What is MND?
The structure of a motor neuron
In the brain and spinal cord of every person there are neurons (motoneurons) that are responsible for the motor function of a particular part of the body. As a result of damage to these neurons, a kind of chain reaction occurs, which leads to gradual paralysis of a person. In particular, the patient loses his swallowing reflexes, his speech disappears, his spine ceases to function normally and, as a result, is completely switched off from normal life. In addition, the patient may experience tetraparesis (paralysis of all four limbs). The combination of these symptoms results in the inability to maintain vital functions, resulting in the death of a person.
Motor neuron disease affects older people, mainly 50–70 years old, and this disease occurs in every 2–5 people out of 100 thousand. The average life expectancy of such a patient does not exceed 4 years.
Basis of peripheral movement disorders
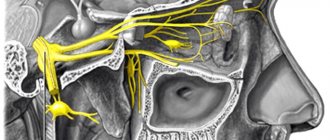
In order to understand the causes of motor disorders when the peripheral parts of the nervous system are damaged, it is necessary to understand the structure of the neuromotor unit. The roots emerge from the spinal cord in pairs: the anterior root is motor, the posterior root is sensitive. Passing through the spinal canal, the sensory and motor roots come together, so all spinal nerves are mixed. They contain efferent and afferent, as well as autonomic fibers from the nodes of the sympathetic trunk. Leaving the intervertebral foramina, the nerves are divided into branches: anterior (innervate the muscles and skin on the anterior surface of the body), posterior (innervate the corresponding structures of the posterior part of the body), meningeal (go to the membrane of the spinal cord) and connective (go to the nodes of the sympathetic trunk). Cranial nerves can have only sensory, only motor, or mixed branches, and the clinic may manifest itself as a violation of sensitivity or movement.
In various diseases, nerve trunks can be affected at different levels, which determines the clinical picture of the pathology.
Main forms of the disease
Motor neuron disease has 4 main forms, including:
- Amyotrophic lateral sclerosis (ALS).
- Progressive bulbar palsy.
- Muscular progressive atrophy.
- Primary lateral sclerosis.
Lateral sclerosis
Damage to the central motor neuron causes this type of disease. ALS is a chronic disease that causes death, usually due to failure of the respiratory system. ALS is the most common type of motor neuron disease. Approximately 80% of MND cases are classified as ALS.
What happens to a neuron in ALS?
Bulbar palsy
This condition affects 10–15% of people suffering from MND. Bulbar palsy is characterized by gradual paralysis of the muscles of the oral cavity, which ultimately leads to failure of the swallowing reflex and death.
Muscle atrophy
Occurs in 5–8% of patients with MND. This disease is characterized by thinning and degeneration of human muscles, as a result of which they atrophy and lose their basic functions.
Primary lateral sclerosis
The rarest form of motor neuron disease, accounting for 2–3% of the total. The disease is characterized by difficulty speaking, deterioration of motor functions of the body, up to complete failure of the legs and the occurrence of related complications.
In addition to the above diseases, the origin of MND can be associated with diseases such as cerebral palsy and spastic paraplegia.
In both cases, the lower neurons are affected, however, in the first case there may be several causes, while in the second the main cause is a genetic mutation.
Difference between a diseased neuron and a healthy one
Motor neuron disease: symptoms, diagnosis and treatment of ALS and other forms of MND
“It all started 9 years ago. I was rock climbing. One day, during another trip to the mountains, my arms and legs suddenly began to cramp while climbing. This happened several times. The first thought was that there was something serious with me, but I immediately laughed at myself in my heart. I decided that such thoughts are paranoia, I’m only 40 years old!”
- What is motor neuron disease
- Different types of motor neuron disease
- Who can get sick
Amyotrophic lateral sclerosis (ALS) is the most common type of motor neuron disease (MND). The disease is also known internationally as Lou Gehrig's disease, motor neurone disease, motor neuron disease or Charcot's disease.
It was the Frenchman Jean-Martin Charcot who first described ALS in 1869, but the disease became widely known after the diagnosis was made to the outstanding American baseball player Lou Gehrig in 1939.
At one time, composer Dmitry Shostakovich, singer and composer Vladimir Migulya, and Chinese dictator Mao Zedong also suffered from ALS.
The most famous person with ALS was the English physicist Stephen Hawking, who lived with the disease for 50 years and is considered the record holder for the longest life expectancy with ALS.
with Russian subtitles.
Reasons for developing ALS
For a long time, the pathogenesis of the disease was unknown, but with the help of numerous studies, scientists were able to obtain the necessary information.
The mechanism of development of the pathological process in ALS is a mutation in the disruption of the complex recycling system of protein compounds that are found in the nerve cells of the brain and spinal cord, as a result of which they lose regeneration and normal functioning.
Targets affected by ALS
There are two forms of ALS – hereditary and sporadic. In the first case, the pathology develops in people with a family history, in the presence of amniotic lateral sclerosis or frontotemporal dementia in close relatives.
The overwhelming majority of patients (90-95% of cases) are diagnosed with a sporadic form of amyotrophic sclerosis, which occurs due to unknown factors.
A connection has been established between mechanical injuries, military service, intense stress and exposure to harmful substances on the body, but it is not yet possible to talk about the exact causes of ALS.
BASS. Risk factors
Interesting: the most famous patient with amyotrophic lateral sclerosis today is physicist Stephen Hawking - the pathological process developed when he was 21 years old. At this time, he is 76 years old, and the only muscle he can control is the cheek muscle.
Stephen Hawking
Direct speech
Elena Zhikina, member of the initiative group of the public association of relatives of patients with ALS:
“When a loved one receives such a diagnosis, you find yourself in a vacuum, both because of the rarity of the disease and because many doctors know nothing about it or consider it hopeless. Yes, there is the Internet, but you only get theoretical knowledge there (although I know people for whom this was enough).
I had a different path: after my loved one was diagnosed with ALS, I was faced with many issues of care and life with such a disease and decided to go to Moscow, where there is a well-established service for helping such patients and the opportunity to get consultations.
As a result, I had a panoramic picture in my head of how and what to do. I also went to Moscow to a special nursing school, after which the idea arose that it would be nice to create a similar system here too. I found support and understanding at the Republican Scientific and Practical Center of Neurology and Neurosurgery.
Now we are only at the beginning of our journey, but the first lesson of the nursing school has already taken place at the Republican Scientific and Practical Center, where representatives of ten families have gathered. There we became acquainted, and people, I see, began to come to life... This is worth a lot, because ALS is a very serious and extremely costly disease.
Let's say we need functional beds, anti-decubitus mattresses, breathing apparatus costing about 4,000 euros, and other special devices.
Symptoms of ALS
As a rule, the disease is diagnosed in adulthood (after 40 years), and the risk of getting sick does not depend on gender, age, ethnic group or other factors. Sometimes there are cases of a juvenile form of pathology, which is observed in young people. In the first stages of ALS, there are no symptoms, after which the patient begins to experience mild cramps, numbness, twitching and muscle weakness.
General information about pathology
The pathology can affect any part of the body, but usually (in 75% of cases) it starts from the lower extremities - the patient feels weakness in the ankle joint, which is why he begins to stumble when walking.
If symptoms begin in the upper extremities, the person loses flexibility and strength in the hands and fingers. The limb becomes thinner, the muscles begin to atrophy, and the hand becomes like a bird's paw.
One of the characteristic signs of ALS is asymmetrical manifestations, that is, symptoms first develop on one side of the body, and after some time on the other .
Pathology may begin in the upper extremities
In addition, the disease can occur in the bulbar form - affecting the speech apparatus, after which difficulties arise with swallowing function, and severe salivation appears.
The muscles responsible for chewing function and facial expressions are affected later, as a result of which the patient loses facial expressions - he is unable to puff out his cheeks, move his lips, and sometimes stops holding his head up normally. Gradually, the pathological process spreads to the entire body, complete muscle paresis and immobilization occur.
There is virtually no pain in people diagnosed with ALS; in some cases, it occurs at night and is associated with poor mobility and high spasticity of the joints.
Criteria for confirming ALS
Table. Main forms of pathology.
| Form of the disease | Frequency | Manifestations |
| Cervicothoracic | 50% of cases | Atrophic paralysis of the upper and lower extremities, accompanied by spasms |
| Bulbarnaya | 25% of cases | Paresis of the palatine muscles and tongue, speech disorders, weakening of the masticatory muscles, after which the pathological process affects the limbs |
| Lumbosacral | 20-25% of cases | Signs of atrophy are observed with virtually no disturbance in the tone of the leg muscles; the face and neck are affected in the last stages of the disease |
| High | 1-2% | Patients experience paresis of two or all four limbs, unnatural expression of emotions (crying, laughter) due to damage to the facial muscles |
Amyotrophic lateral sclerosis (ALS) is an incurable progressive disease of the central nervous system in which the patient experiences damage ... diseases include cramps (painful muscle spasms), lethargy and weakness in the distal arms, bulbar disorders
The above signs can be called average, since all patients with ALS manifest themselves individually, so it is quite difficult to identify specific symptoms. Early symptoms may be invisible both to the person himself and to others - there is slight clumsiness, awkwardness and slurring of speech, which is usually attributed to other reasons.
Important: cognitive functions are practically not affected in ALS - moderate memory impairment and impairment of mental abilities are observed in half of the cases, but this makes the general condition of patients worsen even more. Due to the awareness of their own situation and the expectation of death, they develop severe depression.
How does pathology manifest itself?
Classification
Depending on the location of the primary manifestations of the disease, experts distinguish the following forms:
- Lumbosacral form (impaired motor function of the lower extremities occurs).
- Bulbar form (some nuclei of the brain are affected, which entails central paralysis).
- Cervicothoracic form (primary symptoms appear with changes in the usual motor function of the upper extremities).
On the other hand, experts distinguish three more types of ALS disease:
- Mariana form (primary symptoms appear very early, a slow course of the disease is observed).
- Classic sporadic type (95% of all cases of the disease).
- Family type (differs in late manifestation and hereditary predisposition).
Diagnostics
Diagnosis of amyotrophic lateral syndrome is complicated by the fact that the disease is rare, so not all doctors can distinguish it from other pathologies.
Diagnosis of amyotrophic lateral syndrome
If you suspect the development of ALS, the patient should go to an appointment with a neurologist, and then undergo a series of laboratory and instrumental tests.
- Blood tests . The main indicator of pathology is an increase in the concentration of the enzyme creatine kinase, that is, a substance that is produced in the body when muscle tissue is destroyed.
- Electroneuromyography (ENMG) .
A research method that involves assessing nerve impulses in individual muscles using thin needles. The muscles of the limbs and pharynx are tested, and the results are recorded and analyzed by specialists. The electrical activity of tissues affected by pathology differs significantly from those of healthy ones, and disturbances can be noticed even if the muscle is in good shape and functions normally. Electroneuromyography - Magnetic resonance imaging . MRI in amyotrophic lateral sclerosis is used for differential diagnosis, since with this pathology no pronounced changes in the functioning of the central nervous system are observed. The study allows us to exclude Alzheimer's disease, multiple sclerosis, spinal cord tumors and other similar conditions.
- Transcranial magnetic stimulation (TMS) . An innovative diagnostic technique that allows you to assess the functions of brain neurons that are responsible for motor activity.
Transcranial magnetic stimulation
As additional diagnostic methods, muscle biopsy, lumbar puncture and other studies can be used, which help to obtain a complete picture of the condition of the body and make an accurate diagnosis.
For reference: today, new diagnostic methods are being developed that make it possible to detect ALS in the early stages - a connection has been discovered between the disease and an increase in the level of p75ECD protein in the urine, but so far this indicator does not allow us to judge with high accuracy the development of amyotrophic lateral sclerosis.
Laboratory research
Treatment of ALS
There are no therapeutic methods that can cure ALS - treatment is aimed at prolonging the life of patients and improving its quality.
The only drug that can slow down the development of the pathological process and delay death is the drug Rilutek.
It is mandatory prescribed to people with this diagnosis, but in general it has virtually no effect on the patient’s condition.
Source: //pb17.ru/nevrologiya/bas-bolezn-prichiny-vozniknoveniya.html
Symptoms
Despite the different forms of MND, the manifestation of symptoms is best viewed from the point of view of the location of a person's limbs and certain areas of the human body. So, with this disease the following manifestations are possible:
Hands – the patient is characterized by manifestations of weakness in the hands when performing basic actions (pressing keys on a computer, using a ballpoint pen for writing). Gradually, such procedures may become unavailable to the sick person.
Legs – gradually the patient will not be able to move without assistance.
Expression of feelings - uncontrollable laughter or crying.
Neck and shoulder joints – the muscles of the neck and shoulders gradually weaken, which leads to a deterioration in the respiratory functions of the body.
Speech, swallowing functions - problems with eating food develop, as the person stops swallowing it normally, and possibly speech deterioration, up to the complete loss of the ability to speak.
In addition to the above symptoms, the patient may experience difficulty remembering large amounts of information, and damage to the central motor neuron is characterized by a gradual increase in symptoms. For example, every day it will be more difficult for a person to remember less and less information. Additionally, this may be accompanied by an inability to concentrate attention and low learning ability.
The presence of a symptom such as the inability to remember or find the right words when speaking can also be associated with MND.
Peripheral nerve lesions of the head, neck and upper limb
Peripheral disorders in the head, neck and upper extremities are manifested by the following syndromes:
- Reflex (cervicalgia, cervicocranialgia, cervicobrachialgia, inferior oblique muscle syndrome, Naffziger syndrome (anterior scalene muscle) and many others;
- Compression (cervical myelopathy, vertebral artery syndrome).
In the chest, reflex (dorsalgia, pectalgia), myodystrophic and compression syndromes (radicular and compressive myelopathy) are observed. When peripheral nerves are damaged, reflex syndromes (lumbodynia, lumboischialgia, gluteus minimus or medius muscle syndrome), compression syndromes - radicular, myelopathy, infrapiriformis syndrome of intermittent claudication and piriformis muscle syndrome may occur. The spinal plexuses are formed by connecting branches from certain segments of the spinal cord. The symptoms of their damage allow us to determine the level of localization of the pathological focus.
Cervical plexus
The nerves of this formation innervate the deep muscles of the neck, scalp, neck, ear, diaphragm, and shoulder girdle. The pathology is accompanied by a decrease in muscle tone in these areas, sensitivity disorders, and pain.
Brachial plexus
Peripheral movement disorders with damage to the brachial plexus are determined by the prevalence and localization of the process. With traumatic damage to the superior bundle of this plexus or prolonged throwing of the arms behind the head, for example, during operations, Erb-Duchenne palsy develops, which is characterized by motor disturbances of the proximal arm while maintaining the function of the hand and fingers; the hand hangs like a whip, finger movements are preserved. In case of damage to the lower bundle, Dejerine-Klumpke palsy develops, for which distal plegia is typical, affecting mainly the flexors of the fingers and small muscles of the hand. Total damage to the entire brachial plexus, which can occur with dislocation of the humerus, fractures of the first rib, clavicle, or gunshot wounds in this area, is accompanied by peripheral motor impairment in the form of paralysis.
Quite often, peripheral motor disorders with damage to the brachial plexus develop in case of damage to the median nerve in natural anatomical tunnels. This pathology is characterized by supracondylar-ulnar groove syndrome (excessive flexion of the fingers with severe pain develops), pronator teres syndrome, and carpal tunnel syndrome (severe pain in the fingers, which intensifies when the projection of the median nerve in the wrist area is tapped).
In the case of tunnel neuropathy of the ulnar nerve, peripheral motor impairment is manifested by weakness, followed by atrophy of the hand muscles (this condition develops after prolonged sitting at a desk), weakening of flexion and adduction of the fifth finger.
Thoracic nerves
These structures innervate the intercostal muscles, the skin of the lateral and anterior parts of the chest, as well as the muscular and skin part of the anterior abdominal wall. The most typical motor disorder with peripheral damage to the thoracic nerves is paresis of the abdominal muscles. Also characteristic are girdling, tightening pains in the corresponding areas.
Lumbar plexus
Total damage to this structure is extremely rare. This is possible with fractures of the pelvic bones, spine, in cases of compression by the pregnant uterus, tumor neoplasms, and inflammatory processes in the retroperitoneal space. Most often, lumbar plexopathy develops, which is characterized by pain in the lower abdomen, pelvic bones, lower back, sensitivity disorder in the hips and pelvic girdle, as well as movement disorders in the lumbar spine, knee and hip joint on the corresponding side.
When the femoral nerve is damaged, peripheral motor disorders are manifested by difficulty flexing the lower leg, atrophy of the quadriceps femoris muscle, loss of the knee reflex, and impaired sensitivity of the inner and anterior surface of the thigh. If the nerve is affected above the inguinal ligament, flexion of the hip (its adduction to the abdomen) is impaired, and it becomes difficult to lift the body from a horizontal position.
Sacral plexus
Most often, peripheral motor disorders develop when the femoral nerve, formed from the trunks of the sacral plexus, is damaged. In this case, the flexion of the lower leg is impaired, paralysis of the foot and fingers develops, sensitivity of the entire lower leg and foot is lost, and intense pain syndrome develops.
Causes of the disease
Currently, the causes of MND are not fully understood and the research results are as follows:
in 10% of cases there is a hereditary connection.
in the remaining 90% of cases there is an external influence, including:
- accumulation of heavy metals in the patient’s body;
- advanced age;
- severe psycho-emotional stress;
- excessive sports activities;
- injuries.
In addition, intracellular processes are worth noting as a reason for the progression of a disease such as motor neuron lesion syndrome. These processes are difficult to study, since they take place at the cellular level and do not manifest themselves externally.
For example, surrounding a mononeuron with glial cells contributes to its degeneration. Changes in processes associated with the delivery of nutrients and metabolic products also pose a threat to the normal functioning of mononeurons.
Osteochondrosis
Peripheral motor disorders are more typical for osteochondrosis. The disease is based on damage to the nucleus of the intervertebral disc. Other parts of the spine, musculoskeletal and nervous systems are also involved in the pathological process. There are the following clinical variants of the course of osteochondrosis:
- Primary damage to the intervertebral disc;
- Herniated intervertebral discs. They are formed due to prolapse of the pathologically altered core of the intervertebral disc through a damaged fibrous ring;
- Spondylosis deformans is a manifestation of age-related changes in the spine. They arise due to primary dystrophic changes in the fibrous ring of the intervertebral disc;
- Spondyloarthrosis is a dystrophic-degenerative lesion of the intervertebral joints.
Osteochondrosis is manifested by peripheral motor disorders. It develops under the influence of such factors:
- Genetic predisposition;
- Overload and microtraumas;
- Autoimmune system disorder;
- Dysmetabolic disorders;
- Endocrine diseases;
- Spinal abnormalities.
Diagnostics
For such a complex disease, a simple interview with a doctor is not enough, since some symptoms of the disease have a general orientation. Therefore, electroneuromyography is used to make an accurate diagnosis.
This study allows us to diagnose the slowing of motor processes in neurons.
In addition, the patient undergoes magnetic resonance imaging (MRI), which is necessary to exclude a number of diseases with similar symptoms.
Treatment
As a rule, motor neuron syndrome is an incurable disease, and all efforts of doctors are aimed at prolonging the patient’s life and eliminating the symptoms of the disease.
Medicines prescribed to the patient:
- creatine;
- carnitine;
- Rilutek;
- complex of vitamins.
The main drug is Rilutek. This drug reduces the amount of glutamate during the transmission of nerve impulses. Its analogue is a foreign medicine that is not available to citizens of the Russian Federation - Riluzole. In terms of effectiveness, this medicine is undoubtedly better than Rilutek, but the principle of action of the drugs is almost the same.
Elimination of symptoms of MND includes treatment of muscle spasms, elimination of disturbances in the gastrointestinal tract, respiratory system, etc.
Thus, as a preventive measure for the respiratory system, a drug is used for artificial ventilation of the lungs, and in case of problems with swallowing and eating food, the patient is fed using a special tube.
Causes of peripheral movement disorders
Depending on the level of damage to peripheral nerve structures, all damage to peripheral nerves is divided into 5 groups:
- Vertebrogenic lesions (with such diseases the brain structures are directly affected);
- Damage to nerve roots, plexuses, nodes (radiculitis, meningoradiculitis, ganglionitis, plexitis, traumatic damage to the plexuses);
- Multiple lesions of nerve trunks and roots (infectious polyneuritis, infectious-allergic polyradiculoneuritis, polyneuropathy of allergic, toxic, dyscirculatory, dysmetabolic origin);
- Lesions of individual spinal nerves (compression-ischemic, traumatic, inflammatory);
- Damage to the cranial nerves (neuralgia, neuritis).
The main causes of vertebrogenic lesions accompanied by peripheral motor disorders are degenerative lesions of the spine (spondylosis, intervertebral osteoarthritis, formation of osteophytes), changes in anatomical structures (stenosis of the spinal canal, lumbarization, sacralization), spondylolisthesis (instability of spinal segments), systemic connective tissue diseases (sacroiliitis , ankylosing spondylitis), spinal fracture, infectious lesions, primary tumor foci or metastases.
One of the typical symptoms of damage to peripheral nervous structures is radicular syndrome - a set of symptoms that occur when a spinal root is damaged (usually compressed). This disorder is characterized by the following symptoms:
- Pain syndrome – shooting sensations in the area of innervation of the affected root;
- Peripheral motor disorders – paresis of individual muscles or their groups;
- Impaired sensitivity in the innervated area.
Famous people diagnosed with MND
The most famous people who suffer from MND to one degree or another abroad are Stephen Hawking, and in the Russian Federation - Yulia Samoilova.
Stephen Hawking suffers from amyotrophic lateral sclerosis, and Yulia Samoilova's disease is called spinal muscular amyotrophy (Werdnig-Hoffmann amyotrophy).
So, MND is a serious and deadly disease from which no one is immune, and for this reason it is extremely important to listen to the signals that your body sends you and in no case neglect going to the doctor. Take care of yourself and your loved ones!