All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are clickable links to such studies.
If you believe that any of our content is inaccurate, out of date, or otherwise questionable, please select it and press Ctrl + Enter.
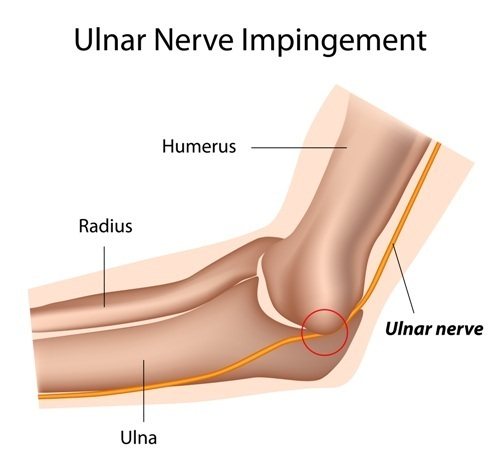
When the ulnar nerve, one of the three main nerves of the arm, is pinched, its compression lesion develops in the form of mononeuropathy of the upper limb; its ICD-10 code is G56.2. Compressive neuropathy is one of the most interesting, yet most challenging aspects of hand surgery. Compression or entrapment neuropathy occurs when a nerve becomes compressed or pinched at some point during its course in the upper extremity. This can lead to changes in function and, if left untreated, results in significant limitation of hand function. Therefore, it is necessary to diagnose and treat these conditions at an early stage. [1]
Epidemiology
Ulnar nerve entrapment in the elbow joint is the second most common compression neuropathy in the arm. The disease can seriously interfere with daily life and work. However, epidemiological studies taking into account risk factors are rare. [2]
The exact statistics of cases of pinched ulnar nerve are unknown, however, as clinical experience shows, its compression in the elbow joint is the second most common cause of neuropathy of the upper extremities. However, Mondelli conducted a retrospective study based on electromyography and estimated the standardized annual incidence of ulnar nerve compression at the elbow to be 20.9 per 100,000.[3] The prevalence of ulnar nerve compression is estimated at 1% in the United States. [4]
Experts note that among peripheral mononeuropathies, the first place in prevalence is carpal or carpal tunnel syndrome, which occurs when the median nerve of the hand is pinched; on the second - cubital tunnel syndrome when the ulnar nerve is pinched in the elbow joint.
Classification
Neuropathy (neuropathy) of the ulnar nerve (also known as corporal tunnel syndrome of the ulnar nerve) has its own classification, which is not as extensive as other ailments. So, depending on the cause of the occurrence, inflammation of the ulnar nerve occurs:
- Primary.
- Secondary.
Primary is associated with the presence of the disease, regardless of the factors that can provoke pinching or neuropathy (prolonged leaning on the elbow, etc.). Secondary, in turn, depend on the underlying disease or external factor (trauma, infectious disease, etc.).
What happens inside when pinched
Depending on the location, the disease may also vary:
- Cubital lesion.
- Pinching in the Guyon canal area.
More than 70% of all cases of pinched nerve occur either in the cubital region or in Guyon's fissure, due to the peculiarities of the nerve's passage.
Causes of pinched ulnar nerve
Highlighting the main causes of pinched ulnar nerve (nervus ulnaris), neurologists emphasize, for the most part, its traumatic origin due to damage at the level of the forearm (ICD-10 code S54.0), which is classified as peripheral nerve injuries. Pinching can also be a consequence of a shoulder girdle injury; fracture of the condyle or epicondyle of the humerus; severe bruising of the elbow (especially a direct blow to its inner part); dislocation or fracture of the elbow joint; wrist injuries.
Often, after injuries, local scars form, due to improper healing of the fracture, bone structures are deformed, and post-traumatic contractures of soft tissues along the nerve occur.
Common causes of compression are prolonged flexion of the elbow and excessive mechanical stress - repeated flexion of the elbow or wrist (intense, repetitive movements); resting on the elbow (pressure on the ulna) for a long time.
If a nerve is pinched in the elbow joint, in the tunnel behind the inside of the elbow, it is diagnosed as cubital tunnel syndrome. [5]
Experts take into account the presence of congenital and acquired deformities of the elbow joint - valgus or varus elbow, which predispose to pinching of the ulnar nerve. Cubitus valgus is a deformity in which the forearm, extended along the body, deviates from it (by 5-29°). Congenital valgus elbow is observed in Turner or Noonan syndrome, and acquired elbow may be a complication of a fracture of the lateral condyle of the humerus. Cubitus varus deformity is expressed in the deviation of part of the elongated forearm towards the midline of the body.
When the ulnar nerve is chronically pinched as it passes through the wrist, ulnar tunnel syndrome, Guyon's canal syndrome, or ulnar carpal syndrome develops.
By the way, both syndromes can be idiopathic. Read more:
Causes of tunnel neuropathy, symptoms and treatment
Tunnel neuropathy is a disease caused by damage to the nerves. The pathology is accompanied by pain caused by compression of peripheral nerves in tunnels - special narrowed openings through which the nerve passes.
Types of neuropathies
A pinched nerve in an anatomical tunnel is neuropathy. It follows that any nerve can be affected, but more often the disease appears in areas as close as possible to the bone. Thus, the following nerves are most susceptible to disease:
- elbow;
- ray;
- median;
- peroneal.
This also explains why the disease often develops in people exposed to a certain type of stress.
Causes of tunnel neuropathy
Anatomical tunnels are narrow openings through which peripheral nerves pass. These are osteo-fibrous, fibromuscular, aponeurotic openings, as well as channels in the ligaments.
Neuropathy is caused by compression of the nerve due to severe narrowing of this tunnel or canal.
the cause of the problem is a pathological narrowing of the gap, which can be due to various reasons, including genetic factors.
Causes of neuropathy include:
- congenital pathologies and developmental anomalies;
- genetic feature;
- excessive loads;
- diabetes;
- injuries and fractures.
The tunnels may be narrow from birth, but for the appearance of neuropathy a provoking factor is necessary, which is the reasons described above.
A separate cause of the disease is metabolic disorders such as diabetes. Due to changes in metabolism, the sudden appearance of neuropathic pain during pregnancy is possible.
The main risk group for developing the disease is people who are regularly exposed to monotonous physical activity. Athletes, some representatives of blue-collar professions (turner, painter), as well as people who work at a keyboard for a long time are susceptible to the disease.
Signs of neuropathy
Each type of disease has its own symptoms. It is often difficult for patients to independently determine the location of the damage, so it is important to know the general signs of such pathologies:
- It's a dull pain;
- local loss of sensation;
- increased pain when moving a limb or during exercise;
- local numbness is possible;
- feeling of “running goosebumps”.
If pain appears after prolonged exercise, it is neuropathy. Only a neurologist can determine exactly which peripheral nerve is damaged and prescribe treatment.
Compression-ischemic lesions of nerves
Tunnel neuropathy develops due to a narrowing of the tunnel, which causes a pinched nerve. This can happen due to overuse or injury.
There is also a compression-ischemic form of pathology, which is caused by compression of nerves and blood vessels as a result of staying in one position for a long time.
Often with this form of the disease, the median nerve, which runs from the shoulder joint, through the armpit and to the hand, is affected. With compression ischemic neuropathy of the median nerve, severe pain and limited mobility of the fingers are observed.
The most common cause of this form of the disease is sleeping in an uncomfortable position.
The disease is often called “honeymoon palsy” because such nerve compression is possible if pressure is placed on the shoulder and armpit area during sleep, for example, when a woman’s head rests on a man’s shoulder at night.
This problem often accompanies people who carry heavy backpacks or bags on their shoulders. Prolonged stress provokes compression of the nerve and the development of pain.
Ulnar nerve neuropathy
Ulnar nerve neuropathy is considered one of the most common forms of the disease. The causes of the pathology are:
- elbow strikes;
- fracture or dislocation of the elbow;
- emphasis on the elbow for a long time, due to professional activities;
- arthrosis;
- compression of the nerve in the wrist area.
This problem is often encountered by people in working professions when handling certain tools that compress the nerve in the wrist area. The disease may begin due to an acquired abnormality of the ulnar groove. This often occurs in people whose work involves prolonged repetition of monotonous hand movements in the elbow area, for example, when stamping or while drilling.
With compression-ischemic neuropathy of the ulnar nerve, symptoms are observed:
- pain when loading the arm;
- pain when pressing on the bony protrusion of the shoulder;
- restriction of finger movement;
- feeling of numbness in the forearm area.
This form of pathology may be accompanied by a feeling of “running goosebumps” in the forearm area.
Causes of hand pain
People who work in jobs that involve repetitive stress on their hands often experience sudden pain in this area.
This condition, known as carpal tunnel syndrome, is common among office workers, writers, pianists, plasterers and woodworkers. Repeated monotonous movements lead to compaction of the carpal tunnel.
As a result, it compresses the median nerve and pain occurs. The same problem can occur with prolonged exposure to vibration, for example, when working with a jackhammer.
Symptoms of carpal tunnel syndrome:
- aching pain that intensifies with exercise;
- numbness of the first three fingers;
- weakening of the muscle located above the thumb;
- increased pain at night;
- limited movement of the first three fingers;
- loss of hand sensation.
The peculiarity of this pain is that it does not go away even at rest. The pain syndrome may intensify at night and radiate to the forearm area.
Possible complications
Any damage to the peripheral nerves can have negative consequences. The likelihood of developing complications largely depends on the degree of damage.
In advanced cases, there is a risk of developing muscle atrophy around the damaged nerve. In case of a chronic disease, the following signs are added to the symptoms of the disease:
- insensitivity of the skin around the damaged nerve to temperature changes;
- general weakness;
- fast fatiguability;
- swelling and bluishness of the skin.
Timely diagnosis of the problem and properly selected treatment help to avoid the development of negative consequences, therefore, if pain occurs, you should immediately consult a neurologist for advice.
Diagnosis of nerve damage
Only a neurologist can diagnose tunnel syndrome or compression-ischemic neuropathy. The diagnosis is made after analyzing the patient's complaints. The doctor will definitely conduct a test that allows you to assess the extent of nerve damage and its location. The patient will need to make a few simple movements with the injured limb.
To assess the extent of damage, it is necessary to analyze nerve conduction using a special examination.
Often pain in the forearm or wrist is caused by osteochondrosis of the cervical spine. With osteochondrosis, irritation of the nerve roots of the spinal canal is possible, which send pain impulses to different parts of the body. If there is instability in the cervical spine, the patient must additionally undergo an MRI to accurately determine the cause of the pain.
Treatment of neuropathy
For the treatment of neuropathy the following is used:
- decompression of the affected nerve;
- symptomatic treatment of pain syndrome;
- relieving muscle spasms;
- massage and physiotherapeutic methods;
- surgical intervention.
Decompression includes the elimination of the provoking factor (often this is a professional activity) and fixation of the diseased limb in the anatomically correct position. For this purpose, orthoses and bandages are used. Wearing an orthosis helps relieve stress on the affected limb. The patient is also advised to rest during treatment.
Analgesics or non-steroidal anti-inflammatory drugs are used to relieve pain. For acute pain, corticosteroid injections are indicated. These drugs also relieve the inflammatory process.
The pain of neuropathy is often aggravated by muscle spasms. Anticonvulsants or muscle relaxants are used to treat the condition. Patients are shown vasodilating medications, both in tablets and for topical application. This helps improve blood supply, relieve spasms and improve local metabolic processes, which speeds up the recovery process.
Manual techniques are used to decompress the nerve. This allows you to get rid of compression and improve local blood supply. Massage is important if there is a risk of developing muscle atrophy.
Acupuncture has a good effect in the treatment of neuropathic pain. Acupuncture helps quickly relieve spasms and improve overall well-being.
However, it is not recommended to replace treatment with physiotherapeutic methods alone, since at least 10 procedures are necessary to obtain a therapeutic effect, whereas with drug treatment relief occurs faster. You cannot tolerate pain; it can make the problem worse.
Surgery
If drug treatment is ineffective, the doctor decides to surgically decompress the nerve. This operation is performed quickly and does not require long-term rehabilitation.
During the operation, the ligaments are cut, which helps relieve pressure on the nerve. In some cases, neurolysis may be necessary, which removes scarring and diseased tissue around the damaged nerve.
Indications for surgical intervention are chronic and recurring neuropathies due to the characteristics of the patient’s professional activity.
Exercise therapy for a pinched nerve
Often, neuropathy limits the patient's movements. In this case, to quickly restore motor activity, a course of physical therapy (PT) is indicated.
Exercises must be done under the supervision of a doctor in a special clinic room. Exercise therapy for neuropathy is especially recommended for those patients who often encounter this problem. Regular exercise will not only help you quickly recover from illness, but will also prevent further development of the disease.
Exercise therapy promotes:
- spasm relief;
- strengthening muscles;
- improvement of motor functions;
- prevention of disease relapse.
Treatment with physical education should begin only after pain and inflammation have been relieved.
Risk factors
Some risk factors for ulnar nerve entrapment include:
- rheumatoid arthritis;
- elbow arthritis, osteoarthritis or arthrosis deformans;
- swelling of the elbow joint;
- inflammation of the tendons (tendinitis);
- synovial chondromatosis;
- synovial cyst (hygroma or ganglion) in the wrist area;
- the presence of supracondylar osteophytes;
- osteoma, cortical hyperostosis, lipoma and other malformations;
- the presence of muscle abnormalities of the upper extremities, for example, 12-15% of people have an additional short muscle anconeus epitrochlearis passing over the ulnar nerve, crossing the ulnar nerve posterior to the cubital tunnel.
- male gender and elbow fracture predispose to the development of ulnar nerve compression at the elbow joint. [6], [7]
- Smoking has been found to be a risk factor for the development of ulnar nerve compression. [8]
Pain in the elbow area with hemophilia
If pain in the elbow joint is caused by arthritis, then most often in such a patient the inflammation affects other joints in addition to the elbow. Monoarthritis is quite rare.
- transition of hemarthrosis into a chronic course with the occurrence of synovitis;
- infection of the joint contents with the development of purulent arthritis;
- loss of fibrin threads in the joint cavity and the formation of adhesions in it, leading to the formation of contractures and ankylosis.
Pathogenesis
The anatomical and topographical features of the ulnar nerve, which is one of the five terminal branches of the brachial plexus - the middle bundle of the subclavian part, largely explain the pathogenesis of its pinching, since there are places of potential compression along the course of the nerve.
From the starting point, the path of the nervus ulnaris lies down along the medial surface of the humerus (humerus); In the middle of the shoulder, the nerve passes through the medial intermuscular septum (called the arcade of Struthers) and follows inside the triceps brachii muscle (musculus triceps brachii). Occasionally, pinching of the ulnar nerve can occur here, since it is fixed by the triceps in the lower part of the shoulder.
How does ulnar nerve neuropathy manifest itself or when the elbow gets an electric shock?
Among lesions of individual nerves, ulnar nerve neuropathy is the second most common and this is primarily due to its location.
Paresis, loss of sensitivity, pain - this is not a complete list of symptoms characteristic of this disease.
In this article we will look at what neuropathy (neuritis) of the ulnar nerve is, treatment and symptoms of this disease.
Anatomy of the ulnar nerve
The anatomy of the ulnar nerve (topography of the ulnar nerve) is not the most complex of all the nerve processes in the human body, but it also has its own characteristics.
The ulnar nerve itself performs a conductive function, like other types of nerves, but its anatomical structure is special.
So, the ulnar nerve takes its origin from the spinal nerve, and to be precise, it comes out of the medial bundle of the brachial plexus, then passes along the shoulder girdle to the human shoulder. The structure of nerves It is worth noting that during the passage from the spinal cord to the shoulder, not a single branch departs from the nerve.
Further, from the shoulder it runs along the back side to the elbow, where it runs along the back of the arm. On the back surface of the elbow, the nerve is located as close to the skin as possible.
After the elbow bend, the nerve enters the cubital canal and it is the entry point that is one of the dangerous ones, from the point of view of pinching or compression (in the cubital groove, the nerve is located in the joint as close as possible to the ulna bones and can be compressed by muscles or the ulna bone, which will cause pain and accompanying symptoms.)
Further, after passing through the cubital canal, the nerve passes along the forearm and divides into two branches: the dorsal and palmar branches.
The innervation of the skin and muscles of the wrist lies on the dorsal branch. The palmar branch runs along the back of the hand and innervates the skin of the palm and the sensitivity of the little finger, ring finger and partly the middle finger.
In addition, it is divided into deep and superficial branches. The superficial one is responsible for the innervation of the skin, and the deep one is responsible for muscle sensitivity.
The deep branch enters Guyon's groove (Guyon's canal) where it can also be compressed or squeezed due to the close proximity of the small carpal bones.
The topographical feature of the nerve structure is important in determining the cause of the disease.
Classification
Neuropathy (neuropathy) of the ulnar nerve (also known as corporal tunnel syndrome of the ulnar nerve) has its own classification, which is not as extensive as other ailments. So, depending on the cause of the occurrence, inflammation of the ulnar nerve occurs:
Primary is associated with the presence of the disease, regardless of the factors that can provoke pinching or neuropathy (prolonged leaning on the elbow, etc.). Secondary, in turn, depend on the underlying disease or external factor (trauma, infectious disease, etc.).
What happens inside when pinched
Depending on the location, the disease may also vary:
- Cubital lesion.
- Pinching in the Guyon canal area.
More than 70% of all cases of pinched nerve occur either in the cubital region or in Guyon's fissure, due to the peculiarities of the nerve's passage.
Symptoms
Symptoms of a pinched ulnar nerve vary depending on the location of the injury or inflammation.
So, with the cubital variant of the disease:
- decreased sensitivity in the elbow;
- pain in the ulnar fossa (with prolonged exposure to the nerve, pain begins to spread to the fingers and to the surface around the elbow);
- problems with moving the little finger to the side (this action causes difficulty);
- muscle weakness;
- decreased motor activity in the hand, numbness;
- the hand takes the form of a “bird’s” or “clawed” paw.
In the case of Guillain's syndrome:
- paresis of the fingers (little finger, ring finger and part of the middle finger), palms, limbs may become swollen or numb;
- paralysis;
- The above mentioned fingers may hurt from the palm side.
Basically, the symptoms in the above cases are identical, with the only exception that the lesion does not affect the back of the hand if we are talking about a pinched nerve in the Guillain's canal.
It is worth noting that the symptoms of the disease often intensify in the morning, after the patient awakens (or the symptoms can cause awakening), since many patients unconsciously put their hand under their head, which leads to numbness and the formation of these symptoms.
Fingers with ulnar nerve neuropathy
Diagnostics
Diagnosis of this disease is carried out using a comprehensive test. Which, in addition to standard neurological tests, also includes instrumental diagnostics.
The study of the disease is carried out by a neurologist, who, at the first visit, clarifies with the patient what is bothering him and the nature of the unpleasant sensations.
Neurological tests include:
- test for bending the fingers into a fist (negative result - if all fingers come together in a fist, and positive if the little finger protrudes slightly);
- test to assess range of motion (the hand is placed on a flat surface and the patient tries to scratch this surface with the little finger and spread the pressed fingers to the sides. If there is a nervous position, this will be quite problematic);
- image of the Okay sign with your hand (a sick person will not be able to complete this test).
Since the patient has quite a lot of different nerves in the arm (radial, median, etc.), the doctor must differentiate inflammation of the ulnar nerve from neuralgia of other nerve endings and roots. For this, the patient is shown instrumental diagnostics that can show not only the cause of inflammation, but also distinguish it from other diseases.
Thus, instrumental diagnostics may include:
- radiography of the elbow joint;
- Ultrasound;
- radiography of the forearm;
- radiography of the wrist joint;
- computed tomography of joints;
- testing nerve conduction velocity;
- physical examination of the elbow joint;
- magnetic resonance imaging (MRI);
- histological examination.
Prevention and prognosis
The prognosis of this disease in most cases is favorable and leaves no consequences, unlike some other ailments. However, an important condition for the absence of consequences is timely treatment.
The disease can be cured in a short time, the main thing is not to delay it.
Regarding the prevention of this disease, the following recommendations can be noted:
- avoid excessive physical activity;
- refusal or reduction of monotonous movements in the elbow joint;
- upper limb gymnastics is excellent for preventing pinching or inflammation of the ulnar nerve;
- regular intake of vitamins;
- visit a massage once every six months (or more often);
- monitor your health and be careful to avoid bone fractures, sprains or bruises of the upper extremities;
- Visit your doctor regularly for routine preventive examinations.
So, ulnar nerve neuropathy is a harmless but unpleasant disease, the course of which is difficult to predict. If symptoms reminiscent of this disease appear, you should not delay contacting a doctor. Get treatment on time and don’t joke with your health, especially when it comes to the nervous system.
Source: https://zen.yandex.ru/media/id/595f61ded7d0a69b431e48f9/kak-sebia-proiavliaet-nevropatiia-loktevogo-nerva-ili-kogda-lokot-bet-tokom-5db12b856d29c100add480db
Symptoms of a pinched ulnar nerve
The ulnar nerve provides innervation to the little finger, half of the ring finger, and sensory innervation of the skin in the hypothenar region, a muscular elevation in the palm (downward from the little finger) and the dorsal region of the hand. It also controls most of the small muscles of the hand (involved in flexion and extension of the medial and distal phalanges of the fingers) and the two large muscles of the anterior forearm, which flex and abduct the hand at the wrist and support the gripping forces of the upper extremities.
Therefore, as a result of its pinching, motor, sensory or mixed motor-sensory symptoms occur. In this case, the very first signs are sensory, which manifest themselves in the loss of sensitivity of the ring and little fingers and paresthesia, that is, numbness or tingling (especially pronounced when the elbow is bent).
Motor symptoms include muscle weakness (weakening of the grip) and difficulty coordinating the fingers supplied by the ulnar nerve. When it is pinched in the elbow joint, neuralgic pain of varying intensity and duration occurs in the elbow area, often radiating to the shoulder. Compression within the Guyon's canal leads to muscle weakness and loss of sensation on the outer side and back of the hand.
Categories of neural dysfunction (McGowan [9] and Dellon [10])
- Mild nerve dysfunction involves intermittent paresthesias and subjective weakness.
- Moderate dysfunction is accompanied by intermittent paresthesias and measurable weakness.
- Severe dysfunction is characterized by persistent paresthesias and measurable weakness.
It is important to know! Doctors are shocked: “An effective and affordable remedy for joint pain exists. " Read more.
Various pathological processes can develop in the elbow joint, due to which partial or complete limitation of movement occurs. Pinching the ulnar nerve threatens not only loss of ability to work, but also a decrease in quality of life.
Types of neuritis
The classification of neuritis is as follows:
Type:
- Mononeuritis - the development of the inflammatory process occurs in one nerve;
- Polyneuritis - the development of inflammation occurs simultaneously in several nerves.
With the flow:
- Spicy;
- Subacute;
- Chronic.
By localization
Optic neuritis – an inflammatory process develops in the optic nerve; divided into:
- Orbital (retrobulbar) neuritis - inflammation develops in the optic nerve located outside the eyeball - from the exit from the sclera to the chiasm.
- Axial retrobulbar neuritis - inflammation develops in the maculopapillary bundle of the optic nerve, which is often accompanied by optic nerve atrophy and vision loss.
- Interstitial retrobulbar neuritis - inflammation develops from the optic nerve sheath to the nerve trunk, deep down.
- Peripheral retrobulbar neuritis - inflammation begins with the optic nerve sheaths, then spreads along the septa to its tissue; proceeds to the interstitial type, with the formation of exudative effusion, accumulating in the subdural and subarachnoid space;
- Transversal neuritis - the inflammatory process spreads to the entire optic nerve, initially developing in the axial fascicle or in the periphery, and then affects other tissues;
- False optic neuritis is an anomaly in the development of the optic nerve, the clinical picture resembles an inflammatory process, while there is no atrophy of the optic nerve or visual dysfunction.
Axial neuritis - inflammation develops in the axial cylinders of the nerve fiber (axon).
Interstitial neuritis - inflammation develops in the connective tissue of the nerve, most often caused by autoimmune processes.
Parenchymal neuritis - inflammation initially develops in nerve fibers (axons and myelin sheath), after which it spreads to the connective tissue parts of the nerve.
Autonomic neuritis - inflammation develops in the peripheral fibers of the autonomic nervous system, accompanied by trophic disorders.
Ascending neuritis - develops mainly when the peripheral part of the arms and legs is injured, after which the pathological process from the periphery moves towards the center of the nervous system.
Cochlear neuritis - inflammation develops in the cochlear part of the auditory nerve, the symptoms of which are tinnitus and decreased sound perception.
According to clinical manifestations:
Gombeau's neuritis is characterized by the disintegration of the myelin sheath of nerve fibers, while the axial cylinder remains intact.
Hypertrophic Dejerine-Sotta neuritis is characterized by hypertrophy of the sheath of nerve fibers, which initially leads to compression of the conductive part of the nerve, after which the nerve begins to gradually degenerate and lose its functionality.
Rossolimo neuritis is one of the forms of hypertrophic Dejerine-Sotta neuritis, characterized by a recurrent course and occurring mainly in childhood.
By etiology (cause of occurrence):
Traumatic neuritis - the development of the disease is caused by nerve injury.
Occupational neuritis - the development of the disease is caused by a person’s professional activity - poisoning (chemical fumes, heavy metals and other substances), exposure to vibration on the body.
Infectious neuritis - the development of the disease is caused by infection of the body, infectious diseases.
Alcoholic neuritis - the development of the disease is caused by alcohol consumption, the effect on the body of which is the removal from the body of B vitamins, which are responsible for the functioning of the nervous system, as well as dead brain cells (the process of cell death occurs during alcohol intoxication).
ul
Causes
The causes of pinched ulnar nerve are divided into post-traumatic and compressive neuropathy.
Post-traumatic causes are caused by the following factors:
- subluxations;
- stretching or tearing of the ulnar nerve, when the nerve path closer to the bone area is pinched;
- lateral type of elbow dislocation;
- with a fracture of the olecranon process combined with anterior dislocation of the elbow.
Causes of compression neuropathy:
- rheumatoid type arthritis;
- deforming form of arthrosis;
- degenerative changes in bone and connective tissue at the site of a healed fracture;
- tumors;
- compression of the muscle tissue responsible for the abduction of the little finger.
Ulnar nerve entrapment can occur during skeletal traction.
Causes of neuritis
Among the main causes of neuritis are:
- Injuries (various fractures, tears, cracks, bruises, electric shock, radiation exposure, etc.);
- Inflammatory processes in the body of various organs (otitis media);
- Tumors;
- Infection of the body - viruses (herpes zoster virus), bacteria and other pathological microorganisms;
- The presence of various diseases - diphtheria, measles, influenza, arthritis, osteochondrosis, kyphosis, scoliosis, lordosis, intervertebral hernia, atherosclerosis, arterial hypertension, vegetative-vascular dystonia, tunnel syndrome, allergies, thyrotoxicosis, diabetes mellitus, brucellosis, uremia, rheumatism, herpes , syphilis, malaria, leprosy, blood diseases;
- Dehydration of the body;
- Hypothermia of the body;
- Poisoning of the body - food, alcohol, drugs, chemicals;
- Hypovitaminosis (vitamin deficiency);
- Hereditary factors (features of body structure).
Manifestations of neuritis can also appear during prolonged stay in an uncomfortable position - during sleep, at sedentary or other sedentary work.
ul
Pinching symptoms
The main symptom of a pinched nerve is the complete loss of sensitivity in the little finger and partially in the ring finger. The hand becomes numb, the fingers feel numb, and signs of muscle atrophy appear. The flexion function of the thumb may also be impaired.
Other symptoms of a pinched nerve in the elbow joint:
- The muscle tissue of the hand weakens.
- Between the index finger and thumb the muscle volume decreases sharply.
- Numbness in the hand and fingers. Loss of sensation in the little and ring fingers. Pain in fingers.
- It is difficult to raise and lower the joint, and the forearm constantly goes numb.
- There is a tingling sensation on the back of the hand.

Symptoms in the form of pain spread throughout the peripheral path of the nerve and joint.
Prevention
To prevent the nerve from getting pinched when a person leans on his elbows, soft cushions should be placed under them. Also, once every few hours it is necessary to take a short break in work (5-10 minutes).
Prevention of this pathology is aimed at preventing repeated compression of the nerve and reducing traumatization of the affected area.
For this purpose, specialized physical therapy is carried out, which prevents muscle atrophy, massage, and treatment of the underlying disease, which may cause a narrowing of the anatomical canal.
The prognosis for mononeuropathy of the ulnar nerve is quite favorable and, after treatment, does not leave negative consequences. An important condition for successful recovery is timely seeking medical help, since postponing treatment means increasing the chances of developing complications.
https://neuromed.online/zaschemlenie-loktevogo-nerva/
Diagnostics
A pinched nerve in the elbow joint is diagnosed using special tests:
- the patient is asked to clench his fingers into a fist;
- The patient's palm is on the table. You need to bend your little finger and spread the rest of your fingers to the side;
- holding a piece of paper with your thumb and index finger.
If there is pathology of the ulnar nerve in the joint, then the patient will not be able to perform the listed movements.
Instrumental methods of diagnostic examination include the following procedures:
- X-ray;
- MRI to study the cervical spine and elbow joint;
- electromyography. The procedure is designed to determine the severity of damage to muscle tissue and the degree of conduction of nerve impulses.
If there is a suspicion of a tumor, a biopsy is taken.
Treatment
Inflammation of the ulnar nerve can be treated on an outpatient basis, since this disease does not require inpatient observation, with the exception of surgical intervention.
Treatment methods are as follows:
- conservative;
- surgical;
- folk
Conservative treatment involves the use of medications, which, in turn, include:
- anti-inflammatory drugs (glucocorticosteroids, diclofenac, ketorolac);
- painkillers (metamizole sodium, anesthetics);
- anticholinesterase drugs (ipidacrine, neostigmine);
- vasoactive drugs (nicotinic acid, pentoxifylline);
- metabolites (B vitamins, alpha lipolic acid).
The greatest effect is caused by injections of the above drugs, as the absorption of the active substance increases.
In addition, the doctor may prescribe a compress with dimexide and cold on the painful area.
At the acute stage, when the pain syndrome has just appeared, it is important to perform a motor blockade of the arm and elbow joint, especially at night.
The patient is recommended to have a fixing bandage, in most cases using a splint made from improvised materials (a needle or a strong stick).
In addition to drug treatment with tablets, physiotherapy is prescribed, which includes:
- UHF;
- phonophoresis;
- magnetotherapy.
An excellent way to eliminate the unpleasant consequences of inflammation (muscle atrophy) is massage and electrical myostimulation.
Surgical intervention (operation) is indicated in case of lack of effect from medications, the presence of a hematoma, tumor, and also in the case of the development of tunnel-type neuropathy.
Types of surgical intervention:
- nerve decompression;
- neurolysis;
- removal of adhesions;
- nerve transposition;
- tumor removal;
- scar removal;
- removal of hematoma.
Any operation, especially one performed on nerves, is performed under anesthesia. Pain relief can be performed using either general or local anesthesia.
Surgical option
Naturally, home remedies are used to treat ulnar nerve neuropathy, which in most cases are aimed at eliminating the pain symptom.
Before you start using traditional medicine, we strongly recommend that you consult your doctor for advice and obtain his permission to use a particular recipe.
Horse sorrel tincture:
Soak the roots of horse sorrel in vodka in a ratio of 1 to 1. Namely, half a jar of roots and half a liter of vodka are used for a liter jar. Infuse the root for at least 10 days and apply as a compress to the sore spot. The effect is enhanced if the compress is done at night.
Bay leaf ointment:
Mix 200 grams of vegetable oil and 4 tbsp. l. finely chopped bay leaf. Leave the ointment for a week. Rub the resulting product into the area that hurts until the pain stops.
Horseradish compress:
Horseradish is ground with raw potatoes in a ratio of 1 to 1 and 1 tbsp is added to the resulting mixture. l. honey The resulting mixture is wrapped in thick cloth and applied to the left or right hand, depending on the location of the pain syndrome, for an hour. Horseradish acts as an anesthetic, and potatoes compensate for its burning effect.
Hand rehabilitation exercises
Additionally, during the recovery stage, the patient is shown physical therapy exercises (PT), as well as classes on specialized equipment.
How to forget about joint pain forever?
Have you ever experienced unbearable joint pain or constant back pain? Judging by the fact that you are reading this article, you are already familiar with them personally. And, of course, you know firsthand what it is:
- constant aching and sharp pain;
- inability to move comfortably and easily;
- constant tension in the back muscles;
- unpleasant crunching and clicking in the joints;
- sharp shooting in the spine or causeless pain in the joints;
- inability to sit in one position for a long time.
Now answer the question: are you satisfied with this? Can such pain be tolerated? How much money have you already spent on ineffective treatment? That's right - it's time to end this! Do you agree? That is why we decided to publish an exclusive interview in which the secrets of getting rid of joint and back pain are revealed. Read more.

We probably all know the feeling when, after a blow to the back of the elbow, a sharp pain spreads throughout the arm. If you constantly press on the nerve, cubital tunnel syndrome will develop. This problem leads to disruption of the passage of nerve impulses and is accompanied by a number of unpleasant symptoms.
Pain in the elbow during flexion and extension due to synovial
- pain when bending and straightening the elbow;
- swelling and stiffness of the joint;
- formation of contractures during a long course of the pathological process;
- hypotrophy of the periarticular muscles;
- in some cases - crunching when moving in the affected joint;
- sometimes with superficially located intraarticular bodies they can be determined by touch.
- swelling and severe pain in the joint;
- limitation in mobility;
- increased pain when trying to make repeated movements with the hand.
Cubital tunnel syndrome - what is it?
This disease occurs frequently. Cubital tunnel syndrome is a compression syndrome of the ulnar nerve. The latter runs along the inner surface of the elbow joint. In the area behind the most protruding bone, the ulnar nerve comes closest to the bone tissue and skin. Because of this, when people hit their elbow, they feel a sharp shooting pain that reaches their fingertips. And the stronger the pressure on the nerve, the more clearly the tingling, numbness and pain are felt.
Cubital tunnel syndrome develops for various reasons. Among the main ones are the following:
- Repeated traumatization. This reason is considered the most common. When performing monotonous, often repeated flexion and extension of the elbow, the tendon arch becomes inflamed, and its edges become much thicker. As a result, the channel narrows.
- Fracture. Injuries to the olecranon or lower shoulder can change the anatomical features of the cubital canal. The formation of spurs and cysts can lead to similar consequences. Therefore, cubital tunnel syndrome often develops against the background of strong elbow blows.
- Prolonged pressure on the ulnar nerve. The syndrome often occurs in drivers and office workers who spend a lot of time leaning on their elbows.
Causes
The ulnar nerve extends from the brachial nerve plexus to the hand, carrying nerve impulses to the flexor muscles of the hand. It is responsible for the work of the muscles of the little finger, and also brings the little finger, ring and index fingers to the middle. The most common disease of this nerve is neuralgia or neuritis.
Problems with the ulnar nerve most often occur in people who have to spend most of their time at the computer. At the same time, office workers have the habit of often leaning on their elbow, which leads to injuries to the ulnar nerve, which is located shallowly in this area of the arm.

It is not uncommon for the radial nerve, which runs very close to it, to be affected simultaneously with the ulnar nerve. In this case, the clinical picture will look like a simultaneous manifestation of neuralgia of the radial and ulnar nerves.
In addition to sitting at a desk, the following factors may influence the development of ulnar neuritis:
- infectious diseases;
- diabetes;
- malfunction of the thyroid gland;
- hand injury in which the nerve endings were damaged;
- hypothermia of the body;
- deficiency of minerals in the body;
- age-related changes;
- vascular pathologies in which the nerve does not receive the required amount of nutrients;
- alcohol abuse;
- osteochondrosis, herniated discs.

Cubital tunnel syndrome - symptoms

Early signs of the disease include numbness in the inside of the hand, ring finger and little finger, which sometimes develops into soreness. These symptoms of cubital tunnel syndrome manifest themselves after the elbow remains in a compressed – bent – position for a long time. In this case, the brush practically does not bend; it is very difficult to move it to the sides.
At later stages, signs of severe cubital syndrome appear. Retraction of the interosseous muscles is observed, the movement of the thumb becomes difficult, and the grip weakens. And all these symptoms only become more intense over time. If suspicions of cubital-ulnar tunnel syndrome do not go away within a month, it is advisable to visit a specialist urgently.
Clinical manifestations
- Positional cubital tunnel syndrome usually does not occur.
- Positive Tinel percussion test over the cubital canal (but may also be positive on the other side).
- Decreased sensitivity along the dorsum and palmar surface of the ulnar edge of the hand, on the fifth finger and half of the fourth finger.
- Weakness of the deep flexor of the fourth and fifth fingers.
- Positive Froment's symptom:
- The tip of the first finger bends as if grasping a card between the pad of the first finger and the radial side of the head of the second metacarpal bone
- The flexor pollicis longus muscle (anterior interosseous nerve) is used for gripping, since the adductor pollicis and first dorsal interosseous muscles do not function when performing a pinch grip.
- Adduction of the first finger is carried out by the extensor longus and/or due to its own weight.
- The lateral key grip is accomplished by the flexor pollicis longus.
Pinched ulnar nerve - treatment at home
If it can be identified at an early stage, then for a disease such as cubital tunnel syndrome, treatment is expected to be conservative. The first thing to do is change the load on the elbow joint. If the latter bends and unbends less often, the pressure on the nerve will decrease. At night, to avoid compression, it is advisable to fix the joint with splints. You will also have to ensure that your elbow remains straight while driving and in front of the computer.
The disease cubital syndrome of the ulnar nerve also requires medication treatment. Patients are usually prescribed:
- anti-inflammatory drugs - Ibuprofen, Paracetamol;
- vitamin complexes – Milgamma, Neuromultivit;
- medications that promote the restoration of the myelin sheath - Copaxone, Glycine (these are prescribed for neuropathies).

Before treating cubital tunnel syndrome, you should definitely consult a specialist. Most doctors recommend combining drug therapy with massage. This procedure helps reduce muscle tension. The effect is achieved by improving blood circulation and lymph outflow. In addition, massage reduces swelling in soft tissues and restores their nerve conduction, stimulates metabolism, and increases muscle tone.
In most cases, exercise therapy becomes an integral part of therapy. Treating cubital syndrome with sports warm-ups is simple but effective. All exercises should be performed while sitting. The elbows should be at 90 degrees to the table surface. The complex consists of the following exercises:
- You can eliminate cubital tunnel syndrome by moving your fingers. First, they should be raised and lowered one by one. The next stage is performing rotational movements. Final - all fingers go down and up except the thumb.
- It is necessary to strongly squeeze the phalanges of the fingers on the sore hand, even if this requires overcoming the pain.
- The last exercise is to move your fingers (each in turn) to the sides. If necessary, you can help yourself with your healthy hand.
One of the most useful folk remedies is red clay. You need to add a few drops of vinegar to it, roll it into a cake and apply it to the sore elbow at night. After three days, the pinched ulnar nerve will begin to go away. If necessary, the clay can be replaced with a horseradish leaf. This remedy works the same way, but for greater effectiveness it needs to be wrapped in a warm scarf.
How to get rid
Treatment of ulnar nerve neuralgia depends entirely on the causes that caused the disease. It is necessary to take antiviral and antibacterial drugs. In case of circulatory problems, papaverine is administered. Be sure to use B vitamins, which have a positive effect on the nervous system. To relieve edema - diuretics.
To combat inflammation, medications from are used, which can be taken in tablet form or used as ointments.
After the pain syndrome has been relieved, physiotherapeutic procedures should begin, which are aimed at restoring and improving tissue trophism. Massage and physical therapy help maintain muscle tone in the forearm and wrist.
From the second week of drug treatment, the doctor may recommend electrophoresis, UHF, and pulsed currents.
As recommended, treatment of the symptoms of ulnar neuralgia can be carried out at home, but only if the disease does not have acute symptoms and is in the first stage of its development.
Traumatic injury is treated in the department. Here, a mandatory x-ray is required, which will show what caused the inflammation, and will also make it possible to find out at what stage of healing the fracture is.
After recovery, further exposure to provoking factors such as hypothermia, advanced infections and viral diseases should be avoided. Be sure to follow a work-rest schedule, give up a sedentary lifestyle, and be sure to visit the pool and gym.
Anatomical and physiological certificate
It is impossible to understand what exactly caused the dysfunction of the ulnar nerve without the most basic knowledge of the anatomy of the human body, since only in this way can one obtain a complete picture of the course of the nerve fibers in the elbow.
The ulnar nerve is a long nerve located in the brachial plexus. It consists of biological fibers CVII-CVIII (7th and 8th cervical), which exit directly from the spinal cord.
On the arm itself, the nerve enters directly from the axillary fossa and moves to the intermuscular septum of the medial region in the middle of the shoulder and lies in the osteo-fibrous canal, which is formed inside the shoulder, tendon and wrist. This canal in the medical literature is called capital or Mouchet's canal.
It is in this place that the ulnar nerve is located almost on the very surface and as close as possible to the bones, and it is here that compression of the nerve fibers most often occurs.
As a rule, everyone who has injured their elbow at least once in their life, be it a fracture or a simple blow to a door handle, has felt quite unpleasant sensations that cause an immediate aggravation of the pain syndrome (also, the nerve can be pulsed in this place independently at any time and well feel it by touch).
After the fiber gradually leaves the limits of this channel, it ends up between the forearm muscles, but still part of its endings are in the muscle area. Moving to the border of the forearm, it is divided into several parts (external and dorsal), as well as into a small palmar branch, passing from the forearm to the palmar ligament and wrist. This part of the human body is responsible for the perception of the outside world - flexion and extension of the limb occurs.
Anatomical knowledge contributes to the fastest diagnosis of pathology.
Common causes of pain
Pathologies of articular bones, ligaments, and muscles provoke pain in the elbow joints. The reasons for this can be varied.
Most often the problem is caused by:
- Bursitis of the elbow joint - treatment at home with folk remedies
- External or internal epicondylitis (in 80% of cases).
- Vertebral pathologies – intervertebral hernia of the thoracic region, when “referred” elbow pain appears (about 20%).
- Arthrosis (up to 10%).
- Arthritis (about 7%).
- Injuries.
Epicondylitis
One of the main causes of pain is epicondylitis, which a person can get at any age. Pain increases with loads, lifting and carrying loads; the cause is injury and overexertion. When palpated, unpleasant sensations occur on the sides of the joint, at the lateral bones.
Hernia
With problems with the thoracic curve of the spine, the nature of the pain is somewhat different. It usually radiates to the arm, so it seems that the whole limb hurts. Typically, pain is caused by pinched nerves due to a herniated disc in the thoracic spine. At first they are insignificant and appear only under load, but then they intensify, becoming sharp and acute. Such attacks are called lumbago.
Important! A sudden attack of pain in the right arm is an indicator of myocardial infarction.
Arthrosis
With arthrosis, aching pain is a consequence of the destruction of articular cartilage. When the arms are fully flexed/extended, discomfort and crunching occurs.
Arthritis
With arthritis, pain occurs even at rest, and when touched it intensifies. The affected area is swollen, reddish in appearance, and there is an increase in temperature. Arthritis is often accompanied by bursitis - inflammation of the periarticular bursa as a result of injury or constant irritation of this area (a person leans on his elbows). In this case, a formation appears on the outside of the hand, elastic when pressed, which is filled with liquid.

Bursitis
Injuries
The most common injuries are fractures, dislocations, as well as sprains and ruptures of tendons. Pathologies are caused by mechanical damage, impacts, accidents. In such cases, severe pain occurs, which increases with movement or touch. There is swelling, hematomas, and the joint itself is deformed. Falls and impacts often result in tissue bruises, and dislocations occur if a person falls on an outstretched arm. With subluxations, the symptoms are similar, although somewhat weaker. Such injuries can be accompanied by ruptures of the ligaments and periarticular capsule, and the pain is very severe and it becomes impossible to move the injured limb.