For most people, the phrase “craniotomy” evokes unpleasant feelings. Many have heard that such operations were performed in ancient times, but if necessary, they are successfully carried out today. Why is craniotomy done? What it is? In what cases is surgical intervention necessary, how scary is it and will a person be able to live a full life after such a procedure?
An operation performed with dissection of the soft tissues of the head and bones of the skull for the purpose of penetration and further examination or operation of brain tissue is called “craniotomy”. What does this mean and who is prescribed this treatment?
Indications for trepanation
Trephination can be prescribed to patients who have various brain diseases, cancer, edema, blood clots, problems with the blood vessels of the brain, nervous disorders, tissue infections and vascular disorders of the dura mater of the brain. Surgery is also prescribed for head injuries, fractures or depression of the skull bones, as well as to relieve intracranial pressure. Another indicator for the procedure may be a biopsy. The craniotomy operation allows you to remove a piece of brain tissue for subsequent research.
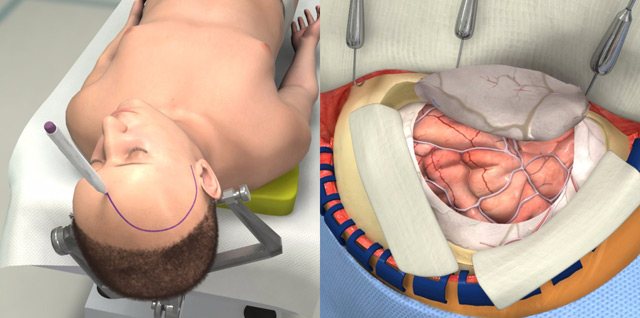
Craniotomy.
Craniotomy is a stage of neurosurgical operation, the essence of which is to “cut out” a section of the bone of the cranial vault to form a trepanation window to access the brain. At the end of the operation, the bone fragment must be put in place and, if necessary, fixed.
This is not a separate type of operation and must be indicated in its full name. For example, “Craniotomy. Removal of acute subdural hematoma" or "Craniotomy. Removal of an intracerebral tumor of the left frontal lobe.”
The term consists of two Greek words: cranion (Greek, kranion - skull) and tomia (Greek, tome - cut). Literally means an incision or dissection of the skull.
Types of operation
The procedure is carried out in different ways; which one will be prescribed for a particular patient is determined by the general indications and the nature of the disease.
- Osteoplastic craniotomy (traditional). In the process, a separate section of the cranial bone is cut out. Then a brain operation is performed, after which the removed part of the bone is returned to its place. If the procedure is successful, additional intervention is no longer required.
- Resection craniotomy. What does it mean? A small hole is made in the skull and expanded to the desired diameter. Unlike the first type, the opening of the skull is not closed with bone tissue after surgery. The brain is no longer protected by the bones of the skull; this function is performed only by the skin and soft tissues.
- Decompressive trephination involves making a small hole in the skull bone. This procedure is prescribed to patients to reduce intracranial pressure.
- An awake craniotomy is when a craniotomy is performed on a conscious patient. This procedure is necessary to monitor the functionality and response of the brain to certain manipulations by the surgeon. The patient does not experience pain.
- Stereotaxy. This type of research uses a computer. With its help, brain tissue is examined, which will then undergo surgery.
Craniotomy: consequences after surgery
Trephination is a complex type of neurosurgical operation, after which serious complications can occur. The procedure can either alleviate or worsen the condition. Despite the unpredictability of the operation, it remains the only chance of salvation for many patients.
Infectious complication
As with most surgical procedures, the risk of infection increases several times. Moreover, infection of brain tissue is a rare occurrence, which is due to the operation being carried out under extremely sterile conditions using disinfected instruments. More often wounds occur on the head. But they can be dealt with by maintaining hygienic care of the damaged area.
Attention! If pathogens have penetrated the membranes of the brain, there is a possibility of developing secondary meningitis. When the infection reaches the brain matter, encephalitis occurs.

Oddly enough, the lungs, kidneys, bladder, and intestines, whose functions are supported by a certain part of the brain, are more often affected by infections. The cause of infection can also be forced limitation of mobility and changes in the patient’s lifestyle after surgery. Treatment is aimed at eliminating pathogenic microorganisms using antibiotics. Therapeutic exercise, adherence to a daily routine, proper nutrition are preventive measures.
Blood clots and blood clots
Thrombosis or thromboembolism of any vessels is a serious outcome after craniotomy, which occurs due to the person’s low activity after the operation. Most often, blood clots form in the lower extremities. A detached blood clot can be transported by blood to the lungs. As a result of blockage of the pulmonary artery, thromboembolism occurs. When the clot reaches the heart, signs of a myocardial infarction appear. In such cases, only timely treatment can save a person.
To prevent blood clots, doctors recommend doing special therapeutic exercises in hospital, and then at home (after discharge). Sometimes medications that thin the blood are prescribed.
Neurological disorders
Most often, disorders of the central nervous system occur when, after trepanation, swelling of adjacent brain tissue is observed. The swelling usually goes away on its own within a few weeks without the use of medications. To speed up this process, diuretics are often prescribed.
Attention! Even if after craniotomy no deviations in the patient’s neurological status are observed, this does not mean that over time, symptoms of dysfunction of the central nervous system will not arise.

Long-term neurological disorders occur with severe damage to brain tissue. For example, impaired speech, mental function, motor activity. The severity of certain complications depends on the location of the damaged area.
Bleeding
Common consequences include bleeding, which can occur during surgery and immediately after it. This anomaly is due to the fact that a large number of vessels are damaged during trepanation. Therefore, the patient is given a drainage immediately after surgery (often after removal of the hematoma). The procedure is necessary to remove biomass. If this is not done, it will accumulate in the skull, compressing nerve fibers and motor centers.
In some cases, it is necessary to perform a second operation aimed at cauterizing or suturing the vessels. In order to avoid such manifestations during surgery, the patient is given intravenous anticonvulsant drugs in advance.
How to prepare for surgery
What does a patient scheduled for craniotomy need to know? What kind of procedure this is, how it will be carried out and how to organize your life for a speedy recovery after it - all these questions should be discussed with your doctor in advance. Before the operation, you should undergo all the necessary studies of the brain and nervous system, and take tests.

You should stop taking blood thinners and anti-inflammatory medications a week before surgery. Taking medications should be strictly controlled by a doctor; self-medication during such a period is unacceptable. Before the operation itself (12 hours before) you need to stop eating and drinking.
Care should be taken about who and how will be able to pick up the patient from the clinic after discharge, who will be able to help around the house during the recovery period and provide other care assistance.
What are the consequences for children and adults?
Among the consequences are:
- Infectious consequences that worsen the prognosis and rehabilitation: meningitis, meningoencephalitis, suppuration of the surgical wound, sepsis and septic shock.
- Disturbances in the functioning of analyzers: visual, auditory, olfactory.
- Epileptic seizures, up to status epilepticus. Paralysis, convulsive seizures.
- Changes in cognitive functions: memory, speech, attention, thinking.
- Brain swelling.
- Bleeding.
- Thrombosis of the cerebral veins and, as a result, stroke.
We must not forget one more cosmetic consequence: skull deformation. After resection trephination, the shape of the patient’s skull changes due to the fact that part of the bone is removed. At the site of the defect, a depression in the patient’s skull will be visible.
- coma;
- bleeding;
- frequent headaches;
- nausea and vomiting;
- elevated temperature;
- nervous disorders;
- swelling;
- hearing, vision, speech and memory impairments;
- malfunction of the digestive and urinary systems;
- convulsions;
- paralysis of limbs;
- infections.
Anesthesia
“How is craniotomy done and does it hurt?” - perhaps one of the most common questions from patients. The operation is in most cases performed under general anesthesia. The patient will not feel the trepanation itself or the surgeon’s manipulations with the brain tissue. After trepanation, painkillers will be prescribed.
In the case of stereotaxy, pain relief is prescribed locally. If a craniotomy is scheduled, during which the patient must remain conscious, general anesthesia will be provided for the period of the operation when the person is not required to remain conscious.
First aid and treatment
Please note that self-medication can only worsen the situation and lead to death, so be sure to consult a doctor.

Typically, first aid includes:
- covering a person’s head with ice packs to reduce pressure on the intracranial box;
- subcutaneous injection of a combination of piracetam and glucose (15 ml and 30 ml, respectively); oxygen therapy.
After first aid is provided, the patient is taken to the hospital, where the necessary examinations are carried out to determine the location of the swelling, its cause and rate of development. The department in which a person is hospitalized depends on the cause of cerebral edema.
During treatment, the following types of swelling elimination are used:
- oxygen therapy;
- special medications that are prescribed only by the attending physician;
- ventriculostomy (lowering intracranial pressure).
The rehabilitation time depends on the stage of the disease. If obvious signs of cerebral edema have disappeared, the patient continues treatment at home under the supervision of a doctor.
Operation process
After the patient is put under anesthesia, the scalp is carefully treated with an antiseptic. An incision is made to expose the required area of the skull. The trephinated skull bone is dissected, removed, and brain surgery is performed.
Once the intervention is complete, the exposed area of the brain is closed. The removed portion of the skull bone is returned to its original location, and surgical sutures are placed on the scalp. To ensure the outflow of fluid and remove blood, drainage tubes are inserted into the operated area, and a bandage is applied to the head. After a few days, the drainage can be removed. The operation itself lasts several hours.
The patient is then sent to the recovery room, where his vital signs are carefully monitored. Pulse, body temperature, breathing and blood pressure are checked regularly. After some time, the operated patient will be transferred to the intensive care ward, and then to the hospital ward.
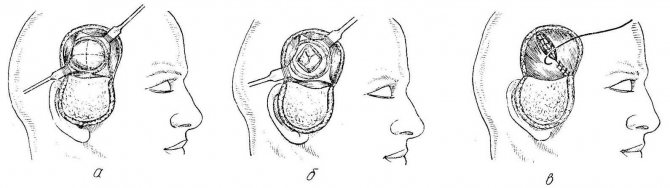
Resection trepanation
Resection trephination is performed to reduce intracranial pressure, which is why it is otherwise called decompressive. In this case, it becomes necessary to create a permanent hole in the skull, and the bone fragment is completely removed.
Resection trephination is performed for intracranial tumors that can no longer be removed, with a rapid increase in cerebral edema due to hematomas with a risk of dislocation of nerve structures. Its location is usually the temporal region. In this area, the skull bone is located under the powerful temporal muscle, so the trepanation window will be covered with it, and the brain will be reliably protected from possible damage. In addition, temporal decompressive trephination provides better cosmetic results compared to other possible trepanation sites.
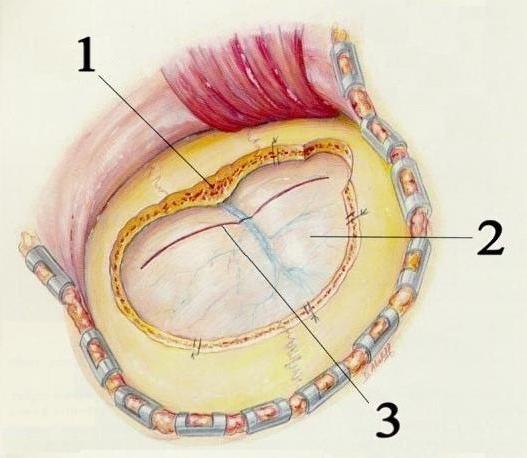
resection (decompressive) trephination according to Cushing
At the beginning of the operation, the doctor cuts out a musculoskeletal flap linearly or in the shape of a horseshoe, turns it outward, dissects the temporalis muscle along the fibers and incises the periosteum. Then a hole is made in the bone with a milling cutter, which is expanded using special Luer bone cutters. This results in a round trepanation hole, the diameter of which varies from 5-6 to 10 cm.
Postoperative period
After the end of the operation, which involved craniotomy, the restoration of the patient’s health begins immediately. The operation itself is quite complex and takes a lot of effort from the patient, so the rehabilitation process is very important. The patient will stay in the clinic from 3 to 7 days, the period depends on the severity of the operation and the patient’s health. If complications arise, the period of stay under the supervision of a doctor will be increased.

Rehabilitation
After craniotomy, a number of rehabilitation requirements must be observed: maintaining hygiene of the affected area, but without soaking it for a long period of time; eliminating physical stress on the head (especially head tilting); performing therapeutic exercises to eliminate stagnant processes; prescription of medications and herbal remedies.
In order to recover quickly after surgery to remove a brain tumor and return to normal life, competent rehabilitation will be required.
The rehabilitation period begins immediately after surgery and can last an average of two to four months.
It is very important to be constantly vigilant after treatment for a brain tumor in order to detect a possible relapse of the disease in time.
Hospital care
It will boil down to the following:
- The patient's head should be kept elevated to reduce blood pressure.
- Fluid intake will be limited, and if vomiting occurs, antiemetics will be prescribed.
- Medicines that reduce the amount of fluid in the body (steroids) may be prescribed.
- Antibiotics are used to prevent infection from occurring.
- After a day, the bandage can be removed from the head of the operated patient. The wound must be kept clean and under constant supervision.
- The patient should begin to walk a little as early as possible. This will prevent pneumonia or blood clots from occurring.
Upon returning home
Excessive stress after such a complex operation is contraindicated, as is playing sports. It will be very good if one of the relatives helps a person organize his life during the first time he stays at home. People after craniotomy often experience psychological stress and depression. They need to communicate with a positive person. Who else, if not your loved ones, can help with this. In some cases, you cannot cope with depression on your own, then you should seek professional help from a psychologist or psychotherapist.
It is equally important to follow the instructions and follow the recommendations of the doctor who will observe the patient who has undergone craniotomy. The consequences of surgery and the speed of recovery largely depend on postoperative care. The operated area of the head should be kept clean. You can’t keep the wound wet for a long time. If the scar changes color or something else goes wrong, you should see a doctor immediately.

Sports are contraindicated; you can’t even do yoga, because many exercises involve bending your head. But light exercise and walks in the fresh air will be beneficial. They will accelerate the blood and prevent the formation of blood clots. It is important to lead a healthy lifestyle, eat right and in a timely manner.
It is necessary to take medications prescribed by a specialist. Decoctions of medicinal herbs will be good aids in recovery, but before using them you should consult a doctor.
Treatment of complications
There are 3 approaches to treating brain tumors:
- Surgical procedures.
- Chemotherapy.
- Radiation therapy, radiosurgery.
Surgery
Surgery in the presence of brain tumors is a priority measure if the tumor is isolated from other tissues.
Types of surgical interventions:
- total tumor removal;
- partial removal of the tumor;
- two-stage intervention;
- palliative operations (alleviating the patient’s condition).
Contraindications for surgical treatment:
- pronounced decompensation on the part of organs and systems;
- tumor growth into surrounding tissues;
- multiple metastatic foci;
- patient exhaustion.
Contraindications after surgery
After the operation it is prohibited:
- drinking alcohol for a long time;
- air travel within 3 months;
- active sports with possible head injury (boxing, football, etc.) – 1 year;
- bath;
- running (it is better to walk quickly, this trains the cardiovascular system more effectively and does not create additional shock absorption);
- sanatorium-resort treatment (depending on climatic conditions);
- sunbathing, ultraviolet irradiation, because it has a carcinogenic effect;
- healing mud;
- vitamins (especially group B).
Chemotherapy
This type of treatment involves the use of special groups of drugs, the action of which is aimed at destroying pathological fast-growing cells.
This type of therapy is used in conjunction with surgery.
Methods of drug administration:
- directly into the tumor or surrounding tissue;
- oral;
- intramuscular;
- intravenous;
- intra-arterial;
- interstitial: into the cavity remaining after tumor removal;
- intrathecal: into the cerebrospinal fluid.
The choice of a specific drug for treatment depends on the sensitivity of the tumor to it. That is why chemotherapy is usually prescribed after a histological examination of tumor tissue, and the material is collected either after surgery or stereotactically.
Radiation therapy
It has been proven that malignant cells, due to active metabolism, are more sensitive to radiation than healthy ones. That is why one of the methods of treating brain tumors is the use of radioactive substances.
This treatment is used not only for malignant, but also for benign neoplasms if the tumor is located in areas of the brain that do not allow surgical intervention.
In addition, radiation therapy is used after surgical treatment to remove remnants of tumors, for example, if the tumor has grown into surrounding tissues.
Side effects of radiation therapy
- hemorrhage into soft tissues;
- scalp burns;
- skin ulceration.
- toxic effects on the body of tumor cell decay products;
- focal hair loss at the site of exposure;
- pigmentation, redness or itching of the skin in the area of manipulation.
Radiosurgery
It is worth considering separately one of the radiation therapy techniques that uses the Gamma Knife or CyberKnife.
This method of treatment does not require general anesthesia and craniotomy. Gamma Knife is high-frequency gamma irradiation with radioactive cobalt-60 from 201 emitters, which are directed into one beam, isocenter. In this case, healthy tissue is not damaged.
The treatment method is based on a direct destructive effect on the DNA of tumor cells, as well as on the proliferation of flat cells in the vessels in the area of the tumor. After gamma irradiation, tumor growth and blood supply are stopped.
To achieve the desired result, one procedure is required, the duration of which can vary from one to several hours.
This method is highly accurate and has minimal risk of complications. Gamma Knife is used only for diseases of the brain.
This effect also applies to radiosurgery. A cyber knife is a type of linear accelerator. In this case, the tumor is irradiated in different directions. This method is used for certain types of neoplasms to treat tumors not only of the brain, but also of other localizations, i.e., it is more universal compared to the Gamma Knife.
Consequences
This is the type of treatment that is prescribed when you need to choose the lesser of two evils. Skull surgery allows you to get rid of the most complex diseases, but at the same time the person is inflicted with an injury that will accompany him throughout his life. The human brain has not been studied as well as we would like, therefore any intervention can have the most unpredictable result, and this is precisely what craniotomy is. The consequences of the operation can be very different or not manifest themselves at all.
People who have undergone brain surgery are susceptible to increased intracranial pressure and are unable to perform complex mental and physical work. Many have to change their work activity and switch to a less paid, but easier one. Giving up your usual lifestyle can be difficult.
The success of the procedure is determined by many factors. Firstly, this is the severity of the disease or injury faced by the patient, and, of course, the qualifications of the surgeon. Physical health and maintaining a good lifestyle before surgery are also important. Smokers are most susceptible to postoperative complications.
Craniotomy: when necessary, implementation, rehabilitation
Author: Averina Olesya Valerievna, candidate of medical sciences, pathologist, teacher of the department of pathological anatomy and pathological physiology for Operation.Info ©
Craniotomy is rightfully considered one of the most complex surgical interventions. The operation has been known since ancient times, when they tried to treat injuries, tumors and hemorrhages in this way. Of course, ancient medicine did not allow one to avoid various complications, so such manipulations were accompanied by high mortality. Now trepanation is performed in neurosurgical hospitals by highly qualified surgeons and is intended, first of all, to save the patient’s life.
Craniotomy consists of creating a hole in the bones through which the doctor gains access to the brain and its membranes, vessels, and pathological formations. It also allows you to quickly reduce the growing intracranial pressure, thereby preventing the death of the patient.
An operation to open the skull can be carried out either plannedly, in the case of tumors, for example, or urgently, for health reasons, in case of injuries and hemorrhages. In all cases, there is a high risk of adverse consequences, since the integrity of the bones is compromised and damage to nerve structures and blood vessels is possible during the operation. In addition, the reason for trepanation itself is always very serious.
The operation has strict indications, and the obstacles to it are often relative, since in order to save the patient’s life, the surgeon can neglect concomitant pathology. Craniotomy is not performed in terminal conditions, severe shock, septic processes, and in other cases it can improve the patient’s condition, even if there are serious disorders of the internal organs.