Often people experience pain that does not confirm the presumptive diagnosis. Pain in the back, chest, nose or eyes. The patient thinks that the heart, teeth.
Such complaints may indicate neuralgia, namely the nasociliary nerve, or Charlin's syndrome, the symptoms and treatment of which will be discussed in the article.
What is nasociliary neuralgia?
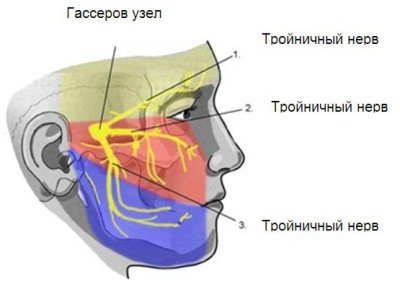
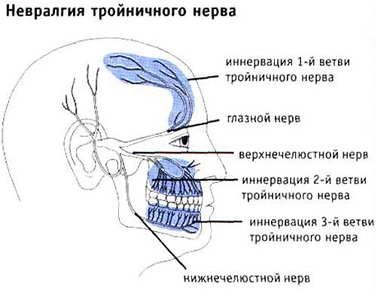
The trigeminal nerve innervates (provides sensitivity) to the muscles, skin of the face, mucous membranes of the nose, mouth, eyes and eardrum. Also goes into the brain.
Divided into three branches:
- Ophthalmic, located in the sinus, orbit and approaches the cerebellum. In the eye area it branches into lacrimal, frontal and nasociliary.
- Maxillary, located in the pterygopalatine fossa of the upper jaw and is divided into the infraorbital and zygomatic nerves.
- Mandibular, extends to the masticatory muscles of the lower jaw.
The nasociliary nerve innervates the anterior part of the nasal cavity, the inner corner of the eye, the root of the nose, the lacrimal sac, and the eyeball.
Symptoms of neuralgia of the ear node
Neuralgia of the ear ganglion is manifested by attacks of vegetalgia that occur in front of the opening of the external auditory canal, in the parotid region and in the ear on the affected side.
Intense burning or throbbing pain radiates to the lower jaw, behind the ear, to the back of the head, neck and shoulder girdle of the corresponding side. The reflex mechanism of pain irradiation leads to its spread to the upper chest and arm. Painful paroxysms can be provoked by ingestion of hot food or drinks, hypothermia of the face, psycho-emotional stress, and excessive physical activity. The duration of an attack of vegetalgia, as a rule, is several minutes, but can be an hour or more. The dependence of the functioning of the autonomic nervous system on external factors (lighting, barometric pressure, temperature changes, air humidity, etc.) determines the characteristic rhythm of vegetalgia - its occurrence mainly in the evening and at night, exacerbation in the autumn and spring.
In some cases of neuralgia, a paroxysm of pain is accompanied by ear congestion or a sensation of clicking in it. The latter is caused by periodic reflex spasms of the muscles of the auditory tube. Often during an attack, patients note a noticeable increase in salivation, while in the interictal period hypersalivation is not observed. Hearing function is not affected.
Classification of the disease
Charlin's syndrome occurs in two forms:
- Typical neuralgic , occurs when the main nerve trunk is damaged. The clinical picture is classic, that is, the symptoms correspond to the disease. Watery eyes, sore nose and eye area,
- Erased hyperpathic . The nasociliary nerve has a main trunk and small branches. When these nerve endings become inflamed, the picture becomes blurred. Symptoms become atypical. Sensitivity may simply be lost or perception may increase.
Neuralgia can also be unilateral or bilateral. It is divided into acute, subacute and chronic forms.
Causes
Women aged 35-40 years are more likely to get sick . Inflammation of the nasociliary nerve occurs for various reasons:
- Due to improper treatment of teeth in the upper jaw. Nerve endings connect to the teeth. If a branch is touched or damaged, then inflammation occurs. More often after difficult removal or remnants of roots in the hole.
- Pulpitis, periodontitis, gingivitis, periodontitis. With a long process, the infection penetrates the nerves.
- When installing crowns and dentures, galvanism sometimes occurs. The so-called electric current in the mouth. This occurs from the influence of the material that is used to make prostheses. Or simply poorly installed, putting pressure on the fabric.
- Injuries to the face and head. Accordingly, when the skin and muscles are damaged, the nerve is injured. It becomes inflamed and symptoms appear.
- Consequence of surgery on ENT organs. Through negligence, the doctor damages the nasociliary nerve. Or inflammation progresses against the background of sinusitis and sinusitis.
- Bacteria and viruses. Sometimes the infection can immediately reach the nerve endings. But that rarely happens. More often it occurs as a complication of conjunctivitis, otitis, and sinusitis. If the body is weakened, then there is a greater chance of a bacterial infection.

The intensity of pain depends on the etiology . In addition, patients may have several causes of inflammation.
Causes, signs and treatment of Frey's syndrome
Frey's syndrome is a type of facial pain that is rare. What signs can be attributed specifically to this pathology, and why do those suffering from this disease hate chewing gum? By learning about the most effective methods of treating Frey's syndrome, you can get rid of the unpleasant condition faster.
Clinical picture of Frey's syndrome
Frey's syndrome is a set of some symptoms that were first described by the French psychiatrist Baillarger.
The pathology was described in more detail by the Polish scientist Lily Frey, which is why in foreign medical literature this problem is more often called “Frey-Baillarger Syndrome”.
If you look in medical dictionaries, pathology also has synonyms - auriculotemporal syndrome or parotid and temporal neuralgia.
That is, based on the name, the ear and temporal regions are affected as a result of a certain effect on the parotid salivary glands and, as a result, damage to the sympathetic and parasympathetic nerve fibers passing here is observed.
Why does Frey's syndrome appear?
SindromFrey is a diagnosis that in 90% of cases is given to patients due to an unforeseen complication of surgical intervention on the parotid salivary glands or others located within 1-3 cm of tissue. Often, after operations performed in the cervical spine, symptoms of Frey's syndrome appear.
Since, as a result of the surgeon's actions, the nerve endings may be cut in some way, their further development is disrupted, and the nerve fibers may grow excessively, causing discomfort to the patient, or join other glands, changing their own function, thereby also causing inconvenience.
In addition to incorrect actions of the surgeon, risk factors for the development of parotid neuralgia include:
- injuries and tumors of the neck and head;
- inflammatory processes;
- neuralgia of nearby areas.
There are frequent cases of the disease manifesting itself in people who are fond of piercing and scarring.
Neuralgia of the parotid and temporal region is a disease of adults; in rare cases, it is observed in newborns. The causes of the anomaly in children are birth injuries that lead to nerve compression. In persons under 30 years of age, the pathology, if it is not congenital, is not recorded in any source.
How not to miss the development of auriculotemporal syndrome?
Many patients notice signs of Frey's Syndrome several months after surgery. Symptoms are initially temporary and begin more often during meals, that is, during the process of chewing food. Signs of pathology disappear, accordingly, only when the chewing process is completed.
A person suffering from this disease can be recognized by the following signs:
- increased sweating in the ear area;
- redness and hyperthermia of the affected area;
- pain spreading to the lower face and ear;
- numbness of some areas of the skin;
- feeling of stuffiness in the ear.
In addition to the process of chewing, massage or involuntary pressure in the area under the jaw can lead to these unpleasant sensations.
Attacks occur more frequently, and if you do not respond to them, the symptoms will become more pronounced.
With obvious progress of neuralgia, Frey's syndrome will make its existence known even after minor stress or minor hypothermia. Therefore, it is better not to postpone a visit to the dentist.
How is the diagnosis done?
In order to accurately determine Frey's syndrome, it is necessary to exclude a number of other diseases, sometimes similar in several symptoms.
To do this, after an examination, which includes several otolaryngological methods, and collection of data from the patient, specific tests are performed. If at the time of an attack a 2% solution of novocaine is injected subcutaneously, the symptoms will disappear.
Or a solution of starch and iodine is applied to the affected area; when the process is stimulated, the area turns shades of blue.
As part of the diagnosis, radiography and ultrasound are required.
How to get rid of Frey's syndrome?
Parotid-temporal neuralgia can be subjected to conservative therapy and radical treatment methods. First of all, they try to get rid of the root cause of the pathology, eliminate the inflammatory or tumor process. Next, they begin to fight the symptoms of the syndrome.
There are 3 types of drug therapy:
- Analgesics, both tablets and subcutaneous injections, will help relieve pain.
- Ganglioblockers are used if there is a suspicion of excessive growth of the nerve ganglion.
- Antispasmodics and corticosteroid drugs are prescribed.
Physiotherapy procedures are used to assist drug treatment:
- Phonophoresis with corticosteroids and exposure to diadynamic currents are particularly successful.
- They use therapeutic muds and applications with natural ingredients.
If these methods remain powerless against auriculotemporal syndrome, regular injections of butolin toxin, better known in cosmetology as Botox, are used. This substance gives decent results - most symptoms disappear for the entire period of action of the drug. Typically injections are given every 9 months.
In more complex cases, it is possible to excise the nerve fibers in the problem area (maxillofacial surgery), but recently such measures have been carried out only as a last resort, when no other methods have helped. The refusal to perform operations is due to the fact that the percentage of partial loss of innervation of the face is high - by getting rid of one problem, the patient can suffer twice as much.
No one is immune from the manifestation of such a pathology. However, you can try to protect your own health by regular examination by specialists and timely treatment of pathologies. If auriculotemporal syndrome cannot be avoided, there is no need to delay treatment.
Source: https://stomastoma.ru/blog/sindrom-freja/
Main symptoms

When a person touches the skin, the pain intensifies . The mucous membranes and skin swell and turn red. Plus, conjunctivitis occurs (inflammation of the mucous membrane of the eye). Pain sometimes occurs when talking, chewing, or inhaling through the nose.
Signs to look out for:
- pain around the eye, worse in the morning,
- involuntary lacrimation,
- increased or absent sensitivity to light,
- the eyelid does not open completely, blinking occurs frequently,
- feeling of dryness in the eyes.
The pain often occurs at night, can last up to several days, or can quickly subside. Localized in the eye area, behind it. A tightening pain may be felt.
With bilateral inflammation, it occurs first on one half of the face, then on the other. Rarely both at the same time.
Possible patient complaints
With Charlin's Syndrome, a person may complain of constant, piercing pain in the nasal cavity . Even strong and painful. When inhaling. The pain is point-like, that is, it is felt on the face in certain places. The patient can point to the points.

It also occurs in the place where the primary disease was: if otitis media, then in the auricle, pulpitis, in the area of the teeth, in the nose, after a herpes outbreak.
They often complain of pain after treatment has already been carried out . That is, neuralgia takes on a central character. After a long course, the process moves from the branches to the nerve trunk. Therefore, pain is felt even after the cause has been eliminated.
Sometimes it happens that the pain radiates to other places . For example, a patient complains of tooth pain. But there is no pathology in it. This happens because the nasociliary nerve has many branches. These branches innervate the upper jaw, skin, nasal mucosa, eyes, and ears.
What you need to know about trigeminal neuralgia:
- symptoms and diagnosis of the disease,
- treatment methods,
- reasons for the development of inflammation of the ear node and auriculotemporal nerve.
Neuralgia of individual branches of the trigeminal nerve
Neuralgia of the nasociliary nerve (Charlin's syndrome) occurs with sinusitis, inflammatory changes in the paranasal sinuses, concha hypertrophy, deviated nasal septum, dental disease, influenza, and chronic infections.
The nasociliary nerve is a branch of the optic nerve. This type of neuralgia is characterized by attacks of excruciating pain in the area of the eyeball or eyebrow, which radiates to the back and the corresponding half of the nose. Sometimes there is orbital and periorbital pain.
The pain occurs mainly in the evening, at night. The attack lasts up to several hours or even days.
The pain syndrome is accompanied by lacrimation, photophobia, increased blinking, hyperemia, hyperesthesia, swelling of the nasal mucosa on the affected side, discharge of liquid secretion from one nostril, pain on palpation of the inner corner of the nasal cavity and half of the nose.
There may be changes in the anterior part of the eye in the form of keratoconjunctivitis, iridocyclitis, scleral training. A differential diagnostic sign of neuralgia is the disappearance of all symptoms after iadocainization of the mucous membrane of the anterior nasal cavity with 2 ml of a 2% lidocaine solution.
Urgent Care. To relieve severe pain, use a mixture of analgin with diphenhydramine, seduxen, sodium hydroxybutyrate, aminazine.
If the long ciliary nerves are damaged, 1-2 drops of a 0.25% dicaine solution are instilled into the eyes once a day. The pain syndrome is relieved after 2 – 3 minutes.
To enhance the anesthetic effect, use a 0.1% solution of adrenaline hydrochloride (3 - 5 drops per 10 ml of dicaine solution). Instillation is prescribed for 5 – 7 days.
Neuralgia of the auriculotemporal nerve (Frey syndrome), or parotid-temporal hyperhidrosis, or auriculotemporal syndrome. The auriculotemporal nerve belongs to the third branch of the trigeminal nerve and contains sensory and secretory fibers for the auricular ganglion.
It innervates the temporal region, the skin of the external auditory canal, the anterior parts of the auricle and is connected by anastomosis with the facial and other nerves.
It is characterized by the appearance on the affected side in the area of innervation of the auriculotemporal (less commonly, greater auricular) nerve of skin hyperemia, sudden sweating in the parotid-temporal region and paroxysmal pain in the depths of the ear, in the anterior wall of the external auditory canal and in the temple area, especially in the temporal area - jaw joint. Often the pain radiates to the lower jaw. This kind of attack occurs when eating certain types of food (spicy, hard, sour, sweet, etc.), as well as in the presence of a number of external stimuli (hot room, noisy environment, etc.).
During these paroxysms, increased salivation is also observed, and often a change in the size of the pupil (first narrowing and then dilating) on the affected side.
Neuralgia of the auriculotemporal nerve is associated with injuries and previous diseases of the parotid salivary gland, an inflammatory process after surgery for mumps, when autonomic nerve fibers are involved in postoperative skin scars, etc.), leading to irritation of the autonomic fibers running as part of the auriculotemporal nerve. and greater auricular nerves.
Urgent Care. Analgesics are prescribed in combination with antihistamines, tranquilizers, neuroleptics, as well as vegetotropic drugs (Belloid, Bellaeton, Bellataminal), non-steroidal anti-inflammatory drugs (piroxicam, indomethacin, ibuprofen, naproxen, diclofenac, etc.).
To treat this disease, various types of physiotherapeutic procedures with iodine preparations, lidase, aloe injections, and mud therapy are recommended, which promote the resorption of scar and adhesive formations in the area of the parotid salivary gland.
Neuralgia of the lingual nerve. Its occurrence is facilitated by infections, injuries, intoxication, vascular factors, etc.
Diagnosis is based on clinical data: the presence of attacks of burning pain in the area of the anterior two-thirds of the tongue, appearing spontaneously or provoked by eating very rough and spicy food, as well as actions associated with movements of the tongue (talking, laughing). Attacks can occur against the background of chronic infection (tonsillitis, etc.
), intoxication, prolonged irritation of the tongue by a prosthesis, sharp edge of a tooth, etc., more often in elderly people with the phenomenon of dyscirculatory encephalopathy.
Sensitivity disorders (usually of the hyperesthesia type) are often detected on the corresponding half of the tongue; if the disease is long-standing, there is a loss of not only pain, but also taste sensitivity.
Urgent Care. During an attack, sedalgin, baralgin or analgin are prescribed per os (0.5 g 3-4 times a day) or intramuscularly 2 ml of a 50% analgin solution in combination with 1 ml of a 2.5% diprazine solution or 1 ml of 0.5% seduxen solution. The tongue is lubricated with a 1% solution of dicaine, or a 2% solution of novocaine, or a 2% solution of lidocaine.
Subsequently, treatment of the underlying disease, sanitation of the oral cavity, vitamin therapy (vitamins B1, B12), and novocaine electrophoresis are carried out.
In some cases, the use of anticonvulsants such as carbamazepine (finlepsin) is effective according to a scheme similar to the treatment regimen for trigeminal neuralgia (increasing the dosage from 0.2 g to 0.6 - 0.8 g, followed by a decrease to a maintenance dose).
Damage to the facial and intermediate nerve systems. Ganglionitis of the knee ganglion (neuralgia of the knee ganglion, Hunt's syndrome). Features of clinical manifestations: characterized by very strong paroxysmal pain in the ear area, radiating to the back of the head, face, and neck.
lasting a few seconds. Herpetic eruptions appear in the area of innervation of the geniculate ganglion (tympanic cavity, external auditory canal, auricle, auditory tube, palate, tonsils, uvula, often the face and scalp).
There may be symptoms associated with impaired innervation of the facial nerve. There are taste disturbances in the anterior 2/3 of the tongue, sometimes hearing loss, ringing in the ears, dizziness, and horizontal nystagmus.
Subsequently, hyperesthesia occurs in the area of the external auditory canal, tragus, anterior wall of the auditory canal, the anterior third of the tongue and the entire half of the face.
Urgent Care. Analgin, baralgin in combination with diphenhydramine (pipolfen, diprazine) are prescribed intramuscularly, ganglion blockers, tranquilizers (seduxen), antidepressants (amitriptyline), neuroleptics (aminazine), 10-15 ml of 1-2% novocaine solution are slowly injected intravenously.
Neuralgia of the Vidian nerve (Faille's syndrome). The Vidian nerve is a connection between the superficial greater petrosal nerve (a branch of the VII cranial nerve) and the deep petrosal nerve (a branch of the sympathetic plexus of the carotid artery).
The causes of its damage are inflammatory processes in the paranasal sinuses and the apex of the pyramid, less often - injuries and metabolic disorders.
Features of clinical manifestations:
- The pain syndrome is sympathetic in nature. The pain is paroxysmal, localized in the orbit, in the nasal cavity, radiating to the upper and (or) lower jaw, to the back of the head, since the Vidian nerve is connected to the pterygopalatine and geniculate ganglia.
- The pain is localized in the orbit, but the eyeball does not hurt.
- The duration of the attack is from one to several hours, attacks often occur at night.
- During an attack, pronounced autonomic reactions are observed (pallor of the face, hyposalivation).
Urgent Care. Prescribe painkillers (tramadol, analgin, baralgin, sedalgin, etc.) in combination with seduxen, non-steroidal anti-inflammatory drugs, ganglion blockers, antipsychotics and antidepressants. The underlying disease that caused the neuralgia is treated.
Damage to the glossopharyngeal and vagus nerve systems.
Neuralgia of the glossopharyngeal nerve (Weisenburg-Sicart-Robineau syndrome) develops with chronic tonsillitis, damage to the paranasal sinuses, teeth, various processes in the posterior cranial fossa, intoxication and enlarged styloid process.
It is characterized by attacks of pain that always begin at the root of the tongue, tonsils, and pharynx. They are provoked by eating, talking, coughing, pressing on the root of the tongue, pharynx, and tonsils. The pain spreads to the velum, ear, throat, sometimes radiating to the eye, angle of the lower jaw, cheek. The duration of painful attacks is 1-3 minutes, the intervals between them are not equal.
During an attack, a dry cough, taste disturbance, unilateral increased sensitivity in the posterior third of the tongue, and sometimes a decrease or absence of taste are noted.
Loss of consciousness, decreased blood pressure due to inhibition of the vasomotor center, weakened mobility of the soft palate, hypergeusia to bitter in the posterior third of the tongue (all taste stimuli are perceived as bitter), and decreased pharyngeal reflex are rarely observed.
Some patients experience pain on palpation in the area of the angle of the lower jaw and certain areas of the external auditory canal during an attack.
With symptoms of neuritis (neuropathy), hypoesthesia occurs in the upper third of the pharynx and the back of the tongue, the pharyngeal reflex decreases, a taste disorder appears in the back third of the tongue (hypergeusia to bitter), swallowing becomes difficult, salivation is impaired (dry mouth).
Urgent Care. Treatment is carried out according to the same rules as for trigeminal neuralgia of central origin. The most effective is carbamazepine, which gives a pharmacospecific analgesic effect, which is associated with the effect on the central mechanisms of painful neuralgic paroxysms.
Prescribe non-narcotic analgesics in combination with seduxen, non-steroidal anti-inflammatory drugs, vitamin B12. Lubricate the root of the tongue and pharynx with solutions of local anesthetic drugs; in severe cases, 2-5 ml of a 1-2% novocaine solution is injected into the root of the tongue; blockade with trichlorethyl or novocaine in the area of the branching of the carotid arteries is indicated.
Diadynamic or sinusoidal currents are prescribed to the maxillary area. The underlying disease is treated and the oral cavity is sanitized.
Neuralgia of the superior laryngeal nerve (one of the branches of the vagus nerve) is characterized by unilateral paroxysmal pain in the larynx, radiating to the ear and along the lower jaw.
It occurs during eating or swallowing. Sometimes attacks of laryngospasm develop. During an attack of pain, a cough and general weakness appear. A painful point is palpated on the lateral surface of the neck just above the thyroid cartilage.
Neuritis leads to a sensitivity disorder in the epiglottis and a decrease or disappearance of the pharyngeal reflex over time. The affected half of the larynx turns out to be motionless, and the gap may narrow.
Urgent Care. Analgesics are prescribed (2 ml of a 50% analgin solution) in combination with 1 ml of a 1% diphenhydramine solution or 1 ml of a 2.5% solution of diprazine (pipolfen) intramuscularly, novocaine - 10-15 ml of a 0.5% solution intravenously. If necessary, 2.5–5 mg of droperidol and 0.05–0.1 mg of fentanyl (thalamonal) are administered intramuscularly in a hospital setting.
Damage to the autonomic ganglia of the face.
Ganglionitis of the pterygopalatine ganglion (Slader syndrome). It occurs more often with damage to the paranasal cavities, mainly the main and ethmoid ones.
Also important are local inflammatory processes (rhinosinusitis, complicated caries, tonsillitis, otitis media), local trauma and general infections (usually ARVI, less often rheumatism, tuberculosis, herpes zoster), as well as mechanical, allergic, constitutional and other factors that cause pterygopalatine irritation node.
Features of clinical manifestations: characterized by a combination of severe pain and vegetative disorders, to describe which the term “vetative storm” is applicable.
The pain is sharp and begins spontaneously, often at night. Localized in the eye, around the orbit, in the root of the nose on one side, jaw and teeth. The pain spreads to the soft palate, tongue, ear, temporal and cervico-humeral region.
At the same time, hyperemia of half the face and conjunctiva, profuse lacrimation and salivation, rhinorrhea from one half of the nose, swelling of the nasal mucosa, ear congestion, and a feeling of noise in the ear due to changes in the lumen and blood supply of the auditory tube appear.
A painful attack may be accompanied by shortness of breath, nausea, vomiting, photophobia, and muscle spasms of the soft palate. The duration of the pain syndrome ranges from several seconds to 1–2 days or more. The pain intensifies under the influence of sound and light. Paroxysms of pain often develop at night. After the attack, noise in the ear and paresthesia remain.
Slader's syndrome differs from trigeminal neuralgia in the significantly longer duration of attacks, the area of pain spread, the absence of trigger zones, the significant severity of autonomic disorders, and the development of painful paroxysms at night.
An important diagnostic sign is the cessation of the attack after lubricating the posterior parts of the nasal cavity with a 3% solution of lidocaine with adrenaline hydrochloride.
Source: https://www.eurolab.ua/encyclopedia/urgent.medica.aid/2391/
Diagnostics
Diagnosis is based on symptoms, medical history, and research:
- The doctor talks with the patient, finds out the symptoms. Finds out what the pain is and where it is located. Are there any infectious diseases in the head area? For example, otitis media, sinusitis, tooth extraction, adenoiditis.
- Then he examines and palpates the damaged area. The presence of swelling and redness is detected.
- When the doctor roughly presents the diagnosis, he examines for the presence of diseases with similar symptoms. That is, differential diagnosis is carried out. Refers for examination to a dentist and otolaryngologist.
- To determine the diagnosis, there is a method of applying a solution of cocaine hydroxide to the mucous membrane of the front of the nose. If the patient stops feeling pain, then this is inflammation of the nasociliary nerve.
- Next, instrumental studies should be carried out. Ophthalmoscopy, MRI of the head, biomicroscopy, anterior rhinoscopy.
- Once the diagnosis is made, treatment is prescribed.
With the help of additional examination, neuralgia of the nasociliary nerve is differentiated from other diseases. And they establish an accurate diagnosis.
Biomicroscopy of the eye
It is performed using a slit lamp , the main part of which looks like a large slit. The device examines the structure of the eye, the back and front walls. This method allows you to see any damage, foreign body, and detect the disease at an early stage. Biomicroscopy allows you to see the condition of the retina and optic nerve.
Ophthalmoscopy
The fundus of the eye is examined using an ophthalmoscope . With the help of an eye mirror you can see blood vessels and nerves. Identify changes, redness, swelling.
Anterior rhinoscopy

In this case, the nasal septum and passages are visible. This is how redness, curvature, atrophy and hypertrophy are noticed.
Sometimes it is possible to examine the nasal cavity using reflector lighting. It is used to examine children, as they may be frightened by an unknown object.
MRI of the head
To accurately confirm the diagnosis, an MRI of the head is performed . X-ray radiation is not used here. The examination is carried out using magnetic fields, which create an energy change in the examination area. This is how photographs are taken without the use of contrast. A cross-sectional image is displayed on the computer monitor.
Prognosis and prevention

A feature of neuralgia of the nasociliary nerve is the subsidence of pain. The patient thinks that the disease goes away on its own and no treatment is needed. Here lies the danger. Even if the pain decreases, treatment is necessary.
Prevention measures include:
- treat ENT diseases in a timely manner;
- prevent the development of infections in the mouth;
- maintain eye hygiene;
- Follow safety precautions to avoid injury.
Inflammation of the nasociliary nerve is a rare pathology . And it occurs more often as a secondary disease. That is, against the background of other infections in the head area. Timely treatment of sinusitis, caries, otitis, and sinusitis will help avoid neuralgia.
What diseases should not be confused with?
Differential diagnosis, excluding diagnoses with similar symptoms. Charlin's syndrome should be distinguished from:
- inflammation of the sinuses, nasal cavity,
- ganglionitis of the pterygopalatine ganglion (the pain goes away when the posterior part of the nasal cavity is lubricated with a cocaine solution. And with inflammation of the nasociliary nerve in the anterior part),
- neuralgia of the maxillary nerve (burning pain under the eye and upper jaw),
- ganglionitis of the ciliary ganglion (pain radiates to the forehead, temple, root of the nose, forearm, neck).
Diagnosis and treatment of inflammation of the trigeminal nerve
Diagnosis is carried out by a neurologist. He determines the diagnosis based on symptoms. Treatment includes a complex of the following measures: taking medications, physiotherapy, and the use of alternative medicine. If the pain syndrome bothers the patient regularly, then treatment is carried out in a hospital. To detect nerve compression, vascular disease, multiple sclerosis or various tumors in a patient, it is necessary to undergo magnetic resonance imaging.
After the specialist has determined the cause of inflammation of the trigeminal facial nerve, he prescribes anicanvulsion drugs. One of the popular medications is Carbamazepine. It has antiepileptic, psychotropic and neurotropic properties. The course of treatment is 30 days, after which the specialist prescribes an extension of the course or reduces the dosage of the drug. Side effects from the drug are general weakness of the body, nausea, drowsiness. When taking Carbamazepine, you need to take a general blood test and undergo a liver test once every 2 months.
In addition to anicanvulsants, it is necessary to take valproic acid drugs, for example, Depakine or Phenytoin. They have an anticonvulsant effect.
To relax muscles and relieve pain, you need to use drugs that have a positive effect on neuromuscular transmission. The most common among them is Baclofen. It is released in the form of tablets. Contraindicated in patients with hypersensitivity to the components of the drug, with epilepsy, with chronic renal failure. Side effects of Baclofen are drowsiness, weakness, nausea, and loss of consciousness.
In case of severe pain, it is necessary to take sodium oxybutyrate.
Quite rarely, a doctor prescribes the amino acid Glycine; the drug must be taken for a month.
If you have a vascular disease, you must take drugs that have a positive effect on cerebral circulation, for example, Cavinton or Trental.
Physiotherapeutic methods must be used in combination with medications. Among them are darsonvalization, laser therapy, ultraphonophoresis, etc. In some cases, a specialist prescribes radiosurgery.
If the patient treated inflammation of the trigeminal nerve with all of the listed drugs, he also needs auxiliary therapy. To reduce the perception of pain, you need to use antidepressants that affect the brain. For example, the drug Amitriptyline reduces pain and eliminates depression. Diazepam or Pimozide can be used to relieve pain. If the pain is very severe, you need to take Lidocaine or Trimecaine. To alleviate the patient's condition, it is necessary to take tranquilizers.
Treatment methods

When treating neuralgia, the cause must be eliminated. Therefore, the patient is sent for consultation to a dentist and otolaryngologist.
Next, the neurologist prescribes antidepressants with an analgesic effect . They have an analgesic effect based on reducing impulse transmission.
Local anesthetics help relieve pain at the site of application. Typically these are ointments or solutions that are applied to the skin.
Vitamins of group B and PP have a therapeutic effect . Drugs from the group of H-anticholinergics are also used. They act on membrane receptors, blocking access to the nerve impulse. Then there is no pain.
For erased hyperpathic form, non-steroidal anti-inflammatory drugs are effective. They reduce pain and eliminate local inflammation (which forms in one place).
Prescribed as eye drops and nasal spray. If such remedies do not help, corticosteroids are used.
In the presence of primary infections, such as pulpitis, periodontitis, sinusitis, antibiotics are prescribed . Physiotherapy is also used. These are ultrasound, vibration massage, diadynamic currents.
Physiotherapeutic procedures
The following procedures apply:
- SMT or DDT as an anti-inflammatory and analgesic.
This method is more often used for neuralgia after the flu. The temporal artery and stellate ganglion are affected for 2-3 minutes. For bilateral inflammation, a half mask is used. - Electrophoresis . Depending on the cause of neuralgia, different drugs are used. Novocaine, iodine, diphenhydramine, platyphylline.
- Exposure to ultrasound for 5-20 minutes . This reduces pain, improves blood circulation and tissue nutrition.
- Face massage . Light movements for 5-6 minutes. It shouldn't cause pain.
- Exposure to diadynamic current . Eases pain. The procedure lasts 20 minutes.

Neuralgia of the auriculotemporal nerve symptoms and treatment
THE CHIEF CHINESE JOINT DOCTOR GAVE INVALUABLE ADVICE: ATTENTION! If you do not have the opportunity to get an appointment with a GOOD doctor, DO NOT SELF-medicate! Listen to what the rector of the Chinese Medical University, Professor Park, says about this .
And here is some invaluable advice on restoring diseased joints from Professor Park:
Read more >>>
The ear ganglion is relatively rarely the cause of neuralgic pain, but still, you need to be aware of this source of pain associated with the cranial nerves, especially since this type of neuralgia can simulate attacks of otitis media, forcing the patient to consult an otolaryngologist in vain.
A little anatomy
The ear ganglion is a very compact but complex “communication hub”. It includes vegetative and sensory fibers. Let us list its functions, from this it will be clear what features will occur if it is defeated:
- sensitive innervation of the temporomandibular joint. All sensations, including pain that occurs when chewing, pass through this “relay”;
- the ganglion provides sensitivity to the skin of the external auditory canal and temporal region;
- its branches innervate the eardrum;
- it supplies innervation to the parotid gland.
The picture shows an ear node
So, neuralgia of the ear ganglion (ganglion oticum) is a disease that occurs with attacks of acute, shooting pain in the ear and parotid area. Reflection of pain (irradiation) can occur in the arm, chest, but more often irradiation occurs in the neck, back of the head and lower jaw.
Nerve ganglia of the cranial cavity
A characteristic manifestation will be the appearance of hypersalivation during an attack of pain. Hypersalivation is in this case increased secretion of saliva. Additionally, there may be a feeling of stuffiness in the ear and the appearance of shooting pains. Hearing is not affected (unlike neuritis of the facial nerve, when in most cases hyperacusis develops).
It is precisely because many nerve fibers are involved in the anatomy of the ear node that the joint work of a neurologist, dentist and otolaryngologist is required to make a correct diagnosis.
This disease belongs to the group of vegetative ganglionitis, and is adjacent to neuralgia of the pterygopalatine ganglion, ciliary ganglion, submandibular and sublingual ganglia.
Autonomic disorders also cause cervical truncitis and ganglionitis of the superior cervical sympathetic ganglion.
Like other neuralgia of the cranial nerves, neuralgia of the ear ganglion occurs due to the occurrence of foci of pain impulses that form spontaneously as a result of the development of infection. Most often, the following diseases and processes lead to the development of painful attacks:
- acute and chronic parotitis – inflammation of the salivary glands;
- sialadenitis, the formation of stones in the salivary glands with blockage of the ducts and the development of secondary inflammation;
- chronic otitis, including purulent;
- chronic tonsillitis (angina);
- inflammation of the sinuses - frontal sinusitis, sinusitis, ethmoiditis and other sinusitis;
- odontogenic diseases of the dental system and oral cavity - gingivitis, periodontitis, stomatitis.
As you can see, all these diseases are inflammatory. Secondary damage to the ear ganglion is also possible if the source of inflammation or purulent infection is distant from the skull. These may be diseases such as damage to the kidneys and urinary tract (pyelonephritis), septic lesions, pneumonia, including chronic, tuberculous processes.
The most important and constant symptom is severe pain in the area of the external auditory canal, somewhat anteriorly, as well as in the temple area and around the ear.
Like all other neuralgic pains, it is very sharp, similar to an electric shock, burning, throbbing and very unpleasant. It is capable of giving, as already mentioned, to the ear, jaw, and shoulder, respectively, to the side of the lesion.
Also, symptoms of neuralgia of the ear node may be indicated by complaints such as pain in the ear, throat and coughing attacks.
What can trigger an attack of this pain? Most often, this is very hot liquid food - soup, tea, going out into the cold and wind, followed by hypothermia of the face. Intense physical work with a rush of blood to the face (bending work).
This pain, like any other neuralgia, can be provoked by stress or psycho-emotional tension. As a rule, an attack of such pain does not last long - a few minutes, and in any case its duration does not exceed an hour.
Sometimes an attack can be provoked by changes in environmental factors such as changes in atmospheric pressure (since the eardrum, whose innervation is connected to the ear ganglion, is sensitive to these fluctuations). Somewhat less frequently, attacks are activated by changes in air temperature (usually a decrease) and humidity.
All of the above makes it clear that the favorite time of year for exacerbation of this type of neuralgia (as, indeed, for most others - intercostal and trigeminal neuralgia) is spring and autumn.
If the pain reaches a certain threshold, the muscles of the Eustachian (auditory) tube respond to it with a spasm. This spasm leads to a change in pressure in the pipe, and the eardrum, releasing excess air, produces a characteristic “click”. Sometimes a feeling of stuffiness in the ear may occur.
An increase in salivation on the affected side during a painful attack is another characteristic sign of this autonomic disorder. During the “light” intervals, the function of salivation is not impaired.
- Clinically - based on the characteristic pattern of complaints. The diagnosis is confirmed by painful points on palpation of the head - Richet's point, as well as increased pain sensitivity and discomfort in the parotid region;
- By performing a special blockade of the ear ganglion using a local anesthetic - novocaine or a smaller amount of lidocaine. This procedure, in addition to verifying the diagnosis, brings significant relief to the patient. The anesthetic is injected into the Richer point with a simple needle. The substance must be injected between the anterior cartilage of the external auditory canal and the process of the mandible without damaging the temporal artery.
- To exclude signs of inflammation in the parotid salivary gland, a dentist must conduct an examination; an otolaryngologist examines for the presence of chronic inflammatory diseases of the ear, nose and throat.
- A bilateral ultrasound of the parotid salivary gland is performed;
- Magnetic resonance imaging of the brain and bone structures of the skull is mandatory to exclude a space-occupying process.
As always, the measures consist of emergency pain relief and general therapy, which treats the underlying cause and prevents the occurrence of new attacks. Treatment is also considered effective if the duration of the “light” intervals increases.
https://www.youtube.com/watch?v=mG0LLR0_alM
For the purpose of pain relief, in contrast to anticonvulsants for trigeminal neuralgia, ganglion-blocking drugs are used: pentamine, arfonade, pyrylene, benzohexonium.
Antispasmodics (No-Shpa, Halidor, papaverine hydrochloride) have a good therapeutic effect. Unlike trigeminal neuralgia, with neuralgia of the ear ganglion, muscle spasm plays a significant role in the pathogenesis of the disease.
Thus, relaxing the muscles of the auditory tube can reduce pain and discomfort in the ear.
Sedatives (valerian, Persen - Forte, Phytosedan) and hypnotics (zopiclone (Imovan), donormil, phenazepam) are used. Previously, barbiturates were used (luminal, veronal, barbamyl, etaminal - sodium), but now, due to pronounced side effects, they are not used.
According to the scheme, B vitamins are used (including nicotinic acid), electrophoresis is performed with novocaine or thiamine (vitamin B 1).
In the photo - The drug “Milgamma” - combination therapy with B vitamins
If salivation is severe, platyphylline is used to reduce secretion. An important link in the treatment of possible edema is taking antihistamines.
Great importance is attached to physiotherapeutic procedures and methods: magnetotherapy, laser therapy, massage, acupuncture, electroacupuncture, warming biologically active points with wormwood cigars.
It should be noted that relapses of the disease are possible. To avoid them, you need to promptly sanitize the oral cavity, cure your teeth, try not to aggravate existing chronic diseases of the ENT organs, and monitor your blood sugar levels.
How to treat temporal tendonitis?
Unlike other tendon diseases, temporal tendonitis does not impair a person's ability to move, but it is accompanied by very painful and unpleasant symptoms.
Temporal tendonitis occurs everywhere and affects people of any age.