Classification
Multiple sclerosis can be divided into the following forms:
- Remitting – exacerbation of the disease alternates with almost complete restoration of lost body functions. In most cases, it is observed in the first stages of the onset of the disease. Quite often a person thinks that the unpleasant sensations have passed and they can forget about the course of the disease, but it returns with the same force.
- Progressive stage of the secondary type. Manifestations of the disease increase, bringing with them serious complications. A person practically does not feel when the condition becomes better, although such periods do occur.
- Progressive stage of the primary type. The most severe form of multiple sclerosis, a person’s condition worsens, while relief occurs only for a short time.
How is multiple sclerosis diagnosed on tomography?
The symptoms of this disease are most often not so pronounced, which is a serious problem. Therefore, in order to make a correct diagnosis and prescribe effective treatment, in-depth diagnostics, namely MPT of the brain, are required.
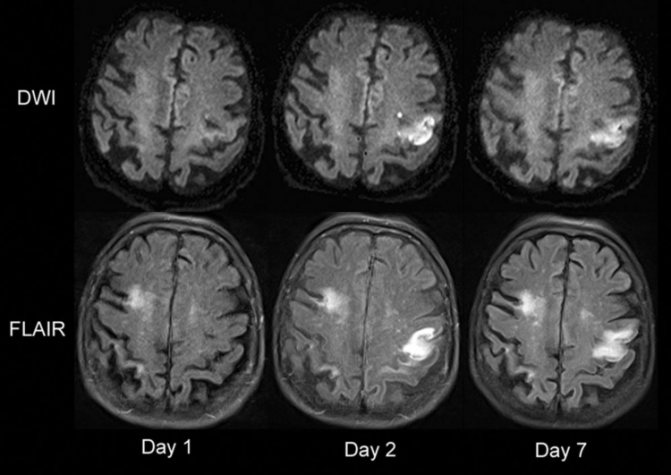
How to recognize the disease based on MRI results? Carefully examining the picture, pay attention to the following signs:
- dissemination over time (determined by a series of studies, taking into account the increase in foci);
- spatial dissemination (note the appearance of new foci of sclerosis in parts of the brain that were not previously affected by the disease);
- accumulation of the contrast agent (a ring-shaped area appears around the sclerotic lesion of the brain, which indicates the active phase of the inflammatory and plaque-forming process);
- formation of perifocal edema around the sclerotic lesion;
- damage to the cerebral hemispheres, brain stem, spinal cord, optic nerve and cerebellum;
- damage to the corpus callosum;
- Dawson's fingers on MRI - elongated foci of the disease are recognized along the fibers of the corona radiata.
Multiple sclerosis is a chronic pathology that can have different forms of progression: exacerbation, when the process of disease development is activated, and the symptoms appear brighter, and remission, when the symptoms of sclerosis disappear, the patient’s general well-being improves, and lost functions are partially restored. In addition, multiple sclerosis is classified into the following types:
- Remitting, when after an exacerbation the patient fully or partially recovers lost functions.
- Primary progressive, when the patient’s condition deteriorates sharply, and remission occurs rarely and most often it is short-lived.
- Secondary progressive, when attacks replace each other, and between them the patient’s condition worsens.
- Progressive with exacerbations, when the patient’s condition worsens slowly and gradually from the onset of the disease.
Indications for MRI for sclerosis are determined by the attending physician. It is difficult to say how long the procedure takes - each case is individual, and the duration of the study depends on the presence of the disease and the presence of affected areas.
During the tomography, the patient must lie still - this is the only way to obtain accurate MRI results.
MRI for sclerosis helps to obtain general information about the disease, the location of lesions, assess the activity of the pathological process, and visualize even the smallest plaques of the disease. If tomography is performed with contrast, this guarantees more accurate research results. But to give the patient a final diagnosis, MRI alone is not enough.
Foci of sclerosis on MRI
In order to establish an accurate diagnosis of multiple sclerosis and see foci of inflammation in the image, it is sometimes necessary to administer special drugs intravenously. After this contrast enhancement, multiple sclerosis lesions accumulate the drug, which is clearly visible on the images.
Multiple sclerosis is a chronic disease characterized by active and remission phases, and the shape of lesions on MRI can inform doctors which phase of the disease is currently ongoing.
There is a classification of multiple sclerosis diseases depending on the shape and location of the lesions:
- If the spinal cord and optic nerve are affected in the image, then this is Devic's disease.
- If the lesions are large and located in the frontal lobes, then this is Ballot's sclerosis.
- Foci of multiple sclerosis that occur in children indicate that this is Schilder's disease.
- If the image shows obvious large lesions with extensive affected areas, then this is the most severe type of multiple sclerosis - Marburg's sclerosis.
The size of the lesions makes it possible to assess how the course of the disease changes over time and whether medical care helps. For example, with successful treatment after a follow-up examination, the lesions usually change their shape from round to oval and decrease in size.
Symptoms and signs of multiple sclerosis
For various reasons, the immune system can fail. Sometimes white blood cells, which are in constant contact with almost all cells of the human body and protect the body from pathogenic bacteria, viruses and parasitic cells, begin to attack the neurons’ own myelin sheaths. As a result, the conduction of the nerve impulse is disrupted.
At the onset of the disease, symptoms may manifest in different ways. Depending on the course and phase of multiple sclerosis, its symptoms can be moderate or pronounced. Establishing an accurate diagnosis at the initial stage of development of MS can be difficult; the symptoms are similar to those of other diseases, so the patient needs to undergo a full examination.
A person should be alert to such manifestations of multiple sclerosis as:
- visual impairment;
- double vision;
- dizziness;
- weakness in arms and legs;
- fast fatiguability;
- urinary incontinence;
- decrease or loss of skin sensitivity;
- epileptic seizures;
- nervous tic;
- dementia;
- pain that occurs when the head is tilted forward;
- impaired coordination of movements.
It is for this reason that people aged 15 to 55 years, if they have certain signs of the disease, should seek advice from specialists.
It is quite difficult to detect multiple sclerosis in the early stages, but with the help of modern diagnostic methods it is quite possible. MRI is one of the few types of examination that helps doctors diagnose the disease and prescribe appropriate treatment, saving valuable time.
Symptoms and signs that make you suspect the presence of multiple sclerosis:
- Loss of voluntary movement, coordination, and weakness in an arm or leg.
- Visual impairment, most often in one eye, bright flickering before the eyes, flashes or disturbances like a retina in front of the eyes.
- The appearance of pathological reflexes
- Dysfunction of the pelvic organs – urinary incontinence, impotence.
- Memory disorders, headaches, paresis and paralysis in one of the limbs.
One symptom is essentially not significant, but a set of symptoms makes you think about the presence of a disease. Sometimes the symptoms are unspecific, sometimes they are very typical. But making a diagnosis and starting treatment based on a set of symptoms alone is quite careless and incorrect. To clarify the presence of multiple sclerosis, the neurologist prescribes an MRI of the brain.
The onset of the disease can occur without pronounced symptoms, which is why it can only be diagnosed with the help of special studies conducted by a qualified specialist. More often, the disease can vary in terms of symptoms, making it difficult to detect without the use of appropriate scans.
We can talk about confirming this diagnosis if the following are observed:
- Failure during physical activity.
- Visual impairment to varying degrees of severity.
- Disorders of stool and urination.
- A feeling of pain without a clearly defined focus.
- Feeling that different parts of the body are numb.
- Fast, rhythmic movements of the limbs.
- Problems with libido and potency.
- Stiff movements and problems with limb mobility.
- Epilepsy attacks.
- Partial or complete paralysis of the limbs.
- Feeling of weakness, chronic fatigue.
- The presence of oddities in human behavior in everyday life.
- Decreased mental function, problems with memory and concentration.
Characteristic symptoms
In order to consult a specialist in time and make a diagnosis of “multiple sclerosis” using MRI, you need to know the main clinical manifestations of this disease.
Symptoms are conventionally divided into early and late. Early symptoms can be present not only in multiple sclerosis, but also in many other diseases. These include:
- dizziness;
- constant fatigue, weakness;
- impaired visual acuity in both eyes;
- strange sensations in the limbs: tingling, goose bumps (so-called paresthesia).
Late symptoms are more specific and are more likely to prompt a doctor to refer a patient for suspected multiple sclerosis to an MRI:
- paresis and paralysis of the limbs (weakness in the arms and/or legs and their complete immobilization, respectively);
- nasal voice;
- memory problems;
- dysphagia - difficulty swallowing food;
- impaired urination and defecation;
- breathing problems up to complete cessation due to paralysis of the diaphragm.
Signs of multiple sclerosis on an MRI of the brain
Compared to other types of examination, MRI of the brain has several advantages. This diagnosis helps to obtain a clear picture of the condition of the brain and spinal cord, since sections are made in several planes, so pathologies are clearly visualized in the images. In order for the MRI results to be as reliable as possible, you need to prepare for the procedure in a special way.
The patient must remove all jewelry. If a person has metal implants or a pacemaker, the examination will be denied. Clothes should be loose and should not have zippers, buttons or other accessories made of metal.
In order not to distort the magnetic resonance scan data, the patient should take a supine position, restore even, calm breathing and try not to move during the entire procedure. If contrast has been introduced into the blood, then after the scan it is necessary to increase the amount of fluid consumed to remove gadolinium from the body as quickly as possible.
Signs of multiple sclerosis on MRI images may include the following pathological changes:
- dynamic observation indicates dissemination;
- the emergence of new lesions in tissues;
- accumulation of contrast at the edges of inflammatory and demyelinating lesions;
- well-defined perifocal zone, characteristic of multiple sclerosis;
- damage to the supratentorial, infratentorial parts of the brain and corpus callosum;
- characteristic shape of plaques (Dawson's fingers).
Because the diagnostic test is done by influencing hydrogen contained in the body, doctors know what multiple sclerosis looks like on an MRI. This is possible because human nerve cells are protected by a layer of myelin: a fatty structure that repels water. A disease such as multiple sclerosis destroys fat, so unprotected tissues are susceptible to the accumulation of excess moisture. It is water that is displayed in the image after scanning and looks like a shadow or, conversely, an illuminated area (the type of scanning is taken into account).
Diagnostic features
Previously, multiple sclerosis was diagnosed only clinically, based on symptoms. Today, the initial diagnosis requires confirmation. If the doctor makes a preliminary determination, a referral is given to find out what the magnetic resonance imaging will show.
The presence of multiple sclerosis may be indicated by the following signs detected during MRI of the brain:
- Accumulation of the contrast agent administered before the MP examination in lesions of the brain or spinal cord.
- Dynamics of increase in the size of lesions when repeating the MRI procedure (for example, within a year). Frequent MRI repetitions do not make sense, since multiple sclerosis develops quite slowly.
- The appearance of edema around the focus of demyelination.
- Damage not only to the nerve sheath, but also to the brain stem and cerebellum.
In addition, MPT can help identify problems such as compression of nerve endings by the bones of the spine. This can happen if the patient suffers from osteochondrosis, intervertebral hernia and other diseases of the musculoskeletal system. Such a negative effect on the spinal cord can be one of the root causes of the development of multiple sclerosis.
White matter lesions vary widely in location; therefore, diagnosis will depend on the location of the lesions in different parts of the brain. The yellow arrow indicates lesions in the white matter, characteristic of many pathological processes, for example, vascular origin. Foci of damage in multiple sclerosis:
- temporal lobe;
- juxtacortical area close to the cortex;
- corpus callosum;
- periventricular lesions.
Damage to the juxtacortical areas is specific to multiple sclerosis. These areas are tightly adjacent to the cortex. The terms “subcortical” and “subcortical” are not used to designate their location, since they are not very specific and are used to describe changes in the white matter of the entire brain up to the ventricles.
The arcuate fibers do not undergo changes if the vessels are affected, and therefore, on T2WI and FLAIR, a band of opacity is visible delimiting the lesion and the cortex. The temporal lobe is one of the most common lesions in multiple sclerosis. On the contrary, with encephalopathy against the background of increased blood pressure, the fronto-parietal region suffers.
The occipital lobe is rarely affected, and the temporal lobe may not undergo changes at all. An early sign of damage to the cerebral arteries, accompanied by infarctions in the subcortical areas, will be the involvement of the temporal lobe in the process.
Below are the main signs that may indicate the presence of multiple sclerosis according to the analysis of MRI images.
- Dissemination criterion over time (increase in foci in a series of studies)
- Dissemination in space (the appearance of new foci in previously untouched areas of the brain).
- Accumulation of a contrast agent (the appearance of a ring-shaped area of increased MR signal along the edge of a multiple sclerosis lesion on MRI, reflecting the active phase of the inflammatory-demyelinating process).
- Perifocal edema around the lesion of multiple sclerosis on MRI, specific for multiple sclerosis and, sometimes, simulating the appearance of the lesion.
- Damage to the supratentorial parts of the brain (cerebral hemispheres, optic nerve) and infratentorial parts of the brain (brain stem, cerebellum and spinal cord).
- Damage to the corpus callosum (the structure connecting the right and left cerebral hemispheres).
- The location of the lesions in the form of elongated zones along the fibers of the corona radiata (Dawson's finger).
These signs of multiple sclerosis on MRI are used by radiologists who examine the brain for differential diagnosis of focal changes and diagnosis.
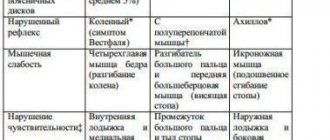
Diagnostic criteria
To simplify the diagnosis of multiple sclerosis on MRI of the brain and systematize clinical data and data obtained using a tomograph, McDonald diagnostic criteria have been developed. Created in 2001, they change every few years based on the physician's experience.
Using these criteria, it is possible to quickly diagnose multiple sclerosis and begin treatment on time.
The main criteria are presented in the table below.
| Symptoms | Instrumental data obtained using MRI |
| ≥ 2 exacerbations ≥ 2 lesions that are clinically evident | MRI confirmation is not necessary |
| ≥ 2 exacerbations 1 lesion that manifests itself clinically | Presence of ≥ 1 lesion on MRI in two areas that are typical for multiple sclerosis: periventricular, infratentorial, spinal cord or waiting for another exacerbation in which a new area of the brain or spinal cord is affected |
| 1 exacerbation ≥ 2 lesions that are clinically evident | presence of both contrast-enhancing and non-enhancing lesions on MRI or presence of new contrast-enhancing lesions on subsequent MRIs or waiting for another exacerbation |
| 1 exacerbation 1 lesion that manifests itself clinically (presence of only one symptom) | Confirmation specific to the second and third columns is required |
| The manifestation of symptoms characteristic of multiple sclerosis increases gradually (primary progressive course) | A minimum of 1 year of disease progression and the presence of at least two of the following three features:
|
All of the above signs on MRI for multiple sclerosis are necessary when making a diagnosis.

Features and stages of MRI diagnostics of multiple sclerosis with and without contrast

The main diagnostic method for suspected multiple sclerosis is MRI to study the features of the brain and spinal cord. It is impossible to accurately confirm the presence of a disease without conducting appropriate examinations. Changes can be detected in the area of damage to the myelin layer of the nerve fiber. This allows for proper monitoring with appropriate dynamics of monitoring the condition and timely changes in drug treatment.
No special preparation is needed for the procedure. It is necessary to wear loose clothing without metal accessories, remove all unnecessary items, and use earplugs. To obtain the most accurate results possible for diagnosing the disease, you must first administer a contrast agent.
Patient preparation and instruction. There are often situations when you have to do a test to check whether there is a personal intolerance to the contrast agent.
Carrying out the procedure itself. First, a contrast agent is administered, after which the patient is placed on a retractable couch, secured with special belts and driven into the tomograph opening.
The result is ready-made images that reflect problem areas in different planes and angles. The information ends up on the computer. The procedure lasts from half an hour to fifty minutes.
Completion of the procedure. The couch extends out of the tomograph tube. The straps are unfastened from the patient's body. After an hour or two, the specialist processes the received images, records them on electronic media and sends them to print to conduct further examination.
Multiple sclerosis can be seen on MRI by foci of demyelination - plaques. The tomography report is issued in two formats - T1 and T2, which allow you to determine the foci of multiple sclerosis and their shape. The function of each mode is individual:
- For T1, a hypointense signal is used, which confirms axonal degeneration (axonopathy, as a result of which the metabolic process in neurons is disrupted). On MRI, these lesions appear as “black holes.”
- For the T2 mode, a hyperintense signal is used, which allows you to obtain images with results where the affected areas of the brain stand out as clear and bright spots. this makes it possible to accurately determine the shape and size of multiple sclerosis plaques.
MRI can detect microscopic sclerosis plaques, up to 1 mm in diameter. It is almost impossible to visualize these lesions using other research methods.
It is not recommended to make a definitive diagnosis of multiple sclerosis without magnetic resonance imaging. The patient is monitored dynamically and appropriate therapy is prescribed. Diagnostics makes it possible to determine the nature of the course of the disease and obtain data on the effectiveness of the selected treatment.

Brain MRI is performed in several ways. Without the introduction of a contrast agent, the affected areas can be identified in the images, but the results of the examination will be uninformative. During scanning, hydrogen protons vibrate in nerve cells under the influence of electromagnetic waves. The tomograph records the received data on an information medium.
It is difficult to say definitively how long an MRI will take for multiple sclerosis. In each specific case, the duration of the procedure will depend on several factors. On average, the diagnosis can be completed within 30 minutes.
Foci of multiple sclerosis
As a consequence of multiple sclerosis (and some other diseases of the nervous system), gliosis develops - the replacement of dead neurons with neuroglial cells, which normally provide auxiliary functions of the nervous tissue. It is these areas that can be seen using examination methods such as magnetic resonance imaging. Neuroglia cannot be a complete replacement for neurons; they only provide normal regulation of metabolic processes. As a result, the appearance of foci of gliosis gradually affects the functioning of the entire nervous system, and the following clinical signs appear:
- Blood pressure surges.
- Headaches that are difficult to respond to standard treatment.
- Impaired coordination of movements, dizziness, and there may be instability.
- Unmotivated general weakness and increased fatigue.
- Deterioration of memory, poor intelligence.
- Convulsive seizures may occur.
Treatment of gliosis consists, first of all, in the fight against the pathology that became its cause ─ in this case, multiple sclerosis.
What does an MRI look like for multiple sclerosis?
In modern practice, diagnosticians use various criteria to determine multiple sclerosis on MPT of the brain.
A disease such as multiple sclerosis is characterized by at least 3 areas with high signal intensity. Of these, two should be in the periventricular space, and one should be in the supratentorial space. The size of the lesions should exceed 3 mm in diameter.
The Macdonald criteria are most commonly used to diagnose multiple sclerosis. There are several variants of the clinical picture of the disease with this method:
- Two or more lesions and exacerbations.
- Two or more exacerbations in the presence of one lesion.
- One exacerbation and the presence of signs of development of 2 lesions.
- One exacerbation and one lesion.
Party criteria

MPT images should show at least 4 foci of hyperintensity on a T2 scan. The size of the lesions must exceed 3 mm in diameter. Multiple sclerosis can also be confirmed if three lesions are visible on the images, one of which is located periventricularly.
Specifics of the examination
Studies of multiple sclerosis are performed not only to confirm the diagnosis, but also to monitor the specific progression of the disease in order to obtain information about effectively developed treatments. These characteristics are estimated based on the most recent images.
Magnetic resonance imaging can be performed in several ways in the presence of this disease. A non-contact study will reveal existing plaques due to the influence of electromagnetic waves. Nerve cells react with the movement of hydrogen proton molecules, which is imprinted on an electronic medium in the form of an anomaly zone near healthy tissues.
At the same time, non-contact diagnostics in the presence of affected nerve fibers provides little useful information. Most often, active lesions of the disease are examined using MRI with a contrast agent. It is introduced (0.1-0.2 mg/kg) before conducting a diagnostic study. To confirm the diagnosis, it is necessary to take pictures in a three-dimensional projection.
Contraindications
The following symptoms prompt one to suspect the presence of developing, progressive multiple sclerosis in a patient:
- Loss of coordination, feeling of weakness in the limbs, difficulty in voluntary movements.
- Gradual loss of visual acuity, and it is often impaired in one eye. A person sees bright flickering or flashes before his eyes.
- Loss of visual field (usually in one eye).
- Development of pathological reflexes.
- Urinary incontinence.
- In men - impotence.
- Memory problems, frequent migraines.
- Paresis or paralysis of the limbs.
One symptom from the list is not yet an indicator that multiple sclerosis is occurring. When several alarming symptoms are observed at once, the attending physician should prescribe the patient to undergo an MRI of the brain to exclude or confirm multiple sclerosis.
Another feature of MS is the variability of symptoms. For example, a patient may only temporarily lose vision in one eye. It is important not to ignore the first signs of the disease, but to contact a neurologist as early as possible.
- Claustrophobia.
- The presence of metal implants, a pacemaker, or an insulin pump in the patient’s body.
- Weight more than 120 kg (for technical reasons).
If the patient is allergic to gadolinium, or has liver or kidney disease, an MRI of the brain to diagnose multiple sclerosis should be performed without contrast.
MRI is prohibited in the following situations:
- if the subject has implanted electronic mechanisms;
- implants and metal prostheses were installed;
- non-removable metal structures;
- pregnancy at a period of less than 14 weeks for conventional magnetic resonance imaging and full gestation for magnetic resonance imaging with the introduction of contrast;
- mental pathology and neurological disorders;
- diseases of the blood system, cardiovascular system. Cannot be performed using a contrast agent;
- allergic reactions to contrast agents.
MPT scanning modes
The most accurate diagnosis of the condition of the brain and spinal cord is possible using two time contrasts - T1 and T2 modes.
When examining in T1 mode, a light signal comes from the white matter of the brain and spinal cord. Foci of damage to the myelin sheath do not appear intensely - dark fragments can be seen in the photographs. This is evidence that axonal degeneration is taking place - a characteristic sign of multiple sclerosis.
T2 mode allows you to more accurately determine the degree of damage to brain tissue. With this scan, the lesions glow as a bright spot, and the white matter transmits a dark signal.
To enhance the signals and obtain a more accurate picture, the patient is injected with a gadolinium-based contrast agent. It accumulates in affected areas and most clearly indicates the zones and boundaries of multiple sclerosis lesions.
Signs and picture of the disease in the picture
A characteristic manifestation of multiple sclerosis in photographs is the identification of multiple small foci in the substance of the brain and spinal cord. They look like areas of clearing in the picture.
In addition, on tomograms the doctor sees the following changes:
If the patient does an MRI 3 months after the clinical debut, the doctor will detect the following changes:
- Multiple lesions that accumulate contrast.
- The areas of clearing are tightly adjacent to the cerebral cortex, affecting the arcuate fibers.
What do multiple sclerosis lesions look like on an MRI image?
Features and stages of MRI diagnostics of multiple sclerosis with and without contrast
The use of contrast agents in magnetic resonance imaging will help indicate specific areas of brain damage, which, when compared with clinical manifestations, will help describe the picture of the disease as a whole.
Along with this, contrast agents containing gadolinium will help establish the age of appearance of the lesions detected during the study. Currently, MRI diagnostic criteria for multiple sclerosis are being improved for earlier diagnosis and timely treatment.