Meningoencephalitis is an infectious disease of the meninges and brain matter, combining the symptoms of meningitis and encephalitis. Caused by pathogens of various natures. It can develop as a separate disease or be a complication of other dangerous diseases. It can also affect the spinal cord. It is almost never cured without consequences, it can cause paralysis, coma, and in about 10% of cases it is fatal.
In the International Classification of Diseases system, ICD-10 is designated by code G04.
Causes of disease
Meningoencephalitis can occur as a reaction to a pathogen, a response from the body's immune system, or as a complication of intoxication. According to the criterion of the causes of the disease, infectious, autoimmune and toxic meningoencephalitis are distinguished. Occasionally, a post-vaccination type of illness also occurs - a reaction to vaccination.
The causative agents of infectious diseases include bacteria, viruses, fungi, parasites, and protozoan microorganisms (amoebas) from open water bodies. The most common forms of infection are viral and bacterial.
According to the type of pathogen, meningoencephalitis is divided into bacterial, viral, fungal and protozoal.
The disease can be transmitted by contact, ingestion of purulent secretions, including airborne droplets.
Classification (forms) of meningoencephalitis
Forms of the disease are usually classified according to various criteria. One of the most basic is the root cause of the development of the disease.
Primary meningoencephalitis is an independent disease caused by:
- ixodid tick bite;
- infection with the herpes virus, infection with rabies, typhoid, neurosyphilis;
- penetration of protozoan microorganisms (toxoplasma, amoebae and others) from dirty water from natural reservoirs onto the mucous membranes.
Secondary meningoencephalitis usually develops against the background of other diseases and traumatic conditions. It can become a complication:
- ARVI;
- pneumonia;
- other purulent pathologies of the ear, throat, respiratory system;
- measles, chickenpox;
- tuberculosis;
- traumatic brain injuries, especially in the presence of open wounds with fractures of the skull bones, dangerous for infection.

According to the nature of the course, meningoencephalitis occurs:
- acute, in which the clinical picture develops within 1-2 days from the onset of infection;
- subacute, the symptoms of which appear 3-8 days after contact with the pathogen;
- fulminant, the symptoms of which occur in a short time (from several hours to 1 day); is very difficult and can lead to death;
- chronic, with periods of exacerbation and remission, which lasts several months or years.
In addition, based on the nature of impurities in the cerebrospinal fluid and affected tissues, the following are distinguished:
- purulent meningoencephalitis (the inflammatory process occurs with the release of pus, a large proportion of leukocytes is detected in the puncture of the cerebrospinal fluid);
- serous meningoencephalitis (cerebrospinal fluid is transparent, but leukocytosis is detected);
- hemorrhagic type of disease (there is an admixture of blood in the cerebrospinal fluid, since the inflammatory process affects the walls of the brain vessels, thereby compromising their integrity).
Stages of the disease
The course of meningoencephalitis is characterized by several stages, which may differ for different types of disease:
- Latent (hidden, incubation) stage – observed in infectious types of the disease. Sometimes it is also called the precursor stage. It varies in duration depending on the etiology.
- The initial stage is the appearance of the first characteristic symptoms of the disease.
- The height of the disease - pronounced manifestations of pathology progress or fade. The apogee of the course of the disease.
- Some types of disease have a stage of paralysis and other pathological abnormalities of the central nervous system (mental disorders, etc.).
- The outcome of the disease is death or recovery with certain consequences.
Bacterial meningitis
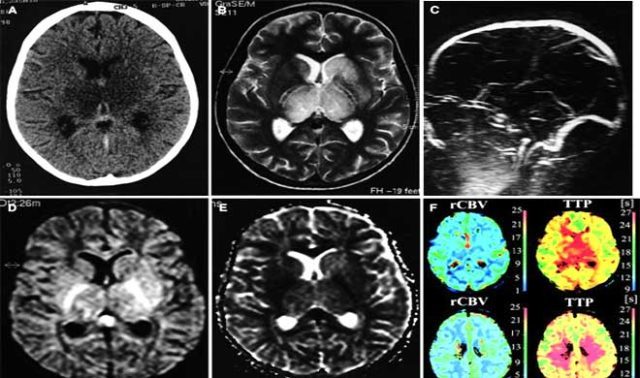
If bacterial meningitis is suspected, cerebrospinal fluid should be examined within the first 30 minutes, and if the results confirm the diagnosis of acute bacterial meningitis, antimicrobial therapy should be initiated depending on the results of Gram staining or bacterial antigen tests. However, if no causative agent can be identified or lumbar puncture cannot be performed within the first 30 minutes, empirical antimicrobial therapy should be started (adjusted based on the patient's age) as soon as blood samples are obtained. In patients with suspected bacterial meningitis who have local neurological manifestations or papilledema, a computed tomography scan (CTS) should be performed before lumbar puncture to rule out an intracranial neoplasm. In such a situation, performing a lumbar puncture is associated with the risk of cerebral hernia. However, performing CTS requires additional time, so antimicrobial therapy should be started immediately, given the risk of delaying treatment. Of course, the value of cerebrospinal fluid culture in patients receiving antimicrobial treatment (if lumbar puncture is delayed until CTS results are available) is significantly reduced, but the results of cerebrospinal fluid parameters, Gram stains, bacterial antigen tests, and blood samples obtained before treatment are likely to confirm the presence or absence of bacterial meningitis.
Recommendations regarding which drug should be empirically prescribed in an emergency situation for suspected bacterial meningitis have changed due to the development of resistance to a number of drugs in microorganisms. Although N. meningitidis strains exhibit relative resistance to penicillin G at minimum inhibitory concentrations (MICs) of 0.1 to 1 μg/ml, patients in whom these isolates are found improve after standard penicillin therapy. Moreover, the prevalence of penicillin-resistant meningococci has not yet reached levels of serious concern everywhere. Thus, in the USA it remains low and has not changed significantly over the past 10 years. For these reasons, we took into account changes in the susceptibility spectrum of H. influenzae type B and S. pneumoniae when making recommendations for empirical antimicrobial therapy.
H. influenzae type B If meningitis caused by H. influenzae is suspected, when prescribing empirical treatment, it must be taken into account that many strains produce P-lactamase; these strains accounted for 24% of all isolates in a US study between 1978 and 1981, and 32% in another US study in 1986. Resistance to chloramphenicol has also been described, with more than 50% of isolates being resistant in a report from Spain . Even in patients in whom chloramphenicol-susceptible isolates are found, the use of chloramphenicol is less preferable from a bacteriological and clinical point of view than the use of ampicillin, ceftriaxone, or cefotaxime for bacterial meningitis in childhood. The second-generation cephalosporin cefuroxime initially appeared to be as effective as the combination of ampicillin and chloramphenicol for bacterial meningitis in childhood, but its effectiveness has been questioned in more recent studies. Thus, in a study in which cefuroxime (Zinnacef, Zinnat, Ketocef) was compared with ceftriaxone in the treatment of bacterial meningitis in children, both regimens were effective, but with ceftriaxone it was much more likely to achieve CSF sterilization (0% versus 9% positive cultures after 24 h) and hearing impairment was less common (11% vs. 18%). Another randomized trial also compared cefuroxime with ceftriaxone in the treatment of bacterial meningitis in children; demonstrated faster CSF sterilization (2% vs. 12% positive cultures at 18–36 hours) and lower incidence of hearing loss (4% vs. 17%) in patients receiving ceftriaxone. This and other studies have confirmed that third-generation cephalosporins (especially cefotaxime or ceftriaxone) are as effective as ampicillin in combination with chloramphenicol for bacterial meningitis in children, predominantly caused by H. influenzae type B, and can be recommended as the drug of choice for empirical antimicrobial therapy for bacterial meningitis in children.
S. pneumoniae The need to take into account the spectrum of resistance to antimicrobial drugs has also led to changes in recommendations regarding empirical therapy for suspected pneumococcal meningitis, as strains have emerged that exhibit relative (MIC 0.1 - 1 μg/ml) or high (MIC greater than or equal to 2 µg/ml) resistance to penicillin G. Almost all resistant strains isolated from cerebrospinal fluid belong to serotypes 6, 14, 19 and 23; Most of the multidrug-resistant strains isolated in the United States have disseminated from the serotype 23 F clone, which was discovered in Spain back in 1978. The frequency of detection of penicillin-resistant pneumococci is increasing throughout the world. An American study conducted from 1979 to 1987 showed that 4.5% of pneumococcal strains showed relative or high resistance to penicillin; in a later study (1991 - 1992), 16.4% of pneumococcal isolates showed resistance to at least to one of the following antimicrobial drugs: penicillins, cephalosporins, macrolides, cotrimoxazole (Bactrim, Biseptol, Septrin) and chloramphenicol. Another American observation (1994) showed that the level of resistance to penicillin was about 20%. In Spain, the incidence of resistance increased from 6% in 1979 to 44% in 1989; the highest incidence was observed in Hungary (58% based on surveillance data from 1988 to 1989). The following factors have been reported to predispose to resistance: age of the patient (younger than 10 or older than 50 years), immunosuppression, prolonged hospital stay, children in day care, infection with serotypes 14 and 23, frequent or prophylactic use of antimicrobials (for example, to prevent inflammation of the medial ear).
Some alternative drugs for the treatment of meningitis caused by penicillin-resistant pneumococci have been tested only in vitro or in animal models, and we have chosen to limit the discussion to drugs that have undergone clinical trials. One such drug is chloramphenicol. However, resistance and clinical failure occur even in cases where the body is sensitive to chloramphenicol: in one study, 20 of 25 children showed a poor clinical response or had residual effects, and some even died. Although disc testing showed the sensitivity of the microorganism, the minimum bactericidal concentration of chloramphenicol for penicillin-resistant pneumococcal isolates was significantly higher than that for penicillin-sensitive isolates, so only subtherapeutic levels of bactericidal activity were achieved and treatment failed. Third-generation cephalosporins are considered the drug of choice for pneumococcal meningitis that exhibits relative resistance to penicillin, but there are reports of therapy failure and pneumococcal strains unexpectedly demonstrating resistance to these cephalosporins (MIC increased from 4 to 32 μg/ml or more).
Dexamethasone Some people with acute bacterial meningitis need immediate treatment with dexamethasone. This is done to mitigate the inflammatory response in the subarachnoid space associated with antibiotic-induced bacterial lysis and the multiple pathophysiological consequences of bacterial meningitis, such as cerebral edema and increased intracranial pressure. Studies conducted in the last 10 years (& adjunctive dexamethasone (0.15 mg/kg every 6 hours for 4 days) in infants and children with suspected or proven H. influenzae type B meningitis; ideally this drug should be given directly before or with the first dose of an antimicrobial drug. Two studies showed that infants and children did not benefit from dexamethasone, but this may be because the drug was given too late. In a randomized trial of giving dexamethasone for 2 or 4 days, no significant differences were found in the incidence of late residual effects, suggesting that patients with meningitis caused by H. influenzae type B may benefit from shorter duration dexamethasone therapy. those with a positive cerebrospinal fluid Gram stain), but clinical data are insufficient to recommend routine use of this drug. We still recommend prescribing dexamethasone to patients classified as high risk (Herson Todd score 4.5 or higher) or patients with severely reduced mental status, cerebral edema, or very high intracranial pressure. Additional use of dexamethasone is especially important in patients with pneumococcal meningitis caused by strains highly resistant to penicillin or cephalosporin, since due to the reduced inflammatory response of the cerebrospinal fluid, the entry of vancomycin there is reduced and sterilization occurs at a later date.
Symptoms of meningoencephalitis
Although the symptoms of different types of disease have their own characteristics, there are general clinical signs of meningoencephalitis:
- severe headaches;
- temperature rise to 38-39 degrees;
- neck pain, impaired muscle movement in the neck;
- photophobia, hypersensitivity to sounds;
- convulsions;
- changes in behavior, signs of impaired thinking, concentration;
- dizziness;
- nausea;
- deterioration of vision, various disorders.

With tick-borne meningoencephalitis, there is a sharp increase in temperature to 38 ° C with aching joints, chills, headaches, nausea and vomiting. There may be hemorrhages in the membranes of the eyes, tingling and numbness of the limbs, paresis, paralysis, and coma.
Herpetic meningoencephalitis is characterized by a latent period lasting several days, but can occur without it. Then the neurological signs of the disease, common to all types, progress, to which is added odor intolerance, up to olfactory hallucinations. A feature of the disease is lethargy and unilateral paralysis, paresis.

Meningoencephalitis caused by the rabies virus, having a very similar clinical picture, is characterized by a slight increase in temperature, irritability, avoidance of contact with people, and also fear of hydrophobia. When experiencing thirst, the patient cannot get a drink due to the spasm of the larynx that occurs from water. Then a spasm begins from the mere sight of water, the sound of its murmur, even its mention in conversation. On this basis, behavioral disturbances may increase. As the disease progresses, soreness in the pharynx and larynx is caused even by a breath of wind, and the patient suffers from lack of air. He begins to rush around, make sudden movements in search of a comfortable body position - this restless behavior gives the disease the name “rabies.” Then hallucinations and damage to the pelvic nerves begin, urinary and fecal incontinence, and an increase in temperature to 40-42 degrees. For some time, the patient experiences relief, but it is deceptive: this stage leads to muscle paralysis and usually ends in death.
A distinctive feature of meningococcal encephalitis is skin rashes. At a late stage, the rash forms irregularly shaped purple or bright red spots on the skin. Otherwise, the clinical picture is similar to other general manifestations of the disease of a neurological and mental nature.

With amoebic meningoencephalitis, the general clinical picture develops after 2-6 days of latent infection. It differs from other types of disease by suppression of the sense of smell and taste; the patient ceases to feel the smells and tastes of food. Convulsions, hallucinations, incoordination of muscle function, imbalance - all this complements the headaches, nausea and other manifestations characteristic of meningoencephalitis. Within 10 days the patient may die. However, some species of protozoa cause the granulomatous amoebic type of the disease, which usually has a subacute course. Sometimes it passes into a chronic form, which worsens into a milder form.
Main symptoms
Meningitis encephalitis can cause a variety of symptoms. Much depends on the type of pathology, the cause of its occurrence, and the type of course. Once the infection enters the body, an incubation period begins. At this time, the human immune system tries to resist the pathogen, causing:
- attacks of headache;
- lethargy;
- increased sensitivity of the skin;
- loss of appetite;
- aching muscles and joints.
The duration of the incubation period depends on the strength of the immune system and the general condition of the body. It often ends after a few hours, giving way to an acute stage. Then the following symptoms are observed:
- increased body temperature;
- chills;
- runny nose;
- cough.
Penetration of infection into the brain can cause psychosis, hallucinations, sleep disturbances, and drowsiness. The onset of meningeal syndrome is accompanied by:
- hearing and vision impairment;
- photophobia;
- red rashes that disappear with pressure;
- hypertonicity of the occipital muscles;
- loss of movement coordination;
- nausea;
- cephalgia.
Diagnostics
At the first signs of illness, you should consult a neurologist. The specialist will interview the patient, as well as his relatives, about complaints, ask about changes in the patient’s behavior, previous events (has there been swimming in open water, tick bites), his medical history, etc. Special neurological tests will help recognize the signs of the disease, which the doctor will ask the patient to perform during the examination. Then you will need to take tests and undergo a series of diagnostic procedures:
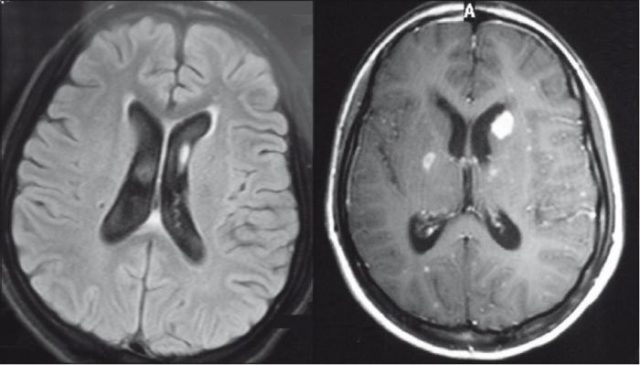
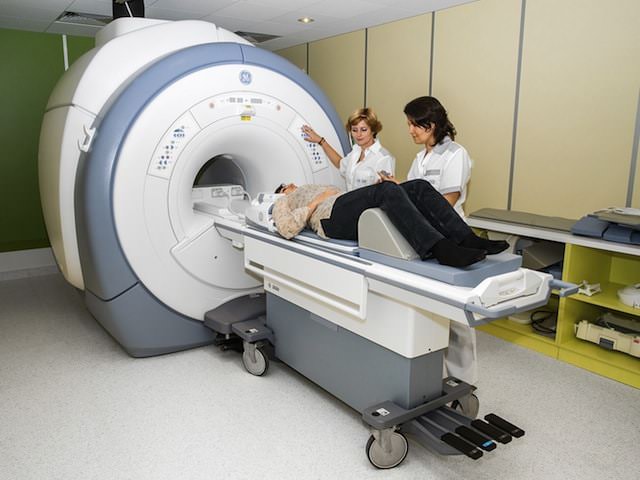
- MRI or brain;
- lumbar puncture (with purulent inflammation, the cerebrospinal fluid will be cloudy, with sediment in the form of flakes; with serous inflammation, it will be transparent; with hemorrhagic inflammation, it will contain blood particles);
- blood tests (the ESR indicator is important, indicating the degree of inflammation, as well as the level of leukocytes), blood culture for sterility to identify the type of pathogen;
- an electroencephalogram may be needed;
- in difficult to diagnose cases, stereoscopic brain biopsy.
The doctor will differentiate meningoencephalitis from other dangerous pathologies: brain tumors, strokes, intoxications, as well as degenerative processes in tissues.
Treatment of meningoencephalitis
Due to the danger of the disease, it is necessary to be treated for meningoencephalitis in a hospital setting. Treatment is carried out comprehensively and includes three main principles:
- The etiological principle, i.e. therapy based on the origin of the disease. For infectious etiologies of the disease, antiviral agents or antibiotics are used.
- Symptomatic treatment – relief of symptoms, alleviation of the patient’s condition. For high temperatures, antipyretics are prescribed, for seizures - anticonvulsants, for epileptic symptoms - anti-epileptic drugs. Severe pain is relieved.
- The pathogenetic principle is the removal of cerebral edema, removal of excess fluid, improvement of nutrition and metabolic processes in tissues.
Increased intracranial pressure is relieved with diuretics (diuretics).
The specific treatment protocol depends on the type of disease, the age of the patient and many other factors.
When the acute period of the disease is left behind, the patient needs to undergo a period of rehabilitation. To restore the body, vitamin complexes, drugs to improve brain activity, physiotherapeutic procedures are prescribed, and sanatorium treatment is recommended. The duration of rehabilitation depends on the severity of the disease, as well as the individual characteristics of the body.

Encephalitic meningitis: diagnosis and treatment of encephalitic meningitis
In order to establish a diagnosis of “encephalitic meningitis,” specialists at the Yusupov Hospital prescribe a laboratory analysis of the cerebrospinal fluid to identify the causative agent of meningitis. In addition, puncture allows you to reduce intracranial pressure, which increases significantly with inflammation of the meninges, due to which patients feel some relief.
After confirming the diagnosis, doctors at the Yusupov Hospital Neurology Clinic develop an individual treatment regimen for each patient. Therapy is carried out using antibacterial, antiviral, anti-inflammatory drugs and immunomodulators. In some cases, hormone therapy is additionally included in the regimen.
The duration of the therapeutic course depends on the stage of the disease, the degree of damage to the brain and its membranes.
Treatment of encephalitic meningitis at the Yusupov Hospital is comprehensive, using not only symptomatic medications, but also modern medicines that improve cellular metabolism, blood circulation, as well as vitamin complexes and restoratives.
Prognosis and prevention
Meningoencephalitis is a disease that rarely goes away without consequences. Some of them gradually fade with adequate treatment, others remain for life. Consequences include disturbances in speech, memory, attention, coordination, vision, hearing, and motor activity. Paresis and paralysis, changes in a person’s behavior and personal qualities are possible.
The most favorable prognosis is for childhood chickenpox meningoencephalitis, which goes away without a trace with proper therapy. For most other types of disease, the prognosis is not as favorable. About a tenth of patients die. People who survive meningoencephalitis most often remain disabled.
There are special vaccinations against infections that cause meningoencephalitis: meningococcus, rabies virus, tick-borne encephalitis, influenza, measles. However, we should not forget about the correct diet, good nutrition, exercise, fresh air and a healthy lifestyle. After all, all this strengthens the immune system and fills a person with vitality.

Meningoencephalitis in children
The disease in children usually occurs due to the greater vulnerability of their immune system. Children's immunity is in the process of formation. There are known cases of intrauterine infection of the fetus due to an infectious disease in a pregnant woman. The so-called vertical route of infection of newborns during childbirth is also possible if the mother is infected with meningoencephalitis.
In children, primary school children, and adolescents, chickenpox and measles meningoencephalitis are the most common.
Children experience the same symptoms as adults, but the disease itself is more acute.
Body temperature can rise to 41 degrees. This causes vomiting, which does not bring the patient any improvement in well-being, and headaches that cannot be relieved by taking painkillers.
Seizures are possible, but they do not always indicate brain damage in a child. In children, seizures can be a consequence of high body temperature. However, the prognosis for the outcome of the disease in childhood is much more favorable than for the disease in adults.
Complications
Bacterial and viral meningoencephalitis are often complicated, especially against the background of reduced immunity. The consequences of the disease include the following conditions and diseases:
- epilepsy;
- paralysis and paresis of the limbs and body;
- hydrocephalus (excessive fluid in the brain);
- delayed mental and mental development;
- death.
The development of complications can cause disability in young patients and requires parents to comply with all doctor’s instructions.

The first symptoms of meningitis or meningoencephalitis are a reason to call an ambulance.
To eliminate the consequences, rehabilitation courses in specialized centers are recommended. In addition, classes with the child are also carried out at home. To do this, the doctor teaches parents special techniques and exercises.