IVH has recently become a significant problem in pediatric neurosurgery. This is explained by the improvement in the quality of nursing for premature babies with low birth weight. According to the literature, among children weighing less than 2500 g, IVH occurs in 60% of cases. Neurosurgical assistance is required for children with severe IVH, leading to the development of progressive hydrocephalus. The severity of intraventricular hemorrhages directly depends on the degree of prematurity. The year 2012 was marked by the adoption of WHO live birth standards. Currently, babies weighing 500 grams are considered live births. Nursing children with extremely low body weight is significantly complicated by the high incidence of severe IVH among them. This is a category of patients for whom the timeliness and skill of providing assistance to them largely determines the degree of further disability. Providing assistance to this category of patients begins at the stage of the maternity hospital. The visiting team assesses the condition of the newborn patient and assesses his transportability.
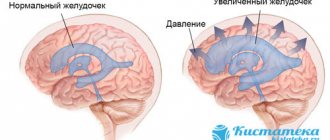
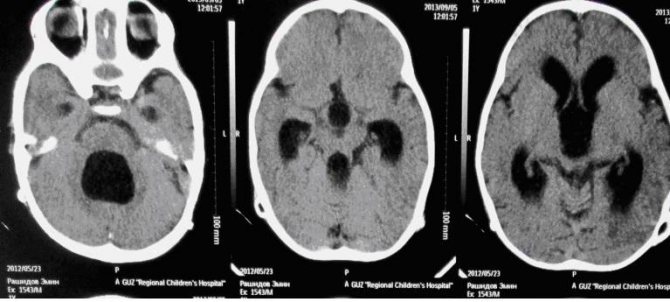
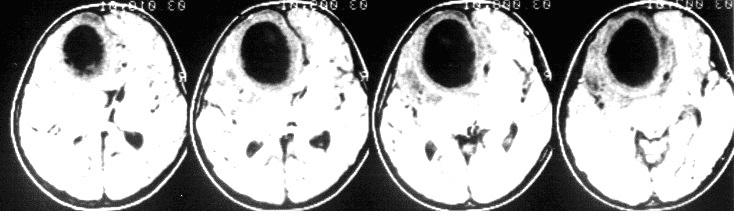
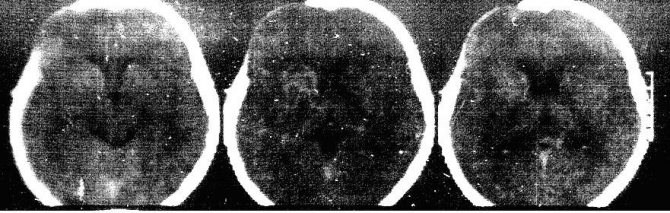
The enlarged lateral ventricles of the brain are clearly visible. The severity of the condition is largely explained by severe intracranial hypertension.
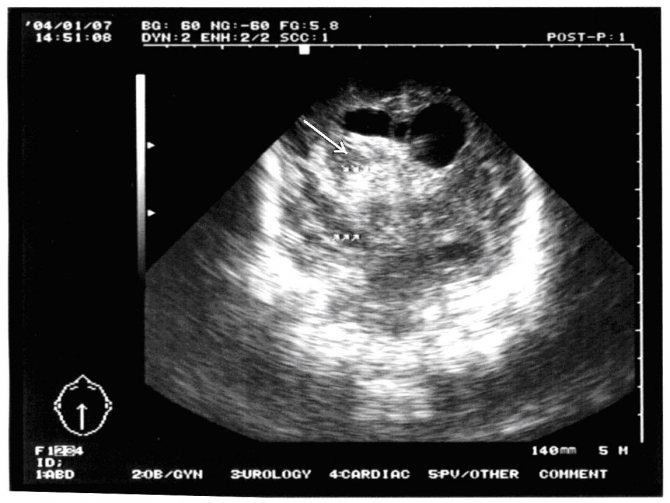
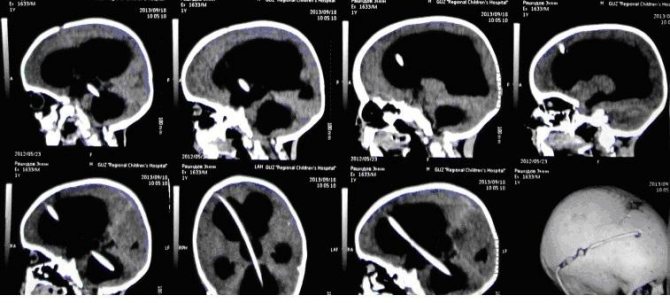
In such cases, we begin treatment with a series of lumbar punctures. Contraindications to lumbar puncture may be the presence of occlusion or a bulging blood clot in the lumen of the ventricles. Sometimes it is possible to compensate for the process with a series of lumbar punctures. To reduce ICP we perform ventricular punctures. Multiple ventricular punctures are not advisable, since it has been proven that frequent ventricular punctures lead to the development of porencephalic cysts. Thus, for long-term unloading of the ventricular system, it is often necessary to resort to various drainage operations. For example, ventriculostomy followed by external drainage. This manipulation is performed under ultrasound control in order to visually control the placement of drainage into the lumen of the lateral ventricle. The image clearly shows the catheter in the lumen of the right lateral ventricle.
This image was taken intraoperatively:
This is necessary because drainage is sometimes left standing for a long time. Against the background of drainage, as a rule, hypertensive symptoms are relieved, hemodynamics are normalized, convulsive syndrome is stopped, and breathing is normalized.
The complexity of the situation is that, against the background of various drainage methods, it is extremely rare to achieve final normalization of liquor outflow. This condition is usually resolved by shunt surgery. But here, too, not everything is simple. It is sometimes possible to achieve cerebrospinal fluid sanitization sufficient to install a shunt only after 1-2 months. This turns this category of patients into a big problem for the department. External drainage requires constant attention and poses a serious risk of infection of the drainage system and the development of ventriculitis. For the last 6 years, we have practically not used external drainage in newborns.
Closed drainage techniques are used, such as the subgaleal reservoir and the installation of Omaya type reservoirs. We use these techniques as the first stage of treatment of hydrocephalus in premature infants with IVH, which allows us to delay shunt implantation until the cerebrospinal fluid is completely sanitized.
Shunt surgery
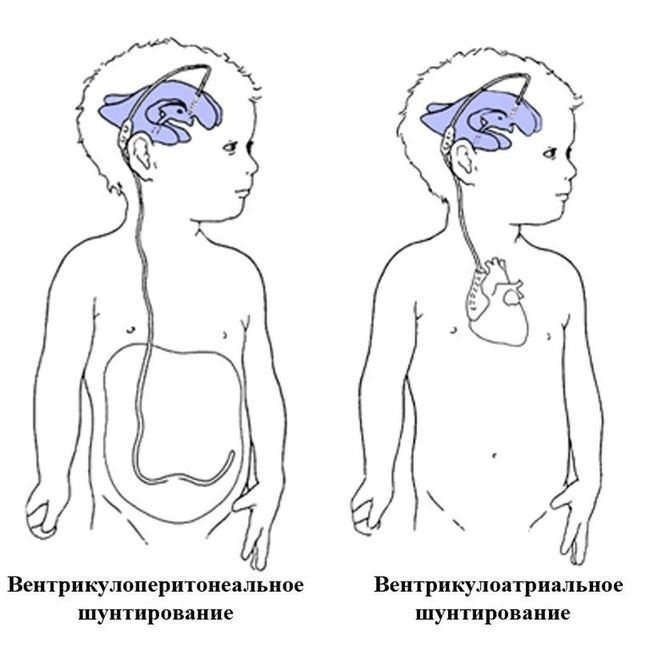
This is the most common treatment for hydrocephalus in infants. The shunt procedure uses two components—a shunt and a valve.
The shunt is a long tube, similar to a catheter, made of silicone (a material inert to the body). The open part of the tube is placed inside the ventricle, where excess fluid accumulates. The tube is then directed under the skin and into the tissue, placing its second end in the ventricle of the heart to reabsorb fluid.
The valve is also attached to the shunt at a point near the ventricle. The one-way valve controls the flow and pressure of fluid draining from the ventricles of the brain. It prevents backflow of cerebrospinal fluid into the ventricle - even when the patient changes position - and mitigates excess drainage of cerebrospinal fluid.
.
Causes and risk factors
Hydrocephalus is caused by an imbalance between the production and absorption of cerebrospinal fluid.
Cerebrospinal fluid is produced in the ventricles of the central nervous system and flows from them through channels into the space surrounding the brain and spinal cord, where it is absorbed into the blood vessels.
Excess cerebrospinal fluid in the ventricles occurs for one of the following reasons:
- Obstruction. The most common cause of hydrocephalus is partial blockage of the normal outflow of cerebrospinal fluid from the ventricles into the subarachnoid space.
- Poor absorption. The problem of insufficient absorption of cerebrospinal fluid into the blood vessels is less common. Its development is most often associated with inflammation of brain tissue.
- Excess production. Even more rarely, there is increased or accelerated production of cerebrospinal fluid, in which it does not have time to be absorbed by the blood vessels.
Causes of congenital hydrocele in a newborn:
- Malformations of the brain stem, in which there is a narrowing of the channels for the outflow of cerebrospinal fluid. It is the cause of approximately 10% of all cases of hydrocele in newborns.
- Dandy-Walker syndrome is a malformation of the cerebellum and cerebrospinal fluid ducts. In approximately 2-4% of infants with accumulation of water in the head, this is the reason.
- Arnold-Chiari malformation is a congenital malformation of the brain.
- Congenital toxoplasmosis is an infectious disease that develops when the fetus is infected with Toxoplasma before birth.
- Bickers-Adams syndrome is a genetic disorder responsible for 7% of cases of hydrops in newborn boys.
All causes of congenital hydrocephalus, which can cause water to accumulate in the head of a newborn child, are associated with the development of brain defects in the fetus.
Causes of acquired dropsy in infants and children:
- The presence of formations in the brain - these include tumors, cysts, abscesses, hematomas. Approximately 20% of cases of water accumulation in the head in infants and older children are caused by these reasons.
- Bleeding into the ventricles of the brain associated with prematurity, head injury, rupture of an aneurysm.
- Infectious diseases – meningitis, cysticercosis.
- Increased pressure in the cerebral venous system.
- Iatrogenic hypervitaminosis A - with this condition there is an increase in the production of cerebrospinal fluid and the permeability of the blood-brain barrier.
Endoscopic ventriculostomy with coagulation of the choroid plexus
The surgical operation of ventriculostomy is accompanied by the destruction of a segment of the choroid plexus, which is part of the cerebrospinal fluid-conducting system of the brain, which produces cerebrospinal fluid. An electrical impulse is used to suppress the functions of the choroid plexus, which prevents the production of excess cerebrospinal fluid.
Endoscopic ventriculostomy of the third ventricle with coagulation of the choroid plexus is the only method of treating hydrocephalus in premature infants and those suffering from it due to spina bifida.
Note that none of the above procedures excludes complications, which means they should be performed by professionals.
What is hydrocele?
Hydrocephalus is a disease in which there is an excessive accumulation of cerebrospinal fluid in the brain.
Normally, cerebrospinal fluid circulates inside and outside the brain and spinal cord, it is produced by the choroid plexuses and is absorbed back into the bloodstream.
Cerebrospinal fluid plays an important role:
- Acts as a brain shock absorber.
- Delivers nutrients to the brain and removes products of its metabolism.
- Compensates for changes in intracranial blood volume by moving between the skull and spine.
Normally, in a healthy person, there is a precise balance between the production and absorption of cerebrospinal fluid. Since it is produced continuously, diseases that block the flow or absorption of cerebrospinal fluid lead to its accumulation and the development of dropsy in the head.
Most often, hydrocephalus is observed in children, so it is parents who are interested in why a newborn child may have excess water in the head.
What are the complications and limitations of treatment?
Before choosing a treatment for hydrocephalus, you need to be aware of the complications associated with it.
Hydrocephalus may recur
Surgical procedures cannot stop the production of cerebrospinal fluid. Therefore, there is a risk of relapse.
However, surgical procedures are successful in reducing symptoms and allowing the child to live relatively comfortably with hydrocephalus for the rest of his life.
Surgical procedures have limitations
- The ventriculostomy procedure only works if the swelling is caused by a blockage in the ventricles. If it is due to other causes, a shunt procedure is the only treatment option.
- Bypass surgery requires complex interventions, such as quickly preparing the child and fasting for six hours before surgery. After surgery, the child should lie in bed and not move for 24 hours. The total hospital stay can last up to three days. All this can be difficult and painful for the baby.
Long-term follow-up is mandatory
Shunts must be periodically inspected and replaced. The operation of the valve should be monitored by a physician at prescribed intervals.
The average length of time a shunt remains in place can be five years, but the replacement interval may vary, depending on the severity of the condition and the doctor's recommendations.
High chances of complications
Shunt valves are susceptible to mechanical damage, malfunction, and clogging. Bacterial infections after surgery most often occur during the first three months.
There is a 30% chance of shunt failure in the first year after surgery. Even a minor infection or problem requires replacement of the entire shunt system.
In addition, ventriculostomy can cause bleeding inside the brain, leading to severe headaches.
Diagnostics
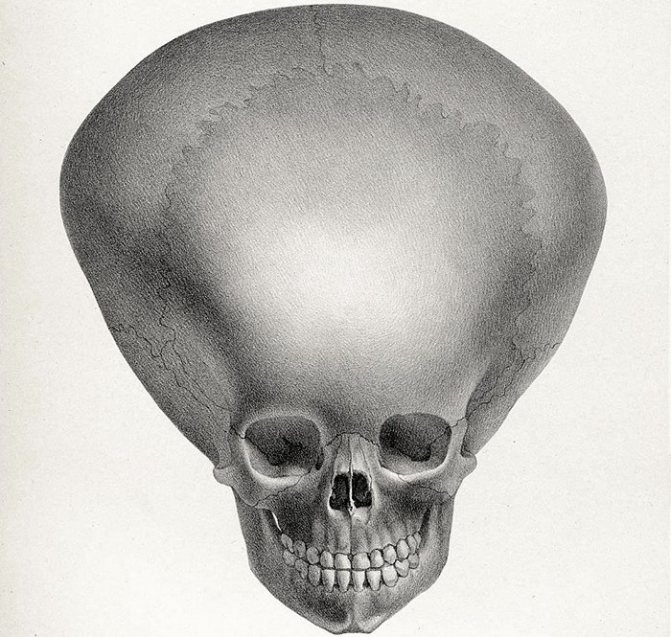
The diagnosis is made on the basis of external manifestations, when the symptoms are clearly expressed, and the causes are also determined. The dynamics of head growth is monitored for up to a year. Indirect signs of the disease are manifested by a monthly increase in head circumference over 3 cm, the appearance of disproportions, the presence of swelling of the fontanelles and suture dehiscence.
Sometimes the size of the head is increased due to heredity, but this is not a congenital anomaly, therefore, if dropsy is suspected, the following is additionally carried out:
- Examination of the fundus by an ophthalmologist;
- Two-plane radiography of the skull;
- Ultrasound of the head (neurosonography) through the fontanelle with measurements of all parameters - performed on a baby up to one year old in cases where it is not overgrown; at an older age, the procedure is technically impossible;
- Carrying out CT and MRI of the head - to identify structural anomalies, the degree of deformation and view the quality of brain structures;
The compensated degree does not appear externally. Additionally, blood tests are required to detect infections, and a puncture of the cerebrospinal fluid is taken to determine its composition. If seizures are present, an EEG is performed.
Signs of infection after surgery
It is very important to be vigilant for any signs of infection after surgery.
If your child develops an infection after surgery, they will have the following symptoms:
- A protrusion or depression on the head where the shunt enters the cranial cavity;
- Swelling or redness in the part of the body where the shunt tube passes;
- Vomit;
- Poor appetite;
- Irritability and frequent crying;
- Drowsiness and lethargy;
- Abdominal pain.
The child will give a repetition of all the symptoms of hydrocephalus. If parents suspect an infection, they should consult a doctor without any hesitation.
When the child is at home after surgery, it is necessary to carefully monitor his condition.
Symptoms
Moderate dropsy does not cause obvious deformities. External hydrocephalus is manifested by an increase in the volume of the cranium with divergence of the cranial sutures. The size of a newborn's head grows rapidly, increasing to 60 cm. A clear venous network appears on the skin. The fontanelles swell, including the lateral ones. Due to cranial deformation disorders, the position of the eyes changes.

“Sunset syndrome” is a typical eye condition in a child with hydrocephalus.
If symptoms appear in the prenatal period, natural childbirth is impossible due to the abnormal size of the head shape. Large amounts of fluid contribute to increased intracranial pressure. A child of 4–5 months of age develops tremors of the chin and hands, and convulsions occur. The disease is accompanied by nausea and vomiting. Pale skin, blurred vision, problems with heart function and eye movement are prerequisites for the disease.
Occlusive hydrocephalus is manifested by a lag in the psychomotor development of the child: the baby is inactive, his movements are difficult.
In an older child, the head size does not increase, but there is a sharp increase in cerebrospinal fluid pressure. This condition is accompanied by severe headaches, impaired memory, psyche, and intellect. The baby screams often. Moderate hydrocephalus is asymptomatic; the baby’s condition depends on the cause.
How to care for a child after surgery?
Surgery is very stressful for a child. Children cannot express their pain and discomfort, and therefore they only cry and are capricious. Parents must take care of the child after surgery to correct hydrocephalus.
You should feed your baby as usual
The child's operation is performed on an empty stomach, and after the operation he experiences hunger. After the baby regains consciousness, the mother can resume breastfeeding right in the hospital, after receiving the doctor's approval.
Normal breastfeeding can be continued at home, as the shunt in the ventricle will not interfere with digestion.
Give your baby solid food
Experts recommend giving your baby enough fruits and vegetables if he can eat solid foods. This diet will provide the child with enough microelements and vitamins, helping the healing process.
There is no need to bathe your child until the stitches are removed.
The doctor may use absorbable sutures or sutures that are removed later.
You do not need to bathe your child until the stitches are removed from the incision site. Removing the stitches means the wound is closed and safe for contact with water and substances such as soap.
Keep the incision area clean and dry
When using antiseptics to regularly clean the skin around the wound, you need to make sure it is dry.
You need to learn in detail about bypass surgery and hygiene after it from your doctor before leaving the hospital.
No physical activity for some time
Surgical wounds take time to heal; it is important that the shunt stays in place. Therefore, for six weeks after surgery, the child should refrain from potentially active games and activities.
The child can return to kindergarten after seven days, but should not receive physical activity.
Teach your child not to touch the shunt
Once the child recovers from the operation, he will become consciously interested in the strange lump on his head. Older babies are likely to touch the lump, which is the entrance of the shunt to the brain, while playing.
You need to teach your child not to touch the shunt by dissuading him with words like “no” every time he tries to do so. You need to keep your child's hands occupied with a toy whenever he feels bored and is about to touch the shunt to play.
US – navigation.
Separately, I would like to dwell on interventions using ultrasound navigation. This type of intervention falls into the category of gentle and minimally invasive. If the surgeon is sufficiently qualified under ultrasound control, manipulations can be performed with high precision. If the child is an infant, then the sensor is installed on the membrane of the large fontanel. In older children, the sensor is placed on the dura mater, for which a trefination hole is applied; often this is not required; it is enough to install the sensor on the temporal bone, which remains “transparent” even in adolescents. Below is an example of the complicated course of hydrocephalus with the so-called. isolation of the fourth ventricle.
In this case, ultrasound navigation made it possible to pass the ventricular catheter through the foramen of Monroe, the third ventricle, recanalize the aqueduct and pass it into the fourth ventricle, thus conducting Panventriculostomy:
On the presented tomograms, a 10-year-old girl has an extensive cyst in the chiasmatic-sellar region, which impedes the outflow of cerebrospinal fluid through the foramina of Monroe and causes occlusive hydrocephalus.
Under ultrasound control, puncture of the cyst was performed through the foramen of Monroe, followed by catheterization and implantation of the Omaya reservoir. Subsequent tomograms confirm the accuracy of catheter placement. Hydrocephalus has decreased significantly.
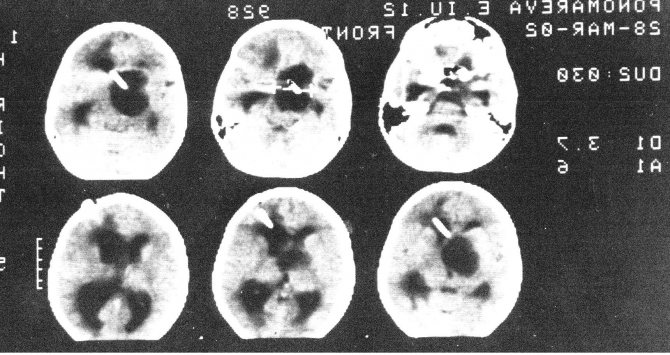
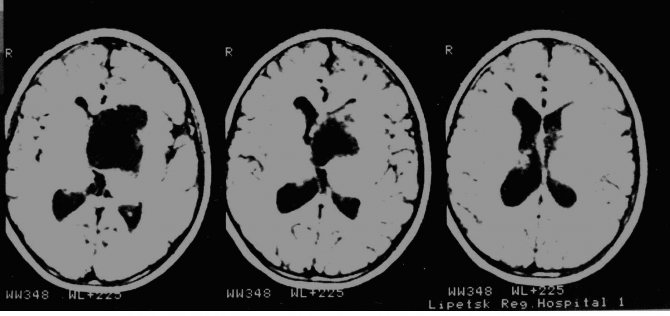
Subsequently, regular (once a month) punctures of the reservoir were performed, which ensured relief of hydrocephalus. The child attends a regular school. Control MRI after a year. It can be seen that the cyst retains its volume, but the hydrocephalus has been relieved.
A very important problem in pediatric neurosurgery is the problem of purulent diseases. The most common are rhinogenic complications, as in this case contact abscess of the frontal lobe. CM. snapshot:
This example has more academic significance, because... At one time, as in this case, it was customary to remove abscesses openly in the capsule.
Postoperative photo:
It is clearly visible that the brain is straightened. The lateral ventricle is not damaged. Subsequently, after 6 months. The child underwent cranioplasty surgery. Discharged without neurological deficit.
Currently, we practically do not use removal of an abscess in a capsule. Modern techniques are minimally invasive. We carry out catheterization of the abscess under ultrasound navigation and evacuation of pus, which makes it possible to easily cure even small and deeply located abscesses, as in this case in a teenager with Down's disease.

Prognosis of hydrocephalus in infants
Here are some important points to know:
- Babies with hydrocephalus have a good survival rate, with about 95% of babies surviving to live long, healthy lives. The life expectancy of such children corresponds to the life expectancy of normal infants. Excellent survival is possible thanks to treatment, which may be complex and imperfect, but still gives the child a better chance of life than living with hydrocephalus.
- The effect of the operation depends on the severity of the hydrocephalus, which affects the outcome of any possible complications. Children with mild hydrocephalus may recover more quickly than children with severe hydrocephalus. However, both will require frequent examinations to avoid any growth retardation.
- With congenital hydrocephalus, irreversible brain damage is possible. This causes parts of the brain to be unable to perform their normal functions. This can lead to other neurological problems such as epilepsy and seizures.
- There is a high chance that a child with hydrocephalus will have developmental delays. This includes learning disabilities, speech impairment, short attention span, memory problems and vision problems. However, experts say that about 50% of children with hydrocephalus grow up with normal cognitive function and intelligence.
- Rehabilitation and educational therapy can help the child catch up on lost development. The US National Institute of Neurological Disorders and Stroke (NINDS) states that rehabilitation treatment helps a child with hydrocephalus lead a normal life with minimal restrictions. Therapists who specialize in hydrocephalus can help avoid any developmental problems. Hydrocephalus should not interfere with a child's normal growth, but given the chance, any parent would no doubt want to avoid it.
Treatment
Conservative treatment is possible only for non-progressive open hydrocephalus. To reduce the amount of fluid, Diacarb, Furosemide, and Mannitol are prescribed. Incorrectly prescribed medication can worsen the child's condition. If the drugs do not have the desired effect, the disease continues to progress, surgical treatment is prescribed. The operation is also indicated in a closed form.
If the symptoms of the disease gradually increase and become a threat to the child’s life, ventricular drainage is performed.
This operation is performed extremely rarely, only in cases where it is impossible to save the child’s life by other methods. It always causes many complications. An increase in the amount of cerebrospinal fluid is caused by neoplasms in the brain. Their removal helps to naturally reduce fluid volume.
Previously, bypass surgery was used to relieve symptoms. This operation was often accompanied by a large number of complications. The child’s quality of life depended on the condition of the shunt; it had to be changed periodically. The latest advances in medicine have made it possible to replace bypass surgery with the endoscopic method of surgery.
The advantages of endoscopy treatment include:
- Low trauma;
- Reduced risk of complications;
- No need to embed foreign bodies;
- Effective reduction in the amount of cerebrospinal fluid.
Replacement hydrocephalus requires constant monitoring. Moderate compensated degree does not require surgical treatment. The child is being monitored at the dispensary. The key to successful rehabilitation and reducing the risk of relapse is a systematic examination and constant monitoring of the amount of fluid in the cavities of the brain and ventricle. Treatment is necessary, even if there is a slight increase in its volume, while internal dropsy is asymptomatic.
Can hydrocephalus in infants be prevented?
Unfortunately, despite its early detection in the womb, it is impossible to prevent hydrocephalus. Researchers are still working to find a way to prevent and treat this condition.
But parents can work to mitigate the risk:
- It is necessary to undergo regular examinations during pregnancy. Never miss a doctor's appointment when a woman is pregnant and stick to the recommended ultrasound schedule. Early detection of the disease gives the baby the best chance of surviving and living a normal life after birth.
- Get vaccinated during pregnancy. It is important to consult your doctor and get yourself vaccinated against diseases such as meningitis, as the disease can affect fetal brain development.
- You need to protect yourself from common diseases to minimize the risk of any adverse effects on fetal development.
- Children need to be protected from head injury . Prepare your home and protect objects that may be in the baby's crawling path. It is important to use a crib with safety bars to prevent your baby from falling. When traveling by car, use a child seat.
- It is worth immunizing your child . Protecting your child from diseases can minimize the risk of them affecting the brain. It is important to consult with your child's pediatrician about the vaccination schedule and follow it.
Hydrocephalus can be a lifelong condition, but most babies tolerate it well. It is worth monitoring for any complications after treatment and bringing your child for regular checkups. Hydrocephalus is certainly complex, but timely treatment is the key to ensuring a long and healthy life for the child.
Rate
—