Diseases of the femoral nerve include neuritis and neuropathy. Neuritis is a disease characterized by inflammation. This is how it differs from neuropathy (in other words, neuropathy). The disease represents any dystrophic, degenerative changes in the large nerves included in the lumbar plexus. With neuritis, various nerve fibers of the peripheral nervous system, including the femoral one, can suffer. If several nerves are affected, doctors diagnose polyneuritis. A disease called neuritis of the femoral nerve, symptoms and treatment of the disease is the topic of this article.
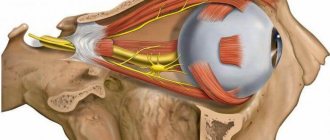
Topography of the femoral nerve
The femoral nerve, the anatomy of which largely explains the causes of the symptoms of neuritis, is classified as peripheral. It originates in the lumbar plexus. The nerve fiber enters the thigh from the pelvic area under the inguinal ligament. It supplies nerves not only to the muscular part of the thigh, but innervates certain parts of the foot and lower leg. This nerve is the most significant in the lumbar plexus. Its large length gives rise to a high frequency of damage.
The bodies of nerve cells are located in the spinal cord, so this is where the nerve impulse originates. A nerve consists of a nerve trunk in which individual fibers are isolated from each other by the myelin sheath. This sheath also supplies the nerve. On top of it there is connective tissue, and along the entire length the fiber is equipped with small arteries.
Nerve plexuses are formed by processes of nerve cells that emerge from the spinal cord and then from the foramina between the vertebrae. Branches of peripheral nerves emerge from them. The reliability of the nervous system is characterized by the fact that the branches of one nerve fiber are formed with the participation of different spinal roots.
Close in location to the femoral nerve is the femoral-genital nerve. It is responsible for the innervation of the muscles of the pelvic floor. The main sign of its damage is pain in the places that it supplies nerves. This is the area of the rectum, anus, genitals, perineum, and also the urethra. If its work is disrupted, a person begins to develop diseases of the genital area. Most often, discomfort occurs in a sitting position.
Topographic anatomy of the cutaneous nerves of the brachial plexus
The lateral cutaneous nerve of the shoulder bypasses the deltoid muscle and is considered the terminal branch of the axillary nerve. It follows the posterior region of the deltoid muscle and the upper posterolateral part, innervating the skin of this area. It has only afferent fibers, so its damage does not impair movement functions.
The medial cutaneous nerve of the shoulder follows from the medial brachial fascicle and perforates the axillary fascia with several branches.
In the area of the axilla, it merges with the lateral branch, founding the intercostobrachial nerves, which together innervate the skin of the medial region.
The posterior cutaneous nerve of the shoulder begins from the axilla, perforates the fascia of the shoulder, divides in the area of the posterolateral part, innervating its skin.
The medial cutaneous nerve of the forearm arises from the 8th cervical and 1st thoracic nerves, passes through the axilla, joins the brachial artery, and descends to the forearm.
Responsible for the anteromedial zone of the forearm.
The lateral cutaneous nerve of the forearm constitutes the terminal branch of the musculocutaneous nerve.
It perforates the fascia of the shoulder and innervates the skin of the lateral forearm.
Why is the femoral nerve affected?
The following reasons usually lead to inflammation of the femoral nerve, which are based on the predominance of cold over heat in the body:
- hypothermia (Cold often serves as a source of diseases of the nervous system);
- bruises, dislocations, fractures (Injuries are dangerous because they cause neuritis and neuropathy);
- inflammation of the pelvic organs (or rather, in one of the organs. This could be the bladder, ureter, prostate gland, rectum, vagina, etc.);
- problems with blood vessels (Compression, pinching of the trunk of the femoral nerve. The cause of this may be a hernia, osteochondrosis, compression occurs during pregnancy, childbirth or surgery);
- intoxication;
- infection (flu, herpes, diphtheria and others).
A general weakening of the body and a lack of vitamins can also lead to neuritis. Interestingly, the disease can appear in people of any age and even in children.
Symptoms of the disease
In most cases, changes in the body manifest themselves gradually. Initially, numbness may occur in areas of the skin on the side of the thigh, then spread to the front. A sensitivity disorder occurs - sensations of burning, coolness, tingling, etc. occur. At the initial stage of the disease, these manifestations are temporary, but with the development of pathology they become permanent. There is pain and difficulty walking. In certain cases, hair loss and thinning of the skin may occur.
Symptoms
Numbness, tingling, goose bumps on the inner and front surface of the thigh.
- Drawing pain along the nerve.
- Bending of the leg in the area of the knee and hip, its movement is difficult. Impaired gait.
- Swelling in the knee and ankle area.
- Depigmentation of the skin at the site of injury.
Hair loss and tropical ulcers sometimes occur. You may also experience general muscle weakness in the affected area.
Femoral nerve compression is also called tunnel syndrome and is a condition related to neuropathy of the lower extremities. It is associated with tissue compression in the area where the inguinal ligament emerges. This disease can easily be confused with neuritis, because the symptoms of the lesions are similar:
- Discomfort and pain in the groin area.
- Lameness during exercise.
- Decreased sensitivity, as well as numbness in the groin area.
- Cramps at the site of the lesion in the groin area.
Among the types of tunnel syndrome, Rott's disease is distinguished. Carpal tunnel syndrome, like neuritis, occurs for certain reasons, which the doctor must identify when starting treatment for the disease. They may turn out to be serious pathologies.
Where is the root of the problem?
Neuropathy of the external cutaneous nerve of the thigh can develop for several reasons. First of all, doctors highlight the following:
- compression of the nerve, which occurs due to anatomical features in the structure of the body - most often compression occurs when bending or rubbing the legs;
- another reason may be excess weight, fat deposits in the thigh and peritoneum;
- tumors and hematomas;
- complications after surgery or an inflammatory process occurring in the abdominal cavity;
- constant wearing of a tightly tightened belt or tight, synthetic underwear, corsets;
- sedentary, sedentary and inactive lifestyle and malnutrition of the affected nerve, as well as degenerative changes occurring in the spine.
In addition, the cause of nerve damage and the development of Bernhardt-Roth disease can be a previous injury, as well as occupational ailments that are inherent in certain categories of professions.
Alternative Treatments
Psychosomatics is of considerable importance for the treatment of neurological diseases. The root of all alternative treatments for neuritis is the belief that all diseases have an internal cause.
For example, Tibetan healers believe that the cause of the development of the disease neuritis of the femoral nerve is an imbalance in the body. It is believed that the body, through illness, signals that there is no harmony in it. Alternative treatment aims to restore harmony and balance to the body. It is complex in nature. The following methods are used:
Lifestyle changes (optimal habits in organizing the day and nutrition are selected based on the individual constitution of the person).
Diagnosis and treatment
Before prescribing a course of treatment, the patient must undergo a full examination, since the disease can be mistaken for a bruise or other pathological condition. Diagnosis is carried out using the following methods:
- electroneuromyography;
- MRI and ultrasound;
- computed tomography and x-ray.
If the preliminary diagnosis is obvious to the doctor, doctors limit themselves to ordering an X-ray examination of the patient, but if there are certain doubts, they most often prescribe an MRI.
Drug course of therapy
Treatment of Bernhardt-Roth disease involves the prescription of medications, therapeutic exercises and physiological procedures.
Regarding the medicinal course of therapy, its main task is to eliminate swelling and inflammation in the area of damage and pinched nerves, and reduce pain.
For this purpose, drugs classified as NSAIDs are prescribed, as well as a course of B vitamins. If the disease is advanced, and drug treatment and physical therapy do not provide positive treatment dynamics, in extreme cases, surgical intervention is prescribed.
For the most part, physiotherapeutic procedures are aimed at eliminating pain and relieving swelling. The most commonly prescribed methods of influence are:
- acupuncture and reflexology;
- radon or hydrogen sulfide therapeutic baths;
- course of therapeutic massage and mud therapy.
At home, the patient can practice exercises from the course of therapeutic gymnastics - bending the legs at the knee joint, swinging the legs, or spreading them to the side. Also an important component of effective treatment is weight control, removal of tumors, and timely treatment of pathologies of the hip joint, if the latter were the direct causes of the development of the pathology.
Pain relief is carried out by doctors using a course of anti-inflammatory medications and analgesics; in more severe and advanced forms they are administered by injection.
In this case, the doctor administers Lidocaine or Novocaine or performs a pain blockade by administering glucocorticoids.
Neuropathy in the brachial plexus
Neuropathy refers to pathological diseases caused by muscle dysfunction of a particular group.
Damage to the brachial cutaneous nerves can be caused by the following factors:
- injuries after childbirth;
- squeezing;
- suppression from tumor;
- radiation exposure;
- congenital abnormalities;
- intoxication;
- inflammatory processes;
- endocrine pathologies;
- hormonal disorders;
- physical damage;
- autoimmune pathologies.
Symptoms of the lesion
The main symptoms are constant or recurrent pain and lack of sensitivity. The pain syndrome is often accompanied by a feeling of intense burning and tingling, causing discomfort to the patient.
Neuropathic pathologies cause the following symptoms:
- loss of sensitivity - numbness;
- goosebumps and burning sensation;
- pain;
- muscle weakness in the arms.
During the initial development of the pathology, no pain is observed, only numbness, tingling and tightness of the skin. As the disease progresses, symptoms become more pronounced. The pain increases after physical activity.
Aching or sharp piercing pain appears in the shoulders, elbows and hands, limitation or loss of mobility, or even complete paralysis.
Diagnostics
Diagnosis of the disease implies:
- examination by a specialist;
- blood analysis;
- chest x-ray;
- Ultrasound;
- electromyography.
In rare cases, a biopsy is prescribed.
Therapy methods
Treatment of brachial nerve neuropathy depends on the severity and specificity of the pathology.
For sprains, painkillers and anti-inflammatory ointments can be used.
To relieve pain, drugs of the analgesic and anti-inflammatory group are used (Brustan, Nimesulide, Ibuklin, Ketanov). For severe pain, local anesthetics (Novocaine, Lidocaine) and glucocorticoids (hydrocortisone, Diprospan) are used.
Physiotherapeutic procedures - mud, massage, darsonvalization - will help restore mobility and prevent atrophy.
Multivitamin preparations, which include Benfotiamine and Cyanocobalamin, play an important role in therapeutic treatment.
If drug therapy is ineffective, surgical intervention must be resorted to.
Pudendal neuralgia
Pudendal (from Latin pudenda - “external genitalia”, derived from pudendum, literally meaning “parts to be ashamed of”) neuralgia (from Greek.
neuron, "nerve" + algos, "pain" is pain in the innervation zone of a nerve or nerves) is a chronic, neuropathic, pelvic pain that is often misdiagnosed and inappropriately treated.
It occurs in both men and women, although research suggests that 2/3 of cases are found in women.
The main symptom of the disease is pain in the genital or anal-rectal area, and the pain intensifies when sitting.
Pain occurs in the pelvic area and can occur on one side or both sides of the body. Patients suffering from pudendal neuralgia describe the pain as burning, stabbing or aching, stabbing.
The sensations are compared to squeezing, twisting and even numbness.
The term pudendal neuralgia (PN) is used interchangeably with “pudendal nerve entrapment,” although one 2009 study concluded that “the prevalence of PN is unknown and is probably rare.”
Additionally, the same study states that “there is no evidence that would equate PN with pudendal nerve entrapment.”
This means that a patient can have all the symptoms of a pinched pudendal nerve listed in Professor Robert Nantez's 2006 criteria, without having the pinched nerve itself.
Clinical anatomy
Sacrococcygeal plexus
The pudendal nerve is a paired nerve, the branches of which are located on the right and left sides of the human body.
- Nerve roots – S2-S4
- Sensory branches - innervate the external genitalia of men and women, as well as the skin around the anus, anal canal and perineum.
- Motor branches - innervate a number of pelvic floor muscles, the external urethral sphincter and the external anal sphincter.
- Autonomic - carry sympathetic nerve fibers to the skin of the dermatomal area S2-S4.
Entrapment of the pudendal nerve at different levels (sciatic spine, sacrospinous and sacrotuberous ligaments, Alcock's canal) is the cause of disabling, chronic and intractable pelvic pain. This pain is highly varied and complex because it is often associated with a variety of functional symptoms that are confusing.
Pathophysiology
Pathological conditions associated with damage to the pudendal nerve
The exact mechanism of nerve dysfunction and damage depends on the etiology. Damage may be one or two sided.
The causes of PN can be compression, stretching, direct trauma to the nerve, radiation. Pudendal neuralgia is a functional pinching in which pain occurs during compression or stretching of the nerve.
Symptoms worsen over time due to repeated microtrauma, ultimately leading to persistent pain and dysfunctional complaints.
The pudendal nerve becomes pinched during prolonged sitting or cycling.
Pudendal neuropathy can be caused by stretching of the nerve due to straining during labor or constipation. Other etiological factors include fitness classes, working out in the gym, weighted squats, leg presses, karate, kickboxing and roller skating.
Sports popular among young people are considered a risk factor, which may be associated with bone remodeling of the ischial spine. Vibration injuries can occur from driving on rough roads and agricultural fields.
Pudendal neuralgia can also be caused by falling on the buttocks.
Clinical picture
The clinical characteristic of PN is pain in the pelvic area, which increases during the day while sitting and decreases if the patient gets up or lies down.
Symptoms also include sexual dysfunction and difficulty urinating and/or defecating. To confirm the diagnosis, it is recommended to use the Nantes criteria.
The pain is similar to that experienced by patients with compression neuropathy.
In most cases, patients describe neuropathic pain as burning, tingling, or numbness that worsens when sitting.
At an early stage, the pain may only appear while sitting, but over time it becomes more or less constant and only gets worse from sitting. Many patients with PN are unable to sit down at all.
It is curious that sitting on the toilet is much less painful for them, which is most likely due to the fact that in this case the pressure is not on the pelvic floor muscles, but on the ischial tuberosities.
Basically, pain with PN only gets worse as the day goes on.
Diagnostics
Professor Robert Nantes' criteria for diagnosing PN
Diagnosis of PN is very difficult, since there are no specific tests for this disease. That is why a thorough history and physical examination are of great importance.
Diagnostic criteria developed by Professor Robert Nantes have become widespread.
According to his theory, five criteria must be present for PN: (1) pain is limited to the area supplied by the pudendal nerve; (2) pain predominates while sitting; (3) the pain does not cause the patient to wake up; (4) no objective sensory defects; (5) the positive effect of injections of painkillers.
Objectively, these criteria reflect the patient’s basic functional level at the beginning of therapy. Once treatment has begun, the same criteria can be used to determine the progress and effectiveness of treatment.
Physical examination for PN focuses on routine neurological evaluation of the pudendal nerve. Sensitivity is determined using a pin prick on each branch of the nerve on both sides.
The dorsal nerve (innervates the female clitoris and head of the penis), the perineal nerve (the posterior area of the labia and scrotum) and the inferior rectal nerve (the posterior area of the perineum) are checked. Hyperalgesia occurs much more often in patients than hypoalgesia.
Normal pinprick sensitivity may occur even if quantitative sensory testing is abnormal. Pressure is applied to the nerve in the Alcock canal, medial to the ischial spine, to produce pain, urinary, or rectal symptoms (Valleix phenomenon).
MRI allows classification of PN depending on the area of nerve entrapment: type I - in the area of the sciatic notch, type II - the ischial spine and sacrosciatic ligament, type IIIa - obturator internus muscle, type IIIb - obturator internus and piriformis muscles, and type IV - pinching of the distal branches of the pudendal nerve.
Differential diagnosis
- Gender-neutral pathologies: Tarlov cysts, coccydynia, chronic pelvic pain (CPP), sciatica, persistent sexual arousal syndrome (PGAD).
- In men: abacterial chronic prostatitis, prostatodynia, idiopathic proctalgia.
- In women: vulvodynia, chronic pelvic pain, endometriosis, vaginismus.
Outcome assessment
- Visual analogue scale (VAS).
- McGill Pain Questionnaire (MPQ).
- Questionnaire for diagnosing the type of pain (Douleur Neuropathique 4 questions - DN4).
- Brief Pain Inventory - Short Form (BPI-sf).
Invasive treatment
These interventions are performed by experienced doctors:
- Surgical release of the pinched pudendal nerve (in some cases, patients may experience pain after surgery and will need the help of a physical therapist to recover).
- Botox/botulinum toxin injections (type A).
- Pulsed high-frequency stimulation of the pudendal nerve, sacral nerve roots or sacroiliac joint.
- Cortisone injections.
- Platelet-rich plasma (PRP) injections.
- Hyaluronic acid injections.
- Neuromodulation using implanted electrodes.
Selection of candidates for surgical treatment must necessarily include a single diagnostic injection of an anesthetic into the area of the pudendal nerve. Let us recall that this procedure represents the fifth criterion for diagnosing PN according to Nantes.
Clinical management of the patient depends on the cause of the nerve injury. When the cause is not obvious, patients are advised to try the least invasive and least risky treatments first.
Non-invasive or conservative therapy
Photos from the seminar on women's health
Friends, Marina Osokina’s seminar “Women’s health: opportunities for restorative fitness and physical therapy” will take place very soon. Find out more...
Physical therapy
The long-term goals of physical therapy are pain relief and improved quality of life.
Physiotherapeutic analysis includes a motor assessment of the patient. It can help detect inappropriate movement patterns that may be causing symptoms of the disease. The analysis also often includes examination of the pelvic muscles (done with great care), which makes it possible to determine the ability of these muscles to contract and relax.
Treatment includes:
- conversation with the patient about the mechanism of pain;
- correction of the biomechanics of movements, body position or activity of the patient;
- internal manual therapy to facilitate healthy muscle contraction and relaxation (if applicable).
Pelvic floor muscle relaxation exercises (PFM)
This is the most preferred strategy for those physical therapists who specialize in pelvic diaphragm dysfunctions and disorders.
Peter Doran and Michel Coppetiers, two Australian physical therapists, conducted a study in which, among other things, they reported a protocol for the treatment of pelvic girdle pain due to pudendal nerve lesions.
They have had great success with a small group of patients using externally guided techniques to mobilize the sacroiliac joints, reducing tension on the sacrotuberous and sacrospinous ligaments. This is a noninvasive approach that should be considered before more aggressive approaches are attempted.
Self-help for PN:
The patient should use a pillow/cushion (donut or C-shaped) that supports the ischial tuberosities and elevates the pelvic floor off the seat. This support relieves excess tension from the MTD and the pudendal nerve. The patient should also avoid positions and movements that provoke pain.
Treatment uses exercises that relax the tense pudendal nerve and provide temporary pain relief:
- Bridge with legs wide apart.
- Swing your legs back in a standing position.
- Abduction and extension of the legs in a side lying position.
- Leg extension in the knee-wrist position.
- Cobra pose.
- Back arches.
The effectiveness of special exercises or yoga asanas in the treatment of chronic pudendal neuralgia has been little studied and requires more thorough research.
Forecast
Pudendal neuralgia greatly affects the patient’s quality of life, but does not affect its duration. Many patients with PN reported on medical forums and support groups that they also experienced depression and a constant feeling of discomfort. However, after correct diagnosis of the disease and with treatment, these symptoms gradually decreased.
Conclusion
Pudendal neuralgia is a painful neuropathic condition that affects areas of the dermatome innervated by the pudendal nerve.
It should be suspected if the patient complains of burning pain in the clitoris/penis, external genitalia in women/scrotum in men, perineum and rectum. Typically, the pain is worse when sitting and decreases or goes away when the patient stands.
It often appears immediately after vaginal surgery, pelvic trauma, or childbirth. To diagnose PN, the Nantes criteria are used. CT-guided pudendal nerve blocks are more accurate than transvaginal injections.
At the very beginning of treatment, factors that provoke pain should be minimized (these include certain actions, positions, movements), and medications should also be used at the initial stage. Physical therapy and Botox injections are used in patients with myalgia MTD.
If conservative treatment does not produce results, then surgical treatment is used: surgical decompression of the pudendal nerve, or pain blocking methods. Knowledge and best practices in this area are rapidly evolving, and changes in diagnosis and treatment protocols for PN are expected in the future.
Source: Physiopedia - Pudendal Neuralgia
Source: //kinesiopro.ru/blog/pudendalnaja-nevralgija/
Pelvic neuralgia: types, symptoms and treatment features
Pelvic neuralgia is a disease that is equally common in both men and women. It is accompanied by pain in the back and pelvic organs, and causes a lot of unpleasant sensations. Pain in this case is caused by damage to the nerve fiber located in the hip area.
In terms of symptoms, neuralgia has similar symptoms to diseases associated with the functioning of the genitourinary system, so women, when the first pain appears, often consult a gynecologist, and men, a urologist. But the test results indicate the absence of infections, and then the doctor orders a comprehensive examination, including an examination by a neurologist. It is he who, based on the nature and location of the pain, will be able to make an accurate diagnosis and prescribe the necessary treatment.
Causes of the disease.
Cutaneous nerves of the lower limb
The lateral cutaneous nerve of the thigh begins from the pelvic cavity, descends, branching from the knee joint, passing to the outer and partially anterior surfaces. It is considered afferent and is responsible for sensitivity. Neuropathy does not impair the motor mechanism.
The medial cutaneous nerve of the thigh emerges from the cruciate plexus, penetrates the gluteus maximus muscle, descends along the posterior surface, reaching the popliteal fossa, branching into the lateral and medial regions. It is considered centripetal. Responsible for the lower part of the buttocks and the back of the thigh. Neuropathy disrupts the forms of sensitivity in the area of innervation.
The medial cutaneous nerve of the calf arises from the popliteal cavity, descends along the gastrocnemius muscle to the junction with the peroneal branch.
The lateral cutaneous nerve of the calf lies on the dorsum of the foot and fuses with the posterior cutaneous nerve.
Topographic anatomy of the femoral nerve: