms.
Neurology, infectology and other areas of medicine can be closely related to ophthalmology in this matter.
During the examination, the participation of other doctors may be necessary, depending on the causes of the disease, in order to prescribe the correct treatment.
Diplopia therapy
When identifying symptoms of diplopia, the patient should understand that they can be signals of a serious illness. It is necessary to consult a doctor immediately to avoid possible complications.
Vision with diplopia
Therapy for double vision consists of curing the underlying disease that caused it. This process requires a positive attitude and determination.
Traditional medicine methods
Implied:
- Drug treatment of infectious or inflammatory diseases.
- The patient wears specially made glasses with prismatic lenses. The centers in these lenses are often shifted, which also corrects vision.
- If the cause of double vision is a disease of the thyroid gland or other diseases of the endocrine system, hormone therapy is performed.
- Specialized gymnastics according to Kashchenko refers to a functional method of treatment. These exercises are intended for a home environment. For example, with partial diplopia, a piece of paper with a stripe is hung on the wall. The patient needs to focus on the strip with both eyes and rotate his head from side to side. The strip must be kept whole, not forked. With sensory bifurcation, the essence of the exercise is to combine double pictures into one.
- If the cause of the split is poisoning, detoxification is performed.
In case of surgical intervention, it can be performed in 2 ways:
- The surgeon shortens one muscle, and at its expense the action of another is compensated.
- The doctor moves the muscles of the eyeball back and sews the crossed tendon to the sclera.
Scheme of surgery to shorten the eye muscle
In addition, the following is carried out:
- Antitumor therapy in the orbit.
- Treatment of abnormalities in the field of neurology and neuropathy.
- The occlusion method, “turning off” one of the eyes, is used in case of damage to several nerves. The doctor offers specialized contact lenses, or if the patient wears glasses, places opaque tape on the lens of the glasses. With the help of occlusion, the patient loses 3D perception. This method is the most practical in developing a habit of vision changes.
- Sometimes botulinum toxin is injected into the patient's eye muscle. This procedure is performed under local anesthesia. The result is temporary or permanent relief from double vision.
Folk remedies
Alternative medicine offers its own recipes for the treatment of diplopia, which cannot in any way be the main methods of treatment, but are auxiliary, restorative:
- Tincture: valerian powder, lavender leaves (crushed), 1 liter of dry white wine. Leave for 3 days, shake occasionally. Filter the finished tincture. Use 2 tsp. half an hour before lunch.
- Flower pollen. Use 1 tsp. in the morning and in the evening. Course - 1 month.
- Vitamin collection. Boil the fruits of hawthorn, rose hips, viburnum for 10-15 minutes, let it brew until completely cool, strain. Drink half a glass twice a day systematically.
This disease cannot be prevented, as it is unpredictable in its development. Prevention is of a general strengthening nature:
- quitting smoking and alcohol abuse;
- healthy eating;
- physical exercise;
- mode;
- sufficient sleep;
- undergoing systematic medical examinations;
- control blood pressure and blood sugar.
There are various types of gymnastics for the eyes, normal binocular vision, muscles of the upper cervical spine, blood circulation of the eyes and brain. It is recommended to use them for the prevention of diseases leading to diplopia.
Antidiabetes
Last time we got acquainted with the complications of diabetes on the cardiovascular and nervous systems, which develop with a long-term moderate increase in blood sugar levels.
Today we will deal with the organ of vision, which is also affected by diabetes. Vision is normal (left) and with diabetic retinopathy (right).
Eye diseases in patients with diabetes occur 25 times (!) more often than in the general population. To better understand the following material, it is recommended to remember the structure of the eye.
Diabetic retinopathy (retinal damage, from pathos - suffering) is one of the leading causes of visual impairment in diabetes. The longer the duration of diabetes, the more often diabetic retinopathy develops: from 5% during the first 5 years of diabetes to 80% with diabetes lasting more than 25 years. It is curious that in children, retinopathy is observed much less frequently and occurs only after the end of puberty (17-18 years). Scientists believe that this is due to hormonal growth factors in children.
Stage I - non-proliferative retinopathy.
Proliferation is the multiplication of cells; this does not yet occur in the first stage of diabetic retinopathy. In diabetes, the smallest blood vessels are most affected (microangiopathy); similar processes occur in the vessels of the retina. Capillaries and venules (the smallest veins) are primarily affected, and microaneurysms (enlarged areas with a reduced blood flow rate) form in them. The mechanism of microaneurysm formation is associated with metabolic disorders in cells and tissue hypoxia (lack of oxygen).
This is what the vessels in the fundus look like normally.
Early microaneurysms. The macula (central part of the retina, macula) is still normal.
Stage II - preproliferative retinopathy (“preproliferative” means “before proliferation”).
In stage II there are already many microaneurysms, they are large. Some microaneurysms, due to a reduced blood flow rate, thrombose and become overgrown with connective tissue, while others burst (rupture) with the formation of hemorrhages. The contents released from the burst vessel are called exudate. At this stage there are a lot of exudates, they are large. Venous anomalies are clearly expressed: vessels in the form of rosaries (beads), tortuous or doubled.
Microaneurysms, “cotton-wool spots” (retinal infarctions due to thrombosis of a nearby blood vessel), hemorrhages (bleeding).
Venous anomalies, microvascular pathology within the retina, ischemia.
Stage III - proliferative retinopathy.
Against the background of microaneurysms and hemorrhages in the retina, hemorrhages into the vitreous body appear at this stage. At the sites of these hemorrhages, areas of inflammation appear, which heal with the formation of connective tissue cords (proliferation - cell multiplication). The strands penetrate from the retina into the vitreous body and gradually shrink, tightening like scars, leading to retinal detachment and blindness.
Proliferative stage of diabetic retinopathy. Scar cords are visible in the vitreous body, which, when wrinkled, cause retinal detachment and blindness. At the base of the cord are newly formed blood vessels (neovascularization).
Since the retinal vessels are pathologically altered (twisted, dilated, with aneurysms) and do not perform their functions well, new vessels are formed. This process is called neovascularization and also refers to the phenomena of proliferation. Random neovascularization can lead to visual impairment.
New, newly formed blood vessels.
Connective tissue around new vessels.
All stages of diabetic retinopathy are characterized by a wave-like course with spontaneous remissions and exacerbations. High and low sugar levels, arterial hypertension, kidney failure, and pregnancy contribute to the deterioration.
Left: preproliferative diabetic retinopathy. Arrows indicate hemorrhages and cotton wool spots. Right: proliferative diabetic retinopathy. Arrows indicate neovascularization.
Stages of diabetic retinopathy (from left to right): 1) normal 2) initial (background) retinopathy 3) non-proliferative diabetic retinopathy 4) severe non-proliferative diabetic retinopathy 5) neovascularization in proliferative diabetic retinopathy 6) fibrovascular membranes (scarring).
Among all blind people, about 7% are diabetics. The causes of blindness in patients with diabetes are:
- vitreous hemorrhage
- diabetic retinopathy
- retinal disinsertion
- glaucoma
- cataract.
A cataract is a clouding of the lens that causes blurred vision.
Cataract is clouding of the lens.
glucose, in proportion to its concentration in the blood, enters the cells of insulin-independent tissues (nervous tissue, lens and retina, kidneys, pancreas, vascular walls), where, under the influence of enzymes, it enters an additional metabolic pathway: glucose? sorbitol? fructose. Unlike glucose, fructose can be absorbed by cells without the participation of insulin.
2) senile (senile) cataracts also occur in healthy elderly people, but in diabetics it matures much faster and therefore more often requires surgical treatment.
This is what people with cataracts see.
Glaucoma is an increase in intraocular pressure. Occurs in 5% of diabetics and 2% of healthy individuals. With glaucoma, the fibers of the optic nerve are damaged, which leads to loss of first peripheral vision, and then central vision.
This is what people with glaucoma see.
For diabetics (and not only for them), the open-angle form of glaucoma is typical, in which the outflow of aqueous humor through Schlemm’s canal, a circular venous vessel located in the thickness of the sclera at the border with the cornea, is impeded. However, in diabetics, damage to Schlemm's canal (venous vessel) is a manifestation of diabetic microangiopathy.
Speaking about eye diseases in patients with diabetes, one cannot help but recall diabetic neuropathy, which leads to damage to the oculomotor nerves. The most common conditions are diplopia (double vision) and ptosis (drooping of the upper eyelid).
Transient (temporary) impairment of visual acuity occurs in patients with diabetes mellitus at the beginning of insulin treatment. The mechanism of this phenomenon is simple. When blood glucose levels are high, approximately the same concentration ends up in the lens, where glucose is converted to sorbitol, which osmotically retains fluid.
READ MORE: Folk remedies for treating demodicosis
As a result, the lens swells and begins to refract the rays more strongly, causing them to collect in front of the retina (myopia). In addition to myopia, sorbitol accumulation contributes to the development of diabetic cataracts. When insulin treatment for diabetes mellitus begins, blood glucose levels drop and the refraction of the eyes (the refraction of rays) weakens, which affects visual acuity.
Glucose is a good breeding ground for bacteria, so diabetes mellitus contributes to the protracted course of infectious and inflammatory diseases, including the eyelids:
- blepharitis - inflammation of the edges of the eyelids
- stye - acute purulent inflammation of the hair follicle of the eyelash or the sebaceous gland of the eyelid
- Chalazion is a chronic (unlike barley) proliferative inflammation of the eyelid margin around the sebaceous gland and eyelid cartilage.
As you have seen, eye damage can be diverse, so patients with diabetes should be examined by an ophthalmologist at least 1-2 times a year. It is necessary to determine visual acuity and fields, and assess the condition of the fundus vessels.
Next time - damage to the urinary system due to diabetes.
Retinopathy is a vascular lesion of the eye that leads to serious damage to the retina, which can result in complete loss of vision. Conservative methods of treating retinopathy in diabetics do not lead to complete relief from the disease, but can slow down the development of pathological changes in the blood vessels.
Retinopathy causes progressive vision loss
As a rule, eye drops are prescribed, the same as for cataracts: Quinax, Taurine, Taufon, as well as:
- Emoxipine, which improves blood circulation and metabolism at the cellular level, resolves hemorrhages. Not used in case of individual intolerance. The use of the drug may lead to burning and itching, which disappear on their own. Apply 1-2 times a day, 1-2 drops for a month;
- Hilo-chest eliminates the feeling of dry eyes that occurs as a result of poor nutrition. Contraindications include hypersensitivity to the components of the product. Has no side effects. Apply three times a day, 1–2 drops;
- Riboflavin is prescribed for type 2 diabetes mellitus. The drug is made on the basis of vitamin B2, which helps normalize hemoglobin synthesis and metabolism, which leads to improved visual function. Improves the functional abilities of fiber. The use of the drug can lead to allergic reactions and temporary impairment of visual acuity. One drop of the drug is instilled twice a day.
- Lakemox protects the corneal epithelium and conjunctiva of the eye. Has a lubricating and softening effect. Stabilizes the membrane structures of the retina. Resolves hemorrhages, reduces swelling. Has an antioxidant effect. Contraindicated in case of individual sensitivity to the components of the drops, a tendency to allergies, or pregnancy. May cause burning, itching, allergies and other local effects. Used for a month, 1-2 drops three times a day. The course of treatment can be repeated after six months.
Along with the use of eye drops, the patient needs to maintain normal general health. Today, the pharmacological industry offers on the market a drug containing only herbal ingredients and capable of fighting not only diabetes, but also its consequences.
Before using the drug, do not forget to consult with your doctor
Causes in pathologies
The study of such causes has shown that they can cause irreversible consequences. The most dangerous pathological processes can be identified:
- motor nerve infection;
- paralysis of the eye muscles;
- the oculomotor nerve is subject to increased pressure.
Accordingly, we can note diseases that cause bifurcation:
- meningitis;
- neurological diseases;
- infectious pathologies;
- orbital tumors;
- vasculitis;
- intoxication of the body.
In the presence of even one disease, the cause of diplopia can be assumed. The symptom will not go away on its own. The underlying disease must be treated, otherwise attacks of this condition will often recur.