The transparent septum of the brain consists of two sheets running parallel to each other, located between the hemispheres of the brain. The structure of the septum is an accumulation of white matter and glia. Between the walls of the partition there is a space - a cavity. It contains cerebrospinal fluid. This space is sometimes called the fifth ventricle, which it is not.
The septum is formed after the 12th week of fetal life. Then a cavity is formed. Normally, the size of the space does not exceed 10 mm. Despite the absence of direct communications with the cerebrospinal fluid pathways, the fifth ventricle still contains cerebrospinal fluid.
Normally, after the second trimester, the cavity between the leaves begins to close. However, there is no definitive time frame for the occlusion of the space: obliteration may end, for example, by the 40th year of life, or remain open until the end of life.
There are pathologies associated with these defects of this structure:
- Lack of partition.
- Cyst in the septal cavity.
- Non-fusion of the leaves of the transparent septum.
These pathologies can act as independent diseases or in a complex of other syndromes. Sometimes these phenomena are considered as individual characteristics of the brain structure, if they do not disrupt human adaptation and do not affect health.
It should be remembered that none of these pathologies threaten human life. The maximum is periodic discomfort.
Causes
Pathologies of the septum of the brain are rare, so there are no exact causes. However, there are assumptions:
- Chronic fetal hypoxia during pregnancy.
- Infections of the mother during pregnancy, for example, toxoplasmosis, or pneumonia.
- Injuries to the skull and brain, if the disease of the septum is of an acquired nature.
- Prematurity. In this case, the cavity of the transparent septum of the brain in a baby 100% contains a cyst.
- Maternal alcoholism.
- Acquired enlargement of the cavity can form due to prolonged boxing sessions.
- Septal cysts can be congenital or acquired. The first option occurs for the above reasons, the second – for skull injuries, hemorrhagic strokes and neuroinfections.
The septum may be absent due to:
- Disturbances in the formation of the corpus callosum.
- Holoprosencephaly is a defect due to which the hemispheres are not separated at all.
- Septo-optic dysplasia is a neurodevelopmental disorder in which the formation of the anterior structures of the brain is disrupted.
Symptoms
Non-fusion of the layers of the septum pellucidum does not develop the clinical picture. However, some American scientific publications report that plate laminae increases the risk of developing mental disorders: bipolar affective disorder, schizophrenia, dissocial personality disorder.
A septum pellucida cyst, if congenital, is considered a type of normal anatomy. The acquired variant develops a clinical picture of the general cerebral type:
- Headache. Appears due to increased intracranial pressure, which is provoked by an increase in the size of the cyst. The headache is usually bursting and aching in nature.
- Periodic disturbances of consciousness. Most often it develops as a type of somnolence - a mild variant of a disorder of consciousness in which the patient is inhibited, apathetic, drowsy and disoriented. There is also lethargy and indifference to any activity.
- Dizziness.
- Vomiting that occurs without previous nausea and is often not associated with food intake. Vomiting usually brings relief to the patient.
- Convulsive seizures. Appear when intracranial pressure increases.
The transparent septum of the brain in newborns may contain a large cyst. Then, due to irritation of the meninges, meningeal symptoms appear in the clinical picture:
- Headache.
- Excitation.
- Nausea and vomiting.
- Excessive skin sensitivity, hypersensitivity to sound, photophobia.
- The child can take a specific meningeal position - the kicking dog position. Hands are pressed to the chest, legs are pulled towards the stomach, which is retracted. Also, due to hypertonicity of the muscles of the back of the head, the head is thrown back.
Absence of the septum pellucidum of the brain is rare. More often, the pathology is recorded in isolation. Does not develop a clinical picture.
Sick sinus syndrome
The term was coined in 1962 by American cardiologist Bernard Lown. The diagnosis can be made if at least one of the typical findings on the electrocardiogram has been demonstrated:
- inadequate bradycardia of the coronary sinus;
- freezing of the sinus node;
- sinoatrial block;
- atrial fibrillation;
- atrial flutter;
- supraventricular tachycardia.
The most common cause of sick sinus syndrome is hypertension, which leads to chronic strain on the atrium and then overstretching of the muscle fibers. The key examination method is long-term ECG.
The coronary sinus can be affected by cardiopathy and diseases that impair the functions of the heart. In most cases, these diseases are associated with pathologies of the coronary arteries. The most common of them:
- Abnormal venous return. This rare pathology corresponds to a congenital malformation affecting the coronary sinus. It causes organ dysfunction, which can lead to heart failure.
- Myocardial infarction. Also called a heart attack. It corresponds to the destruction of part of the myocardium. Deprived of oxygen, cells collapse and die. This leads to cardiac dysfunction and cardiac arrest. Myocardial infarction is manifested by rhythm disturbance and failure.
- Angina pectoris. This pathology corresponds to oppressive and deep pain in the chest. Most often this happens during times of stress. The cause of pain is improper supply of oxygen to the myocardium, which is often associated with pathologies affecting the coronary sinus.
Diagnosis and treatment
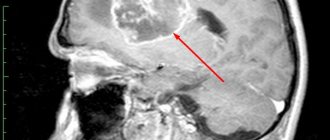
There are no specific symptoms or complaints, so objective data is provided only by an instrumental research method: magnetic resonance imaging.
On layer-by-layer sections with agenesis and underdevelopment of the septum, an increase in the distance between the anterior sections of the lateral ventricles is observed. Often the lateral ventricles are combined into one cavity.
The cyst on MRI looks like a formation with reduced density, which is localized between the anterior sections of the lateral ventricles.
Neurosonography can be used for newborns and pregnant women. The method allows you to identify a brain cyst in the fetus, determine its size and location.
Treatment of diseases of the transparent septum of the brain is not necessary due to the poor clinical picture. Therapy is prescribed when symptoms manifest. In this case, treatment is symptomatic.
During therapy, intracranial pressure is stabilized. For this, diuretics are prescribed, which reduce the amount of fluid within the brain. If they do not help, in an emergency, a ventriculotomy is prescribed - puncturing the ventricles of the brain and draining the cerebrospinal fluid.
For everything else, symptomatic treatment is used. To relieve seizures and mental agitation, anticonvulsants and sedatives are prescribed. To reduce headaches, the patient is given analgesics. In case of frequent vomiting, the water-salt and acid-base status should be balanced.
Pavel Dubrovny, Medical Psychology Specialist Didn't find a suitable answer? Find a doctor and ask him a question!
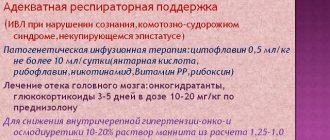
Features of treatment
Modern medicine cannot cure agenesis, but there are methods for correcting the disease. They are selected separately for each clinical case. The doctor takes into account the child’s general well-being, as well as the severity of agenesis of the corpus callosum.
Special medications are used to relieve symptoms. However, doctors are sure: most methods are not able to permanently relieve symptoms. Potent drugs are used for therapy:
- Phenobarbital. Reduces the number of attacks during infantile spasms.
- Benzidiazepines. Psychoactive products that inhibit psychomotor reactions and reduce the number of seizures.
- Corticosteroids. Necessary to combat epileptic seizures.
- Neuroleptics. Used to treat mental disorders.
- Nootropics. Used to correct brain functions.
- Diazepam. Corrects behavioral disorders.
- Neuropeptides. Improves communication between nerve endings.
In addition to medications, surgery is sometimes used to stimulate the vagus nerve. To do this, an electrical pulse generator is introduced.
Such an operation is possible only if agenesis of the corpus callosum threatens acute pathologies of important organs.
Surgery is also prescribed if other methods of therapy do not produce any results. The generator is installed in the subclavian area. After the stimulator is installed, the child should visit the doctor every few months. The advantage of installing a stimulator for agenesis of the corpus callosum is a significant reduction in the number of attacks.
Patients tolerate any symptoms better, but the device may not be effective in some situations. Sometimes pathology causes scoliosis, in which case exercise therapy and physiotherapy are prescribed for treatment. Less commonly, spinal surgery is required to improve the condition of bone tissue.
Agenesis of the corpus callosum (ACC) is characterized by partial or complete absence (agenesis) of the corpus callosum. The corpus callosum consists of transverse fibers. The cause of agenesis of the corpus callosum is usually unknown, but it can be hereditary in either an autosomal recessive or X-linked dominant pattern.
In addition, agenesis can also be caused by infection or injury during weeks 12 to 22 of pregnancy (intrauterine life), resulting in impaired fetal brain development. Prenatal alcohol exposure can also lead to AMT. In some cases, AMT may result in mental retardation, but mildly impaired intelligence, and subtle psychosocial symptoms may also be present.
Partial agenesis of the corpus callosum
AMT is often diagnosed during the first 2 years of life. Seizures of epilepsy may be the first symptom indicating that a child should be tested for brain dysfunction. The disorder can also remain without visible symptoms in the mildest cases for many years.
Morphology
Classic neuroradiological signs of agenesis of the corpus callosum:
- The anterior horns and bodies of the lateral ventricles are widely spaced and parallel (not curved). The anterior horns are narrow and acute-angled. The posterior horns are often disproportionately enlarged (colpocephaly). The concave medial borders of the lateral ventricles are caused by protrusion of the longitudinal fasciculi.
- The third ventricle is usually dilated and elevated with varying degrees of dorsal expansion and mixing between the lateral ventricles. The interventricular foramina are often elongated.
- The interhemispheric groove appears to be a continuation of the anterior section of the third ventricle, since the knee is absent. In the coronal projection, the interhemispheric groove expands downwards between the lateral ventricles towards the roof of the third ventricle. In the sagittal plane, the usual cingulate gyrus is absent, and the middle sulci have a radial or spoke-shaped configuration. Interhemispheric cysts are often visible around the third ventricle. As they increase in size, these cysts can acquire an abnormal configuration and hide underlying defects.
- Absence of the corpus callosum and septum pellucidum.
- Angulation of the anterior horns of the lateral ventricles and their depression along the medial surface by Probst's bundles.
- Radial pattern of grooves and convolutions extending from the roof of the third ventricle.
Definition
Septooptic dysplasia (de Morsier syndrome) is a form of lobar holoprosencephaly. It is characterized by the absence of a transparent septum, hypoplasia of the optic nerves, chiasm and infundibulum.
Epidemiology
More common in women.
Combined hypoplasia of the optic nerves and the absence or hypogenesis of the septum pellucida, in 2/3 of cases accompanied by hypothalamic-pituitary dysfunction.
Morphology
The transparent septum is not formed, thus there is no separation of the lateral ventricles, there are also no interventricular foramina connecting the lateral and third ventricles, and as a result a single ventricular cavity is formed. In addition, there is bilateral underdevelopment of the optic nerves, their diameter is narrower.
Fig.1
Related changes
Possible associated developmental anomalies accompanying septo-optic dysplasia include:
- cortical dysplasia
- agenesis of the corpus callosum
- schizencephaly
- hypohypuitarism
- agenesis of the first pair of cranial nerves
- schizencephaly
Differential diagnosis
- with hydranencephaly,
- with Dandy-Walker cysts,
- with severe hydrocephalus.
The absence or partial formation of a falx and interhemispheric fissure indicates holoprosencephaly.
Clinical picture, treatment and prognosis
The clinical picture varies from mild visual impairment to amaurosis, olfactory disorders up to anosmia, epileptic seizures can occur with cortical dysplasia, and hypothalamic-pituitary dysfunction and delayed psychomotor development are also possible.
Treatment is symptomatic, includes hormonal replacement and antiepileptic therapy, the prognosis is favorable.
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
Radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Expansion of external liquor spaces
June 20, 01:15
Expansion of external liquor spaces…
Girls, who, according to the results of a brain ultrasound, had “expansion of the external cerebrospinal fluid spaces, ventricles of the brain”? What dangers does this bring and what can be done about it? Today we wrote this conclusion after the ultrasound. Now go to a neurologist, and they say she likes to stuff children with medications for any reason, even without it. And how can we find out more about this diagnosis? Continue reading →
Neurologist…
Let me start by saying that I have a big head. The older one has a big one. Unfortunately, I don’t remember the sizes (to compare with the picture that the youngest one has now). At a 1.5 month appointment, the neurologist said that the youngest’s head circumference was larger than normal - 39.5 cm. Born 35 cm. Today we had an ultrasound. In 4 days we are 2 months old.
Results: interhemispheric groove 5 mm, subarachnoid space 4.2 mm. diagnosis: moderate expansion of external liquor spaces. Sent to the children's department for treatment. I say it's hereditary, they insist on hospitalization. The child is calm, eats, sleeps, walks, is active . There is no...
Continue reading →
Expansion of external liquor spaces
Girls who put this on? How expanded was it? we have 5.5 and 5.7, does anyone know the norm? we were prescribed diacarb and asparkam... but I doubt it, I’ll make an appointment with a competent specialist, but I’m interested in your opinion... Continue reading →
NSG results. Upset..
The first NSG at 1 month was good. We went to the second one on the recommendation of the pediatrician - the nasolabial triangle and the skin around the lips began to turn blue. Blue wreaths appeared on the head and eyelids.
The results did not bring sedation - the interhemispheric fissure was widened by 3.7 mm, the left ventricle was enlarged by 3.2 mm, the anterior horns of the lateral ventricles were enlarged, and the external liquor spaces were widened.
The uzist said that indirectly this could be the cause of blueness around the lips, as well as the child’s tearfulness, anxiety, and that a consultation with a neurologist and treatment with vascular drugs, nootropics and... Read more →
Is there hydrocephalus or not?
My girl was born at the 41st week, via PCS, that is, on time and full term. But the cranial sutures did not close and you could stick a finger between them, the fontanelle was and is huge! And we are almost 11 months old. I read on the Internet that this a sign of hydrocephalus. There was no fluid on the NSG.
The neurologist says that this is a sign of rickets and not hydrocephalus. But the MRI report says: “Picture of moderate expansion of the external cerebrospinal fluid spaces of the cerebral hemispheres in the frontal regions.” that is, there is liquid.
But if there was hydrocephalus, would it say yes? Continue reading →
the ventricles are dilated
we're home. In the hospital for 10 days with rotavirus and diarrhea. Diarrhea is still recurring periodically... I was given an NSG at Speransky; I asked for it myself and was shocked. The Uzist aunt is painstaking, meticulous, loves her profession madly... and what did she intend for us to have dilated ventricles (here I am writing...vls 4.9 mm body 2.
7mm vld 6mm body 4mm vt 3.4mm. the walls of the ventricles are thin, the large cistern is not expanded, the cervical tract is 4.5 mm, the liquor media are transparent, the subarachnoid space is 5.3 mm, and the choroid plexuses are symmetrical. echoes of mild hypoxic-ischemic changes...
Continue reading →
walking through torment (many letters)
I request the moderators to move it to the correct category if I made a mistake. Our torment with our youngest son Nikita began in the maternity hospital. The birth itself was easy and painless, but that’s a completely different story. The baby was born with entanglement, but Apgar score 8/9. There were no complaints against him.
They put him to the breast in the delivery room, the baby latched onto it and didn’t want to let go. They transferred us to the postpartum ward and away we go... Some evil nurse from the children's room came and said that she was taking the baby because he was born with an entanglement and night...
Continue reading →
We are healthy!!)))
We left the hospital at 1.5 months, there were a bunch of diagnoses: 1. Minor anomaly of cardiac development, patent ductus arteriosus. 2. Severe respiratory distress syndrome. 3. Severe anemia of prematurity 4. Bilateral catarrhal atitis.% 5. Possible development of retinopathy 6. Perinatal lesion of the brain of hopoxic-hemorrhagic genesis of severe degree. PVC of 1-2 degrees on the left.
Muscular dystonia syndrome. Now we are almost 6 months old, we decided to go for examination, were discharged the other day and here is our result: 1. Signs of structural changes in the abdominal organs were not identified, signs of structural changes in the kidneys and adrenal glands were not identified. 2. Signs of structural changes in the eyeballs not identified. 3. Signs of moderate expansion...
Continue reading →
Autonomic-vegetative dysfunction
Good evening, girls! We had a routine examination with a neurologist at 3 months.
In general, according to the examination, everything was fine, but she didn’t like the fact that we somehow twisted the arms and arched the back (the child was just trying to roll over onto his side), we held his head up, leaned on his legs, the head circumference was normal (40.5), the abdominal circumference was also normal . Fontana 0.5*0.5.
We smile and actively “talk.” Of my complaints, the only thing that has increased is the number of regurgitations, I can regurgitate an hour after eating, but not like a fountain, some kind of clear water. We have been drooling a lot since… Read more →
Urgently. Ultrasound conclusion
Tomorrow we will go to the doctor, but perhaps someone can explain the ultrasound conclusion: Features of the ultrasound: In the area of the caudothalamic sulcus on the left, there is a 5 mm subependymal cyst. In the area of the convexital surfaces of the cerebral hemispheres at the level of the frontal lobes, liquid up to 4 mm high.
Conclusion: Ultrasound signs of dilation of the lateral ventricles and external liquor spaces, subependymal cyst of the left lateral ventricle. In general, we have a cyst and fluid in the brain. Is there anyone here with similar diagnoses? How scary is this? Can a mistake be made in conclusion? What to ask your doctor? Continue reading →
Such are the things...
If we have the opportunity, we’ll go to the dacha tomorrow to breathe some air. And until the weekend. By the way, today we had an ultrasound of the brain and found this: “echo signs of expansion of the external liquor spaces” What kind of bullshit? The uzists themselves did not explain anything, they said to contact a neurologist.
Now I’m wondering where I can find a paid doctor nearby so that I can go to him without a month-long waiting list, after all, the brain is a serious matter...... Oooh, how tired these doctors, hospitals, clinics are already... My husband won’t be able to figure out his upcoming operations, now...
Continue reading →
NSG results, dynamics, treatment regimen
They made our third NSG. Conclusion – No gross violations were identified. Moderate dilation of the anterior horns of the lateral ventricles. In words, the uzistka said that there is an expansion of the external liquor spaces, but at the upper limit of the norm. In conclusion, she did not write this.
The second NSG was in November, its conclusion was the expansion of external liquor spaces. Moderate expansion of the anterior horns of the lateral ventricles. The first NSG was in August, everything was fine there. In general, there were no positive dynamics.
I read on the Internet that such conditions cannot be treated with massages and physiotherapy, medications are needed... Read more →
My son is 4 months old!
My son is now 4 months old. It hasn't been the easiest month for us. We changed the mixture from Nan to Nestozhen, so far so good. The mucus from the poop and the white lumps are gone. There are still rough spots on the skin. I’ve been smearing them with topical cream for the second day, and it seems to be helping.
We won’t go to the appointment until the 6th, so I don’t know my height/weight yet, but I feel like I haven’t gained much weight again. Slips of size 68 are already close))) They gave injections of Cortexin + saline solution, electrophoresis. We finished the massage course, I’m very glad that we did it. Fine…
Continue reading →
Do we have hydrocephalus or not?
My girl was born at the 41st week, via PCS, that is, on time and full term. But the cranial sutures did not close and you could stick a finger between them, the fontanelle was and is huge! And we are almost 11 months old. I read on the Internet that this a sign of hydrocephalus. There was no fluid on the NSG.
The neurologist says that this is a sign of rickets and not hydrocephalus. But the MRI report says: “Picture of moderate expansion of the external cerebrospinal fluid spaces of the cerebral hemispheres in the frontal regions.” that is, there is liquid.
But if there was hydrocephalus, would it say yes? Continue reading →
Source: https://www.BabyBlog.ru/theme/rashirnie-naruzhnyh-likvornyh-prostranstv
Symptoms and clinical manifestations
Hypoplasia of the corpus callosum in a newborn is diagnosed, as a rule, after the first two months of life, but more often it occurs during fetal development.
If doctors looked at the disease before the birth of the child, then during the first 2 years of life the child will develop harmoniously, as befits a normal baby, and only after the specified time has passed, parents may notice some deviations, such as:
- infantile spasms;
- convulsions;
- epileptic seizures;
- weakening of the cry;
- impaired sense of touch, smell and vision;
- decreased communication skills;
- manifestations associated with muscle hypotension.
Infantile spasms are convulsions characterized by sudden flexion and extension of the arms and legs, muscle hypotonia is a condition characterized by decreased muscle tone that can develop in combination with a decrease in muscle strength in the patient.
If in childhood, for some reason, it was not possible to diagnose and recognize the presence of the disease, it will certainly manifest itself in adulthood, symptoms include:
- impairment of visual or auditory memory;
- hypothermia – problems with the body’s thermoregulation (decrease in body temperature below 35 degrees);
- problems with movement coordination.
Symptoms of the pathology can be divided into two parts: non-syndromic and syndromic forms (Davila-Guttierez, 2002).
Nonsyndromic forms are the most common. An unknown percentage of cases remain asymptomatic or are incidentally detected only due to large head sizes. Most patients experience mental retardation, seizures, and/or large head sizes. Hypertelorism is often found. In a study by Jeret et al. (1987) 82% of patients had mental retardation or developmental delay, 43% suffered from seizures, and 31% developed cerebral palsy. However, normal cognitive development was observed in 9 of 63 children, possibly more often since asymptomatic cases are likely to be undiagnosed. Convulsions of any type are possible, including infantile spasms, but more often they are focal. Although an increase in head size is characteristic, sometimes more than 5-7 SD from the average, the indications for shunting are quite strict, since many cases of “hydrocephalus” spontaneously stabilize without causing any problems. Macrocephaly may be due in part to the presence of giant cysts located posterior to the third ventricle. Specific disorders of interhemispheric transmission are either absent or only minimal. However, there are reports of subtle disturbances in interhemispheric communication and topographic memory. In rare cases, endocrinological pathology may be observed.
Syndromic forms are listed below:
Subarachnoid space: causes, symptoms and diagnosis of its expansion :: SYL.ru
The subarachnoid space (SAS) exists in all people.
It is located between the soft and arachnoid (arachnoid) membranes of the brain. Its purpose is the circulation of cerebrospinal fluid, that is, cerebrospinal fluid. Expansion of SAP occurs when a lot of cerebrospinal fluid is formed, or its outflow is obstructed. Since the brain is placed in a limited cavity of the cranium, as the volume of fluid increases, its structures are subject to compression.
There is general (uniform) expansion and local.
Subarachnoid fissure - the layers of the meninges diverge above the recess of the gyrus and connect above its surface; these spaces are called fissures. The concept of SAP expansion is only a conclusion obtained from X-ray, ultrasound or tomographic diagnostics. Additional examinations are needed to determine.
Causes of pathology in uniform and local: increased formation of cerebrospinal fluid; malabsorption due to inflammation, swelling; obstructions to outflow - tumor, cyst, hemorrhage.
They may occur during the period of intrauterine development . In this case, the baby is born with hydrocephalus (water on the brain).
Provoking factors: developmental defects; anomalies in the structure of the skull, its connection with the spine; trauma during childbirth; maternal infectious diseases.
A special form of the disease is atrophy (reduced volume) of the brain and filling of the formed spaces with fluid. It is typical for elderly patients against the background of atherosclerosis, malignant hypertension, complications of diabetes.
Clinical signs:
- In adults: headache that does not respond to painkillers; nausea, vomiting; feeling of pressure on the eyes. Signs appear suddenly or gradually intensify, with periodic subsidence and exacerbation possible. With brain atrophy, expansion of SAP is an incidental finding during examination. Complications due to untimely treatment : unsteadiness when walking; dizziness; instability when changing position; difficulty coordinating movements; sensation of tinnitus, visual disturbances, even blindness; partial immobility or paralysis; muscle spasms; loss of consciousness, convulsions; mood swings, aggression, psychosis.
- In infants: swollen veins on the surface of thin skin; spherical head; the large fontanel is tense, motionless (no pulsation); seam divergence; when tapped, a sound appears, like hitting a cracked pot; upward gaze is limited, there is swelling of the optic discs in the fundus. Consequences: lag in psychomotor development; late acquisition of skills; increased tone of leg muscles; low physical activity, obesity; mental disorders - apathy, no attachment to parents, reduced intelligence.
Examinations for damage to the frontal and parietal lobes: visual examination, radiography, ultrasound, MRI, consultation with an ophthalmologist, puncture, PCR study.
Treatment of expansion of the subarachnoid space. Drug therapy is indicated for meningitis, encephalitis, trauma, and stroke. The complex includes diuretics (Lasix, Diacarb).
Indications for surgery : anomalies of the skull and SAP; benign and malignant neoplasms; intracerebral hemorrhage; brain abscess; adhesive process in arachnoiditis.
If it is impossible to radically eliminate the cause of hydrocephalus, then additional outflow pathways from the cranial cavity are created by shunting.
Read more in our article about the expansion of the subarachnoid space, its symptoms, and treatment.
Clinical signs
Manifestations of SAP expansion differ in adulthood and in infants.
Source: https://medspina.ru/diagnostika/subarahnoidalnoe-prostranstvo-rashirno.html
How to make a diagnosis
Agenesis of the corpus callosum is quite difficult to diagnose. Most cases are detected during pregnancy in the last trimester. The following methods are used to make a diagnosis:
- Echography. The procedure involves studying the structure of an organ using ultrasonic waves. But it does not identify the problem in all cases. If partial developmental anomalies are observed, it is quite difficult to notice them using this study.
- Ultrasonography.
- Magnetic resonance imaging.
Agenesis is difficult to detect because it often develops in combination with other genetic disorders. To accurately determine the presence of agenesis, karyotyping is performed. This is a study that analyzes the karyotype (characteristics of the set of chromosomes) of human cells. In addition to this technique, magnetic resonance imaging and ultrasound analysis are used.
The use of these diagnostic procedures allows you to accurately determine the state of the child’s brain.
How does the pathological process manifest itself?
With agenesis of the corpus callosum, there can be different symptoms. It all depends on what disorders arose during the prenatal period, and how poorly developed the brain is. If this anomaly is present in a child, it will have the following manifestations:
- Atrophic processes occur in the auditory and optic nerves.
- Cyst-like cavities and tumors form at the junction of the cerebral hemispheres.
- There is insufficient development of brain tissue.
- There is an increased tendency to have seizures, which are very difficult to tolerate.
- There are disorders in the form of facial dysmorphism.
- The organs of vision are underdeveloped.
- Cysts appear in the hemispheres of the brain.
- There are pathological abnormalities in the fundus.
- Psychomotor development slows down.
- Abnormal fissures form in the cerebral cortex.
- Lipomas may occur. These are benign neoplasms consisting of fat cells.
- The gastrointestinal tract is not well developed and may contain neoplasms.
- Puberty begins early.
- Low muscle tone.
- Coordination of movements is impaired.
In addition to these signs, the presence of agenesis may be indicated by Aicardi syndrome, when the brain and visual organs are abnormally developed. This is a fairly rare disease. With agenesis, lesions of the skin and bone tissue can also be observed. Such a clinical picture has an extremely negative impact on the condition and development of the child and has a rather low chance of a favorable outcome.
Mild VLS expansion and minimal signs of hyporesorption
I want to immediately warn you that I am not a pediatrician or a pediatric neurologist. I read your story to my wife, since she worked as a pediatrician for many years. My answers will be based both on mine and on the knowledge and experience of my wife: 1) What could be the real reasons for the enlargement of the left ventricle? (My wife had problems with hemoglobin during pregnancy. She took ferlatum, maltofer R, ferretab, then droppers - venofer). Answer: possible causes for internal hydrocephalus must be considered in a comprehensive manner. This could be hypoxia of the fetal brain due to maternal anemia, rapid removal of the newborn from the womb and bilirubinemia. 2) Could enlargement of the left ventricle be an individual norm for a given child? Answer: no, this is not the norm, but, on the other hand, you yourself write that, according to a pediatric neurologist: “your baby has slight expansion of the VLS and minimal signs of hyporesorption,” which, translated into understandable language, can mean: “No There are no gross deviations, but during pregnancy the fetus did not have enough oxygen (brain hypoxia, Gorbatov), because of this, brain cells died (somewhat exaggerated, Gorbatov), as a result of which the left ventricle was dilated (not quite true, Gorbatov). In the future there may be problems with speech development (complete nonsense, Gorbatov). In addition, the fluid that washes the brain is secreted more than it is absorbed (this is hydrocephalus, which means that there is more cerebrospinal fluid than there should be due to its somewhat impaired outflow, which led to minor hydrocephalus, which, in its turn, turn, caused expansion of the left ventricle of the brain, Gorbatov)". 3) Does the enlarged left ventricle put pressure on the brain and can it further provoke an increase in intracranial, and, as a consequence, ocular pressure? Answer: judging by the results of a sonographic examination of your child’s brain, the dilation of the left ventricle of the brain is minimal, due to also minimal hydrocephalus, therefore, it is not worth saying that the dilated left ventricle, with its pressure on the substance of the brain, can cause serious violations, but As for liquor hypertension, it already exists. CSF hypertension has nothing to do with increased intraocular pressure (glaucoma). 4) How dangerous is hyporesorption? Answer: firstly, judging by the sonography conclusion, it is minimally expressed, which caused a slight increase in intracranial pressure, which, in turn, led to an extremely slight expansion of the left ventricle. Let’s just say that as your child develops and the volume of his brain increases, the minimal disturbances in its structure discovered during a sonographic study will be completely leveled out and will have absolutely no negative impact on neuropsychic development. We can only advise you one thing: stop stressing yourself out, calm down and get involved in raising your child, not forgetting to conduct periodic brain studies, as recommended by your pediatric neurologist (sonography, a little later EEG). In terms of the possible negative impact of intrauterine-birth brain injury suffered by your child on his neuropsychic status, it, due to its extreme insignificance, will play a much smaller or even zero role, compared to the possible transmission of a genetic predisposition to those or other mental health problems from either you or your spouse. Some of you strike me as an extremely anxious and suspicious person. 5) Is it necessary to carry out any drug treatment in our case? Answer: if your child does not have any complaints, then I personally do not see the need for treatment. But the decision about whether or not your heir needs to prescribe therapy is entirely within the competence of your attending neurologist. 6) What is your forecast on our issue? Answer: from my point of view, based on the information you provided, the prognosis for the future of your child, due to the intrauterine or birth trauma he suffered, is very, very favorable. Regarding the question of who should monitor your child. Of course, today, a pediatric neurologist. You don't need a child psychiatrist at this time.
Our story of emergence and struggle for life...
We were discharged home when our condition returned to normal. Today we weigh 3870kg and 51cm. Our ductus arteriosus is minimal and should close on its own by the age of one year. Stridor will also go away on its own by one year. We will repair the inguinal hernia after 6 months. We diligently treat ventriculomegaly. And it's not that simple. The intracranial pressure has already been relieved. There are positive dynamics. We start every morning by taking medication. Today we know how to turn on our sides, we don’t smile often. Doesn't hold the head well. We sleep peacefully at night. That's how many trials fell on the tiny child. And the reason for it all is impaired umbilical cord blood flow, which caused intrauterine hypoxia, which led to so many problems.
Causes and predisposing factors
In its normal state, the corpus callosum is a dense plexus of nerve fibers designed to unite the right hemisphere of the brain with the left and ensure the exchange of information between them. This structure is formed from 10 to 20 weeks of pregnancy, the corpus callosum is formed at 6 weeks.
Agenesis can manifest itself in varying degrees of severity: absence, partial or incorrect formation, as well as underdevelopment of the corpus callosum. In most cases, the cause of this disorder cannot be determined, but there are a number of factors that contribute to the occurrence of such a pathology.
Predisposing factors include:
- process of spontaneous mutation;
- hereditary causes;
- chromosome rearrangement;
- the effect of toxins due to taking medications during pregnancy;
- insufficient provision of the fetus with nutrients during intrauterine development;
- viral infections or injuries suffered by the mother during pregnancy;
- disruption of metabolic processes in the mother's body;
- alcoholism during pregnancy.
Identifying the causes of such pathologies is difficult; it is only possible to identify the factors that can provoke their development.
Etiopathogenesis
As mentioned above, the development of agenesis can be triggered by heredity, but most often the reasons for its occurrence cannot be determined. This pathology has two clinical syndromes. In the first case, the patient’s intellectual abilities and motor activity are preserved, and the disease manifests itself as disturbances in the processes of transmitting impulses from the left hemisphere to the right and vice versa. For example, a patient who is right-handed cannot determine which object is in his left hand, because this requires the transfer of information from the right hemisphere to the left, where the speech zone is located. In the second case, together with agenesis of the corpus callosum, the patient also has other malformations of the brain, including disturbances in the processes of neuron migration or hydrocephalus. In such cases, patients suffer from severe convulsive seizures and also lag behind in mental development.
Mothers who are at risk include:
- drink alcoholic beverages during pregnancy;
- suffered from rubella during pregnancy, just like toxoplasmosis or severe forms of influenza;
- were exposed to radiation;
- were subject to general intoxication of the body.
This disease is classified as rare and, according to statistics, occurs in every 10,000th baby.
The problem of expansion of the subarachnoid space
No one will argue that the human brain is quite complex. He is entrusted with many tasks that he must consistently perform throughout his life. For the brain to function properly, it must be provided with adequate nutrition through proper blood supply.
Pathologies associated with brain function are always serious. One of the common problems is expansion of the subarachnoid space. According to the ICD (International Classification of Diseases), expansion of the subarachnoid space in adults is rare; more often, such pathology is found in newborns. We will talk about its causes, diagnosis, treatment and methods of prevention.
Structural features of the brain
To understand the essence of this pathology, it is important to know what membranes cover the brain. There are three of them:
- arachnoid;
- hard;
- soft.
The subarachnoid space is located between the arachnoid and soft membranes. The first covers the entire surface of the brain, which in turn is enveloped by the endometrium.
To communicate with other tissues, plexuses under the arachnoid membrane - membranes - are used. The system of ventricles of the spinal cord and brain consists of the subarachnoid vascular plexuses.
It consists of 4 reservoirs in which cerebrospinal fluid constantly circulates.
Subarachnoid spaces are small cavities in the brain filled with a special fluid (CSF). Their job is to nourish and protect the brain.
The cerebrospinal fluid contains nutrients that are used to maintain the vital activity of nerve cells and the ventricles of the brain. Tissue waste products are also removed through the cerebrospinal fluid.
If the subarachnoid space is expanded, it begins to compress adjacent tissues and blood vessels. Brain cells that do not receive proper nutrition suffer.
Liquor continuously circulates in the cavities of the brain. This is ensured by heart contractions, breathing, and body position. Normally, the volume of liquid filling the cerebrospinal fluid spaces should not exceed 140 ml.
What does this diagnosis mean?
Most often, the diagnosis “Expansion of the subarachnoid space” is made to infants. This pathology can be caused by birth trauma or a deviation in brain development. If an enlarged subarachnoid convexital space is suspected, an ultrasound scan of the brain is performed. This is the main diagnostic method.
If there is an expansion of the cerebrospinal fluid spaces of the brain, the cerebrospinal fluid is unevenly distributed and spills out of the subarachnoid space. The result is hydrocephalus (dropsy), increased intracranial pressure, and dilation of the ventricles of the brain. In this case, the cerebrospinal fluid system does not work correctly, which is why brain tissue and internal organs suffer.
The expansion of external liquor spaces leads to various pathologies (asymmetry of the cranium, impaired vision, speech, coordination, some brain functions, mental development, etc.).
The degree of development of such pathologies directly depends on how much the subarachnoid space is expanded. Weak and moderate expansion of external liquor spaces is amenable to complex treatment if it is started in a timely manner.
If the ventricles are not dilated, then there is a chance that by the age of two the baby’s brain condition will normalize and hydrocephalus will go away.
It is important that parents do not expect everything to go away on its own. You could waste precious time. The bones of the skull will become stronger, but the dropsy may remain. It is imperative to conduct a full diagnosis and, if necessary, undergo a course of treatment.
Sometimes expansion of the subarachnoid spaces can be observed with a tumor, cystic formation or inflammatory process. This is extremely dangerous, as it often leads to death. If medical care is provided on time, the prognosis is quite favorable.
During an inflammatory process, such as meningitis, more cerebrospinal fluid is produced than necessary. A large amount of fluid leads to expansion of the space (dilatation). If the problem is a tumor, then it interferes with the proper circulation of fluids inside the brain, creating a physical barrier to it. Other reasons may be an abscess, a hematoma, due to which cerebral edema began.
Diagnostics
Nowadays, brain pathologies are quite easily diagnosed. For this purpose, hardware methods are used (ultrasound, MRI), and, if necessary, lumbar puncture. The latter allows not only to detect a tumor, but also to examine all its layers and structure. This method allows you to select the treatment regimen for cystic and other formations as accurately as possible.
Basic diagnostic methods:
- Neurosonography. Duration of the procedure is ~ 15 minutes. It is carried out when it comes to a newborn, and consists of attaching a special ultrasound sensor to the patient’s head. Through the open fontanel, it allows you to collect information about the state of the brain. The advantage of this method is that it can be performed frequently, without any consequences for the baby. Now neurosonography is done in the maternity hospital to exclude pathologies of brain development. The result is deciphered by a pediatrician or neurologist.
- CT, MRI. These methods, although effective, are expensive. They are mainly used to diagnose children over 3 years of age and adults. Now considered the most accurate. To diagnose infants, using CT or MRI is very problematic, since the patient must lie absolutely still during the procedure. If such a diagnosis is indicated for a small patient, it is performed under general anesthesia.
- Cisternography. The purpose of the procedure is to determine how correctly the flow of cerebrospinal fluid is directed. It allows you to accurately determine the type of hydrocephalus in a particular patient.
- Angiography. With this diagnostic method, a special contrast agent is injected into the artery. The goal is to identify deviations in vascular patency.
- Neuropsychological examination. The patient is examined and the doctor interviews him. This examination is carried out in children over 3 years of age and adults. The doctor collects the data from all tests and the results of a visual examination. The goal is to identify disorders in the functioning of the brain.
The results of an ultrasound or MRI should only be deciphered by an experienced doctor. Self-diagnosis is unacceptable and extremely dangerous here. It is very important to accurately establish the cause of the pathology and immediately begin to eliminate it. This directly affects the course of recovery and further functionality of the brain.
A blood test is also carried out, the patient’s behavior, the presence of symptoms, and their severity are assessed.
Alarming symptoms
When the convexital spaces expand, the following symptoms are observed:
- constant headache (it appears immediately after waking up);
- nausea;
- vomit;
- dizziness;
- memory impairment (in adults);
- irritability;
- drowsiness;
- fatigue;
- in children, the size of the skull increases;
- high sensitivity to light and sound.
At first, the disease occurs without visible symptoms. Then they make themselves felt, but the intensity may vary. It depends on the degree of brain damage and the amount of cerebrospinal fluid released. If the lesion is local and minor, symptoms may be minimal.
This condition responds well to treatment, but it is important to start it at the first sign of pathology, before irreversible structural changes occur. The larger the accumulation of fluid, the more significant these changes are. Over time, the cavities may become larger.
External changes may occur in infants - the cranium enlarges (especially its frontal or posterior hemisphere), and basal brain functions suffer.
The causes of pathology at different ages differ. In infants, this is most often birth trauma, meningitis, arachnoiditis, or developmental pathologies (genetic code is disrupted). In adults – mechanical trauma, pseudocyst or tumor.
There are different degrees of uniform expansion of the subarachnoid space:
- light (1-2 mm);
- average (3-4 mm);
- severe (4 mm or more).
Localization also varies (interhemispheric, posterior, anterior, etc.). Different amounts of fluid may accumulate, and the external manifestations will also be different. Sometimes the skull becomes enlarged and there is pronounced asymmetry.
Treatment
In order for treatment of the enlarged arachnoid or subarachnoid space to be as effective as possible and tissue damage to be minimal, you should seek the help of a neurologist as early as possible. His consultation is mandatory if there has been an injury, including a birth injury, there is a suspicion of an inflammatory process, or if the listed symptoms are bothering you.
Please note that this pathology can be asymptomatic for a long time.
For successful treatment, it is important to establish the exact cause and eliminate it. Liquor dynamics must be taken into account. It can express the degree of expansion, show how much the surrounding tissues, vessels, and nerves suffer. Often, sinusitis, intracranial pressure, otitis media, and infectious diseases can provoke expansion in a child.
With this development, antibacterial drugs and B vitamins are prescribed. Treatment can be quite long. It is prescribed purely individually, taking into account the nature of the pathology and the age of the patient.
The patient must be constantly under the supervision of doctors; in the first stages of treatment, he may be placed in the neurology department.
It is important to limit the spread of cerebrospinal fluid, protect the hemispheres and sulci of the brain from compression, and clear the path for fluid to drain. To do this, it is important to determine exactly which area is affected, which lobe of the brain suffers from compression. This could be the hypothalamus, the cerebellum, several departments at once, etc.
This deviation in children is treated with a complex of drugs:
- means for removing excess cerebrospinal fluid (Asparkam, Veroshpiron, Diakarb);
- agents that improve brain trophism (Pantogam, Cavinton).
For the treatment of children over 3 years of age and adults, slightly different tactics are chosen. They are shown:
- barbiturates;
- diuretics;
- saluretics;
- glucocorticosteroids;
- plasma substitutes (solutions);
- painkillers;
- vasoactive agents.
Not all of the listed drugs are included in the treatment regimen. Their selection directly depends on the identified cause. If the problem is hydrocephalus, diuretics are prescribed; when the cause is an infection, antibiotics are prescribed.
It is advisable to supplement treatment with medications with physioneurological procedures. They reduce symptoms, restore the metabolism of cells and brain tissue. The goal of treatment is to restore blood supply to the brain and normal drainage of cerebrospinal fluid. This will stabilize intracranial pressure and restore the metabolism of cells and tissues.
The prognosis for the outcome of treatment, despite the complexity of therapy, is quite favorable. The main thing is to start it in a timely manner and continue until the brain condition returns to normal.
Sometimes it happens that drug therapy does not bring the desired effect. In such cases, surgical intervention may be required.
This disease absolutely cannot be treated on its own. The help of a competent doctor, complete diagnosis, and long-term complex treatment are required.
Please note that in an advanced state, such a pathology leads to dementia, lack of coordination, speech defects, mental retardation, urinary incontinence and a number of other undesirable manifestations.
One of the most dangerous complications is hydrocephalus. It can cause a number of irreversible vicarious changes, for example, blindness, speech disorders. It can also cause the child to lag behind in development.