Parkinson's disease is one of the most complex neurological pathologies. It occurs mainly in older people; young people suffer from Parkinsonism in isolated cases. Treatment of the disease was unsuccessful for a long time, and the patients themselves were considered hopeless.
Breakthroughs in medicine and pharmacology have made it possible to create special drugs to help patients, however, for a significant category of patients, surgery for Parkinson's disease remains the only hope for improvement.
Postoperative prognosis
Surgery for Parkinson's disease is a matter of last resort. It is resorted to if conservative therapy does not give hope for improvement, or the patient has contraindications to taking medications.
Statistical results on the treatment of Parkinson's do not yet represent a breakthrough in medicine - 55% of patients have significant improvements after surgery, in a third of patients the improvements are questionable, and the condition of 15 percent of those operated on remains unchanged.
However, surgical intervention for such a disease is actively used in medical practice and therapy of this complex disease.
Forecast
If the patient's dominant symptom is tremor (shaking), then the prognosis will be much more favorable than in persons suffering from motor slowing. Today, the statistics are such that, due to active pharmaceutical development of the latest drugs, it is possible to prolong the life of patients and significantly improve its quality.
It is impossible to completely cure the pathology, and its specific prevention has not yet been developed. If contact with specialists was timely, and auxiliary treatment was chosen correctly, then further progression of the process can be stopped, maintaining working capacity and prolonging the patient’s life for a long time. If the disease is started by the lack of adequate therapy and self-medication, then this is fraught with a reduction in life expectancy to 7-9 years.
Contraindications
Surgical interventions for Parkinson's disease are not performed for all people suffering from this disease. For some people, hopes for treatment with surgery remain unfulfilled due to the presence of contraindications to surgery. It can be:
- severe depressive states;
- mental disorders;
- decompensated diseases of internal organs;
- focal lesions of brain tissue;
- coagulopathies (blood clotting disorders);
- dementia (dementia).

The surgical method is used in individual cases for patients with severe speech disorders. Therefore, for patients with speech disorders, operations do not guarantee an improvement in the situation and in some cases are not used.
They are not always inclined to perform surgery in cases where patients suffer from severe concomitant pathologies or are at risk of developing severe complications.
Types of surgical interventions
Help with the disease can be provided by several types of surgical intervention. For Parkinson's disease, operations are performed with fundamentally different approaches to eliminating the signs of pathology.
Thalamotomy
Surgical intervention using the thalamotomy method began to be performed for parkinsonism in the 50s of the last century. This was one of the first methods to help people with Parkinson's disease, and therefore thalamotomy had a number of side effects, as well as low postoperative effectiveness.

The essence of the surgical intervention was the destruction of the pathways in the thalamus and the destruction of the nuclei responsible for the occurrence of the impulse.
For a long time, thalamotomy was the only choice in the surgical approach to treating Parkinson's, and was also used in the treatment of other neurological pathologies.
In a modification of stereotactic thalamotomy, the operation involves the introduction for a certain period of time of electrodes that produce electrical stimulation of brain structures. During the destruction (destruction) of pathological foci, impulses in the ventrolateral and subthalamic nuclei either do not arise or are not carried out.

For parkinsonism, the operation gave good results - positive dynamics were noted in seventy percent of operated patients, however, statistics show that almost 65% had relapses.
Neurotransplantation
Neurotransplantation is a novelty in the surgical treatment of Parkinson's. The first operations were carried out by Swedish specialists more than thirty years ago. At first, the success of such an operation was not obvious, since it was not possible to completely cure people from parkinsonism, however, positive trends increased significantly, especially while taking medications.

The Swedish experience began to spread everywhere, and many clinics around the world began to use this method of radical therapy for parkinsonism. Patients were implanted with either a piece of tissue or a cell suspension. The transplant was embryonic tissue from four embryos of the first trimester of development.
As further studies confirmed, dopaminergic activity in the area of the transplant increased in the operated people . This made it possible to achieve the following results:
- Almost all patients experienced a decrease in motor symptoms of the disease to one degree or another.
- The duration of action of the key drug, Levodopa, increased.
- The characteristics of tremor changed, especially the indicators of movement deceleration and their ability to adapt.
- Improvements after surgery became obvious much earlier - in some patients they occurred immediately after surgery, and in others - within 3-6 months after surgery.
There are practically no complications in the surgical treatment of Parkinson's disease, since the embryonic tissue has a high survival rate and does not provoke postoperative risks.
To date, several hundred patients have already been operated on using this technique, but it is still difficult to compare the results, due to the difference in supportive conservative treatment in the postoperative period, various rehabilitation methods, etc. Reviews about the results of the operation are both positive and negative.
Pallidotomy
Pallidotomy is a type of surgery to treat Parkinson's disease. The operation was first performed in the 60s of the last century, but it was postponed for twenty long years due to hopes for the use of drugs for conservative treatment.
The technique became widespread only in the 90s. XX century Today, surgery is practically not used, since it has been replaced by deep brain stimulation.
The indication for surgical treatment by pallidotomy is the preservation of cognitive abilities in patients with motor abnormalities and “on-off” phenomena. Pallidotomy is also performed in patients with muscle spasms and hyperkinesia. When performing surgery for Parkinson's disease using pallidotomy, it is possible to intervene on only one side.

If surgery is necessary on the second side, it is performed no earlier than six months after the first operation . It has been noted that bilateral surgery is more fraught with complications than unilateral surgery, and in general, the unilateral method is better tolerated by patients, especially in old age.
Before surgery, all medications are stopped half a day before surgery. The surgeon makes a trefination hole in the skull and places an electrode near the area of interest. During the intervention, a conversation is held with the patient, his ability to think, speak, see and hear is assessed (operation under local anesthesia). During the operation, stimulation is performed at several points.
The first positive results can be seen after the operation. Surgery is much better tolerated than thalamotomy, but there is also a risk of complications.
Deep brain stimulation
Deep stimulation surgery is new. Used in patients with severe symptoms of Parkinson's disease. Surgical treatment of Parkinson's disease with this method makes it possible not to destroy brain cells, affecting healthy tissue.
The purpose of the procedure is to block electrical signals emanating from pathological foci . It is used as a method of therapy in seriously ill patients whose symptoms cannot be controlled with medications.
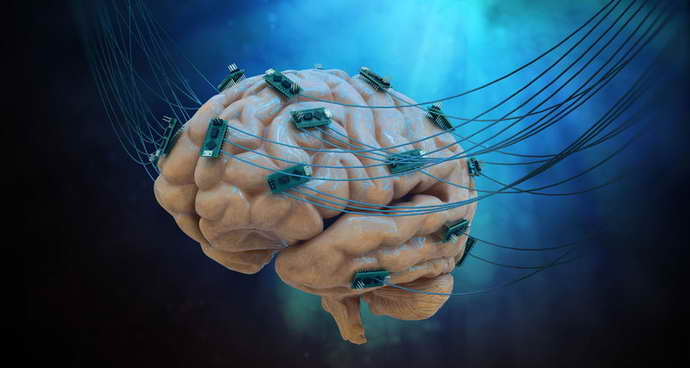
The blocking system is a pacemaker-like device that delivers impulses to target structures in the brain. Typically targets are the globus pallidus, thalamus, and subthalamic nucleus.
Deep brain stimulation
When medications fail to stop the progression of Parkinson's disease symptoms, surgery becomes inevitable. Thalamotomy and pallidotomy are performed only unilaterally, so their use does not always lead to the desired results. In addition, destruction of the structures of the central nervous system is associated with the likelihood of irreversible complications. Neurostimulation is considered an effective and gentle method of surgical treatment.
Neurostimulation is the introduction of an electrical stimulator into certain areas of the brain. Deep stimulation allows you to block unhealthy impulses, which has a positive effect on the patient’s motor functions.
Deep brain stimulation is prescribed for muscle rigidity, severe tremors of the limbs, and slowness of movement. Compared to drug treatment, neurostimulation provides a lasting effect.
Among the benefits of stimulation are:
- reducing doses of medications, and in some cases stopping them;
- the ability to change settings depending on the stage of therapy;
- the ability to completely remove the system in case of complications.
The implantation of the neurostimulation system is carried out by an experienced surgeon. The process includes two stages - implantation of electrodes into the brain structure, as well as installation of a neurostimulation device and its extension under the skin in the chest area. An extender is used to deliver the signal from the stimulator to the brain. Bilateral stimulation is possible, with two sets of electrodes and extensions installed.
The electrode is a thin wire with a diameter of up to one and a half millimeters. It is implanted in the area of the cerebral cortex, where signals from the neurostimulator are received through special contacts. The surgeon implants one or more electrodes, depending on the severity of the patient's condition.

The pulse generator is implanted under the skin in the chest area, usually 2-5 days after the first stage of the operation. The small device includes an electronic generator and an accumulator (or battery).
The doctor adjusts the device by setting the polarity and frequency, amplitude and duration of the pulses. During the adjustment process, the patient informs the doctor about his feelings, which allows him to select the optimal parameters. After turning on and setting up, the stimulator begins to send electronic impulses to the central nervous system through a wire system.
The patient remote control is used to turn the device on and off, select programs, and check the battery charge level. The battery-powered device is replaced every 5 years, from the battery 10. The battery is charged every 1-2 weeks, for two hours.
The effect after neurostimulation occurs within two months. Some patients note positive dynamics within a couple of days after turning on the stimulator. The disease becomes stable for a period of five years or more; in some cases, the effect persists for life.
How is surgery performed for Parkinson's disease - video
When choosing surgery for Parkinson's disease, the doctor takes into account the individual characteristics of the patient, the course of the disease, and the frequency of attacks.
If surgery is successful, patients may not always be able to stop taking medications, but in a significant proportion of cases, positive results lead to a gradual reduction in the volume of pills. The final recommendations for patients are given by the doctor leading the patient in the rehabilitation process.










