Viral meningitis is most often caused by enteroviruses, which can be transmitted both through the air and by eating unwashed vegetables and fruits. It is worth noting that children more often suffer from viral meningitis because they have an immature immune system and their body is not able to fight this kind of virus.
Causes of infection
You can get meningitis at any age. There are many causes of the disease:
- Viral meningitis in children is caused by bacteria of chickenpox, mumps, measles, scarlet fever;
- Purulent wounds near the brain (on the face, neck, head);
- Insect bites (encephalitis ticks, mosquitoes);
- In old and senile age, the cause of the disease can be fungi;
- Tuberculosis (this type is the most dangerous, difficult to treat and leaves consequences).
A person can catch the infection anywhere: when swimming in bodies of water, through saliva, through food and water.
Viruses that cause meningitis:
- Enteroviruses that cause intestinal diseases;
- Staphylococci, which were formed as a result of pneumonia, sepsis, abscesses;
- Herpes can cause viral meningitis;
- Tuberculosis bacillus;
- Mumps, HIV;
- Fungal infections, candidiasis.
There are cases when infectious bacteria join enteroviruses, causing purulent inflammatory processes. This leads to the development of serous meningitis with complications in the functioning of the central nervous system and brain.
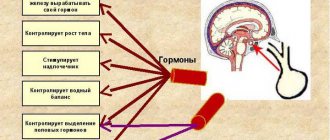
Causes
The disease can develop either independently, when a virus enters the body, or against the background of a previous infection. The disease is most often provoked by enteroviruses (Coxsackie and ECHO), which affect the intestinal mucosa. Viral meningitis can also be caused by herpes virus, adenovirus, cytomegalovirus and other infections.
Most often, outbreaks of meningitis of viral origin occur in the summer. The disease begins to progress very quickly and is easily treatable with timely diagnosis. Symptoms resemble cerebral arachnoiditis.
Depending on the causative agent of the disease, there are many types of viral meningitis that have similar symptoms. Let's look at them in more detail.
General symptoms
Signs of meningitis in children and adults appear quite quickly and are:
- Chills, fever with high body temperature (up to 40 degrees);
- Impaired consciousness, hallucinations;
- Fear of bright light (patients try to turn towards the wall and cover their heads);
- Regardless of food intake, nausea and vomiting begin, which does not bring relief;
- Bursting, sharp pain in the head, worsening when turning, from loud sounds and bright light;
- Inability to pull the head to the chest and straighten the legs.
Infectious meningitis
The incubation period is the period of time between the entry of an infectious pathogen into the body and the appearance of the initial signs of the disease. Meningitis is an infectious disease in which the inflammatory process develops in the membranes of the brain and spinal cord. The causative agents of meningitis are transmitted from a sick person to a healthy person through airborne droplets or contact. Sometimes infection occurs by eating food contaminated with animal excrement, water contaminated with microorganisms, or insect bites. The first signs of the disease do not appear immediately after the patient becomes infected. The incubation period ranges from 4 to 10 days. At the Yusupov Hospital, doctors use modern laboratory tests to make a diagnosis and conduct instrumental examinations using the latest diagnostic equipment from the world's best manufacturers.
Treatment begins immediately after an accurate diagnosis has been established. Antibacterial and antiviral therapy is carried out using the most effective drugs to which meningitis pathogens are sensitive. To treat patients, drugs registered in the Russian Federation are used, which have a minimal range of side effects.
Incubation period and symptoms of meningococcal meningitis
Meningococcal meningitis refers to bacterial forms of inflammatory diseases of the meninges. The causative agents of the infection are Neisseria meningitis of 12 serological groups. Infectious agents are transmitted from person to person through droplets of secretions from the throat and upper respiratory tract of the carrier or patient. The spread of microorganisms is facilitated by close and prolonged contact (kissing, sneezing or coughing towards another person, living in close proximity to an infected person, sharing utensils). Typically, the incubation period for meningococcal meningitis in adults and children lasts 4 days, but can vary from 2 to 10 days.
The most common symptoms of meningococcal meningitis are:
- stiff neck;
- heat;
- headache;
- nausea and vomiting;
- increased sensitivity to light;
- confusion.
Neurologists make the initial diagnosis of meningococcal meningitis through a clinical examination followed by a spinal tap to obtain and examine cerebrospinal fluid. Sometimes bacteria can be seen when examining the cerebrospinal fluid under a microscope. The diagnosis is confirmed by growing microorganisms from cerebrospinal fluid or blood samples based on an agglutination test or polymerase chain reaction. To determine measures to combat infection, laboratory technicians identify the serotype of the pathogen and determine sensitivity to antibiotics.
A patient with meningococcal meningitis is hospitalized in a neurology clinic. Antibacterial therapy begins immediately after a spinal puncture. Antibiotics are administered intramuscularly or intravenously: penicillin, ampicillin, chloramphenicol or ceftriaxone. Before the first antibiotic injection, glucocorticoids are administered intravenously. Dehydration therapy is carried out with Lasix, furosemide or mannitol. Infusion therapy consists of intravenous drip administration of solutions that have a detoxifying effect and replenish fluid loss by the body.
Viral meningitis
The incubation period for viral meningitis varies between 2-10 days. When infected with enteroviruses - from 1 to 18 days, with the mumps virus - up to three weeks, more often from 10 to 18 days. The incubation period of acute aseptic meningitis (Armstrong's choriomeningitis) lasts from 8 to 12 days.
The disease is most often caused by the ECHO and Coxsackie viruses, mumps, herpes simplex (type II), influenza, measles and rubella. In the prodromal period, the symptoms of viral meningitis resemble those of an infectious disease, the complication of which is inflammation of the meninges. Patients are worried about malaise, headache, and catarrhal symptoms are detected. Body temperature may rise to 40 o C, nausea and vomiting may occur.
After 3-5 days, meningeal signs appear:
- rigidity, tonic tension of the muscles of the neck and back of the head;
- Kernig's sign (inability to straighten the leg at the knee);
- Brudzinsky (flexion of the leg and thigh);
- hyperesthesia (photophobia, intolerance to noise and sounds).
With secondary serous meningitis against the background of mumps, all groups of lymph nodes may enlarge. A skin rash is characteristic of viral meningitis caused by the Coxsackie virus serotype and ECHO. Often there are no symptoms of viral meningitis.
At the Yusupov Hospital, patients with viral meningitis are treated aimed at destroying infectious agents, development mechanisms and symptoms of meningitis, immediately after taking samples of cerebrospinal fluid and blood for laboratory testing. Doctors take an individual approach to the choice of drug doses depending on the age and severity of the patient’s condition. Only drugs that do not have side effects are used.
Pneumococcal meningitis
People with weakened immune systems, especially young children, are susceptible to pneumococcal meningitis. The disease is severe and often causes serious complications. The causative agent of the infection is pneumococcus. Microorganisms are transmitted from a sick person or bacteria carrier through airborne droplets and contact. When a patient develops meningitis, there are no symptoms in adults during the incubation period.
The incubation period (from the moment of infection to the appearance of the first signs of meningitis) can range from one to three days. The disease begins acutely and is characterized by the following symptoms:
- high temperature up to 40°;
- chills;
- increasing pain in the head;
- signs of intoxication;
- vomiting;
- involuntary trembling or cramps of the limbs;
- photophobia and intolerance to loud sounds;
- increased skin sensitivity;
- weakness.
Young children are more susceptible to the disease. They exhibit the following symptoms:
- signs of increased intracranial pressure;
- severe shortness of breath;
- swelling of the fontanelle;
- moaning cry and crying;
- blue discoloration of the nasolabial triangle, tip of the nose and fingers;
- Frequent regurgitation or severe vomiting.
By the second or third day of the disease, stiffness of the neck muscles, meningeal symptoms, and complete or partial paralysis of the limbs appear. Paralysis of the oculomotor nerves may then develop.
In order for the treatment of pneumococcal meningitis to be effective, doctors at the Yusupov Hospital begin antibacterial therapy for pneumococcal meningitis immediately after taking blood and cerebrospinal fluid samples. With pneumococcal meningitis, the cerebrospinal fluid is turbid and viscous, acquiring a greenish tint. The amount of glucose in the liquor decreases, the content of protein and cellular elements increases.
Treatment of pneumococcal meningitis in adults is not carried out during the incubation period, since the symptoms of the disease do not allow an accurate diagnosis to be made. After identifying the causative agent of the infection and determining the sensitivity of pneumococcus to antibiotics, targeted antibacterial therapy is carried out. If there are contraindications for performing a lumbar puncture, empirical treatment of meningitis is carried out with antibiotics, to which most pneumococci are sensitive. Penicillins, carbapenems, cephalosporins or vancomycin are most often used.
Complex treatment of pneumococcal meningitis includes symptomatic and pathogenetic therapy, dehydration treatment, and immunostimulation. If a condition that threatens the patient’s life develops, doctors in the intensive care unit provide oxygen therapy through nasal catheters or, if indicated, perform artificial ventilation of the lungs using the latest ventilators.
Incubation period in adults
The nature of the first symptoms of meningitis depends on its type.
Infectious. The incubation period lasts from one to ten days from the onset of infection, usually 5-6 days. Immediately after the virus is introduced into the body, a person begins to feel weak, a sharp increase in temperature, often nauseated and loss of appetite. Even in the initial stage of the disease, the patient experiences dizziness and severe headaches.
Serous. It is characterized by a very short incubation period - from several hours to 2-3 days. At the onset of the disease, the patient experiences severe pain in the head, accompanied by frequent vomiting and an increase in body temperature up to 40 degrees. Serous meningitis develops mainly in people living in large cities.
Viral. The incubation period lasts from 2 to 4 days. Symptoms are similar to serous meningitis. In addition to severe headaches that cannot be relieved by any painkillers, the person experiences a disorder of consciousness.
Purulent. It is considered one of the most dangerous forms of meningitis. A few hours after infection, the patient begins to experience pain in the back of the head. After this, the headache gradually increases and spreads. Many patients experience seizures and spend most of their time delirious.
The very first signs of meningitis are similar to the symptoms of influenza and acute respiratory infections. This causes late consultation with specialists.
Types of viral meningitis
One of the most severe viral meningitis in its manifestations is encephalitic meningitis , since not only the membranes are affected, but also the brain tissue. This disease can occur after suffering purulent diseases of the ENT organs, mumps, or with a herpetic infection.
Important! In the absence of proper treatment, encephalitic meningitis progresses to a severe stage, when focal meningeal lesions of the brain occur. In this case, neurological disorders are noted, in the form of hallucinations, disturbances of consciousness and sleep.
Herpetic meningitis most often develops in people who previously had genital herpes, since the causative agent of this disease is the herpes simplex virus. In rare cases, it can be caused by the varicella zoster virus.
Important! The causative agent of herpetic meningitis remains in the human body for life, manifesting itself when immunity decreases.
Influenza and tuberculous meningitis is also a type of meningitis of viral origin, but it is quite rare.

Incubation period in children
Unlike adults, children may not always complain of a headache. But based on the child’s behavior, one can suspect incipient meningitis:
- The baby becomes sleepy, lethargic, and becomes hungry;
- Periodic vomiting appears (regardless of whether the child has eaten or not);
- Body temperature rises (up to 39-41 degrees);
- In a lying position, the baby stretches his body and constantly throws his head back;
- Reaction to bright lights and loud sounds is negative;
- In infants, the fontanel (the area between the bones of the skull) swells;
- Convulsions with short-term cessation of breathing may occur;
- When picking up an infant in his arms, he pulls his legs towards his chest;
- With some types of meningitis, a dark red (brown, purple) rash appears on the child’s legs and buttocks.
If at least 2-3 such signs are detected, it is necessary to urgently call a team of doctors. Even if the disease is not meningitis, such symptoms require immediate hospitalization of the baby.
Incubation period of meningitis: duration and features
Meningitis is a disease of infectious etiology (pathogens: bacteria, viruses, protozoa, mycoplasmas, chlamydia, parasites) with different routes of transmission and varying duration of the incubation period. It is characterized by inflammatory processes affecting the membranes (soft, arachnoid) of the brain - brain, spinal cord.
The nature of the course is distinguished: fulminant (the clinical picture develops within 24 hours), acute (rapidly progressing with worsening symptoms), chronic (lasts longer than 4 weeks). Complications: toxic shock, confusion, stupor, coma, convulsive syndrome.
Definition of pathology
Meningitis of any form is contagious. Incubation period is the time period from the moment an infectious agent enters the body until the symptoms of meningitis appear. Incubation is a latent period of the disease, when the pathogen that has entered the body actively multiplies, creating a colony that can cause pathological processes. The duration of incubation depends on the number and degree of activity of the invading infectious agents.
The duration of the period is influenced by the state of the patient’s immune system. For example, pneumococci, getting on the mucous membrane of the oral cavity and upper respiratory tract, can be asymptomatically present in the body for a long time. The inflammatory process involving pneumococci develops as a result of provoking factors - hypothermia, acute respiratory diseases, influenza.
Types of disease
The duration of the incubation period for meningitis varies depending on the type of pathogen, the individual characteristics of the body (the degree of activity of the immune system, the presence of chronic somatic diseases, the age of the patient) and the nature of the course. Taking into account the type of pathogen and the nature of the course, the following forms of pathology are distinguished:
- Viral. Initiated by encephalitis, mumps and herpes simplex viruses, cytomegalovirus, enteroviruses (Coxsackie, ECHO). The incubation period of viral meningitis is usually about 2-4 days.
- Bacterial. Pathology is initiated mainly by meningococci, staphylococci, pneumococci, tuberculous mycobacterium, and hemophilus influenzae. Chronic forms are characterized by damage by Borrelia (Lyme disease), Treponema pallidum (syphilis), and Leptospira (leptospirosis). The incubation period for bacterial meningitis is on average 4 days. The incubation period can vary from 2-10 days.
- Purulent. Characterized by inflammatory processes with the formation of pus. The main pathogens: streptococci, Haemophilus influenzae and Escherichia coli, pneumococci. Risk factors include injuries and surgical interventions in the head area. An analysis of the cerebrospinal fluid reveals an increased concentration of white blood cells. The incubation period of purulent meningitis often varies between 2-5 days.
- Serous. Characterized by serous changes in the cerebrospinal fluid. Analysis of the cerebrospinal fluid reveals lymphocytic pleocytosis. It develops mainly with the participation of polio viruses, mumps, enteroviruses, and less often with the participation of bacterial microflora - mycobacterium tuberculosis, treponema pallidum. It is transmitted by sneezing, coughing, touching, or shaking hands. The incubation period for serous meningitis averages about 1-18 days.
Meningitis is detected in 50% of patients diagnosed with tick-borne encephalitis. Incubation of tick-borne encephalitis lasts 1-30 days. Fungi such as Candida and cryptococci can also provoke the disease. The secondary form of the disease develops against the background of the primary focus of the infectious lesion:
- Otitis is inflammation of the inner ear.
- Sinusitis is inflammation of the paranasal sinuses.
- Tuberculosis is a source of infection in the lungs.
- Osteomyelitis is a source of infection in bone tissue.
- Pulpitis, gingivitis, periodontitis and other infectious diseases of the oral cavity.
At risk are people with diagnosed diseases - lymphoma, septic endocarditis, chronic pathological processes in the cranial paranasal sinuses, purulent processes in the chest, diabetes. This group includes patients after treatment with immunosuppressants for a long time.
Characteristics of the incubation stage
The risk of infectious damage to nervous tissue increases in patients who have undergone surgery in the cranial area, surgery to bypass the ventricular system, or with a history of traumatic brain injury. The following factors play an important role in the pathogenesis of meningitis:
- Properties of the pathogen. Virulence (the degree of the pathogen’s ability to infect the body), neurotropism (the desire of the pathogen for nervous tissue).
- The reaction of the body of an infected person. Influencing factors: age, dietary habits, social and living conditions, previous injuries in the head area, immune status.
- The background on which microorganisms and macroorganisms come into contact. Influencing factors: overheating, hypothermia, insolation (exposure to sunlight).
Depending on how meningitis is transmitted, the length of the incubation period may vary. With oral and airborne infection, the disease often develops faster. Main routes of transmission:
- Contact and household. The infection is transmitted from a sick person by coughing, sneezing, or talking through airborne droplets. The agent enters the mucous membrane of the mouth and nasopharynx, from where it spreads throughout the body through the bloodstream. The agent is transmitted by contact if personal hygiene is not observed.
- Hematogenous. The spread of pathogens throughout the body occurs through the bloodstream. This path of development of the disease is associated with the presence of foci of inflammation in different organs, from where pathogens enter the area of the meninges through the bloodstream. When inflammation of the respiratory tract, tuberculosis, syphilis, toxoplasmosis, candidiasis, Lyme disease, and autoimmune connective tissue diseases is detected, the risk of meningitis increases.
- When using invasive medical equipment (intravenous catheters, surgical instruments).
- Placental. The infectious agent is transmitted from mother to fetus. In medical practice, this route of transmission of meningitis is rare.
- Perineural. Through layers of connective tissue.
You can become infected by swimming in a body of water, if the water is contaminated and there are sick people or carriers of the infectious agent in the water pool at the same time. You can get sick by eating contaminated food and water. Some types of pathogens are transmitted by the bite of insects, mainly encephalitis ticks.
In adults
Initial symptoms of meningitis in adults may occur during the incubation period. A febrile state (chills alternating with fever) develops against the background of toxic damage to the body. As a result of the active reproduction and activity of pathogenic microorganisms, toxic substances are released that provoke such reactions.
After the agent penetrates the tissues of the nervous system in the area of the meninges, the first meningeal and cerebral symptoms appear. Symptoms are associated with irritation of the membranes. This period is characterized by increased production of cerebrospinal fluid with a violation of its resorption - absorption. Other primary signs:
- Swelling of brain tissue in the area of the membranes.
- General intoxication of the body.
- Increased intracranial pressure values. Against the background of a destructive process, hydrocephalus develops.
After the incubation period of meningitis is completed, changes occur in the body of adults (increased permeability of the blood-brain barrier, damage to the endothelial layer of intracranial capillaries, impaired blood microcirculation, metabolic disorders, hypoxic processes), which subsequently lead to the appearance of characteristic symptoms.
In fulminant and acute cases, symptoms may appear several hours after incubation. On visual examination, Kernig's and Brudzinski's symptoms, increased body temperature, pain in the head area, and other meningeal signs are observed.

In children
Against the background of the proliferation of pathogenic microflora, cerebral edema often develops, which leads to the appearance of cerebral, focal symptoms (stupidity, depression of consciousness, convulsions) in the early stages of the disease. Following the incubation period, children develop initial symptoms of meningitis:
- Body temperature rises to 38-41º.
- Pain in the head area, dizziness. The pain is diffuse, intense, bursting.
- Hemorrhagic rash.
- Lack of appetite.
- Apathy, lethargy, drowsiness or, on the contrary, increased irritability, psychomotor agitation.
- Increased sensitivity to external influences - bright light, loud sounds.
- Lessage's sign (in infants).
Rigidity of the neck muscles - hardness, spasticity, inflexibility, myalgia - pain in the muscle tissue, tachycardia - heart rhythm disturbance, hyperemia - redness of the facial skin, complement the overall picture of the initial manifestations of the pathology.
Possible consequences
In childhood and adolescence, the consequences of meningitis can be life-threatening. The physiological structure of the child's body predisposes to the occurrence of generalized, pronounced reactions - neurotoxicosis, convulsive and encephalic syndrome. Common complications: stupor, psychomotor agitation, hyperkinesis, coma, mental disorders.
In severe cases, progressive cerebral edema develops. If the condition worsens, the likelihood of dislocation of brain structures increases, which can lead to respiratory and cardiac arrest and death. In cured children, the consequences of the illness can be expressed in the occurrence of epilepsy, inhibition of mental development, and hearing loss.
The duration of the incubation period varies significantly depending on the individual characteristics of the infected person, the type and degree of activity of the pathogen.
YOU MAY BE INTERESTED in: Serous meningitis prevention Moderate meningitis consequences Windy meningitis
Diagnostics
Procedures for an accurate and definitive diagnosis are carried out in a medical setting.
These include:
- Laboratory tests of the patient’s urine, feces and blood;
- Bacteriological examination of mucus taken from the nasopharynx;
- Lumbar puncture (taking cerebrospinal fluid).
Diagnosis carried out during the incubation period (1-2 days after infection) makes it possible to begin timely treatment, as a result of which 95% of patients fully recover.
Characteristics of the disease
An increase in incidence is observed approximately once every 5 years.
This is due to the fact that it is precisely this period of time that the virus needs in order to mutate and become immune to existing methods of protection.
Most often, meningitis of enteroviral etiology occurs in the summer and autumn . The virus, having penetrated the body, spreads, penetrating, in particular, into the membranes of the brain, causing their inflammation.
After some time, the child begins to show the first symptoms, and the clinical picture develops rapidly.
And if at the initial stage of development of the pathology the child feels only a slight malaise, similar to the manifestations of ARVI, then after a short period of time the baby’s condition sharply worsens.
Complications
A severe illness leaves behind serious complications. These include:
- Strabismus;
- Blindness;
- Hearing loss;
- Paralysis;
- Developmental delay, hydrocephalus in children;
- Thinking disorders in adults;
- Epilepsy;
- Death.
If the course of the disease is unfavorable, by the end of the first week of treatment the patient falls into a coma and convulsions become more frequent. Everything ends in death.
Complications occur in 15-20% of those who have had meningitis. The likelihood of complications depends on the severity of the infection. Most often, complications occur after bacterial meningitis, less often after viral meningitis.
Traditional treatment
It is impossible to get rid of the symptoms of meningitis infection in adults using traditional medicine recipes. Such remedies will only help you alleviate your condition until a doctor or ambulance arrives. They are also used to speed up the recovery period. We strongly recommend taking the following herbal decoctions, which have powerful anticonvulsant, diuretic and antipyretic effects:
- 3 tsp. dry lavender, pour 500 ml of boiling water and leave the resulting mixture for 10 minutes. Drink 100 ml of this decoction 4 times a day.
- Pour a tablespoon of poppy seeds into a glass of preheated milk and leave for 12 hours. After this, drink 3 times a day about half an hour before meals.
- Pour 10 grams of crushed cranberries into a faceted glass of boiling water, leave the resulting mixture for 4 hours. After this, drink 70 ml of the medicine three times a day.

Treatment
All procedures for the treatment of meningitis are carried out in a hospital setting. The length of stay in a medical facility depends on the type of infection and the presence of complications.
Drugs and procedures:
- Antibiotics (intravenous and intramuscular administration);
- Disinfection therapy (intravenous administration of hemodez, plasma, albumin, glucose, etc.);
- Prescription of B vitamins, glucocorticoids, ascorbic acid;
- Diuretics to prevent brain swelling;
- Oxygen therapy (oxygen and nasal masks).
If therapy in the early stages of the disease is effective, the patient will spend no more than a week in the hospital. In complicated cases, treatment in a medical setting can take up to several months.
Treatment of pneumococcal meningitis
Pneumococcal meningitis
– a disease that requires immediate medical treatment in a hospital. During therapy, the patient must adhere to bed rest and eat high-calorie foods with a rich chemical composition. To combat the symptoms of meningitis infection in children, drugs with the active ingredients Ceftriaxone, Benzylpenicillin, and Cefotaxime are most often prescribed. For these purposes, medications such as Tetracycline, Sulfanilamide, Vancomycin are also used.

To get rid of traces of pathogenic organisms and completely cleanse the internal environment of them, detoxification therapy is carried out: it includes drinking plenty of fluids and drips with a solution of glucose, sodium chloride and salt.
If pneumococcal meningitis occurs in a person with a weakened body, he is injected with fresh frozen plasma or leukemia.
To speed up treatment and relieve swelling of the brain, specialists prescribe patients a number of diuretics, such as Manitol or Furosemide. It is also necessary to establish cerebral circulation - Pentoxifolline and Vinpocetine are used for these purposes.
In order to establish normal metabolism of nervous tissue, as well as restore communication between neurons, after complete recovery, a person is prescribed therapy with nootropics and neurometabolites: Piracet, Glycine, Pyriditol or hopantenic acid. On average, the course of treatment lasts about six months.

Viral meningitis: first signs, treatment, symptoms and diagnosis. Methods of disease transmission
Viral, or serous-lymphocytic meningitis is an infection that affects the soft membranes of the brain. This is one of the most common types of meningitis, most often caused by enterovirus infections.
Despite the fact that this form of the disease has a favorable prognosis for recovery, improper and untimely treatment can lead to irreversible changes in some parts of the brain, leading to permanent neurological disorders.
Therefore, at the first signs of viral meningitis, you should immediately consult a doctor.
Ways of spread of infection
The carrier of enteroviruses that can cause serous-lymphocytic meningitis is a person. In addition to patients with pronounced clinical forms, sources of infection spread can be patients with erased signs of the disease and healthy virus carriers. The entry point for infection is the gastrointestinal or respiratory tract.
Viral meningitis is transmitted both by airborne droplets (through direct interaction with a patient) and by contact household contact (through infected household items, dishes, toys, contaminated food and water).
The main risk group for morbidity includes children under 9 years of age, the elderly and people with weakened immune systems.
Course of the disease
Several days pass from the moment of initial infection with enterovirus until the full clinical picture of the disease manifests itself. Having penetrated the mucous membrane and formed a primary infectious focus, the pathogen enters the circulatory system and is introduced into all organs.
With strong immunity, inflammation does not develop, and the virus can remain latent in the body, turning the infected person into a virus carrier.
The incubation period of viral meningitis, which primarily affects the pia mater, lasts from 2 to 7 days. At this stage, the patient is an active spreader of infection. After this time, the first signs of the disease appear.
The disease is characterized by an acute onset with severe symptoms of intoxication. Body temperature suddenly rises (often exceeding the threshold of 40°), chills and severe headache appear, caused by an increase in intracranial pressure.
The fever can last for 4-5 days, then the temperature gradually decreases. In some cases, a relapse of the febrile state may occur with a repeated jump in temperature.
Main clinical signs of viral meningitis
With a favorable course of the disease and timely treatment, the main meningeal symptoms are absent or not pronounced. However, in severe cases, in the absence of adequate treatment and the presence of complications of the underlying disease, manifestations characteristic of all types of meningitis are added to the listed symptoms.
The following are considered characteristic symptoms of viral meningitis:
- persistent severe headache;
- repeated debilitating vomiting (without preliminary nausea);
- gastrointestinal disorders;
- hyperesthesia of the sensory organs (increased sensitivity to bright light, noise, discomfort from touching the skin);
- catarrh of the upper respiratory tract (rhinitis, pharyngitis);
- high blood pressure;
- in infants there is tension and bulging in the area of the large fontanel.
In addition to general indicators of well-being, there are a number of specific signs of inflammation of the meninges.
These include:
- hypertonicity of the occipital muscles (pain in the cervical spine when trying to turn the head or tilt it down);
- the presence of a “cocked hammer” position (the patient at rest lies on his side, throwing his head back and pressing his arms and knees to his chest);
- Brudzinsky's symptom complex: buccal (when the patient presses on the cheek, the patient reacts by involuntarily bending his arms at the elbows and twitching his shoulders), upper (when the patient's head is tilted to the chest, his knees involuntarily bend);
- Kernig criterion (in the supine position the patient bends the leg at the hip joint by 90°, if difficulties arise with extension, this indicates the presence of an inflammatory process in the meninges);
- Lesage syndrome, which is diagnosed in infants (the child is lifted up, held by the armpits; if he spontaneously pulls his legs towards his chest, this is one of the signs of meningitis).
Diagnostics
Despite the fact that the symptoms of viral meningitis are quite recognizable, you should not self-medicate in order to prevent the development of severe complications.
It must be remembered that only a qualified specialist can correctly determine the cause of the disease, confirming the primary diagnosis using instrumental research methods and prescribing complex therapy based on it.
This is especially true for young patients, since viral meningitis in children can occur atypically, with vague symptoms and, most importantly, rapidly.
To clarify the diagnosis and begin treatment measures, it is necessary to conduct laboratory tests. If meningitis is suspected, be sure to:
- general urine and blood tests;
- blood test for biochemistry;
- study of cerebrospinal fluid;
- additional instrumental studies as necessary (MRI, EEG, etc.).
Preventive actions
Since viral meningitis in most cases is a consequence of the introduction of pathogenic microorganisms of the intestinal group into the human body, the following is recommended to prevent the disease:
- observe the rules of personal hygiene;
- carry out sanitary treatment of water and food products (especially carefully in the summer);
- refrain from swimming in public bodies of water with standing water;
- avoid crowded places during periods of seasonal peaks in the incidence of viral and infectious diseases;
- carry out preventive vaccination of children in accordance with the vaccination calendar.
Viral meningitis is considered less dangerous than bacterial meningitis. The main risk group includes young children, in whom inflammation of the meninges can cause serious impairment of motor activity and cognitive disorders.
If all recommendations of the attending physician are followed, the prognosis for complete recovery of patients is quite favorable: 90% of adults avoid negative consequences and complications from the disease.
Causes
More than 60% of cases of serous meningitis are caused by enteroviruses, which are the main causative agents of viral meningitis. Infectious agents that cause inflammation of the meninges include:
- enteroviruses (70-80% of cases);
- arboviruses;
- Coxsackie viruses type A and B;
- parotitis;
- togaviruses;
- HSV type 2;
- cytomegalovirus;
- adenoviruses
The incidence of viral meningitis increases sharply in the summer. Rotavirus meningitis develops extremely rarely.
Complications and consequences
If the child receives medical care in a timely manner , the risk of developing serious complications is low.
However, if you delay visiting a doctor and starting treatment, enteroviral meningitis can leave very unpleasant and dangerous memories, such as:
- recurrent headaches;
- sleep disturbance;
- nervous activity disorder;
- intellectual inhibition.
The most serious consequences of the disease include:
- significant or complete loss of hearing and vision;
- irreversible changes in the structure of the brain;
- mental retardation;
- speech dysfunction;
- limitation of motor activity (paralysis, loss of sensitivity);
- tendency to develop epilepsy.
Prevention
To avoid getting viral meningitis, you should not swallow water while swimming in open water.
You should observe the rules of personal hygiene and thoroughly wash vegetables and fruits before eating. To prevent influenza, vaccination is carried out. If you have signs of viral meningitis, call the Yusupov Hospital. Doctors examine patients using equipment from leading European and American companies. To treat patients, neurologists use effective antiviral drugs that have a minimal range of side effects.
Make an appointment
Author
Polina Yurievna Vakhromeeva
Neurologist