Issues discussed in the material:
- Why do older people have memory problems?
- What diseases does memory disorder indicate?
- What types of memory impairment are there?
- How to improve memory in old age?
As a person ages, the processes of fading become more active. Signs of physiological aging are changes in appearance, psyche, and decreased performance. Memory becomes worse. First of all, in old age, its short-term form suffers. A person forgets events that happened very recently, for example, a day ago, does not remember why he left the house, but at the same time easily reproduces the details of situations that happened to him in childhood or youth.
Elderly citizens often lose orientation in space, their attention and ability to learn are impaired, and they sometimes cannot find the right words. Poor memory in older people is usually associated with the onset of Alzheimer's disease, the most common form of dementia, a severe and incurable disease described in 1906 by the German physician Alois Alzheimer. Fortunately, this is not always the case, and age-related memory changes are not necessarily a symptom of serious pathologies.
The nature of amnesia in old age
In older years, a person’s brain functionality decreases, the process of cellular renewal slows down, and biochemical processes deteriorate. The body is aging.
Although memory loss in older people is a common problem, it is not a necessary consequence of aging. In a healthy elderly person, memory functions worse, but is generally normal, with minor defects. He analyzes and assimilates new information more slowly, remembers large amounts of data worse, and may forget the name of someone he knows.
Serious memory impairment is associated with the influence of external causes: head injuries, circulatory disorders, mental disorders, long-term use of drugs and others.
Memory deteriorates gradually. First, a person forgets the events of the present, then - details and details. Then the memory of the events of youth returns. Then the person forgets personal information and stops recognizing people.
Causes
Age-related changes are the background for the development of memory problems. They cause disruptions in brain function. If a person does not train his mind, his memory will weaken over the years.
The causes of memory loss are varied. The main ones include the following:
• Lack of oxygen (hypoxia), due to which the brain suffers and remembers new information worse • Hypertension - high blood pressure • Cardiovascular diseases, which lead to impaired cerebral blood flow • Traumatic brain injuries • Severe chronic illnesses: varicose veins, diabetes diabetes, Alzheimer's disease, central nervous system problems • Intoxication of the body
The causes of memory impairment are also classified into groups. Thus, there are physiological and psychological causes of amnesia.
Physiological reasons are associated with disturbances in the functioning of the hippocampus and cerebral circulation, a decrease in the amount of proteins and hormones. These reasons include hypertension, ischemia, cerebral hypoxia, vascular aneurysm, oncology, varicose veins, intoxication of the body, taking medications and others.
Psychological ones include stress, frequent conflicts, psychotrauma, increased emotional and mental stress, loneliness, monotonous lifestyle, depression, chronic fatigue and others.
Diseases that cause memory impairment
The most common cause is traumatic brain injury. The second main reason is associated with poor blood circulation in the brain, which occurs with vascular atherosclerosis.
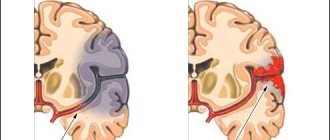
Having a stroke interferes with healthy blood flow to the affected area, leading to memory problems.
Vascular lesions in diabetes mellitus lead to various abnormalities, including in the functioning of the brain.
Encephalitis and meningitis affect all brain activity. If a person is diagnosed with these viral diseases, timely therapy must be started.
Thyroid disease can impair the memory of an older person. Such a patient experiences depression, irritability, weight gain, and muscle swelling. To solve the problem, normalize the level of iodine in the body with the help of medications and food.
Alzheimer's disease causes memory loss and decreased intellectual abilities. Most often it occurs in people aged 65-80 years. Unfortunately, modern medicine is not able to cure this disease, but it is possible to prolong the patient’s life and improve its quality with the help of palliative therapy. Therapy must be started as early as possible, otherwise amnesia will lead to serious consequences.
Causes of memory loss in older people
Changes that occur in the human body with age can cause disruptions in brain function. First of all, this concerns memory. Fortunately, not all cases of its deterioration are a manifestation of senile dementia. Our brain is capable of producing new cells at any age. However, as you know, the function trains the organ. If you don't work on your memory, it will constantly deteriorate.
- Recommended articles to read:
- Spots in an elderly person: causes and ways to get rid of them
- Extensive heart attack - consequences and chances of recovery
- Skin of older people: its features and main diseases
There are three known physiological reasons that result in memory impairment with age:
- Deviations in the functions of the hippocampus. This is an area of the brain involved in two types of memory - declarative and spatial.
- Reduced levels of hormones and proteins that stimulate the formation of neural connections.
- Cerebrovascular accident. Leads to memory loss and negatively affects cognitive skills.
Thus, memory lapses in older people can be caused by reversible (involutional) or irreversible processes that arise as a result of destructive changes in the brain. It is important to distinguish them from each other in time. There is nothing wrong with the fact that you forgot where you left this or that thing, or called a friend by a different name. In old age, a person is more easily distracted and often has problems remembering information.
To make it easier to understand what causes led to memory loss in older people, they were divided into several categories:
- Associated with brain damage. These are, for example, traumatic brain injuries, brain cancer, stroke.
- Associated with deterioration in the performance of other equally important organs.
- Unfavorable factors such as sleep disturbances, regular stress, sudden changes in lifestyle, increased stress on the brain, especially memory.
- Alcohol abuse, smoking, frequent use of sedative medications and hard drugs.
- Natural age-related changes.
Memory impairment in the elderly: what to look out for
If a person periodically forgets some things, calls people by other people’s names, there is nothing wrong with that. Such rare forgetfulness and temporary memory lapses are typical for older people and do not harm his life.
You need to be wary when memory lapses in an elderly person occur frequently, progress and are accompanied by a deterioration in mental abilities: the ability to think logically, speak well, etc. This is how senile dementia can develop.
The person may have difficulty with everyday activities. If he pronounces words incorrectly, gets lost in space, behaves inappropriately in society, you need to take the person to a doctor.
What should you be wary of when memory loss occurs in older people?
If an elderly person periodically loses memory and this is not associated with the onset of senile dementia or other serious diseases, then such temporary lapses will not significantly affect his daily lifestyle. But if there is a progressive weakening of at least two intellectual abilities (memory and speech or abstract thinking and the ability to think logically), then this is a reason to be wary. Such changes may be a sign of senile dementia.
Thus, if memory decline does not interfere with a person’s daily life, it is associated with normal age-related processes. In the case of serious pathologies, the old person has difficulty performing simple, familiar tasks that previously did not cause inconvenience.
Read the material on the topic: Doctor for older people - features of the geriatrician profession
Alarming symptoms that indicate a greater likelihood of developing dementia in an elderly person are loss of orientation in familiar places, distortion of words or phrases, and inappropriate social behavior. In such cases, you should consult a doctor as soon as possible. You will need to undergo a medical examination to proactively prevent possible problems in the future.
A neuropathologist, taking into account the individual characteristics of the patient, will propose measures to eliminate reversible processes and prescribe a course of memory treatment in older people. The sooner and more accurately the diagnosis is made, the sooner therapy can begin. And this will allow you to get rid of reversible impairments of memory and attention and improve the quality of life in case of incipient Alzheimer's disease or other types of dementia.
When you see a doctor, be prepared to answer the following questions:
- Since when have memory problems been observed?
- what exactly is difficult to remember;
- memory impairment was gradual or sudden;
- Do problems arise in your usual activities?
The specialist will also be interested in topics related to the patient’s lifestyle and the medications he is taking. As a rule, an elderly person is monitored for several months, after which, based on the information collected, the doctor will be able to prescribe the necessary medication and physiotherapeutic treatment.
Types of memory disorders
Amnesia is divided into types depending on the nature of the loss of information. There are the following types of memory loss:
• Partial or complete. With partial, a person cannot remember some events of his life; with complete, memories disappear entirely. • Short term or long term. In short-term, a person does not remember new information that he received in the last hours or days; in long-term, he forgets events from the long past - from several months to several years ago. • Temporary or permanent. Temporary is associated with temporary forgetfulness, then the memory is restored (for example, a person forgets the name of a friend, and after a while remembers). Permanent amnesia is the loss of information that a person can no longer remember. • Anterograde (a person forgets the past, but remembers the present well) or retrograde (on the contrary: a person remembers the present poorly, but remembers the past well). • Gradual or sudden. Gradual memory loss occurs over time; memory weakens slowly. It is difficult to diagnose and predict. In case of sudden memory loss, a person immediately forgets important data: first and last names, address, loved ones. A lost pensioner with sudden amnesia cannot remember where his house is or clearly explain its location. • Sharp. Happens suddenly and has a strong impact. With it, a person cannot normally do even simple everyday activities; he forgets what he was going to do today. This amnesia is caused by brain pathologies or emotional problems. If you do not pay proper attention to the disease, it will begin to progress. • Visual - affects visual perception, a person does not recognize loved ones, familiar places. • Reversible (can be cured) and irreversible (cannot be cured). • Global - a person does not remember the past and does not remember new events.
There are also other types of memory loss:
• Korsakovskaya. Develops due to alcohol abuse. People forget events during periods of severe intoxication or hangover. • Senile. Develops over the years. People with this disorder increasingly remember events from past years. • Post-stroke. An attack that has been suffered impairs the functioning of a person’s senses and thinking. • Semantic. A common senile amnesia, in which memories of the outside world are lost. In a mild form a person forgets the names of objects, in a moderate form he does not remember what different objects are for, in a severe form both disorders are combined. • Procedural. A person loses everyday skills. Forgets how to brush teeth, wear clothes, and use cutlery. He needs constant help. • Professional. Associated with a person's work. He forgets how to properly perform his professional duties.
Amnesia in old age, together with disorders of thinking and attention, leads to senile dementia. The disease is progressing. It all starts with forgetfulness of individual moments and events. For example, a person forgets whether he closed the door or took his medicine. Then the events of the past are forgotten, and then the person stops recognizing his acquaintances.
Symptoms
Amnesia is accompanied by the following symptoms:
• Confusion. Restless thoughts cause short-term memory loss. • Speech problems – associated with brain disorders. May occur due to dementia or head injuries. The person speaks indistinctly, changes words, does not pronounce the ending, and loses the logic of the conversation. • Headaches that provoke infections and traumatic brain injuries. • Trouble concentrating – caused by an infection or brain tumor. Inattention interferes with a person's ability to perform daily activities. • Impaired coordination and orientation in space. These symptoms may indicate the onset of Alzheimer's disease. • Tremor – develops along with memory loss. With sudden forgetfulness and panic, a person experiences trembling in the body. • Feeling tired. It can develop due to exercise, thyroid problems, brain tumors, or a virus. • Dizziness – indicates a lack of coordination. • Bad mood, lack of interest in everyday activities and events.
Symptoms occur in different combinations. If a person has already developed senile dementia, then additional disturbances in movement and orientation in space occur.
Also, amnesia in the elderly is characterized by additional signs that manifest themselves in psychology, behavior, and human health:
• Changes in handwriting • Violation of given promises, forgetfulness about upcoming events • Absent-mindedness in terms of daily affairs. A person may forget about simple actions: close the door, turn off the iron, etc. • Negligent hygiene: a person stops taking care of himself, forgets about the rules of cleanliness, does not maintain order at home. • The person becomes slow and cannot perform normal activities well. • Irritability, aggressiveness, demandingness, capriciousness, vulnerability, and touchiness arise. • The patient calls relatives by other people's names.
Memory loss is itself a symptom of other illnesses, often mental or neurological disorders.
LiveInternetLiveInternet
In old age, neurological disorders of the brain often occur. One of the most severe and steadily progressing diseases is Alzheimer's disease (AD). The pathogenetic mechanisms of its appearance are neurodegenerative processes, and the main symptom is early maladaptive syndrome with memory impairment. In addition, diseases that lead to these disorders include acute cerebrovascular accidents. During such ischemic attacks, the brain is seriously damaged, so memorization and memory in general are impaired. Also, diseases leading to memory impairment include anxiety-depressive disorders and extrapyramidal pathology. Not only diseases can lead to cognitive disorders in old age. It is believed that some of the changes that occur are a physiological norm during the aging process of the body and, in particular, the brain. A decrease in cognitive abilities worsens a person’s quality of life, which is a very significant and pressing medical and social problem, which is quite difficult to solve. If a person loses clear memory, he cannot work normally, cannot perform everyday tasks, and cannot communicate with people on the same level as before. Memory loss is a tragedy for a person, which is why we talk so much about it now. Cognitive disorders lead to discord between relatives. People change the usual patterns of their lives, become irritated, and often experience stress and quarrels with each other. In addition to personal problems, these diseases lead to large economic losses for the state, since the need for treatment and rehabilitation of patients requires the expenditure of serious funds. In addition, memory loss often begins at working age, which leads to the loss of a person capable of working and disability. Modern medicine cannot yet fully restore a person with such problems, but work in this direction is underway and there are some successes. At the end of the 20th century and the beginning of the 21st, scientists obtained innovative data on the structure, pathogenetic features and neurochemical transformations of major neurodegenerative diseases. This knowledge has made it possible to reconsider some approaches to treatment and build new therapeutic regimens. It has been proven that symptomatic treatment for developing dementia in old age is effective and this effectiveness has been fully proven in practice. Risk factors for the development of memory disorders The next risk factor is genetic predisposition. This factor, however, like age, cannot be corrected in any way. AD is one of the most common causes of dementia and this disease is completely genetically determined, that is, completely dependent on heredity. The risk of developing asthma is especially high in the presence of sick close relatives who became ill before the age of 60 years. Those who became ill after the age of 60 most often acquired the disease by accident. However, the risk of the disease in relatives of these people increases significantly. The first and most significant risk factor has always been and will be old age. Memory loss in old age is normal, as many believe. By the second half of life, the human brain undergoes changes that subsequently lead to the formation of the diseases described above. These changes reduce the effectiveness of the brain's protective barriers and mechanisms. In old age, the number of neural connections decreases, the number of synapses decreases, and the activity of the dopamine, norepinephrine, and acetylcholine systems, which contribute to the conduction of impulses along nerve fibers, decreases. Neuronal plasticity, that is, the ability of neurons to vary functional properties during adverse effects, is reduced, and thus the compensatory capabilities of the brain and nervous system, in general, are practically reduced to a minimum. Another equally important cause of memory loss is cardiovascular pathology, and among the entire area, arterial hypertension stands out in importance. Non-synchronous studies in different world regions have shown that the presence of arterial hypertension in middle age significantly increases the risk of developing neurodegenerative changes in the brain in old age. Why arterial hypertension contributes so much to the development of memory impairment is now being clarified, but there are opinions that foci of microinfarctions form in the brain, which lead to the development of AD and vascular cognitive impairment. For example, type 2 diabetes mellitus reliably leads to cognitive impairment. The Rotterdam study confirmed that the risk of developing memory impairment in patients with type 2 diabetes is 2 times higher than in peers from the control group. Abdominal obesity and hyperlipidemia also contribute to the development of memory impairment as a person ages. Scientists have identified a pattern of maximum risk of developing these changes in patients simultaneously suffering from type 2 diabetes mellitus, arterial hypertension, and abdominal obesity. Traumatic brain injury is a serious risk factor, depression, deficiency of B vitamins, female gender. Methods of non-drug prevention of folic acid deficiency, insufficient active intellectual and physical activity in youth. 1. A diet containing sufficient amounts of natural antioxidants. Natural antioxidants include vitamins E and C, which are present in vegetable oils, citrus fruits, and seafood. The “Mediterranean diet” is able to provide the human body with all the necessary substances that improve neurotransmitter activity and communication between neurons. 2.Memory training is systematic and constant. People with intellectual work are least susceptible to cognitive disorders in old age. Of course, dementive manifestations are present, but such people can cope with them much easier and more effectively. All older people need memory and attention training. 3. Adequate regular physical activity. There is reliable evidence that CI disorders appear much later in older people if they are physically active. This dependence can be explained by the positive effect of physical activity on the emotional sphere, cardiovascular system, and body mass index. Prevention of CI and treatment of the cardiovascular system Diseases of the cardiovascular system affect the formation of CI, so for many years scientists have been wondering what effect does the treatment of these diseases have on the risk of CI in old age? Some studies suggest that, for example, the calcium channel blocker nitrendipine may be prescribed as a preventative treatment when early symptoms of dementia develop. Eprosartan and a combination of perindopril with indapamide have also shown their effectiveness in the prevention of CI. Other antihypertensive drugs did not produce such effects. It should be noted that such positive effects of the drugs described above appear only when blood pressure is stabilized within normal limits. The use of statins in the prevention of CI is of great interest. Recently, experimental evidence has emerged that increased cholesterol negatively affects not only the condition of peripheral blood vessels, but also contributes to the formation of senile plaques in the brain, as in AD. There are few studies on statins and their preventive effect, so the data is quite contradictory and unproven. Metabolic and vasoactive treatments for memory loss are used. These treatments are very accessible and are prescribed almost everywhere. At the same time, good results are achieved in improving memory and eliminating other vascular symptoms. The patients' well-being improves and their mood rises. The neuroprotective effect of these drugs is being hotly debated. For example, ginkgo biloba increases microvascular tone by acting directly on arterioles without the stealing effect. The rheological properties of blood improve, there is no pathological thrombus formation. Memoplant, which contains ginkgo biloba, is used very quickly in elderly patients due to its excellent vasoactivity and antioxidant effect. During studies of this drug, it was revealed that against the background of placebo (dummy effect), CIs developed more often than in the group of patients taking Memoplant. Another approach to therapy is the use of the NMDA receptor blocker memantine. This method is accepted by official medicine. When preventing and treating CI, it is necessary to understand that without treatment of concomitant diseases, the effect will be low or there will be no effect at all. In old age, a person has a sufficient baggage of diseases that will develop or aggravate cognitive impairment. Such diseases include hypothyroidism, chronic heart failure, chronic obstructive pulmonary disease, and substance abuse. From the above it follows that the treatment of cognitive impairment should be comprehensive and affect all pathological conditions present in the patient in order to achieve the most positive result. Thus, there are currently established therapeutic approaches to patients with cognitive impairment at all stages of the pathological process. In elderly people without cognitive impairment, preventing their occurrence is the correct and timely treatment of cardiovascular diseases, systematic intellectual exercises, balanced nutrition and physical activity. For cognitive impairment that does not reach the severity of dementia, it is advisable to carry out vasoactive and neurometabolic therapy. In patients with dementia, acetylcholinesterase inhibitors and memantine are the first choice drugs. At all stages of cognitive impairment, treatment of concomitant somatic diseases and correction of the emotional state are relevant.Diagnostics
A neurologist diagnoses and treats the problem. The person may also be sent to a neurosurgeon, psychotherapist and other specialists.
Diagnosis begins with a detailed interview with the patient. Experts find out the symptoms and nature of amnesia and its cause. They use information about a person’s health and illnesses to find the root cause. This information will help restore healthy brain activity.
During the interview, the specialist finds out the following points: • When memory impairment began • What is the nature of the problem: memory is lost abruptly or gradually • What is difficult to remember • Are there any problems with everyday activities • What is the patient’s illness and what medications is he taking?
The patient undergoes laboratory tests to determine nervous system disorders that affect memory. For research we use:
• Biochemical blood test • Cerebrospinal fluid analysis • Electroencephalogram • Toxicological tests • Brain examination • Blood vessel analysis • DSM – duplex scanning of cerebral vessels • CT – computed tomography of the brain • Doppler ultrasound of cerebral vessels
It is necessary to carefully study the patient's situation and observe him for some time in order to correctly identify the problem and prescribe the correct treatment.
Memory tests
These memory exercises can be done independently at home to test your memory.
Test No. 1
The “Shopping List” test is suitable for testing short-term memory. Write down any 10-item shopping list on a piece of paper. Let the elderly person study it for 40 seconds and remember it. Then check how many items from the list the person remembers: you can ask orally, or write down on paper. Missing an item or incorrectly named word from the list is counted as an error. If there are no errors, then everything is fine with the memory. If a person has up to 4 errors, then he has normal memory for old age. If there are 5 or more errors, the brain needs help.
Test No. 2
Ask the subject to draw a clock face with a specific time. This test not only tests the memory of an elderly person, but also the soundness of his thinking. If the dial is depicted evenly, the numbers are located correctly and do not stand out from the general row, the hands are also even and correctly indicate the given time - the person is healthy, his memory is in order. When dementia begins, the drawing will be crooked, the numbers will be of different sizes, in the wrong order, the arrows will be uneven, and show the wrong time. Severe deviations from the normal pattern may indicate the onset of dementia. This simple test can be done regularly to check on an older person. If severe defects are detected in the drawing, the person should be taken to a doctor for diagnosis.
Test No. 3
This test tests long-term memory. You need to write down several contacts of your loved ones on a separate sheet - up to 5-10 numbers. Try to learn this list, and then check the quality of memorization after 1-3 days. If a person can correctly recall most of his contact list, he is doing well with long-term memory. If not, there is something to work on.
Stay calm and... could you do it again?
Chances are, you won't be as flexible at age 60 as you were at 20. Or as fast. Or strong. Time affects your body, and your brain is affected too. The connections between brain cells that create and store memories change with aging. Just like proteins, the hormones that support our brains don't work as well as they used to. As we get older, we need to understand the difference between typical forgetfulness, which is not pathological, and the warning signs that the cognitive decline that dementia causes is beginning.
Details aren't everything
Typical of aging : you forgot to meet a friend, but remembered about it later. You remember going to a wedding last year, but you're a little hazy about all the guests who were there.
Please note : you are confusing the directions left and right. You ask friends and family about the same details over and over again. You forget about events that happened recently or details of a conversation that just took place.
Beware of numbers
Typical of aging : You make minor financial mistakes from time to time. You forgot to pay the bill on time, but paid it a little later. Or you just added 3 tablespoons of sugar instead of teaspoons.
Please note : You find it more difficult to concentrate to make plans and solve problems. Numbers feel like a foreign language, and you find it difficult to manage your finances or take your medications as prescribed.
Dementia in the elderly when it comes to more than just fun and games
Typical of aging : You need help setting the clock on the microwave or recording your favorite shows. You forgot for a moment whether a straight flush beats a straight flush in poker or vice versa.
Please note : you may not be able to master the use of your cooker. You have forgotten the rules of the game of basketball or tennis that you have played or watched regularly for many decades.
Where did I put this?
Typical of aging : you have to check your pockets, the kitchen table, your car; you repeat all the steps until your keys are finally found.
Please note : you put things in unusual places, find your phone in the freezer. You can't remember what steps to follow and what places to check to find your keys, or you accuse someone of stealing things.
Why am I here?
Typical of aging : sometimes you come into the kitchen and can't remember what you needed there. You sometimes forget the name of the street when explaining directions. It may take you a little longer, but you always get to familiar places.
Please note : you cannot find your way home or you get confused in places that you know well.
Give me this, what's it called?
Typical of aging : you forget the name of an object. The word is on the tip of the tongue, but is not remembered.
Please note : you name things incorrectly, sometimes it is really paradoxical: a “spoon” can become a “bed”. You stop mid-sentence and have no idea what you were saying.
I just want to be alone for a while
Typical of aging : The combination of work, family and social demands leaves you feeling exhausted, even if you enjoy those things.
Please note : You can no longer support the sports teams you would normally follow. You avoid communicating with people to hide the problems you have.
Senile forgetfulness: what is his name...
Typical of aging : you suddenly forget the name of your best friend or name your grandchild after your son-in-law.
Please note : you really can't remember your son's name.
Self-care disorder
Typical of aging : you are in a hurry and forget to brush your teeth in the morning.
Please note : you don't just forget to brush your teeth, you don't remember how to do it. You cannot choose the right clothes for the weather and fasten all the buttons.
Seriously, it's not a problem
Typical of aging : You worry about your memory, but your family doesn't. You remember when you forget things and how you feel at that moment.
Note : Your family is worried about you, but you don't know what they're talking about and you think you're fine.
If my problems are not typical, then what is happening to me?
Many diseases can cause memory problems. People often think about Alzheimer's disease or other types of dementia. This is one possibility, but there may be other types of pathology behind it, and some of them may be reversible. For example, it could be a lack of vitamin B12, one of the key vitamins for your brain. Or depression, thyroid problems, even lack of fluid.
When to see a doctor
If any of these warning signs sound familiar or are affecting your daily life—your job, hobbies, and family relationships—consult your doctor. It's a good idea if one of your family members goes to the doctor. Normal age-related memory changes will give you pause for a moment, but they shouldn't stop you from moving on with your life.
How to prevent memory loss
Do all the normal things that are good for you: hang out with friends, exercise, eat well, get enough sleep and don't smoke. Think of your brain as a muscle - exercise it. Do crossword puzzles or Sudoku. Read books or magazines that challenge your mind. Learn a foreign language or master a new musical instrument. Do activities that require planning, such as gardening or quilting.
Treatment
A specialist will study the situation and draw up a treatment course. The sooner the diagnosis is made, the sooner therapy can begin. With reversible memory loss, this is especially necessary: it is easier to restore memory and prevent dementia.
Therapy uses medications, physiotherapy, psychological methods, dietary changes, and folk remedies.
Treat the root cause of amnesia. This can be acute or chronic circulatory failure in the brain, which occurs due to cardiovascular diseases. If a person has atherosclerosis of the head arteries, arterial hypertension, or heart disease, they need to be treated.
Medicines
For atherosclerosis of the main arteries, antiplatelet agents are prescribed, and for high cholesterol, statins are prescribed. If the cause is head injury, the person is prescribed medications to improve metabolism: absorbable, nootropic, diuretic. If memory loss occurs due to dementia, neurotropics are used. It is necessary to combat harmful factors: physical inactivity, smoking, obesity, diabetes mellitus - they can lead to cerebral ischemia.
• Antiplatelet agents and vasodilators improve cerebral blood flow and tissue blood supply. • Neuroprotectors and antioxidants harmonize metabolism in neurons, making a person more resistant to hypoxia and adverse effects. Combined neuroprotectors are drugs with multiple effects to solve several problems at once. • Memantines help with Alzheimer's disease. • Nootropic drugs stimulate cognitive abilities, improve metabolism in cerebral tissues. They help fight aging, mental disorders, and improve memory. • Anticholinesterase drugs inhibit the development of dementia in old age. • Antioxidants. They block the action of free radicals, heal and renew tissues, and make cells resistant to hypoxia. • Adaptogens - herbal remedies and multivitamin complexes. Help the body fight age-related changes.
ethnoscience
Useful herbs for general strengthening will have a good effect on the health of the entire body and improve memory. They are recommended to be used as additional means to primary drug therapy.
Several recipes:
• Pour eleutherococcus roots (40 g) with water (0.5 l), heat and boil for 10 minutes. The decoction is taken 150 ml four times a day. • Pour 1 liter of hot water over walnut leaves (50 g), cover with a towel and leave for several hours. Take 150 ml three times a day. • Pour thyme (1 tbsp) into a jar and add boiling water, leave for 15 minutes. Take one cup 3 times a day. This remedy improves memory and slows down the development of amnesia. • If memory loss is due to a head injury, you can use a walnut-based remedy. Chop the peeled walnuts into small pieces and add honey. Take one tablespoon three times a day for a month. • For atherosclerosis, which also affects memory, it is useful to take a thinning agent based on dill seeds. Place one tablespoon of seeds in a saucepan, add 0.5 liters of hot water, leave for half an hour. Take half a glass before meals 3 times a day.
The following folk remedies are useful:
• Drink pumpkin juice regularly, the daily norm is 100 ml • Drink a decoction of dried rowan bark • Eat 4 pieces of young pine buds • Drink clover tincture for 2 months
Nutrition for amnesia
It is important to change your diet. If a person is addicted to junk food, he needs to switch to a healthy diet. It is useful to include foods that strengthen memory: apple, banana, carrots, cottage cheese, sour cream, nuts, chocolate, potatoes, horseradish. Food should be rich in vitamins; you can take vitamin complexes.
Dietary recommendations:
• The basis of the diet should be plant foods and dairy products • You need to eat in small portions and regularly, follow a meal plan by the hour. • Food must be fresh and prepared from quality ingredients. • You need to avoid fatty, fried, smoked and spicy foods. Eliminate processed foods, fast food, and high-calorie foods.
Examples of healthy dishes that can be included in the menu: whole grain porridge with milk, buckwheat/rice as a side dish, light broth soup, lean meat, cottage cheese casserole, vegetable stew, fruit salad.
Additional treatment
Electrophoresis and massage are popular physiotherapy procedures. In psychological treatment, exercises are used to train the brain. Psychotherapy helps the patient to recall forgotten events. Hypnotic practices may be used.
Exercise therapy improves motor and brain activity, blood circulation, and endurance.
If the cause of memory loss is a hematoma or brain tumor, the person is prescribed neurosurgery.
The course of treatment is drawn up by the doctor after a thorough diagnosis. You can’t choose your own remedies and self-medicate. If you notice obvious symptoms of amnesia, you should immediately consult a doctor. Treatment is necessary: if the problem is neglected, it can reduce a person’s quality of life and worsen his social ties with society. In old age, amnesia progresses without treatment.
Memory impairment in the elderly
P
Increased forgetfulness is one of the most common complaints in elderly patients. Memory loss in old age can be both a consequence of physiological age-related changes in the central nervous system and a pathological symptom of a number of brain diseases. Therefore, a careful analysis of the nature of mnestic disorders is of great importance for the early diagnosis of neurogeriatric diseases and the selection of the correct tactics for patient management.
Physiological changes in memory
Numerous experimental psychological studies are consistent with everyday observations that older people learn new information worse than young people. Age-related difficulties in the mnestic sphere usually arise when handling large amounts of information or when working simultaneously with several sources of information. This may make it somewhat difficult for older people to learn new skills and requires a more strict external organization of professional activities (for example, the use of notebooks, schedules, etc.). At the same time, physiological forgetfulness never extends to current or distant life events, as well as general knowledge acquired in young or middle age. The presence of amnesia for current events, partial loss of professional or everyday competence is always a pathological sign indicating the onset of a brain disease [5,29,31,43].
Memory decline in old age is combined with a number of other changes in cognitive functions
. The latter relate primarily to reaction time, which tends to increase with age [29,31]. As a result, older adults take longer to perform the same amount of mental work than younger adults. Fatigue during mental exercise in old age also develops somewhat faster than in young people. Obviously, these phenomena are based on “neurodynamic” (in the terminology of A.R. Luria) changes in higher nervous activity, that is, a decrease in the activating influences on the cerebral cortex from nonspecific activating cerebral structures [8–11].
Physiological age-related changes in cognitive functions, according to neuropsychological research methods, occur between the ages of 40 and 65 years. Age-related changes in cognitive functions are non-progressive: thus, according to F. Huppert and M. Koppelman, healthy individuals over 65 years of age are not inferior in memory performance to individuals in the age range of 55–65 years, but both are significantly inferior to those aged twenty [39]. It is assumed that physiological changes in higher brain functions are based on changes in cerebral metabolic processes associated with hormonal changes [39,43].
In everyday medical practice, distinguishing between normal and pathological changes in cognitive functions is often a very serious problem. An attempt at a neuropsychological approach to this problem consists in the use of special techniques that stimulate the attention of patients at the memorization stage. For example, the patient is asked to sort the presented words into semantic groups (plants, animals, etc.), and then the name of the group is used as a hint for reproduction (methodology by Grober and Buschke, 1988). It is believed that in the presence of only physiological memory decline, such stimulation of attention equalizes the performance of elderly and young people [27,35,36]. It should also be noted that visually presented information is remembered in old age better than auditory-speech information [29].
However, with relatively mild pathological forgetfulness (for example, in the earliest stages of organic brain damage), neuropsychological research methods can give false-negative results. Therefore, from a practical point of view, active complaints of forgetfulness should always be considered a pathological symptom. However, this symptom can be both organic and functional (psychogenic) in nature, which requires additional consideration.
Memory impairment due to organic brain damage
Most often, progressive memory loss in old age is a manifestation of Alzheimer's disease.
(BA). AD is one of the most common neurogeriatric diseases of a degenerative nature. According to statistics, this disease underlies at least half of the cases of dementia in the elderly and is observed in 5–10% of people over 65 years of age [19].
The risk of developing asthma is primarily due to genetic factors. The presence of cerebrovascular insufficiency and a history of traumatic brain injury are also considered pathogenetic factors. In typical cases, the first symptoms of the disease appear at the age of about 70 years and affect the mnestic sphere. Common complaints from patients: the inability to remember what they just read or saw on TV, the names of new acquaintances, difficulty finding the right word in a conversation. Forgetfulness is progressive in nature and at advanced stages of the disease it spreads to life events: first of the immediate past, and then of the more distant one (Ribault’s law). Advanced stages of the disease are also characterized by other cognitive disorders: difficulties in spatial orientation, counting and speech disorders [26,40,41,43,47,54].
The rate of progression of mnestic and other cognitive impairments in AD is individual. The age of onset of the disease can serve as a marker for the severity of genetic burden: the more severe the genetic defect, the earlier the disease begins and progresses faster. Therefore, presenile forms of asthma are less favorable in prognostic terms. When asthma begins in old age, disease progression may be slower. Sometimes there is a long-term stationary state of cognitive impairment, which does not exclude the diagnosis of AD [26,40,48].
Diagnosis of AD is based on the presence of dementia, the core of which is memory impairment, and the absence of clinical and neuroimaging signs of focal brain damage. At the predementia stages of the disease, when almost the only clinical manifestation is memory loss, the diagnosis, according to the recommendations of the AD Association (NINCDS-ADRDA), is formulated tentatively (“possible AD”) [48].
Another common neurodegenerative disease, dementia with Lewy bodies,
(DTL). DLB is related to AD in genetic, neurochemical and pathomorphological terms. The distinctive clinical signs of this disease are the motor symptoms of parkinsonism and the early development of neuropsychiatric disorders in the form of recurrent visual hallucinations. In some cases, motor or psychotic disorders may come to the fore of the clinical picture, overshadowing relatively mild or moderate mnestic and other cognitive disorders [49].
In contrast to AD or DLB, memory impairment with vascular lesions of the brain as part of discirculatory encephalopathy
(DE) are presented more modestly. In typical cases, DE is characterized predominantly by a “subcortical” type of cognitive impairment. This is due to the fact that the basal ganglia and deep parts of the medulla are the zone of “terminal blood supply” and are therefore most vulnerable to insufficiency of cerebral blood flow [4,13,14,17,38]. “Subcortical” dementia is characterized primarily by slowness of cognitive processes and dysregulation of voluntary activity in the form of inactivity, inertia, perseveration and impulsive behavior [18,32]. It should be noted that the term “subcortical” dementia itself is not accurate, since these symptoms have a “cortical” pathogenesis associated with dysfunction of the frontal regions of the brain [16]. The latter probably arises as a result of deafferentation of the frontal cortex due to disruption of frontostriatal connections [14,17,38].
Memory impairments in DE, as in other “subcortical dementias,” are secondary in relation to dysregulatory disorders. They are based on insufficient activity and disturbances in the planning of mnestic activity. Memory impairments in this case, as a rule, are obvious only when using neuropsychological research methods, but do not extend to current life events [4,14,17,18,32].
Often vascular damage to the brain is combined with neurodegenerative changes
. The incidence of “mixed” (vascular degenerative dementia) is at least 20%, which is significantly higher than expected from a random combination of two diseases. Experimental observations are consistent with clinical ones and indicate that cerebral vascular insufficiency is the unfavorable background that accelerates the clinical implementation of genetic predisposition to AD. Therefore, among people with vascular diseases of the brain, the incidence of asthma is higher than in the population [40,47].
Dysmetabolic disorders
as a result of somatic or endocrine disease,
nutritional disorders, intoxication
can also cause memory and attention disorders in old age or can aggravate disorders associated with structural brain damage. Among the dysmetabolic causes of cognitive disorders, the most important to note are hypothyroidism, liver failure, chronic hypoxemia as a result of respiratory failure or sleep apnea, deficiency of cyanocobalamin and folic acid, abuse of alcohol and psychotropic drugs.
Functional memory disorders
Complaints of memory loss are a typical symptom of anxiety and depressive disorders. Mental disorders of anxiety and depression are the most common cause of increased forgetfulness in young and middle age, when organic memory disorders are rare. In old age, both functional and organic memory impairments are quite expected, and their combinations are often encountered [47]. This is due to the high prevalence of depression in the elderly. The latter has both organic and situational prerequisites. We are talking, on the one hand, about involutive changes in neurotransmitter systems, and on the other hand, about changes in social status, loss of close relatives, and the occurrence of chronic diseases, which often occurs in old age. In addition, depression can be a manifestation (sometimes the debut) of organic brain damage, for example, Parkinson's disease, dementia with Lewy bodies, cerebrovascular insufficiency, etc.
Memory impairments in anxiety-depressive disorders are most often explained in psychodynamic terms. It is assumed that the basis for insufficient memorization is the inability to switch attention from current psychological experiences to solving current cognitive problems. The inability to concentrate on everyday problems can be so severe that the patient ceases to cope with his professional and everyday responsibilities (“pseudo-dementia”). However, objective disturbances of mnestic function, according to neuropsychological research methods, are absent or minimally expressed and cannot explain the degree of maladjustment. Memory impairments, as a rule, do not affect emotionally charged events. Anxiolytics, in particular benzodiazepines, improve memory and recall of information
. This is due to the secondary nature of mnestic disorders in relation to anxiety, since according to their pharmacological properties, benzodiazepines, on the contrary, weaken the processes of registration and consolidation of the memory trace [33,43,47].
The functional nature of memory disorders can be judged on the basis of the above-mentioned features of mnestic disorders and their combination with other symptoms of anxiety and depression. It should, however, be noted that the presence of depression does not mean the absence of organic brain damage. On the contrary, as already noted, emotional disorders are typical of many organic diseases of the central nervous system.
Principles for the management of memory impairment in the elderly
Complaints about memory loss in old age require, first of all, the objectification of cognitive impairment. For this purpose, neuropsychological research methods
. The following methods are the easiest to use and very informative: a brief study of mental status, a clock drawing test, the Grober and Buschke technique in various modifications, memorization and retelling of a short text (for example, “Jackdaw and Doves” according to the method of A.R. Luria) [5 ,8,36,37,46]. To assess the extent of the impact of cognitive disorders on everyday life, a conversation with the patient’s relatives or his colleagues is necessary. If there is objective evidence of cognitive impairment and changes in daily lifestyle as a result of the latter, a diagnosis of dementia is legitimate. It is important to note that when making a diagnosis of dementia, one should not wait for the patient to become severely maladjusted. According to current guidelines, the presence of clinically significant deterioration in cognitive function that affects daily life is a sufficient basis for the diagnosis of dementia [12,20].
If there are complaints of forgetfulness, but minimally expressed objective cognitive impairment, as well as in the absence of changes in the usual lifestyle, the diagnosis, according to the ICD-10 recommendations, can be formulated as “mild cognitive impairment” [12].
Treatment of cognitive impairment
both at the stage of mild cognitive impairment and at the stage of dementia, should, if possible, be etiotropic or pathogenetic. However, in all cases the following measures are advisable:
– correction of dysmetabolic disorders
, which may cause or aggravate existing mnestic disorders. In some cases, it may be advisable to prescribe ex juvantibus therapy with cyanocobalamin and folic acid. It is important to note that with timely diagnosis and treatment, cognitive impairment of a dysmetabolic nature is reversible;
– treatment of diseases of the cardiovascular system
. As noted above, vascular damage to the brain has pathogenetic significance both in dyscirculatory encephalopathy and in neurodegenerative diseases. Therefore, control of arterial hypertension, hyperlipidemia, administration of antiplatelet agents and other known measures are the pathogenetic treatment of most cases of dementia;
– depression treatment
. In the presence of emotional disorders, psychotherapy and psychopharmacotherapy for depression are mandatory measures, regardless of whether cognitive impairment is only psychogenic or emotional disorders are secondary to organic brain damage. In the treatment of depression in elderly people with memory impairment, drugs with anticholinergic properties, such as tricyclic antidepressants, should be avoided. Selective serotonin reuptake inhibitors are more appropriate.
An accurate nosological diagnosis for dementia is based on a thorough analysis of anamnestic, clinical and neuropsychological data, as well as neuroimaging data. To select the optimal treatment, both the nosological affiliation and the severity of dementia, the presence of emotional disorders and other features of the case are important.
For mild or moderate dementia in AD and DLB, acetylcholinesterase inhibitors
. Today, there is the largest evidence base regarding the effectiveness of drugs in this group. Acetylcholinesterase inhibitors are effective both against memory impairment and other cognitive functions, and against neuropsychiatric symptoms such as sleep disturbances, hallucinations and delusions. The constant use of drugs of this pharmacological group contributes to a significant increase in the length of time of relative functional independence of patients with asthma. The widespread use of these drugs is somewhat limited by dyspeptic side effects associated with excessive cholinergic activity. In the presence of depression, these drugs can aggravate its manifestations [1,3,7,21,24,25,28,30,42,44,45,53].
Recent controlled studies in North America, Europe, and Southeast Asia suggest that the peptidergic drug cerebrolysin
, when administered intravenously in a dose of at least 30 ml, 20 infusions per course, has a beneficial effect on cognitive functions, possibly not inferior to the effect of acetylcholinergic drugs. The advantageous aspects of using Cerebrolysin include its effectiveness not only in neurodegenerative but also in vascular dementia, good tolerability, and a possible neuroprotective effect [2,5,15,22,34,51].
Glutamatergic drug memantine
has a beneficial effect on cognitive functions in AD, as well as in vascular and mixed dementia. According to some data, the symptomatic effect of memantine is more pronounced in more advanced stages of dementia. The neuroprotective effect of the drug is also discussed, associated with a decrease in glutamate-mediated excitotoxicity in relation to acetylcholinergic neurons [50,52].
Standardized preparation of Ginkgo extract (Tanakan)
, with its constant use, contributes to a slower progression of the neurodegenerative process due to its antioxidant properties, the ability to activate the metabolism of brain neurons, improve the rheological properties of blood and microcirculation. The main active ingredients of Tanakan are flavonoid glycosides, terpene substances (ginkgolides A, B, C, bilobalide) and proanthocyanidins. These substances have a multidirectional positive effect on the processes of free radical oxidation, tissue metabolism and microcirculation. Under experimental conditions, it was shown that Tanakan affects neurotransmitter processes in the central nervous system. This is demonstrated by its ability to enhance the release of neurotransmitters from presynaptic nerve terminals, inhibit the reuptake of biogenic amines, and enhance the sensitivity of postsynaptic muscarinic receptors to acetylcholine. All of the above determines the advisability of using Tanakan in the complex treatment of memory and attention disorders in elderly patients [6, 23].
At the stage of mild cognitive disorders that do not reach the stage of dementia, an accurate nosological diagnosis is not always possible due to the insignificance of neuropsychological symptoms, sometimes only the subjective nature of the disorders. Often, in order to verify the pathological nature of the disorders and clearly determine the nosological affiliation of the case, long-term observation of the patient is necessary. However, the lack of complete confidence in the pathological nature of the disorders and in a specific diagnosis should not be a reason for the doctor’s inaction, since it is at the stage of mild cognitive impairment that pathogenetic therapy has the greatest chance of success.
In addition to the correction of dysmetabolic disorders, treatment of vascular diseases of the brain and depression, for mild cognitive impairment it is advisable to use multimodal drugs that are effective in both degenerative and vascular diseases of the brain and have neuroprotective properties. Today there is positive experience in conducting repeated courses of intravenous infusions of Cerebrolysin
(30–60 ml per 200 ml of saline intravenously, 20 infusions per course, 2 courses per year) and many months (possibly many years) of taking
Tanakan
(40–80 mg three times a day) [6,15].
The question of the advisability of memory training in old age is very controversial. To date, there is no evidence that memory training can prevent or slow the progression of neurodegenerative or vascular disease of the brain. However, with the stationary nature of the disorders, teaching the patient to use certain memorization strategies and increasing the level of attention undoubtedly helps to increase the effectiveness of mnestic activity.
Thus, memory impairment in old age is one of the most pressing medical and social problems.
The use of modern diagnostic methods and pharmacotherapy can significantly improve the quality of life of elderly people with cognitive disorders, extend the time of functional independence, and reduce the economic and social burden that falls on patients’ relatives and society as a whole. Literature:
1. Bukatina E.E., Grigorieva I.V., Sokolchik E.I. Efficacy of amiridine in the early stages of Alzheimer's disease. //J.neuropathol. and a psychiatrist. –1991. –T.91., No. 9. –P.53–58.
2. Vereshchagin N.V., Lebedeva N.V. Mild forms of multi-infarct dementia: the effectiveness of Cerebrolysin. //Sov.Med. –1991. –No.11. –P.6–8.
3. Groppa S.V. Drug correction of Alzheimer's disease. // Journal of Neuropathology and Psychiatry. –1991. –T.91. –No. 9. –P.110–116.
4. Damulin I.V., Yakhno N.N. Cerebrovascular insufficiency in elderly and senile patients (clinical computed tomography study). // Journal of Neuropathology and Psychiatry. –1993. –T.93. –N.2. –P.10–13.
5. Zakharov V.V., Damulin I.V. Diagnosis and treatment of cognitive impairment in the elderly. //Guidelines. Edited by N.N. Yakhno. –Moscow: MMA im. I.M. Sechenov. –2000.
6. Zakharov V.V. Application of tanakan in neurogeriatric practice. // Neurological journal. –1997. –T.5. –P.42–49.
7. Zakharov V.V., Damulin I.V., Yakhno N.N. Drug therapy for dementia. //Clinical pharmacology and therapy. –1994. –T.3. –No. 4. –S. 69–75.
8. Luria A.R. Higher cortical functions of humans. //Moscow: Moscow State University Publishing House. –1969.
9. Luria A.R. Fundamentals of neuropsychology. //Moscow: Moscow State University Publishing House. –1973.
10. Luria A.R. Neuropsychology of memory. Memory impairment due to local brain lesions. //Moscow: Pedagogy. –1974.
11. Luria A.R. Neuropsychology of memory. Memory impairment in deep-seated brain lesions. //Moscow: Pedagogy. –1976.
12. International statistical classification of diseases and health-related problems. Tenth revision. (ICD-10). //–Geneva, WHO. –1995.
13. Shmidt E.V. Classification of vascular lesions of the brain and spinal cord. //AND. Neuropathology and Psychiatry. –1985. –T.85. –pp.192–203.
14. Yakhno N.N., Levin O.S., Damulin I.V. Comparison of clinical and MRI data in dyscirculatory encephalopathy. Message 2: cognitive impairment. //Nevrol.zhur. –2001. –T.6, No. 3. –P.10–19.
15. Yakhno N.N., I.V.Damulin, V.V.Zakharov, O.S.Levin, M.N.Elkin. Experience with the use of high doses of Cerebrolysin in vascular dementia. // Ter Archive. –1996. –T.68. –No. 10. –P.65–69.
16. Yakhno N.N. Current issues in neurogeriatrics. //On Sat. N.N. Yakhno, I.V. Damulin (eds.): Advances in neurogeriatrics. -Moscow. –1995. –Part 1. –P.9–29.
17. Yakhno N.N., Damulin I.V., Bibikov L.G. Chronic cerebrovascular insufficiency in the elderly: Clinical and computed tomographic comparisons. //Clinical gerontology. –1995. –N.1. –P.32–36.
18. Albert ML Subcortical dementia. In: Alzheimer's disease: Senile Dementia and Related Disorders. –New York, Raven Press, 1978, V.7, pp. 173–180.
19. Amaducci L., L. Andrea. The epidemiology of the dementia in Europe.//In A. Culebras, J. Matias Cuiu, G. Roman (eds): New concepts in vascular dementia. –Barseleona: Prouse Science Publissher. –1993. –P.19–27.
20. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. –Washington: American Psychiatric Association. –1994.
21. Anand R., Hartman R., Gharabawi G. Worldwide clinical experience with Exelon, a new generation of cholinesterase inhibitor in the treatment of Alzheimer's disease. //Eur J Neurol. –1997. –Vol.4, Suppl.1.–PS37.
22. Bae CY, Cho CY, Cho K. Et al. A double–blind placebo controlled, multicenter study of Cerebrolysin in Alzheimer's disease. //J Am Geriatr Soc. –2000. –Vol.48. –P.1566–1571.
23. Bars P., Katz M., Berman N., Itil T., Freedman A., Schatzberg A. A placebo-controlled, double-blind, randomized trial of an extract of ginkgo biloba for dementia. // JAMA. – 1997. –Vol.278, N.16. –P.1327–1332.
24. Bartus RT Drug to treat age related neurodegenerative problems. //J Am Ger Soc. –1990. –V.38. –P.680–695.
25. Beatty WW, N. Butters, DS Janowsky. Patterns of memory failure after scopolamine treatment: implication for cholinergic hypotesis of dementia. //Behav Neural Biol. –1986. –V.45. –P.196–211.
26. Becker JT, FJHuff, RDNebes et al. Neuropsychological function in Alzheimer's disease: pattern of impairment and rates of progression. //Arch Neurol. –1988. –V.45. –No. 3. –P.263–268.
27. Bushke H, E.Grober. Genuine memory deficit in age associated memory impaiment. //Dev Neuropsychol. –1986. –V. 2. –P.287–307.
28. Chrisensen, N. Malty, AFLorn et al. Cholinergic 'blockade' as a model of the cognitive deficit in Alheimer's disease. //Brain. –1992. –V.115. –P.1681–99.
29. Ciocon JO, JFPotter. Age–related changes in human memory: normal and abnormal. //Normal and Abnormal Geriatrics. –1988. –V.43. –N.10.–P.43–48.
30. Claus JJ, C. Ludvig, E. Mohr et al. Nootropic druds in Alzheimer's disease. //Neurology. –1991. –V.41. –P. 570–574.
31. Crook TH, R. Bartus, S. Ferris et al. Age Associated memory impairment. Proposed diagnostic criteria and measures of clinical change. //Dev Neuropsychol. –1986. –V.2. –P.261–276.
32. Cummings JL Subcortical dementia. //New York: Oxford Press. –1990.
33. Сurran HV Benzodiazepines, memory and mood: a review. //Psychopharmacology. –1991. –V. 105. –P.1–8.
34. Gauthier S. Results of a 6–month randomized placebo–controlled study with Cerebrolysin in Alzheimer's disease. //Eur J Neurol. –1999. –Vol.6, suppl.3. –P.28.
35. Grober E., H. Buschke. Genuine memory deficit in dementia. //Dev Neuropsychol. –1987. –V.3. –P.13–36.
36. Grober E., H. Buschke, H. Crystal et al. Screening for dementia by memory testing. //Neurology. –1988. –V.38. –P.900–903.
37. Folstein MF, SEFolstein, PRMcHugh. Mini–Mental State: a practical guide for grading the mental state of patients for the clinician. // J Psych Res. –1975. –V.12. –P.189–198.
38. Hershey LA, Olszewski WA Ischemic vascular dementia. //In: Handbook of Demented Illnesses. Ed. by JCMorris. –New York etc.: Marcel Dekker, Inc. –1994. –P.335–351
39. Huppert FA, MDKopellman. Rates of forgetting in normal aging: a comparison with dementia. //Neuropsychology. –1989. –V.27. –No. 6. –P.849–60.
40. Iqbal K., B. Winblad, T. Nishumura, N. Takeda, H. Wishewski (eds). Alzheimer's disease: biology, diagnosis and therapeutics. //J.Willey and sons ltd. –1997.
41. Karlsson T., L. Backman, A. Herlitz et al. Memory improvement at different stages of AD. //Neuropsychol. –1989. –V. 27. –No. 5. –P.737–42.
42. Kopelman MDand THCorn. Cholinergic 'blockade'as a model for cholinergic depletion. //Brain. –1988. –V.111. –P.1079 – 1110.
43. Kopelman MD Amnesia: organic and psychogenic. //Br J Psych. –1987. –V.150. –P.428–442.
44. Kopelman MD The cholinergic neurotransmitter system in human memory and dementia: a review. //Quart J Exp Psychol. –1986. –V.38. –P.535–573.
45. Kumor V., M. Kalach. Treatment of Alzheimer's disease with cholinergic drugs. //Int J Clin Pharm Ther Toxicol. –1991. –V.29. –No. 1. –P.23–37.
46. Lezak MD Neuropsychology assessment. //NY University Press. –1983. –P.768.
47. Lovenstone S., Gauthier S. Management of dementia. London: Martin Dunitz, 2001.
48. McKahn G., D. Drachman, M. Folstein et al. Clinical diagnosis of Alzheimer's disease: Report of NINCDS ADRDA Working group under the audits of the Department of Health and Human Services Task Force on Alzheimer's disease. //Neurology. –1984. –V.34. –P.939–944.
49. Perry R., I. McKeith, E. Perry. Dementia with Lewy bodies. clinical, pathological and treatment issues. //Cambridge University Press. –1996. –P.510.
50. Reisberg B., Windscheif U., Ferris S. et al. Memantine in moderately severe to severe Alzheimer's disease: results of placebo–controlled 6 month trial. //Neurobiol Aging. –2000. –Vol.21. –P.S275.
51. Ruther E., Ritter R., Apecechea M. et al. Sustained improvement in patients with dementia of Alzheimer's type (DAT) 6 months after termination of Cerebrolysin therapy. //J Neural Transm. –2000. –V.107. –P.815–829.
52. Sahin K., Stoeffler A., Fortuna P. Et al. Dementia severity and the magnitude of cognitive benefit by memantine treatment. A subgroup analysis of two placebo–controlled clinical trials in vascular dementia. //Neurobiol.Aging. –2000. –Vol.21.–P.S27.
53. Sarter M. Taking stock of cognitive enhancers. //Trends Pharm Sci. –1991. –V.12. –No. 12. –P.456–461.
54. Wilson RS, AWKasniak, JHFox. Remote memory in senile dementia. //Cortex. –1981. –V.17. –P.41–48.
Home treatment and prevention
If a person does not have a serious condition, they can be treated at home in the comfort and peace of mind. The therapeutic course includes taking medications, performing useful exercises and medical recommendations.
To improve your health, you must comply with the following conditions:
• Sleep at least 8-9 hours a day. An additional 1-2 hour nap during the day is also recommended. • Maintain good communication with loved ones: relatives, friends, neighbors. • Avoid conflicts and stressful situations, create a calm, friendly atmosphere at home. • Stop smoking and drinking alcohol. • Eat harmoniously and nutritiously. • Walk outdoors every day. • Involve the elderly relative in family and household affairs.
Recommendations for people with memory loss
• Twice a year you need to undergo a medical examination to monitor the person’s condition. • Every year it is useful to go to a sanatorium or resort to improve the general condition and health of the nervous system. • Maintain a logical connection between the past, present and future. To avoid memory lapses, you need to talk to a person about his biography in order to maintain a healthy memory. • Keep a diary in which to record the events of the day. This will help to record facts and restore memories if they are lost. • Discuss different topics: a movie watched, a book read, events experienced. • Do drawing or music. • Walk outdoors every day. • Maintain mental work, learn new things.
Thanks to the active work of the brain, the connection between cells is strengthened, thanks to which a person maintains sanity and good thinking for a long time.
To maintain healthy memory, you need to lead an active lifestyle. Proper nutrition, walks in the fresh air, and suitable physical activity are necessary. Bad habits need to be abandoned.
To maintain strong memory for many years, older people need to monitor their overall health. Diseases affect the quality of memory. It is necessary to control sugar and cholesterol levels, and treat chronic diseases.
It is necessary to maintain brain health through intellectual activities: reading, learning new things, solving puzzles, being creative, developing in any area.
Tips from medical experts for preserving memory:
• Maintain healthy cholesterol levels. If left unchecked, memory problems may develop in old age. • Take a course of ginkgo biloba extract (40 mg) - this will improve memory. • Include foods with natural antioxidants in your diet - they will prevent the weakening of brain activity. • Contact a psychologist when you discover the first problems with memory.
Memory training in old age
To train your memory, it is important to be aware of the memory characteristics of older people. Pensioners have better developed logical, rather than figurative, memory, so information that a person actively thinks to remember, he assimilates and remembers better. Repeating new information many times will also help you remember something new. It is easier for a person to remember what makes sense to him.
To improve memory in an elderly person, it is useful to follow these recommendations:
• Be physically active. Suitable physical activity will support healthy memory. • Drawing with both hands. On a sheet of paper, try to simultaneously draw the same objects with both hands, for example, two squares, circles, triangles. Next, you can choose more complex shapes: flowers, trees, clouds. The hardest thing is to depict different objects at the same time. This exercise will train both hemispheres of the brain. • Write a summary of the text, as in your school years. You can use a short read text, radio or television news. Express the main meaning, retain more facts and precise details, maintain the style of the narrative. • Remember the last person you saw, his appearance in great detail. • Learn poetry by heart. • Perform usual actions differently. Brush your teeth with the other hand, go to the store a different way, etc. • Memorize lists. Lists can be anything: thematic and consisting of different words, everyday ones (for example, shopping in a store or a to-do list for the week). You can learn a foreign language by making lists to memorize. • Learn to play a musical instrument. • Activities to develop fine motor skills of the fingers: rotating small objects between the fingers, knitting, modeling and others. • Solve puzzles, crosswords and riddles. You can work with any information, learn foreign languages. • Take regular breaks from work for rest, for example, changing activities from mental to physical (walking, exercising, cleaning). • Keep a diary. Such an organizer will not only make the work of the brain easier, but will also help train your memory by recording notes. • Read more. This will train motor and visual memory and develop thinking. It is useful to retell what you read and analyze the work. • Train attention to detail. Remember down to the smallest detail what this or that object, person, place looks like. • Develop a positive outlook on life.
Each memory problem in old age is an individual case that requires professional study. Relatives of an elderly person need to remember the signs of amnesia in order to be able to recognize the onset of the disease in time. If you suspect a disease, you need to take the person to a specialist. Treatment is necessary in any case; self-medication is not allowed.
To strengthen and improve memory in old age, you need to follow useful recommendations, lead a healthy lifestyle, and maintain mental and physical activity. In this way, you can preserve a strong and good memory for many years.
Memory impairments in old age: modern possibilities of prevention and therapy
The medical and social significance of cognitive impairment is beyond doubt. Impairments in memory and other cognitive functions significantly reduce the quality of life of patients, negatively affect professional activity, reduce the ability to learn, acquire new knowledge and skills, and cause reactive emotional disorders. Severe cognitive impairment (CI) also has a negative impact on the quality of life of relatives, often forcing them to change their usual way of life, and in some cases to stop or reduce their professional activities. The economic losses of society associated with the pathology under discussion are very noticeable, especially increasing during the transition to the stage of moderate and severe dementia [9]. It should be recognized that the problem of prevention and treatment of cognitive impairment in old age is still very far from being resolved. However, at the end of the 20th and beginning of the 21st centuries, new scientific knowledge was gained about the pathophysiology and neurochemistry of the main dementing diseases, which made it possible to optimize therapeutic approaches. Today, the effectiveness of symptomatic treatment of dementia in old age is considered fully proven. Approaches to the development of pathogenetic therapy for AD and other common diseases with dementia are being actively developed. The epidemiological data accumulated to date make it possible to determine optimal approaches to the primary and secondary prevention of cognitive impairment: correction of known risk factors for memory and attention impairment in old age [1,2,11,24,26,30]. Risk factors for cognitive impairment The strongest and most independent risk factor for cognitive impairment is advanced age. With age, the brain undergoes a number of regular changes that make it more vulnerable to various pathological influences. Thus, with age, brain mass and the number of synapses decrease, and the activity of dopaminergic, noradrenergic, acetylcholinergic and other neurotransmitter systems changes. These involutional changes ultimately reduce neuronal plasticity. The latter term is usually understood as the ability of neurons to change functional properties in response to external influences. A decrease in neuronal plasticity leads to a decrease in the compensatory capabilities of the brain (the so-called “cerebral reserve”) [1,2,8,10,11]. Another risk factor for the development of cognitive impairment, which, like age, cannot be corrected, is genetic burden. The most common cause of dementia, AD, is a genetically determined disease. The risk of developing asthma is especially high if you have close relatives who become ill before the age of 60 (presenile form). AD with such an early onset is characterized by an autosomal dominant type of transmission and high penetrance of pathological genes. Asthma with onset after age 60 is usually sporadic. Nevertheless, the risk of illness in the immediate relatives of such patients is higher than the statistical average [1,2,11]. The most important risk factor for cognitive impairment is diseases of the cardiovascular system, especially arterial hypertension. Based on data from large population-based studies conducted independently in different regions of the world, the consensus was that the presence of hypertension in middle age is associated with an increased risk of developing memory impairment in old age. Moreover, there is a statistical connection not only with vascular cognitive impairment, but also with the risk of developing AD. Possible mechanisms by which arterial hypertension provokes the occurrence or clinical manifestation of asthma are currently being clarified. Most likely, decompensation of a subclinically occurring degenerative process as a result of lacunar infarctions and/or progression of leukoaraiosis is of decisive importance [7,15,43,46]. It has recently been shown that type 2 diabetes also significantly increases the risk of developing cognitive impairment. According to the Rotterdam study, the risk of developing dementia, and specifically AD, is approximately 2 times higher in patients with type 2 diabetes compared to their peers. At the same time, patients receiving insulin have the greatest risk, which is more than 4 times higher than the statistical average. Similar data were obtained from the Canadian study of health and aging. According to the LADIS study (European study of the relationship between leukoaraiosis and disability - leucoaraiosis and disability study), there is a statistical connection between diabetes mellitus and a characteristic marker of the neurodegenerative process - atrophy of the medial temporal lobes of the brain [5,6,25,34]. Hyperlipidemia and abdominal obesity in midlife also increase the risk of developing cognitive impairment with aging. It is natural that the maximum risk is observed with a combination of arterial hypertension, hyperlipidemia, abdominal obesity and type 2 diabetes mellitus, which is often observed in patients with the so-called “metabolic syndrome” [11,15,34]. Proven risk factors for cognitive impairment in old age also include traumatic brain injury and a history of episodes of depression, female gender, deficiency of B vitamins and folic acid, low intellectual and physical activity in young and middle years of life (Table 1) [1 ,2,11,30]. Non-drug methods for preventing cognitive impairment Non-drug methods for preventing cognitive impairment include a diet enriched with natural antioxidants, systematic training of memory and attention, and rational physical exercise. Natural antioxidants are vitamins C and E, which are found in citrus fruits, vegetable oils, seafood and other foods. According to some retrospective observations, the so-called “Mediterranean diet”, enriched with natural antioxidants, helps prevent CI and dementia. For this purpose, it is recommended to use more vegetables, fruits and seafood in the diet [40,47]. Epidemiological studies indicate that people with intense intellectual work are less susceptible to CI and dementia. Patients with a high intellectual level have more developed cognitive skills, which allow them to more successfully overcome the difficulties that appear at the onset of dementing brain disease. Thus, a high intellectual level in the premorbid provides a greater or lesser delay in the time of clinical manifestation of the disease [14,31,48]. Systematic exercises to train memory and attention are recommended for both healthy elderly people and people with mild cognitive impairment. The feasibility of such exercises is based on the idea of cognitive functions as a store of knowledge and skills that are formed during life. In other words, a person in the process of life learns strategies and skills for perceiving, processing, remembering and reproducing information. Human memory is not a simple “repository” where information is stored, and the effectiveness of mnestic activity depends not on the volume of memory, which is unlimited and changes little even with severe brain damage, but on the memorization and reproduction strategies used [3,11,30]. Memory training programs include increasing the patient’s motivation to remember and reproduce, teaching effective memorization strategies (so-called “mnemonic techniques”), developing the ability to maintain an appropriate level of attention for a long time, actively including emotional support (as is known, emotionally charged information is remembered better) and imagination. The effectiveness of systematic training of memory and attention has been proven in patients with mild dementia, as well as in non-dementia (mild and moderate) cognitive impairment [33,36,44]. Epidemiological observations indicate that regular physical activity also helps reduce the incidence of dementia. A number of studies have shown that people who exercise regularly have a lower risk of developing dementia in old age. Probably, this phenomenon is based on the beneficial effect of a physically active lifestyle on the cardiovascular system, body mass index, and emotional sphere [12,13,27,38]. Treatment of cardiovascular diseases and prevention of CI As mentioned above, arterial hypertension and hyperlipidemia are proven risk factors for CI, both of vascular and degenerative nature. In this regard, the question of what effect timely and adequate therapy of these pathological conditions has on the risk of developing CI is widely discussed in the literature. Some large randomized international trials of various antihypertensive agents have analyzed the incidence of dementia or the rate of progression of cognitive impairment as additional indicators of safety and effectiveness (Table 2). A preventive effect against the progression of cognitive impairment and the onset of dementia was shown with the calcium blocker nitrendipine, the angiotensin type II receptor blocker eprosartan, and with the use of a combination of perindopril and indapamide. Other antihypertensive drugs did not have a significant effect on the incidence of dementia or the rate of progression of cognitive impairment [17,29,35,39,41,43,49]. It should be noted that the preventive effect of antihypertensive drugs can be discussed only if there is no increase in daily blood pressure variability during the therapy. Significant fluctuations in blood pressure during the day, associated with irregular or incorrect medication use or orthostasis, significantly increase the risk of ischemic brain damage. In addition, it is important to emphasize that normalization of blood pressure should be achieved systematically and gradually. Long-term arterial hypertension leads to changes in the reactivity of cerebral vessels and disruption of the mechanisms of autoregulation of cerebral blood flow. Under these conditions, a rapid decrease in the patient’s usual blood pressure numbers can lead to worsening cerebral hypoperfusion, the occurrence of acute cerebrovascular accidents and chronic cerebral ischemia. A pronounced and rapid decrease in blood pressure in the presence of hemodynamically significant atherosclerosis of the main arteries of the head is especially dangerous [7,43]. The prospects for using statins to prevent cognitive impairment in old age are of great interest. In recent years, it has been established that the accumulation of cholesterol has a pathogenetic significance not only in the formation of atherosclerosis of large arteries, but also in the process of formation of senile plaques in the brain parenchyma, characteristic of AD. However, the number of studies on the putative preventive effect of statins on CI progression is limited. Their results to date are contradictory [20,37,42]. Vasoactive and neurometabolic therapy. As is known, drugs that improve cerebral microcirculation and neuronal metabolism are the most frequently prescribed in neurological practice in our country, especially in elderly patients. With the use of these drugs, there is an improvement in memory, attention and other cognitive functions, especially in patients with cerebrovascular pathology, an improvement in the emotional state and well-being [1–3,11]. The likely neuroprotective effects of vasoactive and neurometabolic drugs are widely discussed. Thus, numerous experimental and clinical studies were devoted to the study of the neuroprotective effect of EGB 761 (Memoplant), an extract of relict Ginkgo biloba leaves, standardized for the content of active substances (flavonoid glycosides, ginkgolides, bilobalides). It has been shown that the active ingredients of the drug Memoplant normalize the tone of microcirculatory vessels, having a greater effect on the affected arterioles and without causing a steal effect. Other active substances of EGb 761 - ginkgolides - acting on the neuronal membrane of blood cells, reduce the aggregation of platelets and erythrocytes. Thus, Memoplant improves the rheological properties of blood, prevents thrombus formation and the release of mediators that increase smooth muscle tone [19,23]. The vasoactive and antioxidant effects of the drug Memoplant provide grounds for its use in elderly patients to prevent the onset or progression of cognitive disorders. The effectiveness of EGb 761 was studied in one of the world's largest studies on the prevention of cognitive impairment (Oregon Study), the results of which were published in 2008. In this study, 118 elderly people over 85 years of age were followed for 3 years. The condition for inclusion in the study was the absence of cognitive impairment at the baseline visit. It was shown that with placebo, the likelihood of developing cognitive disorders was greater than with active therapy. It should, however, be noted that the preventive effect was statistically significant only in those patients who followed the prescribed dosage regimen of the drug for the required time [16]. The effectiveness of Memoplant in already developed cognitive disorders was also assessed in a number of international randomized studies, which involved a total of about 2000 patients with asthma or cerebrovascular diseases. It has been shown that with the use of 120–240 mg/day. of this drug for at least 6 months. there is a decrease in the severity of cognitive disorders, improvement in the behavior of patients with dementia of various etiologies, and an increase in their independence in everyday life (Table 3, Fig. 1). It should be emphasized that, taking into account the cited studies, higher doses of the drug (240 mg) are preferable than previously accepted [21,22,28,32,45]. Acetylcholinergic and glutamatergic therapy. According to the generally accepted international standard, drugs with neurotransmitter action are of priority at the stage of dementia. Since the 70–80s. In the 20th century, it was convincingly shown that a decrease in the synthesis and activity of acetylcholine is a key neurochemical defect in AD. Subsequently, it was found that the subcortical arteriolosclerotic form of vascular dementia, dementia with Lewy bodies and Parkinson's disease are characterized by very similar neurotransmitter changes. All this served as the basis for the initiation of the use of acetylcholinesterase inhibitors (tetraaminoacridine, ipidacrine, donepizil, rivastigmine, galantamine) for dementia in old age. Currently, the symptomatic effect of these drugs at the stage of mild and moderate dementia has been fully proven both by randomized studies and everyday clinical practice. The likely ability of acetylcholinergic therapy to slow down the progression of the degenerative process in AD is also discussed. At the same time, studies of the effectiveness of acetylcholinesterase inhibitors at the stage of non-dementia (moderate) cognitive impairment have led to conflicting results [1,2,11,24,26,30]. Another generally accepted therapeutic approach to dementia is the use of the reversible NMDA glutamate receptor blocker memantine. Experimental data indicate that both the neurodegenerative process and chronic ischemia and hypoxia are accompanied by an increase in the activity of the glutamatergic system, which is one of the important mechanisms of neuronal damage. In addition, activation of the glutamatergic system occurs during the process of consolidating the memory trace when memorizing new information. In dementing diseases, excessive activation of the glutamatergic system disrupts this process, and its decrease during the use of memantine helps restore the normal pattern of assimilation of new information. The clinical effectiveness of memantine is considered proven in moderate to severe dementia. According to some data, including our own experience, memantine may also be effective in the stages of mild dementia and non-dementia (moderate cognitive impairment) [1,2,11,24,30]. Treatment of concomitant diseases and correction of emotional state. Comorbidity in older age is widespread, and most older adults have multiple chronic conditions. Many somatic diseases and exogenous intoxications cause or aggravate cognitive impairment in elderly people due to systemic metabolic disorders. Therefore, when developing a strategy for conducting elderly patients with cognitive disorders, attention should be paid to concomitant somatic pathology, the presence of chronic alcohol, drug or other intoxication. The most adverse effect on cognitive functions is have hypothyroidism, B12 -deficiency, liver and kidney diseases, chronic obstructive lung diseases, chronic heart failure, prolonged use of psychoactive drugs. In all cases, for the first time diagnosed cognitive disorders, laboratory screening of common metabolic disorders should be carried out [11,30]. Very often, cognitive disorders in old age are combined with emotional disorders of the anxious -depressive series. At the same time, the relationship between cognitive and emotional disorders can have a causal or parallel character. So, it is known that severe depression can cause cognitive impaired frontal nature. On the other hand, the beginning dementrating process is often accompanied by anxiety -depressive disorders as an emotional reaction to the disease with relatively intelligent criticism. Finally, often cognitive and emotional disorders are not connected by causal relationships, but are united by a common psychophysiological substrate, which is observed, for example, with dysfunction of the frontal lobes of the brain. In any case, the presence of emotional disorders requires pharmacological correction. In this case, antidepressants with a cholinolytic effect should be avoided [11,30]. Thus, at present, there are developed therapeutic approaches to patients with cognitive disorders at all stages of the pathological process. In elderly persons without cognitive disorders, the prevention of their occurrence is proper and timely treatment of cardiovascular diseases, systematic intellectual exercises, rational nutrition and physical activity. With cognitive disorders that do not reach the severity of dementia, it is advisable to conduct vasoactive and neurometabolic therapy. In patients with dementia, the first choice preparations are acetylcholinerase and memantine inhibitors. At all stages of cognitive insufficiency, the treatment of related somatic diseases and the correction of the emotional state are relevant.
Literature 1. Gavrilova S.I. Pharmacotherapy of Alzheimer's disease // Moscow: Pulse Publishing House, 2003. –115 P. 2. Damulin I.V. Alzheimer's disease and vascular dementia // Ed. N.N. Yakhno. – M., 2002. – P.85. 3. Zakharov V.V., Yakhno N.N. Memory impairments // Moscow: GeotarMed. – 2003. – 110 P. 4. Zakharov V.V. All-Russian research program for epidemiology and therapy of cognitive disorders in old age (“Prometheus”) // Neurological Journal. –2006. – T.11. – P.27–32. 5. Zakharov V.V., Sosina V.B. Cognitive impairment in patients with diabetes // Neurological Journal. – 2009. – T.14. No. 4. – pp. 54–58. 6. Sosina V.B., Zakharov V.V., Yakhno N.N. Non-dementia cognitive impairment in patients with type 2 diabetes // Neurological Journal. – 2010. – T.15, No.4. –P.25–30. 7. Starchina Yu.A., Parfenov V.A., Chazova I.E., Pustovitova T.S., Yakhno N.N. Cognitive disorders in patients with arterial hypertension // Journal of Neurology and Psychiatry named after. S.S. Korsakov. – 2008. – No. 4. – P.19–23. 8. Yakhno N. N., Lavrov A. Yu. Changes in the central nervous system during aging // Neurodegenerative diseases and aging (Guide for doctors) / Ed. I. A. Zavalishina, N. N. Yakhno, S. I. Gavrilova. – M., 2001. – P. 242 – 261. 9. Yakhno N.N. Cognitive disorders in a neurological clinic. //Neurological journal. – 2006. – T.11. – Appendix No. 1. – P. 4–12. 10. Yakhno N.N., Zakharov V.V., Lokshina A.B. Impaired memory and attention in old age // Journal of Neurology and Psychiatry named after. S.S. Korsakov. – 2006. – T.106. – No. 2. – P.58–62. 11. Yakhno N.N., Zakharov V.V., Lokshina A.B., Koberskaya N.N., Mkhitaryan E.A. Dementia. Practical guide for doctors // M.: MEDpress-inform, 2010. – 272 P. 12. Abbott RD, White RD, Ross GW et al. Walking and dementia in physically capable elderly men //JAMA. –2004. –Vol.292. – No.12. – P.1447–1453. 13. Colcombe SJ, Erickson KI, Raz N. et al. Aerobic fitness reduces brain tissue loss in aging humans // J. Gerontol. A. Biol. Sci. Med. Sci. – 2006. –Vol.61. –N. –P.1166–1170. 14. Dartigues JF, Gagnon M, Letenneur L et al. Principal lifi–time occupation and cognitive impairment in French elderly cohort (PAQUID) //Am. J. Epidemiol. –1992. –Vol.135. –N.9. –P.981–988. 15. DiCarlo A., Baldereschi M., Amaducci L. Et al. Cognitive impairment without dementia in older people: prevalence, vascular risk factors, impact on disability. The Italian Longitudinal Study on Aging // J. Am. Ger. Soc. –2000. –Vol.48. – P.775–782. 16. Dodge HH, Zitzelberger T., Oken BS et al.. A randomized placebo–controlled trial of ginkgo biloba for the prevention of cognitive decline. // Neurol.– 2008.– Vol. 70.– P. 1809–1817. 17. Forette F., Seux M.L., Staessen J. et al. Prevention of dementia in randomized placebo–controlled systolic hypertension in Europe (SYS–EUR) trial // Lancet. –1998. –Vol. 352. – P.1347–1351. 18. Graham JE, Rockwood K, Beattie EL et al. Prevalence and severity of cognitive impairment with and without dementia in an elderly population // Lancet. –1997. –Vol. 349. –P.1793–1796. 19. Halama P. Was leistet der Spezialextrakt (Egb 761) //Therapiewoche. –1990. – Vol.40. – P. 3760–3765. 20. Heart Protection Study collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomized placebo-controlled trial // Lancet. –2002. –Vol.360. –P.7–22. 21. Ihl R., Bachinskaya N.Yu., Korczyn A. et al. Efficacy and safety of a once daily formulation of Gingko biloba extract (EGb 761) in dementia with neuropsychiatric features: a randomized controlled trial // Int. J. Ger. Psych. –2010. Epub ahead of print. 22. Kanowski S, Hoerr R. Ginkgo biloba extract EGb 761® in dementia: Intention-to-treat analysis of a 24-week, multi-center, double-blind, placebo-controlled, randomized trial. // Pharmacopsychiatry. – 2003. – Vol. 36.– P. 297–303. 23. Kleijnen J., Knipschild P. Ginkgo biloba // Lancet.–1992. – Vol.340 : Nov 7.–P.1136–1139. 24. Knopman DS Current treatment of mild cognitive impairment and Alzheimer's disease // Curr. Neurol. Neurosci Rep. –2006. –Vol.6. –N.5. – P.365–371. 25. Korf ES, van Straaten EC, de Leeuw FE et al. Diabetes mellitus, hypertension and medial temporal lobe atrophy: the LADIS study. // Diabet Med. – 2007.– Vol. 24(2).– P.166–171. 26. Kurshner HS Mild cognitive impairment: to treat or not to treat? //Curr. Neurol. Neurosci Rep. –2005. –Vol.5. –N.6. –P.455–457. 27. Laurin D., Verreault R., Linsay J. et al. Physical activity and risk of cognitive impairment and dementia in elderly persons //Arch. Neurol. –2001. –Vol.58. –N.3. –P.498–504. 28. Le Bars PL, Katz MM, Berman N. et al.. A placebo-controlled, double-blind, randomized trial of an extract of Ginkgo biloba for dementia. North American EGb Study Group // JAMA. – 1997. – Vol. 278.– P.1327–1332. 29. Lithel H., Hansson L., Skoog I. et al. The study on cognition and prognosis in the elderly (SCOPE): principal results of a randomized double blind intervention trial // J. Hypertention. –2003. –Vol.21. – P. 875–886. 30. Lovenstone S., Gauthier S. Management of dementia. – London: Martin Dunitz, 2001. 31. McDowell I., Xi G., Linsay J., Tierney M. Mapping the connection between education and dementia // J. Clin. Exp. Neuropsychol. –2007. –Vol.29. –N.2. –P.127–141. 32. Napryeyenko O., Borzenko I. Ginkgo biloba Special Extract in Dementia with Neuropsychiatric Features; A randomized, placebo-controlled, double-blind clinical trial // Drug research. – 2007. – Vol. 57(1). – P. 4–11. 33. Olazaran J., Muniz R., Reisberg B. et al. Benefit of cognitive–motor intervention in MCI and mild–to–moderate AD // Neurol. –2004. –Vol.63. –N.12. –P.2348–2353. 34. Ott A. et al. Association of diabetes mellitus and dementia: The Rotterdam Study// Diabetol.– 1996.– Vol. 39.– P.1392–1397. 35. Prince MJ, Bird AS, Blizard RA, Mann AH Is the cognitive function of older patients affected by anti–hypertensive treatment? Results from 54 months of the Medical Research Council's trial of hypertension in older adults //BMJ. –1992. –Vol.304. –P.405–412. 36. Rapp S., Brenes G., Marsh AP Memory enhancement training for older adults with mild cognitive impairment: a preliminary study //Aging and mental health. – 2002. –Vol.6. –N.1. –P.5–11. 37. Rockwood K., Kirkland S., Hogan DB Use of lipid-lowering agents, indication bias and the risk of dementia in community-dwelling elderly people //Arch. Neurol. – 2002. –Vol. 59. –P. 223–227. 38. Rovio S, Kareholt I, Helkala EL et al. Leisure–time physical activity at midlife and the risk of dementia and Alzheimer's disease // Lancet. Neurol. – 2005. –Vol. 4. – N.11. –P.705–711. 39. Scrader J., Luder S., Kulschevski A. et al. Morbidity and mortality after stroke – Eprosartan compared with nitrendipine for secondary prevention (MOSES) // Stroke. – 2005. –Vol. 36. –P. 1218–1226. 40. Scrameas N, Stern Y, Tang MX et al. Mediterranean diet and risk for Alzheimer's disease //Ann. Neurol. – 2006. – Vol. 59. – N.6. – P.877–879. 41. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the systolic hypertension in the elderly // JAMA. –1991. – Vol. 265. –P.3255–3264. 42. Shepherd J., Blauw G., Murphy M. et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomized placebo controlled trial //Lancet. – 2002. – Vol. 360. – P.1623–1630. 43. Skoog I., Gustafson D. Clinical trials for primary prevention in dementia // Dementia therapeutic research / K. Rockwood, S. Gauthier (eds). – London a New York: Taylor a Francis. – 2006. – P.189–212. 44. Smidt IW, Berg IG, Deelman BG Memory training for remembering names: initial results in the healthy elderly // Tijdchr. Gerontol. Geriatr. – 1997. –Vol. 28. – N.4. –P.155–162. 45. Schneider L., DeKosky S., Farlow M. et al. A randomized, double–blind, placebo–controlled trial of two doses of Ginkgo biloba extract in dementia of the Alzheimer's type // Curr. Alzheimer's Res. – 2005.– Vol. 2(5).– P. 541–551. 46. Snowdon DA, Greiner LH, Mortimer JA et al. Brain infarction and the clinical expression of Alzheimer's disease. The Nun Study // JAMA. –1997. –Vol. 277. – N.10. – P.813–817. 47. Solfrizzi V., Colacicco AM, D'Inttrono A. et al. Dietary intake of unsaturated fatty acids and age-related cognitive decline: an 8.5 year follow-up of the Italian Longitudinal Study on Aging // Neurobiol. Aging. – 2006. –Vol. 27. –N.11. – P.1694–1704. 48. Stern Y., Alexander GE, Prohovnik I., Mayex R. Inverse relationship between education and parietotemporal perfusion deficit in AD // Ann. Neurol. – Vol. 32. – N.3. – P.371–375. 49. Tzourio C., Andersen C., Chapman N. et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease //Arch. Intern. Med. – 2003. –Vol.163. – P.1069–1075.