How serious the destruction of personality will be caused by the disease schizophrenia depends on the type of its course. In some patients, symptoms increase over the years; a person can live with a family for a long time and use medications to prolong remission. Others are completely asocial; they cannot work, study, or start a family.
There are gradual, fur-like (development by attacks) and mixed course of schizophrenia. In this article we will talk mainly about the progredient course. This is a type of disease progression in which changes occur slowly and continuously. Such schizophrenia proceeds without remission, the defect in thinking and behavior rapidly increases.
Symptoms of schizophrenia
The first symptoms appear during the period of personality maturation: somewhere from 15-17 years. In men, the debut (onset) of schizophrenia occurs before the age of 25, in women - more often from 20-22 to 35 years.

Everyone's debut manifests itself individually. These can be different manifestations:
- outbursts of uncontrollable, biased aggression;
- an influx of torn thoughts that terribly frighten the patient himself;
- Depersonalization, that is, alienation from one’s own personality, sometimes appears faintly and spasmodically;
- there may be stopping thoughts or parallelism;
- loss of feelings of attachment to family;
- ambivalent emotions.

Over time, the symptoms become more complex. In the case of a continuously progressive course of the disease, these changes appear gradually and increase almost imperceptibly. But still, the process of destruction of thinking is constantly moving forward. Only sometimes the symptoms are alleviated. The following symptoms gradually develop:
- movement disorders appear;
- derealization - when doubts arise about the reality of existing things;
- an unreasonable and irresistible desire to perform some incomprehensible actions;
- inexplicable fears, paranoia, delusional states.
Hallucinations tend to appear much later, after several mood disorders. The progressive course of the pathology may not arouse suspicion among others. But many patients suddenly change their habits, stop taking care of their appearance and leave home to wander. And this is a clear sign of the presence of pathology.
Prevention and treatment
The onset of schizophrenic psychosis can be prevented through an active physical and social lifestyle. A person must have strong personal attitudes, engage in activities that are interesting to him, and constantly strive for self-development.
There is no general system for treating endogenous diseases: in each case, the specialist selects an individual approach to the patient. Timely treatment, as well as a well-chosen technique for this purpose, allows us to make favorable prognosis for the outcome of the disease.
- Drug treatment – taking antidepressants, nootropics, mood regulators, etc. It is prescribed when the patient’s condition is serious.
- Sociotherapy in the form of rehabilitation measures is prescribed in case of social isolation of the patient, his lack of initiative, or decreased professional activity.
- Psychotherapy. It is recommended by doctors in the period between attacks of the disease, when the patient’s condition improves and stabilizes. Its task is to strengthen the patient’s personal attitudes.
- Family therapy. An important role for the effectiveness of treatment is played by the work of a specialist with the immediate environment of a schizophrenic. Moral support from relatives and their understanding of the situation have a beneficial effect on the patient and give him self-confidence. In addition, they must monitor the intake of prescribed medications.
Schizophrenia, regardless of its type and type of course, is a serious mental disorder, the treatment of which should be handled exclusively by a psychiatrist. With its help, a schizophrenic will be able to adapt as much as possible in society without feeling like a defective part of it.
Paroxysmal and progressive course of schizophrenia
In psychiatry, the following types of course of the disease are distinguished: favorable and unfavorable, as well as progressive, mixed and paroxysmal.
A favorable course means a slowly developing personality disorder. Whereas with an unfavorable type, a person becomes completely unrecognizable in 5-8 years and completely loses touch with reality.

The progressive course is characterized by the fact that the patient gradually loses contact with the outside world, but is not aware of this. He has no remissions, the patient cannot understand the reason for the changes occurring. Blurred consciousness and emotional disorders completely “drag” him into the area of distorted perception. The progressive type of course most often affects not teenagers, but people over 30 years of age.
There are sluggish progressive, moderately progressive and malignant types of progression depending on how serious the symptoms are and how quickly the foundations of personality are destroyed.
The paroxysmal course is distinguished by the fact that the patient only sometimes feels attacks. He may be hospitalized once a year, undergo medication therapy, and return to living and working. However, in complex forms, attacks are repeated frequently, more than 3 times a year, and after each attack the psyche rapidly deforms. This leads to disability.
Progress of the disease
Diseases of the schizophrenia spectrum are acquiring new forms and course variations over time. Therefore, psychiatrists are forced to regularly review their classification: an accurate determination of the type of mental pathology makes it possible to prescribe the most effective treatment.
Until recently, the medical literature identified four main types of disease:
- continuously flowing;
- paroxysmal-progressive (fur-like);
- sluggish;
- recurrent (periodic).
Now most psychiatrists insist that the last two types must be considered as mental disorders of the schizophrenia spectrum: schizotypal and schizoaffective personality disorder. Based on this, modern psychiatry began to distinguish two main forms of schizophrenia: furry-like and continuously flowing.
Continuously progressive course
This type of continuous progressive schizophrenia may not make itself felt to others for a long time. The person talks little, behaves distantly, but none of his loved ones will even think that he is sick. In fact, significant changes are happening inside his brain. The core of the personality seems to be torn into two parts. The behavior lacks any purposefulness or logic. A person is unable to make even a simple decision.
The brain begins to work violently and chaotically, creating strange images and sensations in the body. At first, a person is frightened by these states and goes for a long walk alone, chewing on the same thoughts. Students abandon their studies and lock themselves alone in a dark room. Sometimes young people begin to get involved in some strange, frightening esoteric practices that were not previously inherent in them. Gradually, some kind of mania, anxiety disorders, or voices in the head that come from nowhere appear. Emotionally such a person is unstable. You can't put pressure on him.
Stages and degrees of spinal osteochondrosis
The stages of spinal osteochondrosis are also distinguished:
- initial stage of spinal osteochondrosis,
- stage of rupture of the fibrous ring of the intervertebral disc,
- stage of outcome and residual effects of spinal osteochondrosis.
The severity of osteochondrosis of the spine during its x-ray examination:
- straightening of lumbar lordosis, slight flattening of the intervertebral disc, small exostoses, proliferation of uncinate processes;
- slight narrowing of the intervertebral foramina and spinal canal, decreased disc height, spinal instability;
- significant narrowing of the intervertebral foramina and spinal canal.
Features of sluggish schizophrenia
The difference between sluggish schizophrenia is that such an illness develops over years and even decades. However, neither hallucinations nor special delusional states appear. There are some defects in thinking, such as fragmented thoughts or mild depersonalization. However, no significant changes occur. A person learns to live with the fact that his thought stream is a little strange, admits it. His behavior can be somewhat autistic, and his speech is rather pretentious. But he can work in ordinary jobs where serious responsibility is not expected.
Many domestic psychologists previously equated low-progressive schizophrenia with schizotypal disorder.
Features of the hereditary pathology clinic
Any type of pathology (infections, burns, injuries) has its own patterns of clinical manifestation, which are based on the interaction of the damaging factor with the body. Knowledge of these patterns helps the doctor in diagnosing diseases and treating patients. Hereditary pathology, despite the enormous nosological diversity, has some specific features that the doctor needs to know as guidelines in his diagnostic searches.
The characteristics of clinical manifestations of hereditary pathology are based on genetic patterns of action and interaction of genes. Below we will outline the general signs of hereditary diseases, allowing the doctor to suspect the role of hereditary factors in the etiology and pathogenesis of the disease in question.
Family nature of the disease
If a doctor, when examining a patient, receives information about similar cases of the disease in the family, this serves as a direct indication of their possible hereditary nature. Therefore, in the presence of family cases of the disease, a second stage of examination of the patient should be carried out, aimed at differential diagnosis of a specific hereditary disease. At the same time, the presence of the disease in only one member of the pedigree does not exclude the hereditary nature of this disease, since the disease may be the result of a new dominant mutation in one of the parents or heterozygosity of both parents for a recessive disease (segregation of the mutant phenotype).
Chronic, progressive, relapsing course
Hereditary diseases that begin at any age are characterized by a chronic course with a progressive clinical picture.
A few examples.
- Chronic pneumonia with bronchiectasis develops in children with the pulmonary form of cystic fibrosis.
- Long-term digestive disorders occur with celiac disease (synonyms: celiac disease, gluten enteropathy), intestinal form of cystic fibrosis, disaccharidase deficiency.
- Children with Duchenne muscular dystrophy gradually lose motor activity due to muscle atrophy. Due to the progressive nature of the course, this disease is called progressive muscular dystrophy.
Many new forms of hereditary diseases were discovered during the examination of groups of people with chronic pathology.
The chronic process of hereditary diseases develops as a result of the constant action of a mutant gene. The degree of chronicity and progression of the same disease varies in different patients, which is explained by the interaction of genes (the genotype of each person is individual). The recurrent course of hereditary diseases is caused by both genetic and environmental factors. Genetic causes include features of the functioning of genes in a patient, i.e. regulation of their activity within the limits established by the genotype. Environmental factors include complications of the main pathological process (activation of microbial factors, malnutrition) and additional damaging effects (cooling, infections, stress).
Specific symptoms of hereditary diseases
The presence of rare specific symptoms or their combinations in a patient gives reason to think about the congenital or hereditary nature of the disease. For example, dislocation or subluxation of the lens of the eye is characteristic of three hereditary forms: Marfan syndrome, Weil-Marchesani syndrome and homocystinuria. Blue sclera is characteristic of osteogenesis imperfecta and some other connective tissue diseases. With alkaptonuria, the urine darkens on the diapers. Patients with phenylketonuria have a mouse-like odor. If bleeding occurs, one may think of von Willebrand's disease or hemophilia. Rough facial features are characteristic of patients with mucopolysaccharidosis. An asthenic physique with a changed chest occurs in Marfan syndrome. A disproportionate ratio of limbs to torso, low stature, and a peculiar facial skull indicate the presence of achondroplasia. Right- and left-sided asymmetry in the size of the face and limbs suggests hereditary hemihypertrophy.
Multiple pathological changes in organs and systems
The primary involvement of many organs or even systems in the pathological process allows us to think about the hereditary cause of the disease. Most mutant genes that cause hereditary diseases have a pleiotropic effect, as a result of which many organs are involved in the process.
The pleiotropic effect of a gene (pleiotropy is the influence of one gene on the formation of several traits) is a universal genetic pattern that is directly related to the clinical manifestations of hereditary pathology. It is well known that any monogenically determined hereditary disease is always characterized not by a single symptom, but by a specific combination or complex of disorders in different organs and systems. From a clinical and genetic point of view, it is necessary to distinguish between primary and secondary pleiotropy.
The importance of the concept of pleiotropy for medical genetics has been reviewed more than once since its formation. The original view that all aspects of the phenotype, and therefore all manifestations of Mendelian syndrome, depended on a single function (or dysfunction) of the mutant allele has been continually supported by evidence. However, the perception of the importance of pleiotropy gradually diminished, especially in the 1940s, when the “one gene, one enzyme” hypothesis was formulated. Studies conducted in mammals and in patients with inherited connective tissue disorders support the view that “gene” pleiotropy probably does not exist. However, abandoning the concept of pleiotropy would be premature. From a medical-genetic point of view, the concept of the presence of the phenomenon of pleiotropy is legitimate and helps to understand, in some cases, the relationship between the clinical symptoms of diseases.
Primary pleiotropy is due to the biochemical mechanisms of action of the mutant protein or enzyme - the primary products of mutant alleles.
Mutant alleles of various genes that control the synthesis of collagen and fibrillin lead to disruption of the properties of fibrous connective tissue. Since connective tissue is the basis of all organs and tissues, the multiple influences of these mutations on the clinical picture (phenotype) in such hereditary connective tissue diseases as, for example, Ehlers-Danlos and Marfan syndromes are understandable: disturbances in the structure of the vascular wall (especially the aorta), subluxation lens, mitral valve prolapse, skin hyperextensibility, joint hypermobility, etc.
With phenylketonuria, phenylalanine metabolism is disrupted, as a result of which tyrosine is not synthesized. As a result, the formation of melanin decreases or stops, which leads to hypopigmentation of the skin, hair and iris. Pathological metabolites (phenylpyruvic acid, etc.) cause disruption of the development and functioning of the nervous system (increased excitability, tremor, seizures, mental retardation). It would seem that these are very heterogeneous symptoms, but the basis of all these multiple manifestations is the primary effect of the deficiency (or absence) of phenylalanine hydroxylase activity.
Secondary pleiotropy is caused by complications of primary pathological processes. For example, in thalassemia, thickening of the skull bones and hepatolienal syndrome are the result of secondary processes that arose due to increased hematopoiesis and hemosiderosis of parenchymal organs.
Cystic fibrosis is caused by an error in the synthesis of a transmembrane protein that provides ion transport in cells. Impaired ion transport of Na+ and SG leads to the formation of thick mucus in the bronchi or in the exocrine pancreas. This is followed by secondary processes of pulmonary infections and digestive disorders. Both of these are secondary pleiotropic effects.
Thus, the pleiotropic effect of genes determines one of the characteristic features of the clinical manifestation of hereditary diseases - the involvement of many systems and organs in the pathological process. Such an important generalized diagnostic sign of hereditary pathology should serve as a diagnostic guideline for the doctor.
Congenital nature of the disease
Both normal and pathological alleles are involved in different periods of ontogenesis - from embryonic to senile. As emphasized above, the congenitality of pathological signs does not always indicate the hereditary nature of the disease. However, at least 25% of all forms of genetic hereditary diseases and almost all chromosomal diseases begin to form in utero. When a child is born with a complex of pathological signs, the disease is said to be congenital. Examples of congenital hereditary diseases are chromosomal syndromes, achondroplasia, ichthyosis, X-linked hydrocephalus, autosomal recessive true hydrocephalus, etc. Examples of congenital, but not hereditary diseases are rubella, thalidomide, syphilitic, alcoholic, hydantoin and some other syndromes, the etiology of which is established with targeted collection of anamnesis related to the first weeks of pregnancy.
The congenital nature of the disease is often observed in hereditary metabolic diseases. The following list of acute manifestations in infants should “tune” the doctor to diagnose them using biochemical or molecular genetic methods: vomiting, refusal to eat, convulsions, hyperventilation, lethargy, coma, jaundice, hyperthermia, altered tone of the mouse.
Test for schizophrenia
You can distinguish a sane person from a sick person thanks to a special test. The test is called "Mask". A healthy person, when turning the mask, sees an illusory “real” face on the screen, despite the fact that in reality it is curved in the opposite direction. But a schizophrenic with a continuously progressive course of schizophrenia has a different view of reality, a different perception. The fact is that the brain of a schizophrenic, like the brain of a genius, is not susceptible to any illusion. This is due to its high activity.
Schizophrenia in medical literature
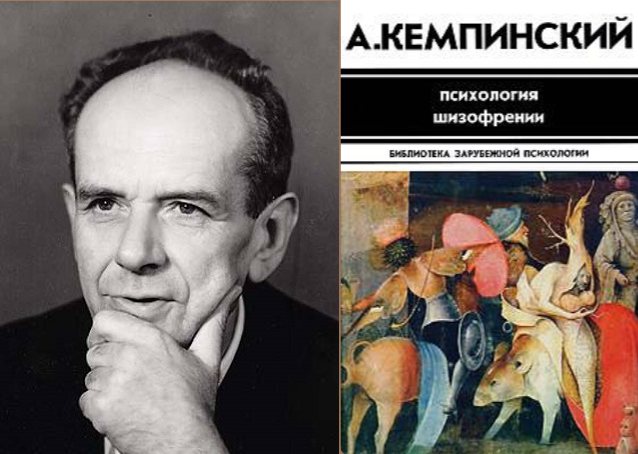
Among specialists in the psychiatric field, the work of the famous Polish philosopher, practicing psychiatrist and psychologist Anton Kempinski is now particularly popular. In his work “Psychology of Schizophrenia,” he originally interprets the causes of the emergence and development of psychosis, which attracted attention.
The psychiatrist calls schizophrenia a mysterious illness, a royal disease, linking it with the wealth of experiences that patients experience. The author notes that, despite numerous descriptions, they are stereotypical, one-sided, fragmentary.
A. Kempinsky, taking into account the description of the clinical picture of schizophrenic disease made earlier, relies on his many years of experience in the treatment and rehabilitation of patients. In his monograph, he scientifically and philosophically proves that schizophrenics are special people who do not need to be excommunicated from society. Their peculiarity lies in the disruption of “information metabolism” - the energy exchange of a sick person with the environment. This is one of the new definitions that the author used in his work.
The educational book is understandable not only to specialists, but also to ordinary people who want to learn more about schizophrenia and look at it from the inside.
Course of spinal osteochondrosis
Course of spinal osteochondrosis:
- recurrent course of spinal osteochondrosis,
- chronically relapsing course of spinal osteochondrosis,
- chronic course of spinal osteochondrosis.
According to the type of course of spinal osteochondrosis:
- regressive type of spinal osteochondrosis,
- non-progressive course of spinal osteochondrosis,
- progressive course of spinal osteochondrosis.
Periods of spinal osteochondrosis:
- debut of spinal osteochondrosis,
- exacerbation of spinal osteochondrosis,
- remission (complete, incomplete) of spinal osteochondrosis,
- period of relative stabilization, residual period of spinal osteochondrosis.
The essence of the disease
The disease is characterized by a sharp deterioration in mental health
Fur-like schizophrenia is the same mental disorder as any other form of the disease, but with its own specific course. The main feature is the sudden onset of exacerbation. In other words, one minute a person is healthy, but experiences a slight decline in mood, and the next moment he develops delusions, hallucinations and other symptoms inherent in schizophrenia. An exacerbation can last from several weeks to several years, and then suddenly goes away as if nothing had happened. A repeated attack can occur at any time, and the trigger is anything.
Thus, a fur coat-like course can be characteristic of any type of schizophrenia.
The second name is the paroxysmal-progressive course of the disease. This term should be analyzed in more detail to understand what we are dealing with. Everything is clear with the word “paroxysmal” - these are periodic exacerbations of symptoms, manifested by attacks, the duration of which depends on the characteristics of the patient. The word “progredient” can be safely replaced with the simpler and more understandable word for Russian people, “progressive”. However, the medical term covers more of a change in the symptoms of a disease. So, this form of schizophrenia is characterized by several features:
- changes in symptoms from attack to attack;
- worsening symptoms;
- increase in schizophrenic defect.
In other words, with each new attack more and more productive symptoms of the disease appear.
In ICD-10, fur coat-like schizophrenia is not designated by a special code. This description is used exclusively by psychiatrists to facilitate patient management in the clinic, but the term itself is not official.
Clinical manifestations of fur coat-like schizophrenia
All types of schizophrenia are characterized by negative personality changes; with this type of disease they begin to appear gradually, increasing after each attack. Fur-like schizophrenia may initially have the following symptoms:
- Obsessive ideas appear.
- The patient begins to consider all his actions as if from the outside; he believes that he cannot manage and control them.
- Paranoid ideas arise, which lead to excessive suspicion, a person looks for his enemies everywhere, and delusions of grandeur appear.
Subsequent symptoms arise as qualitatively new manifestations of a mental disorder. Attacks of this disease have a different clinical picture. Most often this is:
- Depressive-hallucinatory states.
- Acute paranoid.
- Catatonic-depressive.
- Depressive-obsessive states.
This is only a small part; in fact, the manifestations of the disease are much wider.
Fur-like schizophrenia may have varying degrees of depth of developing mental defects. They differ not only in variations, but also in the degree of progression.
In some cases, this form of the disease is close to malignant and can result in schizophrenic dementia. In other situations, progressive tendencies are weakly expressed, and the disease proceeds in a sluggish form, personality defects are insignificant.
Quite often it happens when fur coat-like schizophrenia occupies an intermediate position between two variants of the course. If you ask a doctor about how often such patients have attacks, he will answer that almost a third of all patients with this disease can suffer an exacerbation only once, while in others the pathology reminds itself once every few years.
Personality changes do not directly depend on the number of attacks. Even numerous exacerbations may not result in pronounced manifestations of mental defects.
Residual or residual schizophrenia
This form in its course belongs to the chronic type of pathology. A characteristic feature of this type is the long period of remission after a mental episode. The remission period on average varies from nine to fourteen months. In some cases, patients experience only a single attack in their entire lives; for the rest of the time they are in a state of remission. As a rule, the personality defect in the residual form is not expressed or is completely absent.
The clinical picture develops as follows:
- lethargy;
- lack of initiative, lack of will;
- detachment from society;
- reluctance to self-care, in particular to hygiene procedures.
Positive symptoms in the form of hallucinations and delusions are usually absent or mildly expressed. Negative symptoms manifest themselves to a greater extent, but without significant personality changes, dementia does not develop.
Treatment must be comprehensive; psychotherapy comes to the fore; without it, drug treatment cannot bring the desired result. Social rehabilitation and help from loved ones and specialists are also important.
Causes of development of fur coat-like schizophrenia
At present, it is still not fully understood what reasons lead to the development of fur coat-like schizophrenia. The pathological genesis is not clear, but developmental factors are believed to include:
- Genetic features.
- Features of the human constitution.
- Belonging to a certain gender and age.
It is difficult to recognize the main cause of schizophrenia, but most often it is:
- Anomalies in brain development.
- Hereditary predisposition.
- Exhaustion of the female body during pregnancy.
Whatever factor causes the development of this pathology, therapy should always be carried out. A competent specialist will help improve the patient’s quality of life and return him to normal existence as much as possible.