| This article lacks links to sources of information. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on July 18, 2020 . |
| Carpal tunnel syndrome | |
| View of the incision across the wrist. The median nerve is shown as a yellow dot near the center. The carpal tunnel is not indicated, but a circular structure surrounding the median nerve is visible | |
| ICD-10 | 56.056.0 |
| ICD-10-CM | G56.0 and G56.00 |
| ICD-9 | 354.0354.0 |
| ICD-9-CM | 354.0[1] |
| OMIM | 115430 |
| DiseasesDB | 2156 |
| MedlinePlus | 000433 |
| eMedicine | orthoped/455 pmr/21pmr/21 emerg/83emerg/83 radio/135radio/135 |
| MeSH | D002349 |
| Media files on Wikimedia Commons | |
Carpal tunnel syndrome
(
carpal tunnel syndrome
, English carpal tunnel syndrome,
CTS
) (carpal “carpal” < Latin
carpus
“wrist” [2]) is a neurological disease manifested by prolonged pain and numbness of the fingers. Refers to tunnel neuropathy. The cause of the disease is compression of the median nerve between the bones, transverse carpal ligament and tendons of the wrist muscles.
Carpal tunnel syndrome is most common in older women. This disease is considered occupational in workers who perform monotonous flexion-extension movements of the hand (for example, when assembling machines). Sign language interpreters, motorcycle racers, cyclists, pianists, bowlers, e-sports players, drummers and, often, experienced artists also suffer from this disease.
Symptoms of the syndrome occur in computer users, such as computer game players (active and long-term use of the keyboard and mouse in an incorrect position). It is widely believed that long-term daily computer work that requires constant use of a keyboard is a risk factor for developing carpal tunnel syndrome, but research results in this regard are conflicting.[3] There is a study in which carpal tunnel syndrome was detected in every sixth person examined who worked on a computer. According to it, those users whose hand is extended by 20° or more relative to the forearm when working with the keyboard are at greater risk.[4] At the same time, other scientific studies indicate that there are no significant differences in the incidence of this syndrome in the group of constant keyboard workers when compared with the general population.[5]
It is often called “tunnel syndrome,” although this is incorrect - there are many other tunnel syndromes (syndromes of nerve compression in a narrow canal), this is just one, the most famous of them.
Causes of the disease
The occurrence of tunnel syndrome (ICD 10 code - G56.0) is observed when there is a discrepancy between the volume of intracanal tissues and the volume of the canal itself. As a result of such a discrepancy, the internal contents of the channel become pinched, causing pathological consequences. Basically, the process of nerve pinching is observed during long and monotonous loads on the hands. This can occur as a result of professional activity, when a person’s work involves stress on the hands.
With this type of work, the tendons in the canal become compacted and grow, thereby putting pressure on the nerve. Also, when there is an uncomfortable position of a person’s hand when performing work, severe tension occurs in the wrist muscles, which, in turn, causes swelling.
Carpal tunnel syndrome can occur due to other pathologies, even with their treatment, they are not related to the load on the arms. These causes of the syndrome include:
- The presence of diabetes mellitus, and the neurofibers are damaged, thereby causing swelling of the nerve.
- Diagnosis of a fracture or other injury to the wrist, which changes the volume of the canal.
- For systemic diseases of the inflammatory environment, in which damage to the connective carpal tissue occurs and pathological swelling of the tendons of the wrist occurs.
- The presence of hypothyroidism and many similar hormonal disorders, which are directly related to the development of carpal tunnel syndrome.
A noticeable complication of carpal tunnel syndrome is observed in those people who have bad habits and are diagnosed with obesity. With any noticeable imbalance in the human body, the condition of the nerve and tendons in the canal is reflected, especially if left untreated.
Brachial plexitis :: Symptoms, causes, treatment and code according to ICD-10
Name: Brachial plexitis.
Brachial plexitis
Brachial plexitis.
Damage to the brachial nerve plexus, manifested by pain in combination with motor, sensory and autonomic dysfunction of the upper limb and shoulder girdle. The clinical picture varies depending on the level of plexus damage and its genesis.
Diagnosis is carried out by a neurologist together with other specialists; it may require electromyo- or electroneurography, ultrasound, radiography, CT or MRI of the shoulder joint and plexus area, blood biochemistry studies, C-reactive protein levels and RF.
It is possible to cure brachial plexitis and completely restore the function of the plexus only within the first year, provided that the cause of the disease is eliminated, adequate and comprehensive therapy and rehabilitation are carried out.
The brachial plexus is formed by the branches of the lower cervical spinal nerves C5-C8 and the first thoracic root Th1. Nerves emanating from the brachial plexus innervate the skin and muscles of the shoulder girdle and the entire upper limb.
Clinical neurology distinguishes between total damage to the plexus - Kehrer's palsy, damage to only its upper part (C5-C8) - proximal Duchenne-Erb palsy, and damage to only the lower part (C8-Th1) - distal Dejerine-Klumpke palsy.
Depending on the etiology, brachial plexitis is classified as post-traumatic, infectious, toxic, compression-ischemic, dysmetabolic, autoimmune. Among plexitis of other localizations (cervical plexitis, lumbosacral plexitis), brachial plexitis is the most common.
The wide distribution and polyetiology of the disease determines its relevance both for neurologists and for specialists in the field of traumatology - orthopedics, obstetrics and gynecology, rheumatology, and toxicology.
Brachial plexitis Among the factors causing brachial plexitis, injuries are the most common. Damage to the plexus is possible with a fracture of the collarbone, dislocation of the shoulder (including habitual dislocation), sprained ligaments or damage to the tendons of the shoulder joint, bruise of the shoulder, cut, stab or gunshot wounds to the brachial plexus area. Often, brachial plexitis occurs against the background of chronic microtrauma to the plexus, for example, when working with a vibrating instrument or using crutches. In obstetric practice, obstetric Duchenne-Erb's palsy, which is a consequence of birth trauma, is well known. The second place in prevalence is occupied by brachial plexitis of compression-ischemic origin, which occurs when the fibers of the plexus are compressed. This can happen when the hand is in an uncomfortable position for a long time (during deep sleep, in bed patients), when the plexus is compressed by an aneurysm of the subclavian artery, a tumor, post-traumatic hematoma, enlarged lymph nodes, an additional cervical rib, or Pancoast cancer.
Brachial plexitis of infectious etiology is possible against the background of tuberculosis, brucellosis, herpetic infection, cytomegaly, syphilis, after suffering from influenza, sore throat.
Dysmetabolic brachial plexitis can occur with diabetes mellitus, dysproteinemia, gout, metabolic diseases.
Iatrogenic damage to the brachial plexus is possible during various surgical interventions in the area of its location.
Brachial plexitis manifests itself as a pain syndrome - plexalgia, which has a shooting, aching, drilling, aching character. The pain is localized in the collarbone, shoulder and spreads to the entire upper limb. Increased pain is observed at night, provoked by movements in the shoulder joint and arm. Then muscle weakness in the upper limb joins and progresses to plexalgia. Duchenne-Erb palsy is characterized by hypotension and decreased strength in the muscles of the proximal arm, leading to difficulty moving the shoulder joint, abducting and raising the arm (especially when it is necessary to hold a load in it), and flexing it at the elbow joint. Dejerine-Klumpke's palsy, on the contrary, is accompanied by weakness of the muscles of the distal parts of the upper limb, which is clinically manifested by difficulty in performing movements with the hand or holding various objects in it. As a result, the patient cannot hold a cup, fully use cutlery, fasten buttons, or open a door with a key. Movement disorders are accompanied by a decrease or loss of the ulnar and carporadial reflexes. Sensory disturbances in the form of hypoesthesia affect the lateral edge of the shoulder and forearm in proximal paralysis, and the inner region of the shoulder, forearm and hand in distal paralysis. When the sympathetic fibers entering the lower part of the brachial plexus are affected, one of the manifestations of Dejerine-Klumpke palsy can be Horner's symptom (ptosis, pupil dilation and enophthalmos). In addition to motor and sensory disorders, brachial plexitis is accompanied by trophic disorders that develop as a result of dysfunction of peripheral autonomic fibers. There is pastiness and marbling of the upper limb, increased sweating or anhidrosis, excessive thinning and dryness of the skin, and increased brittleness of the nails. The skin of the affected limb is easily injured, and the wounds do not heal for a long time.
Malaise. Sweating. Weakness in the arms. Muscle weakness (paresis).
A neurologist can establish a diagnosis of “brachial plexitis” based on medical history, complaints and examination results, confirmed by electroneurographic examination, and in its absence, by electromyography. It is important to distinguish plexitis from brachial plexus neuralgia.
The latter, as a rule, manifests itself after hypothermia, manifests itself as plexalgia and paresthesia, and is not accompanied by motor disorders.
In addition, brachial plexitis should be differentiated from polyneuropathy, mononeuropathies of the nerves of the arm (neuropathy of the median nerve, neuropathy of the ulnar nerve and neuropathy of the radial nerve), pathology of the shoulder joint (arthritis, bursitis, arthrosis), glenohumeral periarthritis, radiculitis.
For the purpose of differential diagnosis and establishment of the etiology of plexitis, if necessary, a consultation with a traumatologist, orthopedist, rheumatologist, oncologist, and infectious disease specialist is carried out; Ultrasound of the shoulder joint, X-ray or CT scan of the shoulder joint, MRI of the brachial plexus area, X-ray of the lungs, study of blood sugar levels, biochemical blood test, determination of RF and C-reactive protein, etc. Examinations.
Differentiated therapy is determined by the genesis of plexitis. According to indications, antibiotic therapy, antiviral treatment, immobilization of the injured shoulder joint, removal of hematoma or tumor, detoxification, and correction of metabolic disorders are carried out. In some cases (usually with obstetric paralysis), a joint decision with a neurosurgeon is required on the advisability of surgical intervention - plastic surgery of the nerve trunks of the plexus. The general direction of treatment is vasoactive and metabolic therapy, which provides improved nutrition and, therefore, faster restoration of nerve fibers. Patients with brachial plexitis receive pentoxifylline, complex preparations of B vitamins, nicotinic acid, and ATP. Some physiotherapy procedures are also aimed at improving the trophism of the affected plexus - electrophoresis, mud therapy, thermal procedures, massage.
Of no small importance is given to symptomatic therapy, including relief of plexalgia. Patients are prescribed NSAIDs (diclofenac, metamizole sodium, etc.), therapeutic blockades with novocaine, hydrocortisone ultraphonophoresis, UHF, reflexology.
To support muscles, improve blood circulation and prevent contractures of the joints of the affected arm, a special complex of exercise therapy and massage of the upper limb is recommended.
During the recovery period, repeated courses of neurometabolic therapy and massage are carried out, exercise therapy is continuously carried out with a gradual increase in load.
42a96bb5c8a2ac07fc866444b97bf1 Content moderator: Vasin A.S.
Source: https://kiberis.ru/?p=34237
Symptoms of the disease
Carpal tunnel syndrome (ICD 10 code - G56.0) is a fairly common disease, especially in women. Males are approximately 10 times less susceptible to this disease. There is no age limit for developing the disease. But most often, tunnel syndrome occurs during hormonal changes in the body at the age of about 50 years. In people under 30 years of age, pathology is almost not observed.
Carpal tunnel syndrome is characterized by a gradual development: first, one hand is affected, mainly the dominant one (for right-handers - the right, for left-handers - the left). As the disease progresses, the other arm is also involved in the lesion, but less painfully.
At the initial stage of the disease, symptoms of numbness and tingling of the fingers (right or left) occur in the morning. During the day, such symptoms disappear without a trace. Subsequently, symptoms of night numbness and tingling of the fingers, pain or burning are added, excluding the little finger. In some cases, such symptoms can be observed throughout the palm, right up to the elbow area. The severity of the symptoms can disrupt a person's natural sleep: he cannot sleep due to pain, burning and numbness. You can eliminate such symptoms by lowering your arms along the body and moving them, thereby improving blood circulation.
At the next stage, night and morning symptoms are added by daytime discomfort: the arms lose strength and become clumsy. In some cases, you can observe a change in the color of the skin, which is expressed in its pallor.

It should be taken into account that the symptoms and signs of the disease may differ in each specific case. This is why it is better to consult a doctor.
Classification
A classification of plexitis has been developed, which reflects the cause of the pathological process, its localization, the degree of damage to the nerve plexus, and the stage of development of the disease.
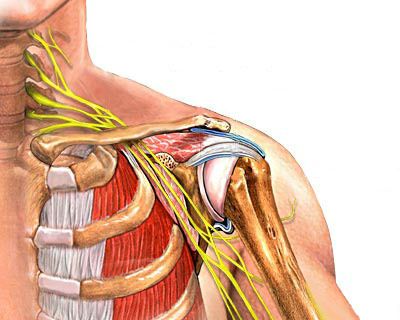
Schematic representation of the cervical and brachial nerve plexus
Based on the location of the disease, they are distinguished:
- cervical plexitis – inflammation develops in the cervical plexus;
- brachial plexitis - inflammation affects the pleural plexus, extends to the upper shoulder girdle and arm;
- lumbar and sacral plexitis - inflammation is located in the lumbar plexus, affects the gluteal muscles, the sacral area, and the lower limb is involved in the pathological process.
You may also read: Tendinitis of the supraspinatus muscle of the shoulder joint
- traumatic;
- compression-ischemic;
- infectious;
- allergic;
- intoxication;
- metabolic;
- post-traumatic birth.
According to the prevalence of the pathological process, they are distinguished:
- unilateral plexitis (right-sided or left-sided);
- double-sided
According to the severity of damage to the nerve plexus:
- partial (individual nerve trunks or nodes are involved in the inflammatory process);
- total (all structures of the nerve plexus are affected).
According to the stage of the disease:
- neurological phase;
- paralytic phase.
In the international classification of diseases ICD 10, plexitis belongs to the heading G54, G55, M50-M51, depending on the cause of the development of the pathology.
Diagnostics
Diagnosis and examination of the patient is carried out by doctors such as a rheumatologist, arthrologist, and neurologist. Basically, the doctor determines a pathology such as carpal tunnel syndrome (ICD 10 code - G56.0) at the first examination, based on the person’s complaints and the results of special tests. The latter include:
- Nitel test. The test involves tapping the narrowest part of your wrist with your finger. In the case where there is carpal tunnel syndrome, the person will feel tingling in his fingers when the doctor performs this action.
- Cuff test. The test involves the doctor placing a blood pressure cuff on the area just below the elbow and just above the wrist. When pressure is applied to the cuff, the person will feel tingling or numbness in the fingers.
- Raised hands test. At the same time, the arms are raised up and held for a minute. If a person does not feel discomfort after thirty seconds, then there is no tunnel syndrome. Otherwise, the diagnosis is confirmed.
In addition to such tests, a clinical blood test and a rheumatic test are prescribed. This is necessary to rule out arthritis. In cases where carpal tunnel syndrome is not a consequence of arthritis, such tests do not reflect any changes in indicators.
It is also necessary to exclude diseases of the cervical spine, the symptoms of which may be similar to those of carpal tunnel syndrome. To do this, the doctor prescribes an X-ray examination and tomography of the cervical area.

Electromyography is also performed, which studies muscle contraction in response to electrical stimulation of the nerve. In other words, this diagnostic method clarifies the location of nerve damage, and also determines the presence of other causes of its damage.
Treatment
Mild type syndrome (ICD 10 code - G56.0) needs to be treated with medications, a special bracelet and exercise control. For moderate to severe forms of the disease, surgical intervention is indicated. Methods for eliminating the disease include:
- Treatment at home. The first step is to regulate your daily life, which is important in achieving relief from the symptoms of the pathology. This consists of limiting high loads on the hands and fingers and, if possible, changing the type of professional activity.
- Adjusting your diet. This disease is due to the fact that the body has a deficiency of vitamin B6, but this is not necessarily the case. In some cases, the syndrome occurs when the level of the vitamin in the body is normal. If there is a deficiency, the doctor prescribes multivitamin complexes.
- Taking medications, namely, oral non-steroidal drugs. Such drugs help reduce inflammation, swelling and pain. You can take it without a doctor’s permission, but only for a short time. Anti-inflammatory ointment is actively used.
- Gymnastic exercises performed at home.

Description
Cervical plexitis. Damage to the cervical nerve plexus of infectious, traumatic, compression-ischemic, toxic, dysmetabolic origin. The clinical picture includes pain, sensory disturbances, hiccups, difficulty trying to cough or speak loudly, and shallow and rapid breathing. Diagnosis is carried out using radiography, ultrasound, tomography, and electrophysiological studies. The main goal of treatment is to eliminate the causative factor in the development of plexitis and conduct restorative neuroprotective and vascular therapy.
Surgery
For moderate and severe types of carpal tunnel syndrome, surgical treatment is necessary. In the event that treatment with a splint and medications does not bring the desired recovery, they resort to another type of treatment - surgery. Otherwise, after a few months you may end up with irreversible consequences.
The operation consists of making a transverse incision of the ligament, which helps to increase the space inside the canal. This operation means either one limited incision or two miniature ones with the introduction of flexible instruments. The operation is performed using local anesthesia.
An operation with two incisions is more gentle, as there are smaller scars and a shorter recovery period. Both interventions are performed on an outpatient basis.
Each operation subsequently requires restriction of the use of the affected arm. As a rule, full return of hand function can be observed after ten weeks. There are certain rules that must be followed after the operation:
- Hand writing is allowed after six weeks.
- You can drive the car after two days.
- Grasping objects with your hand is recommended after three months.
The operation may be accompanied by side effects:
- Pain syndrome and inflammation in the incision area.
- Surgery may cause symptoms to return.
Gymnastics in disease prevention
Physical exercises are more suitable for the prevention of carpal tunnel syndrome, which can be performed at home

. It is recommended to do exercises before starting work, which will help prevent injury. You can do the following hand exercises at home:
Performing exercise 1 – Arms in a straight position in front, palms turned towards you vertically. Maintain the pose for five seconds.
Performing exercise 2 - Hands in a straight position in front of you, fingers relaxed. Hold for ten seconds.
Performing exercise 3 – Hands in front of you, palms bent into fists. Bend your wrists down without unclenching your fists. Hold for five seconds.
Performing exercise 4 – Hands are placed along the line of the body, while shaking the hands.
The doctor can select exercises individually.
Syndrome during pregnancy
Symptoms such as numbness and tingling in the hands and feet occur in many women during pregnancy. This may be a manifestation of carpal tunnel syndrome, the symptoms of which occur at night and upon awakening. As a rule, the syndrome during pregnancy is observed in the 2nd and 3rd trimesters.
The reason for this is hormonal changes in the body and retention of fluid. As a result, soft tissues swell during pregnancy, including the ligamentous apparatus. Diagnosis is carried out by a neurologist using methods that are harmless to the fetus. It is recommended to treat pathology during pregnancy using unconventional methods.

Treatment of carpal tunnel syndrome during pregnancy, which can eliminate the symptoms and manifestations of the disease, must be timely, otherwise it can cause degeneration of the nerve fiber, which is fraught with chronic pain. It is prohibited to treat the syndrome during pregnancy with pharmacological drugs, as this is very dangerous for the fetus. Manual therapy and reflexology during pregnancy are known to help improve hormonal health. Therapeutic massages and gymnastics are also used.
Symptoms of the disease
Plexitis can appear in the neck, shoulder, and lumbosacral area. Accordingly, the symptoms of the disease in these areas are different.
Cervical plexitis has the following symptoms. The sides of my neck hurt very sharply. The pain can be paroxysmal and spread to the back of the head. The neck muscles become weak. A person is unable to turn his neck or tilt it to the side.
Since inflammation involves the phrenic nerve, which innervates the diaphragm, prolonged hiccups occur. Breathing is impaired. The person breathes shallowly. As you inhale, your abdomen draws in. The patient is unable to cough or talk loudly.
If you experience these symptoms, it is important to immediately consult a doctor in order to take timely treatment measures.
Plexitis in the neck area is included in ICD-10. ICD-10 stands for International Classification of Diseases, 10th revision. In it, each disease has its own code.
The symptoms of brachial plexitis are as follows: the collarbone hurts a lot. Soreness radiates to the arm. The pain intensifies with excessive activity of the upper limb. The skin of the hands and shoulder girdles lose their sensitivity, and the muscles of the hands are very weak. Because of this, the limb cannot be lifted. The soft tissues of the hand swell, the skin on the hands becomes pale and cold, and the nails on the fingers begin to break and crumble very badly.
Brachial plexitis or brachioplexitis is part of the ICD-10 and has its own code. It should also be treated.
Symptoms of lumbosacral plexitis are as follows:
- there is severe pain in the lower back and leg;
- the sensitivity of the skin of the lower limb decreases;
- the leg muscles weaken very much, because of this the person is not even able to lift them;
- soft tissues of the legs swell;
- feet are constantly cold and pale.
Lumbosacral plexitis can also be found in the ICD-10 list.