The interest of neurologists, psychiatrists, therapists and endocrinologists in vegetative paroxysms is explained by the fact that this variant of vegetative pathology occurs quite often, is characterized by a variety of clinical manifestations, can simulate diseases of internal organs and is often accompanied by neurotic symptoms.
Particular attention is drawn to the question of the relationship of some vegetative seizures to “autonomic diencephalic epilepsy,” identified by Penfield in 1929, and which is now more accurately called “hypothalamic” or “hypothalamic-mesencephalic” epilepsy.
Classification
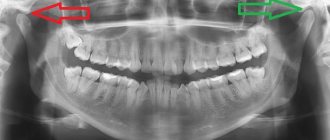
Autonomic paroxysms are divided into epileptic and non-epileptic. The former may accompany temporal lobe epilepsy or be an expression of hypothalamic epilepsy. The second, non-epileptic crises are observed in functional disorders of the nervous system (neuroses), autonomic dystonia, caused by increased reactivity of autonomic structures at various levels (cortical, hypothalamic, brainstem, sympathetic nodes of the border trunk, solar plexus). According to their symptomatology, vegetative paroxysms are divided into sympathetic-adrenal, vago-insular and mixed.
The laboratory for the study of nervous and humoral reactions has proposed the following classification of autonomic paroxysms.
Autonomic paroxysms against the background of a functional disorder of the nervous system of non-epileptic nature.
Autonomic paroxysms against the background of focal damage to the central nervous system of both epileptic and non-epileptic nature.
Autonomic paroxysms in the suffering of peripheral vegetative formations (sympathetic border trunk, solar plexus) of a non-epileptic nature.
In the second group, depending on the primary level of damage, the following subgroups are distinguished: a) autonomic paroxysms with predominant suffering of rhinencephalic structures of an epileptic nature; b) autonomic paroxysms with predominant damage to the hypothalamic structures of both epileptic (hypothalamic epilepsy) and non-epileptic nature; c) autonomic paroxysms with predominant suffering in the caudal parts of the brain stem.
In most cases, autonomic crises arise in connection with dysfunction or organic pathology of the hypothalamus and are non-epileptic in nature (in at least 75% of cases), which is why this chapter will focus mainly on them.
Definition of paroxysms
Vegetative-vascular paroxysms are a collective concept that includes all the sudden changes in the functioning of the ANS. They manifest themselves as a complex of symptoms.
The main features of such attacks:
- Suddenness. Pathology occurs without warning and quickly increases after the influence of a provoking factor.
- Emotional dependence. Most paroxysms progress after strong experiences (both positive and negative).
- Functional character. Seizures are manifestations of a disorder in the functioning of the ANS and its structures. When their functions are normalized, the problem goes away.
A synonym for vegetative-vascular paroxysm is crisis. There are several options for the development of the clinical picture against the background of different manifestations of specific pathological reactions. In each case, the characteristics of the symptoms are noted, on the basis of which they are differentiated.
- Paroxysms are characteristic mainly of young patients. In older people, they occur much less frequently due to sclerotic changes in the body and a decrease in the overall ability to quickly mobilize. The vessels lose their elasticity and cannot expand or contract quickly enough to cause a crisis.
- Women get sick more often than men. This is noticeable during menstruation and pregnancy - a hormonal imbalance occurs, which further aggravates the malfunction of the ANS.
What it is?
An attack of vegetative-vascular dystonia, or vegetative-vascular crisis, is an acute course of the syndrome in which a psycho-vegetative disorder develops, which arose due to a disruption in the functioning of the entire reticular complex. Leads to a decrease in activity and performance, slowing down the speed of thinking. Another name for a vegetative crisis is a panic attack. The crisis is diagnosed in people after 20, however, the factors of its manifestation can be recorded in early childhood. Women are more susceptible to attacks due to their emotional nature.
In most cases, the crisis is asymptomatic, but the sensations of the first attack are remembered by the person for a long time. The situation is aggravated by a panic attack, with the duration of the attack reaching several hours. Those affected by a crisis remember the sensations for the rest of their lives and are afraid of repetition. Cases of daily vegetative-vascular crisis were recorded.
The causes of vascular crisis are divided into primary and secondary. The root causes are usually considered to be located at the gene level associated with pathologies of the nervous system. Secondary causes include:
- prolonged stress;
- physical stress;
- excessive mental stress;
- depletion of the heart muscle and vessel walls, which leads to organ dysfunction;
- hormonal disbalance;
- shattered psyche;
- heredity;
- problems with the functioning of internal organs;
- head injury;
- allergy;
- passive lifestyle.
Swelling of the limbs, rapid heartbeat and panic attacks are characteristic symptoms of VSD.
VSD is characterized by variable signs of manifestation, they depend on the severity of the disease, appear periodically or constantly (daily). Factors have their own frequency, which depends on the type and nature of the problem. Often, VSD phenomena are associated with signs of other diseases. It is usually difficult for a specialist to make a correct diagnosis. Symptoms of a vegetative crisis:
- panic attacks;
- then increasing and then subsiding headache pain;
- cardiopalmus;
- numbness of the limbs;
- increased sweating;
- labored breathing;
- lethargic state;
- disturbed sleep patterns;
- anxious state.
Often, a vegetative-vascular crisis is marked by pain in the heart area, radiating to the upper left part of the body (arm, shoulder blade, forearm). Signs appear and disappear during the day, this is characterized by individual differences in the body. Signals of vegetative-vascular dystonia are more pronounced during extreme heat. However, the course of the disease can pass without the presence of symptoms, which makes it difficult to provide timely assistance to a person.
Mechanism of occurrence
Functional abnormalities in the functioning of the hypothalamus and peripheral parts are secondary in nature and disappear after the provoking factor is eliminated.
Sometimes the cause of crises is organic damage to the structures of the ANS (tumor, infection, injury), which aggravates the course of the disease. In this case, the diagnosis of VSD is not made, since crises are caused not by an imbalance, but by organic pathology, and are no longer the main condition, but a secondary manifestation.
Depending on which department of the ANS (sympathetic or parasympathetic) predominates, the functioning of specific organs is enhanced or weakened. Traditionally, the following are affected by paroxysms:
- heart;
- vessels;
- nervous system;
- endocrine glands.
During a sharp activation of the ANS, a sudden manifestation of the main manifestations of the disease occurs. For some, this will result in a hypertensive crisis, while others fall into depression.
What is vegetative-vascular dystonia (VSD)?

Vegetative-vascular dystonia ( VSD
) is a disease of the autonomic nervous system. The autonomic nervous system (ANS) regulates the functioning of blood vessels and internal organs. It is divided into the sympathetic and parasympathetic systems. The action of the ANS systems is opposite: for example, the sympathetic system speeds up heart contractions, and the parasympathetic system slows it down.
And these functions are very diverse and vitally important. This:
- Maintain normal body temperature and blood pressure
- Processes of cardiovascular activity
- Digestion and urination
- Activities of the endocrine and immune systems
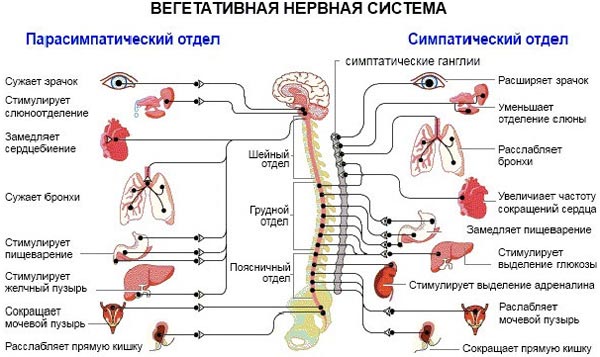
With VSD, the balance between the parasympathetic and sympathetic systems is disrupted, which causes symptoms that worsen overall health. Symptoms of VSD do not pose a threat to human life, but sometimes they can signal the presence of serious problems in the vascular, nervous, cardiac or other vital systems.
The pathology is usually detected in childhood or young age, the peak of symptoms occurs at the age of 20-40 - the most productive and active period, while the usual rhythm of life is disrupted, professional activity becomes difficult, and family relationships suffer.
In modern medicine, vegetative vascular dystonia is not considered as an independent disease, since it is a set of symptoms that develop against the background of the course of some organic pathology. Vegetative-vascular dystonia is often referred to as autonomic dysfunction, angioneurosis, psycho-vegetative neurosis, vasomotor dystonia, autonomic dystonia syndrome, etc.
The main signs of VSD are:
- Pain in the heart (cardialgia);
- Arrhythmias;
- Respiratory disorders;
- Autonomic disorders;
- Fluctuations in vascular tone;
- Neurosis-like conditions.
Thus, vegetative-vascular dystonia is not an independent disease, but a complex syndrome that is part of the total clinical picture of various psycho-emotional, somatic, neurological or mental diseases.
The pathology can appear in early childhood or adolescence, but, as a rule, it does not cause much concern. According to statistics, the peak occurs in the age period from 20 to 40 years. It has been proven that the female population is more susceptible to the disease than the male population.
It is diagnosed in 60–70 percent of cases in adults and in 10–15 percent in children and adolescents.
The causes of vegetative-vascular dystonia are very different and, sometimes, lie in early childhood or even the period of intrauterine development. Among them, the most important are:
- Intrauterine hypoxia, abnormal birth, childhood infections;
- Stress, neuroses, severe physical overload;
- Traumatic brain injuries and neuroinfections;
- Hormonal changes during pregnancy and adolescence;
- Heredity and constitutional features;
- The presence of chronic pathology of internal organs.
Behavioral factors and lifestyle can contribute to vegetative dystonia:
- Excessive addiction to alcohol and coffee
- Great mental or physical stress
- The type of temperament and character traits also plays a role: The most balanced sanguine people by type are least susceptible to VSD
- On the contrary, choleric and melancholic people are at risk
Mentally balanced, cheerful people suffer from autonomic disorders much less often than anxious, irritable and suspicious people
People suffering from VSD are sensitive to life changes. For them, the test becomes a change in climate, moving a long distance, to a different time zone - unpleasant symptoms begin to appear.
Types of paroxysms

Depending on the symptoms, they are divided into the following types:
- sympathoadrenal;
- vagoinsular;
- mixed.
The first group includes sudden deterioration of the condition, which is caused by activation of the sympathetic division of the autonomic nervous system.
- People with such paroxysm are anxious, irritable, and sometimes even aggressive.
- Their blood pressure rises, headaches appear, their skin turns pale, and their pupils dilate.
Sedatives have worked well in treatment.
Vagoinsular vegetative-vascular crisis progresses against the background of hyperactivation of the parasympathetic part of the nervous system. Because of this, inhibition of most internal reactions is observed:
- the person is gloomy;
- his blood pressure drops;
- there is sweating, the urge to have a bowel movement, nausea and vomiting;
- pupils constrict;
- heartbeat becomes rare.
The mixed type combines the features of the two options above. It indicates a pronounced imbalance in the functioning of the ANS with constant activation of one or another of its departments.
They are classified according to severity as follows:
- Lungs. They last 10–20 minutes and go away on their own without the use of medications.
- Average. Lasts up to one hour. They manifest themselves as severe symptoms with a noticeable decrease in performance.
- Heavy. The patient is disturbed for more than 60 minutes. Accompanied by pronounced signs of autonomic dysfunction with a strong deterioration in well-being. Elimination requires the use of specialized medications.
First aid
Regardless of how the attack of vagoinsular crisis goes, first of all, be sure to call an ambulance or a doctor to prevent possible further deterioration of the situation.
The patient must be placed compactly, preferably lying on a flat, soft surface, while all collars and buttons that may complicate or disrupt the breathing rhythm must be unbuttoned.
If possible, provide the patient with maximum access to fresh air, apply cold to the body, try to calm down if the person has a sudden panic or a nervous breakdown from previous symptoms.
It is advisable to give drops or tablets of clonidine, validol, valerian or valocordin.
If a person is unconscious, monitor the urge to vomit and help him get rid of them in time by throwing his head to the side. Before doctors arrive, be sure to monitor your pulse and skin color.
Nocturnal paroxysms
Nocturnal paroxysmal dystonia is a separate type of vegetative attacks that does not fit into the traditional classification. Unlike other forms of pathology, the causes of its origin are still unknown.
The problem manifests itself as episodes of chaotic motor activity involving the limbs and the whole body after waking up.
Clinically, nocturnal paroxysm of dystonia resembles an epileptic seizure, but with normal electroencephalography (EEG) readings. It is believed that the reason for the appearance of such movements is the loss of inhibitory mechanisms in the brain stem.
Normally, they interfere with human muscle activity during sleep. The pathology is manifested by characteristic seizures. The average episode length is 10–60 minutes. Treatment has not yet been developed.
Nutrition and diet
Proper nutrition for vegetative-vascular dystonia in children and adults requires the exclusion of certain dishes and products from the diet. Basically, this is food containing a large amount of bad cholesterol, which increases excitability and negatively affects the tone and structure of blood vessels.
There are no hard and fast rules. VSD has a psycho-emotional etiology, so it is extremely important that the patient does not experience unnecessary stress. The diet should leave a feeling of lightness, and not constant restrictions, which in itself can lead to depression even for a healthy person.
Proper nutrition for vegetative-vascular dystonia is based on the principles:
- the diet contains many foods containing magnesium and potassium;
- Products that stabilize blood pressure are required;
- Liquid intake will help normalize the water-salt balance.
The basic rules when creating a menu and diet for people with vegetative-vascular dystonia are the following:
- Food should be beneficial to the body.
- Food should be healthy.
- It is necessary that with food intake, all the necessary beneficial elements for its functioning enter the body.
The diet for vegetative-vascular dystonia of the hypertensive type includes foods and dishes with a reduced salt content. Allowed:
- vegetable soups with cereals and soups not based on strong meat/fish broth with a minimum amount of extractive substances without adding spices and seasonings.
- It is preferable to consume whole grain bread or with bran; in small quantities, rye or wheat bread.
- Meat and poultry should be of low-fat varieties and are best consumed boiled and baked.
In the hypotonic form of VSD, vegetables and fruits should contain vitamin C and beta-carotene, it is recommended to rely on:
- citrus fruits, bananas, pineapples. You can eat potatoes, semolina, and white flour bread.
- To increase blood pressure you need to eat nuts, buckwheat, brains, liver, pomegranate.
- Herring and cheeses can be introduced into the diet a couple of times a week, this will increase blood pressure.
- Sweets, chocolate, coffee and cocoa have a good effect.
With cardiac form of VSD
Products with magnesium and potassium are recommended. Introduce into the diet:
- oatmeal and buckwheat, beans and onions, peas and eggplants, grapes, peaches, apricots, raisins and dried apricots.
- From drinks, choose juices, compotes and jelly.
- Fermented milk products, chicken egg dishes, lean fish and meat are of great benefit.
Symptoms

The clinical picture of paroxysms caused by dysfunction of the ANS varies depending on the predominance of its specific part.
Typical symptoms of sympathoadrenal crisis:
- Marked emotional lability. People are mostly anxious, overly irritable, and sometimes aggressive.
- Acceleration of heart rate. The patient feels a beating in the chest, which is constantly intensifying.
- Increase in blood pressure. Constriction of peripheral vessels in combination with increased myocardial contractions lead to increased readings on the tonometer.
- Pain in the heart area. Stitching, pressing, burning sensations are noted.
- Headache. Mostly sudden, but short-lived. It has a pulsating and pressing character. Localized in the frontal, temporal, occipital regions of the skull.
Patients with sympathoadrenal paroxysm suddenly turn purple, and convulsions may even occur. They tend to express emotions too strongly (screaming, crying).
The vagoinsular variant is characterized by a predominance in the regulation of the peripheral organs of the parasympathetic division of the ANS. Classic symptoms of such paroxysm:
- Deterioration of mood. The person is apathetic, whiny, and does not want to communicate with other people.
- Bradycardia. Functional arrhythmias progress.
- Breathing problems. Shortness of breath, lack of air, and compression of the lungs appear. Some people note the presence of a non-existent obstruction in the bronchi that prevents them from breathing normally.
- Blood pressure drop. In severe forms of paroxysm, a person may even faint. The main danger remains the risk of injury from a fall or progression of symptoms while performing work or driving.
- Discomfort throughout the body. A person is often unable to determine where it hurts. The unpleasant sensation is aching in nature, occurs frequently, and is mildly expressed.
The mixed form of paroxysm is manifested by a combination of the above symptoms with varying degrees of severity.
Complications
The course of vegetative-vascular dystonia can be complicated by autonomic crises, which occur in more than half of patients. Depending on the predominance of disorders in one or another part of the autonomic system, sympathoadrenal, vagoinsular and mixed crises are distinguished.
If we talk about neurological and cardiac disorders that can provoke the disease, they manifest themselves in the following:
- decreased efficiency of the heart muscle, interruptions in its activity;
- development of hypertension or hypotension - high and low blood pressure;
- disturbances in the functioning of the urinary system, increased urge to go to the toilet;
- changes in the autonomic regulation of the eyes, which leads to deterioration of vision;
- failure in the metabolic process, loss of body weight;
- development of weather dependence - an acute reaction of the body to changes in weather conditions;
- improper functioning of the vascular system, leading to poor nutrition of brain tissue;
- gastrointestinal dysfunction - constipation, diarrhea, bloating, etc.
The consequences of VSD are essentially its aggravated symptoms, which occur already in the early stages of the development of the syndrome, but do not cause much concern to patients.
Features of the flow
Treatment of vegetative paroxysms is complex. It is carried out using both specialized drugs (mainly affecting the functioning of the ANS) and non-drug methods:
- acupuncture;
- aromatherapy;
- physiotherapy;
- meditation.
By fixing the factor that provokes the appearance of the next paroxysm, with its further elimination, it is possible to normalize the person’s condition.
It is possible to completely eliminate the occurrence of attacks by normalizing the balance between the branches of the autonomic system and increasing the threshold of excitability of the nervous system.
Treatment of VSD in adults

Treatment of VSD
is carried out comprehensively and includes the following points:
- Normalization of daily routine, sleep, rest;
- Elimination of physical inactivity using dosed physical activity (PT);
- Therapeutic massage and water procedures;
- Balneotherapy (treatment with mineral waters);
- Phototherapy;
- Limiting sources of emotional experiences - computer games, TV shows;
- Counseling and family psychological correction;
- Normalization of nutrition (regular consumption of food enriched with vitamins);
- Electrophoresis;
- Drug therapy.
The most difficult stage in therapeutic intervention is eliminating the causes that led to the autonomic disorder. Reviews from patients with vegetative-vascular dystonia indicate that a person is often independently able to determine the factors contributing to the manifestation of the syndrome. They indicate stress, overwork, quarrels and conflicts in the family, leading to an attack of VSD.
Drugs for vegetative-vascular dystonia
If non-drug methods are ineffective, pharmaceutical drugs are prescribed. These drugs are selected individually for each patient, starting with minimal doses and gradually increasing to the desired concentration. Particular attention is paid to getting rid of chronic foci of infection in the body, treating endocrine and other pathologies.
Drug treatment is determined by the predominant symptoms in a particular patient. The main group of drugs for VSD consists of drugs with a sedative effect:
- Herbal remedies – valerian, motherwort, novo-passit, etc.;
- Antidepressants – cipralex, paroxetine, amitriptyline;
- Tranquilizers - seduxen, elenium, tazepam, grandaxin.
Depending on the disturbing complaints, the doctor may prescribe tablets for vegetative-vascular dystonia of the following drug groups:
- potassium and magnesium preparations (Magne B-6, Panangin, Asparkam) - to improve vascular tone and the relationship between nerve cells;
- beta-blockers (Metaprolol, Anaprilin) – for persistent arterial hypertension;
- nootropics (Piracetam) - to normalize metabolic processes and improve blood circulation;
- antidepressants (Amitriptyline, Cipralex) – for severe symptoms of depression to regulate the functioning of the central nervous system;
- tranquilizers (Diazepam) - to provide a sedative effect in cases of anxiety and panic attacks.
Physiotherapy for VSD
Physiotherapy in the treatment of vegetative-vascular dystonia is aimed at regulating vascular tone, normalizing metabolism and eliminating pain. The nature, systematicity and intensity of the procedures are selected by the doctor in accordance with the characteristics of the disease.
The effects that physiotherapy produces on a patient with vegetoneurosis are:
- calming – electrosleep, electrophoresis of sedative drugs, aeroionotherapy;
- tonic – magnetic and laser therapy, inductothermy;
- vasodilator - galvanization, local darsonvalization;
- vasoconstrictor - electrophoresis of adrenaline and other adrenomimetic drugs (drugs that stimulate adrenergic receptors);
- antiarrhythmic - electrophoresis of potassium chloride, lidocaine.
Therapeutic massage and water treatments
Physical effects on the body, in particular therapeutic massage and water procedures, improve blood circulation, improve the functioning of the lymphatic system, if necessary, restore the structure of the spine (in the case of osteochondrosis), and along with the spine, the nerve channels with the vessels that pass through it are aligned. In addition, massage allows you to relax, relieve stress, and improve muscle tone.
Physical exercise
Most experts in the field of prevention and treatment of vegetative-vascular dystonia agree that physical rehabilitation should be put in first place.
It is various physical exercises that can significantly help in the fight against the disease. But what is important here is the correct balance between the complexity of the physical exercise and the abilities of a particular patient. This is the only way to achieve the best results.
What should you avoid?
Some actions of the patient can aggravate the condition of VSD. Thus, if there are already existing disorders in the functioning of the autonomic nervous system, you should not:
- excessively involved in meditation;
- create additional stress for the body or exhaust yourself with increased physical activity;
- go on diets for a long time or even starve;
- be an inveterate pessimist;
- drink alcoholic beverages, smoke;
- listen to recommendations from people who do not have the appropriate medical education (especially in matters of drug treatment of the disease).
Prevention of pathological condition
To prevent the vagoinsular crisis from recurring, preventive measures should be followed. These include:
- Healthy lifestyle.
- Breathing exercises.
- Proper nutrition.
- Alternating loads with rest.
- Use of herbal sedatives. Among them are infusions of valerian, motherwort, and ginseng.
In some cases, psychotherapeutic treatment and antidepressants are required to get rid of feelings of fear and anxiety.
Source: FB.ru
Panic attacks
The prevalence of PA in the general population (aged 15 to 54 years), according to American and European studies, is similar and amounts to 2–5%. The proportion of patients with PA among those seeking primary care is about 10%. Panic attacks develop in women twice as often as in men. There are two age peaks: 15–19 years and 35–50 years.
About half of patients presenting to primary care with medically unexplained symptoms meet diagnostic criteria for panic disorder. Patients with panic disorder are often dissatisfied that tests and examinations do not reveal any diseases, and seek medical help repeatedly for symptoms that bother them.
Panic disorder often co-occurs with other mental illnesses and increases the risk of suicide. Thus, depression is diagnosed in approximately a third of patients suffering from panic disorder. Patients with panic and anxiety disorders often abuse alcohol, which alleviates symptoms of anxiety and reduces treatment.
The development of panic disorder is associated with the effect of psychotraumatic factors on predisposed patients.
Background mental and somatic diseases (endocrine system diseases, CVD), organic brain lesions, and, to a lesser extent, temperament and genetic characteristics are considered as predisposing factors.
Psychotraumatic factors:
- situations with potential danger, threats;
- uncontrollable or unwanted events that cause a significant decrease in self-esteem;
- Road accident, injury, rape, attempted murder;
- serious illness, death of loved ones and relatives.
PA in people suffering from panic disorder can be provoked by drugs or foods that have a stimulating effect (caffeine, yohimbine, products containing glutamate), as well as withdrawal of substances with a sedative effect (alcohol, barbiturates, benzodiazepines).
Folk remedies

There are many folk remedies for vegetative-vascular dystonia; below we have collected several effective recipes for different types of VSD.
Hypertensive type (high blood pressure):
- Hawthorn helps best. Here you can use the following recipe: keep a teaspoon of the product in a water bath (250 ml of water) for 4 hours; This infusion can be drunk 25 grams three times a day.
- Mix lemon balm, lingonberry leaves, and hawthorn flowers in equal proportions. Measure out 8 g of the mixture, pour in 0.3 liters of boiling water and infuse. You need to take the decoction 50 ml 5 times a day;
Hypotonic type (when blood pressure is low):
- take 1 part each of zamanika roots, rose hips and hawthorn berries, 2 portions each of chamomile and St. John's wort. Take 10 g of raw materials, pour a glass of cold water and leave for 4 hours, then heat in a water bath for 15 minutes, leave for an hour, filter. The volume is drunk in 3 doses during the day;
For surges in blood pressure, you can use a special infusion:
- it includes ingredients such as hawthorn flowers (20 grams), lily of the valley flowers (10 g), valerian root (20 g), hop cones (10 g), peppermint leaves (15 g), fennel fruits (15 g);
- one tablespoon of this mixture (well crushed) is poured into a glass of boiling water;
- To infuse, you need to put the solution in a cool place for three hours, then bring to a boil and let cool.
For VSD, for a general tonic effect on the body, use an infusion using echinacea, hops and rhodiola (golden root). To make this product you will need:
- Echinacea inflorescences;
- Rhodiola rosea root;
- Hop cones.
Mix in a ratio of 2:2:1 and add hot water at the rate of one glass of water per tablespoon. collection When the infusion has cooled, you need to add one tbsp. l. honey The infused herbal remedy is drunk during the day in three doses. Use this remedy every day for a month. It is advisable to carry out such treatment once a year.
The prognosis of vegetative-vascular dystonia is favorable; often its manifestations remain forever in childhood. However, without prevention and treatment, vegetative-vascular dystonia can lead to a persistent increase in blood pressure, which changes the structure and functions of various internal organs; to disturbances in digestive processes, etc.
In case of VSD, it is necessary to conduct regular (usually seasonal) courses to prevent exacerbations, for which the following are prescribed:
- herbal medicine,
- vitamin therapy,
- massage,
- physical therapy,
- physiotherapeutic procedures,
- Spa treatment.
We explained in simple words what kind of disease this is and why it is important to start treating vegetative vascular dystonia on time. Take care of your health and at the first signs and symptoms of VSD, consult a doctor.
Stopping attacks
To relieve vegetative paroxysms of any nature, benzodiazepine tranquilizers are best suited: Clonazepam, Alprazolam.

With long-term use of benzodiazepines, addiction occurs, and cessation leads to “withdrawal syndrome.” In addition, the use of these drugs is limited by the irreversible decline in intelligence in the elderly, and the fact that people taking drugs of this group for a long time are more likely to fall (cannot stand on their feet).
There are non-benzodiazepine tranquilizers-anxiolytics - H1-histamine receptor blockers (Hydroxyzine, Valocordin-Doxylamine), GABAergic drugs (Grandaxin, Stresam). However, insufficient knowledge does not allow them to be widely recommended.
For mild attacks of anxiety with palpitations, Anaprilin has a sufficient anxiolytic effect. The drug should not be used for bradycardia, AV block, low blood pressure, as well as in patients with bronchial asthma and diabetes, peripheral vascular diseases, pheochromocytoma.
Traditionally used to relieve autonomic paroxysms, neuroleptics (Teraligen, Thioridazine, Chlorprothixene), ergot and belladonna alkaloids (Bellataminal, Nicergoline) have a wide range of side effects (dry mouth, drowsiness). International guidelines do not recommend the use of these drugs for the relief of anxiety.
It is advisable to use neuroleptics for autonomic disorders in patients receiving intensive care. In this case, their sedative effect does not matter.
There are two approaches with similar effectiveness:
- pharmacotherapy: course treatment with antidepressants (selective serotonin reuptake inhibitors (Zoloft, Paroxetine, Citalopram), selective serotonin and norepinephrine reuptake inhibitors (Venlafaxine), tricyclic antidepressants (Amitriptyline, Clomipramine); the use of monoamine oxidase inhibitors has been less studied.
- cognitive behavioral psychotherapy (the patient is explained the nature of the disease and panic attacks; taught techniques to increase self-esteem, breathing techniques that increase the level of carbon dioxide in the blood, muscle relaxation techniques; taught to soberly assess what is happening during an attack and placed in situations that cause fear; informed about recurrent nature of the disease).
Both methods have advantages and disadvantages. They do not contradict each other and can be used simultaneously.
DO YOU KNOW THAT…
Panic “attacks” creative people
The great Russian writer Leo Tolstoy. Hollywood beauty is actress Kim Basinger. The main character of the movie "Spider-Man" is Tobey Maguire. The idol of young girls is the main “Twilight vampire” Robert Pattinson. Star of the films “The Lord of the Rings”, “Pirates of the Caribbean” Orlando Bloom. Oscar winner Adrien Brody.
The dazzling blonde Basinger, as a teenager, could not leave the house for months - she was periodically overcome by an inexplicable fear, “forbidding” appearing in public.
The star of the film “The Pianist” Adrien Brody publicly declared to the public during his Oscar presentation: “Oh, how tired I am of panic attacks!”
Leo Tolstoy, during a trip to the city of Arzamas, unexpectedly experienced such an acute attack of inexplicable fear that he even described it in his “Notes of a Madman.” By the way, it was the “Arzamas horror” that forbade the writer from even thinking about ever returning to this city again.
American scientists have hypothesized that the same gene that “programs” a person for depression is responsible for the tendency to panic attacks. By the way, it is found in 2 million Americans. However, doctors do not encourage people to come to terms with the fact that a person is a carrier of the ill-fated gene. On the contrary, they insist that you can get out of such a psychological tailspin by taking vitamins, playing sports or devoting time to your favorite hobby.
But colleagues of American researchers - scientists from Taiwan - have established a direct relationship between panic attacks and snoring. After observing 8,700 patients diagnosed with obstructive sleep apnea for 10 years and almost 35,000 clinic patients who did not suffer from these sleep disorders, researchers proved that the disruption of brain neurons caused by apnea also contributes to the appearance of panic attacks.
In the group of those suffering from obstructive apnea, the risk of developing panic disorder was noted to be 2.17 times higher than in the “control” group.
To avoid this problem in the future, experts recommend the following for prevention:
- at the first symptoms, consult a neurologist;
- avoid stressful situations.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.