Antidepressants help restore normal levels of chemicals in the brain that are involved in regulating sadness and anxiety. In people with depression who take antidepressants, the levels of neurotransmitters (hormones) in the brain normalize. When antidepressants, which affect the brain by affecting serotonin, are suddenly stopped, the body may respond by developing physical and emotional symptoms caused by the sudden absence of the increased serotonin levels that occur when taking the antidepressant.
These symptoms are not the same as physical withdrawal from the drug. Physiological withdrawal occurs when a patient takes a drug that can be addictive. However, the question “How to get off antidepressants” is asked by patients to a psychiatrist very often. In some cases, you can take antidepressants for the rest of your life, but their withdrawal is also possible, but this issue should be dealt with by a specialist. The patient must understand that it is possible to decide how much antidepressant to take only together with the attending physician. Psychiatrists at the Yusupov Hospital individually develop optimal timing and dosages for taking medications for each patient, allowing them to achieve the desired treatment effect while avoiding side effects.
Antidepressants are not addictive. The effect of antidepressant withdrawal is not related to addiction, but may reflect the physiological effects of stopping the drug in the same way as when a person with diabetes stops taking insulin. Almost one in five people who take antidepressants for six weeks or more may experience withdrawal symptoms if they suddenly stop taking the medication.
It is impossible to predict whether you will experience withdrawal symptoms after stopping an antidepressant. Scientists believe that suddenly stopping an antidepressant does not give the brain time to adjust to rapid changes in neurotransmitter levels. Therefore, you should not stop taking antidepressants.
All depression medications have the potential to cause unwanted symptoms, but some are much more likely to cause symptoms than others. Withdrawal symptoms are more likely to occur with antidepressants that remain in the body for a shorter period of time, especially those that affect both serotonin and norepinephrine.
You should not suddenly stop taking antidepressants, even if you feel better. Stopping antidepressants too early may cause depressive symptoms to return. If you need advice on taking or properly stopping antidepressants, or you have undesirable symptoms that have developed as a result of self-cessation of an antidepressant, and you urgently need advice from a psychiatrist, contact the Yusupov Hospital. You can make an appointment with a private psychiatrist at our clinic on the website.
The Yusupov Hospital employs doctors who have higher medical degrees.
education and specialization in psychiatry. Doctors at Yusupov Hospital
They regularly take advanced training courses and do internships in leading foreign psychiatric clinics.
When treating patients, doctors at the Yusupov Hospital use only new medications that have passed all studies and have proven effective in treating mental illnesses in the Russian Federation and have a minimal range of side effects.
Causes
Psychoactive substances include narcotic drugs, nicotine, alcohol, as well as some medications - antipsychotics, painkillers and sedatives. All these substances affect the functioning of the central nervous system and the human psyche. Medicines return the body to normal functioning and improve the general well-being of patients. Drugs, alcohol and nicotine change the psychophysical state, relax or, conversely, cause a surge of strength and energy. Under their influence, intoxication occurs - a special state of the body, characterized by causeless joy and high spirits. In acute poisoning with psychotropic drugs, signs of euphoria are replaced by symptoms of psychoneurological and vegetative-vascular disorders. These changes are associated with the effects of active compounds on hormonal, neurotransmitter and protein systems. Their long-term effects are addictive. The body functions that maintain its optimal state fade away. If the supply of a neurotropic substance is suddenly stopped, the body’s biological systems will not be able to restore the production of a natural analogue, and withdrawal syndrome will develop.
When a person uses psychoactive substances for a long time, it is difficult for him to take a break and quit them. His mood changes dramatically: joy and happiness disappear, psychological discomfort arises, reaching a mild degree of depression. The patient constantly has thoughts about the need for a new “dose”. These thoughts lift your spirits. This is how psychological dependence is formed - the body gets used to using substances that temporarily enhance physical or psychological activity. They become necessary to receive positive emotions.
In addition to psychological dependence, changes occur in the body at the cellular level. Chemical processes and metabolic reactions change, the functioning of all organs and systems is restructured, and the general condition worsens.
For withdrawal symptoms to develop, it is not enough to use a psychotropic substance once. It must be taken continuously over a certain period of time. Withdrawal symptoms occur when the intake of a substance is reduced or stopped. The dosage form of the pathology develops when a patient who feels an improvement independently interrupts the treatment course.
In persons with the syndrome, tolerance to a psychotropic substance increases, pathological dependence is formed, self-control is lost, and abstinence develops with personality degradation and exhaustion of the body.
Depending on the nature of the syndrome, the following forms are distinguished:
- Regenerative form - rapid and independent recovery of the body without medical assistance.
- Stable form - the satisfactory condition of patients is maintained with the help of medication.
- Intermittent form - exacerbations and remissions replace each other, patients need professional medical care.
- Degenerative form - patients are hospitalized in a hospital with severe manifestations that are extremely difficult to eliminate. The prognosis of the pathology is unfavorable, relapse is possible.
Prescribing antidepressants
Drugs in this group are more often used as maintenance therapy. The basis for treating anxiety and depression is communication with a psychologist. Antidepressants are represented by a wide variety of drugs, which are usually divided into several groups depending on the mechanism of their effect on the patient’s body:
- Monoamine oxidase inhibitors are further divided into two types. Non-selective drugs are first-generation drugs that are practically not used in medical practice today. They are difficult to combine with other medications and require a special diet to prevent side effects. High toxicity also causes refusal of their use. Selective monoamine oxidase inhibitors are more modern antidepressants. This group includes drugs such as Moclobemide and Selegiline. High dosages also require serious dietary adjustments.
- Selective neuronal reuptake inhibitors of various neurotransmitters, including serotonin, norepinephrine and dopamine. The principle of their operation is aimed at suppressing impulse transmission. This allows you to limit the pathological activity of the brain and reduce the harmful effects on other systems. The most modern and easily tolerated are drugs from the group of substances that affect serotonin. This includes drugs such as Paxil and Rexetine based on paroxetine, Sirlift, as well as Cipramil and Cipralex. The most widely used representative of serotonin reuptake inhibitors is Fluoxetine or Prozac.
- Monamine receptor agonists are another modern group of drugs that are well tolerated by patients and have a pronounced therapeutic effect. This type of antidepressant includes the drug "Remeron" based on mirtazapine.
- Non-selective inhibitors of neuronal monoamine reuptake are divided into several groups based on the similarities and differences in their chemical structure. They are represented by a wide range of medications, including Anafranil.
All these means are used in neurology and psychiatry to correct the cognitive functions and emotional state of the patient. They are also useful in the fight against withdrawal symptoms in alcoholism and drug addiction.
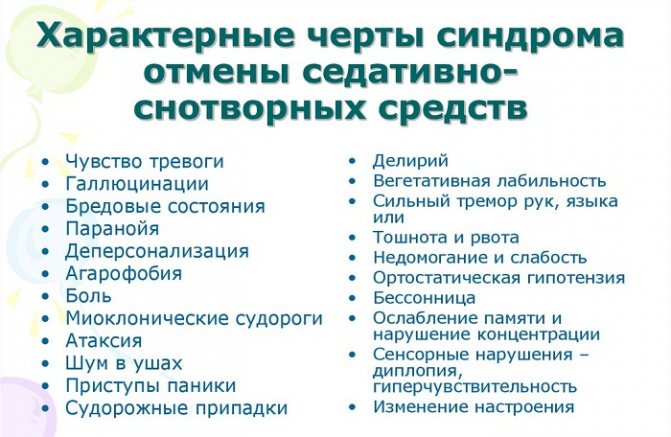
Symptoms

General clinical manifestations of pathology:
- Asthenization of the body - severe lethargy, causeless weakness, depression, decreased ability to work and concentration, insomnia, progressive apathy, loss of interest in hobbies and work, memory impairment, vestibular disorders, headache, periodic shortness of breath, pressure surges.
- Emotional disorders - irritability, tendency to depression, negative attitude towards current events, chronic fatigue, daytime sleepiness, shallow sleep at night, weak immunity, decreased libido, emotional dullness, negative thoughts. They are aimed at satisfying the desire to receive a new dose of a substance. This desire becomes paramount, displacing innate tendencies and aspirations - food and sexual instincts.
- Dyspeptic symptoms - nausea, vomiting, heaviness and pain in the epigastric region, discomfort after eating, dizziness, alternating constipation and diarrhea, rapid filling of the stomach with a small amount of food, flatulence, rumbling in the intestines, heartburn, belching, in children regurgitation after eating.
- Dysfunction of internal organs - tachycardia, shortness of breath, tremor, hyperhidrosis, hyper- or hypotension, stool disorders, dyspepsia, lower back pain, urination problems.
- Pain syndrome manifests itself as uncomfortable and painful sensations throughout the body. In this case, the pain does not have a specific localization. Patients with withdrawal syndrome often complain of periodic twitching of facial muscles, discomfort while walking, stabbing pain in the heart, which is accompanied by profuse night sweats, swelling and discoloration of the skin, paresthesia of the limbs during a painful attack, and muscle weakness.
Clinical manifestations of the pathology increase gradually and also gradually disappear. The severity of symptoms depends on the causative factor, that is, the type of addiction.
Manifestations of certain forms of pathology
Clinical manifestations of alcohol withdrawal syndrome occur three days after the start of binge drinking and reach their maximum by the 10th day of drinking alcohol. Patients have a disturbed mood, a feeling that something is missing, “everything is not right.”

The main manifestations of the disease include:
- insomnia,
- chronic fatigue,
- weakness,
- dry mouth,
- skin hyperemia,
- pressure fluctuations,
- headache,
- hyperhidrosis,
- dyspepsia,
- clouding of consciousness,
- trembling all over the body,
- ataxia,
- hallucinosis,
- anxiety, fear,
- violation of orientation in space,
- nightmares,
- depressive state
- aggression,
- guilt,
- melancholy and print,
- suicidal thoughts.
How dangerous
There are cases when a person has a hard time with drug withdrawal syndrome. In this regard, in the United States it has long been mandatory to write on all antidepressants that their use can lead to suicide. Relatives need to talk to the person suffering from depression and observe their behavior to identify the presence of suicidal thoughts.
It is necessary to urgently seek help from a doctor if the patient experiences:
- thoughts of suicide;
- worsening depression;
- anger, aggression;
- increased anxiety;
- insomnia;
- irritability;
- hyperactivity:
- sudden mood swings.
You can stop taking the drug only after consulting a doctor, who will tell you how to do it correctly, based on the characteristics of the prescribed drug. Antidepressant withdrawal syndrome is similar to a relapse of depression. The main difference is the duration and severity of symptoms. During an exacerbation of the disease, they are pronounced and do not go away on their own.
For most people, withdrawal symptoms are not dangerous at all. If you don't know what's going on, it can be alarming. But it rarely causes problems that you cannot live with for several weeks, which is what it takes for them to disappear.
There are very rare cases where serious problems arise due to the physical effects of stopping medication. You may also relapse and become depressed again. If this happens, the original disorder (depression) appears with an increased effect.
Diagnostic measures
Diagnosis of withdrawal syndrome is complex, consisting of a thorough and comprehensive examination of the patient. Specialists assess the general condition of patients, paying special attention to the main symptoms.

- Anamnesis collection - long-term use of a psychotropic substance and its withdrawal.
- Listening to the patient's complaints.
- Familiarization with documents - extracts, medical records, and other papers.
- General examination, determination of neurological status.
- Clinical diagnosis – identification of somatic, neurological and psychopathological signs of the syndrome.
- Measurement of pressure and heart rate.
- General blood and urine analysis, blood testing for basic biochemical markers.
- Determination of the amount of neurotropic substance in the blood that provoked the syndrome.
What drugs will worsen the disease?
You should not take antidepressants or painkillers. The doctor warns about this condition before prescribing Paxil. The combination may cause gastrointestinal bleeding. Anxiety, rapid heartbeat and elevated body temperature are also possible.
You need to take your antidepressant correctly. Even vitamins and nutritional supplements can lead to unexpected reactions.
It is important to pay attention to side effects during therapy. You should tell your doctor about all problems. If suicidal or other dangerous thoughts arise, consultation with a medical professional is required.
Healing procedures
Treatment of withdrawal syndrome is complex and multicomponent. Its direction is determined by the severity of symptoms, the type of psychotropic substance, the well-being of patients and the presence of concomitant pathology. General therapeutic measures are carried out in outpatient, inpatient or intensive care settings. Debilitated patients with signs of dehydration and hyperthermia, tremors, hallucinosis and other mental disorders are subject to mandatory hospitalization.
Pathology treatment regimen:
- Detoxification is the removal of consumed substances and breakdown products from the body. Drinking plenty of fluids, intense sweating and a hygienic shower are basic detoxification methods. At home, oral administration of “Regidron” and enterosorbents: “Polysorb”, “Activated carbon” is also recommended. In the hospital, patients are given infusion therapy - saline, glucose, and diuretics are administered intravenously. In severe cases, blood purification is prescribed using plasmapheresis, hemosorption, and hemodialysis.
- To prevent withdrawal, the neurotropic substance should be withdrawn gradually. They start with a dose that stabilizes the general condition of the patients, and then it is slowly reduced until complete failure.
- Symptomatic treatment is aimed at eliminating severe clinical manifestations. Patients are prescribed anticonvulsants - Carbamazepine, Clonazepam, Primidone; antipsychotics - Aminazine, Sonapax; antipyretic drugs - Nurofen, Paracetamol, Ibuklin; antihypertensive drugs – “Enalapril”, “Indapamide”, “Tenorik”; analgesics – “Baralgin”, “Ketonal”, “Nimesil”; sedatives - “Persen”, “Tenoten”, “Afobazol”; tranquilizers - Sibazon, Relanium, Grandaxin; antidepressants - Amitriptyline, Fluoxetine, Azafen; nootropics “Phenibut”, “Piracetam”, “Pantogam”; metabolic drugs - Mildronate, Riboxin, Trimetazidine.
- General restorative and restorative therapy - bed rest, walks in the fresh air, physiotherapy, optimal physical activity without overwork, breathing exercises, drinking enough liquid, enriching the diet with first courses, fruit drinks, non-carbonated drinks. All patients without exception are recommended to take vitamins and minerals.
- Psychotherapy – individual and group sessions aimed at getting rid of addiction; coding; psychological support from family and friends; creating a calm and friendly family environment; prevention of stressful and conflict situations.
Withdrawal syndrome with an integrated approach to treatment has a favorable prognosis and ends in recovery. Symptoms of the pathology gradually disappear, and body functions are restored.
Reviews
Ruslan, 38 years old, Yaroslavl
He was treated by a psychotherapist for depression. The doctor prescribed Fluoxetine for a course of two months. I felt better while taking the drug. As soon as I stopped using it, withdrawal symptoms developed: causeless anxiety, insomnia and periodic tremors in my hands. The doctor prescribed sedatives to ease the withdrawal process.
Evgenia, 26 years old, Syktyvkar
I took Cipralex for 3 months while undergoing psychotherapy for prolonged depression. The effect of the drug occurred after two weeks of use. I started to feel better and began to slowly reduce the dosage. After finishing taking the medication, complaints of migraine and dizziness appeared, that is, withdrawal syndrome occurred. It went away on its own on the 10th day.
Source: ProSindrom.ru
From a pharmacological point of view, several half-lives (3-4) can be distinguished as a time interval for the breakdown of a compound, since during this time there is an 8-16-fold decrease in the concentration of the drug. We also need to consider active metabolites. For example, caffeine breaks down into paraxanthine, theobromine, and theophylline, all of which have their own effects and half-lives that persist beyond the decay periods of the parent compound.
The answer to this question largely depends on the characteristics of the drug itself. It also depends on the body's genetic makeup and other drugs and foods a person may ingest, as these can all affect the drug's metabolic pathways. For example, grapefruit juice can significantly increase the elimination time of many drugs because it inhibits an important enzyme that breaks down these drugs (CYP3A4).
Whether a person takes a drug for many years or a few days of years does not greatly affect its half-life, in most cases, from a pharmacological point of view. Most medications are absorbed and excreted the same way no matter how long you take them. However, if you really wanted to know “how long does it take to recover from taking the drug for 30 years?”, then the question will not be so simple. It takes longer for your body to adjust to a drug- or substance-free state than it does to simply remove the drug from your body. You may have become physically and psychologically dependent on psychotropic pills, for example, phenozepam.
Some doctors claim that half the life of the drug is important, but ultimately this is not true. Drugs usually do not affect the body without the body's involvement in the process, especially if they have been part of the body's ecosystem for many years. Many psychotropic pills, especially pharmaceutical ones, are lipophilic, meaning they can be stored in fatty tissue. In addition, a number of psychotropic drugs are involved in the metabolism of fats, proteins and carbohydrates, sometimes potentially leaving a lingering effect on your body. Not all medications fall into this category, and sometimes the hardest part of detoxification for people using certain hydrophilic drugs can be in the first few days, even after decades of using the drug.
Psychotropic drugs typically change the physical structures of the brain and/or body systems and alter their functioning in a way that may be indefinite in duration, whether you are taking the drugs or not. They also tend to cause withdrawal symptoms due to physical dependence, which usually entails chronic (ongoing) use of psychotropic substances. Changes may even be registered at the epigenetic level, and many commonly used psychotropic drugs appear to be associated with long-term risks and dysfunctions that continue even after the cessation of psychotropic drug use (and even after a short duration of their use). That is, the removal of drugs from the body, in any form (active metabolites, inactive metabolites, potential tissue structures, etc.) will not end with restoration or a more significant process of “cleaning” from the drug.
Since not all patients react equally to the same psychotropic drugs, doses or duration of their use, it is impossible to answer the question unambiguously: how long the “cleansing” period, the recovery period or the process of general recovery lasts, since it is very individual. Even individual stages, such as withdrawal, can last anywhere from a few days to more than a decade, depending on how someone reacts to a particular drug or the context of its use.
Most doctors will not be very helpful in answering these questions and may give advice or information that is untrue or even harmful. Gather multiple opinions, look at or talk to relevant specialists (eg, toxicologists, pharmacologists, and physicians who deal with systemic or holistic disease and health), and delve into the literature available on the Internet (through databases). And seek out those sick people, especially your peers, who have been through what you are about to go through (online communities, local support groups, medically assisted programs, etc.).
Do not stop taking a psychotropic medication without exploring the appropriate and safest way to taper your dose and take care of yourself during the period after you stop treatment, including management if symptoms of withdrawal or relapse occur. There is a movement called “mental survival,” whose proponents talk about quitting psychotropic medications. I have met some people who have not taken these drugs for 5 years and still experience significant adverse reactions. Psychotropic pills are a double-action weapon; sometimes they save people, but then they can lead to consequences that are difficult to cope with.
Source: minutkoclinic.com
Video: about withdrawal syndrome from tranquilizers and antidepressants
Video: personal experience with antidepressant withdrawal
Nicotine withdrawal syndrome is manifested by a desire to return to smoking. Cigarettes cause significant physical and psychological dependence. When the next dose of nicotine penetrates the organs, the smoker feels euphoria (nicotine actively excites the nervous system). From the article you will learn how smoking withdrawal syndrome manifests itself, what negative consequences it brings, and what to do if you are a long-term smoker.
The concept of antidepressants
Examples of antidepressants:
- Amitriptyline;
- Venlafaxine;
- Vortioxin;
- Doxepin;
- Agomelatine;
- Trazodone;
- Phenazepam.
Their therapeutic effect is cumulative and manifests itself on days 3-10. The beneficial effect develops due to the accumulation of neurotransmitters at the ends of nerve receptors and improved conductivity in parts of the brain.
These chemicals were discovered in 1957. Their main function is a positive mood, ease of reactions, a change in character in a softer direction, and a significant improvement in the state of a person’s psyche. The pharmacological properties of such substances differ. There are antidepressants that have an inhibitory, calming effect. There are drugs, on the contrary, that increase performance.
Some medications have a positive effect on brain activity: memory and attention improve, and even cognitive activity increases (nootropic effect). Such drugs are used both in psychiatric practice and for the correction of current conditions of vegetative-vascular dystonia, long-term pain of various etiologies.
There are no absolutely harmless antidepressants. If they calm, then they are addictive.
How does the syndrome manifest?
Symptoms of smoking cessation occur after an hour and a half of abstinence. Lack of nicotine causes the following side effects: anxiety, headaches, and sometimes fever. Poor sleep, weakness, high blood pressure, disruption of the cardiovascular system, and allergies occur. Monthly stress may occur.
Smoking cessation syndrome is also accompanied by an increased emotional state, dry mouth, cough with sputum, and shortness of breath. Added to these are a large appetite, a feeling of lack of air, and increased sweating.
These symptoms are pronounced in the first week of quitting smoking. Then the condition improves. For some, smoker's syndrome makes itself felt only on the 10th day after stopping nicotine. In general, the duration of withdrawal syndrome, depending on individual characteristics, lasts for a week to a month, that is, thirty calendar days.
Nicotine withdrawal is the term used by narcologists to describe withdrawal syndrome when quitting smoking. A certain amount of nicotine is actively involved in metabolism, interacting with the central nervous system. When you quit cigarettes, you may crave them for years, and there will be no signs of withdrawal. Often, within two years of quitting tobacco, the body is completely freed from the harmful effects of nicotine.
Reviews
Ilya S .: “I took Zoloft to treat depression. When the time came to stop taking it, I acted strictly on the doctor’s recommendation. I reduced the dosage very slowly, divided the tablet into two parts, and calculated the required concentration. Since the initial dosage was small, the withdrawal lasted about a month. At the same time, no side effects bothered me. When it was time to stop taking it completely, no symptoms arose either.”
Daria N .: “I was prescribed Zoloft to combat panic attacks. I took it for three months, there were no panic attacks, so I decided to stop. After discontinuation of the drug, an almost constant headache occurred, followed by insomnia. About a week later I had one panic attack, but I decided to continue weaning myself off the drug. There were no more attacks, the headache went away after two weeks, and the insomnia persisted for a long time, so I had to see a doctor again.”
Psychiatrist: “Many people do not want to take antidepressants because they are afraid of becoming dependent on the pills. What they call addiction is actually withdrawal. Zoloft is one of those antidepressants that can actually be harmful to your health if you stop taking it. But in reality, everything is not so scary. It’s enough just to slowly reduce the dosage of the drug and there will be no withdrawal symptoms.”
Source: antidepressant.ru
Development of the condition by day
Smoking withdrawal syndrome or nicotine withdrawal forces you to work hard on yourself and show strong-willed qualities. This is a smooth process, which, however, is not as painful as it seems. The symptoms go away gradually, as does the desire to quit smoking. We invite you to consider the table of nicotine withdrawal syndrome in a month.
| Time without cigarettes (days) | Violations |
| 1-3 | Trouble sleeping, mild anxiety, low appetite, mild emotional irritation. |
| 3-6 | Disturbance in sleep patterns (frequent getting up at night), depression, heartburn, “squeezing” of the heart, dizziness when bending over, tinnitus. |
| 6-9 | The skin peels, small pimples appear, swelling of the face and limbs. An unbalanced psycho-emotional state, the presence of a mucous lump in the throat, abdominal pain, gastrointestinal problems. |
| 9-12 | Lethargy, dizziness, skin dries out or secretes oily substances too actively. Complete loss of sleep at night, desire to sleep during the day. |
| 12-15 | Increased urge to smoke, wet cough, nervous breakdown, constipation. |
| 15-18 | Raging appetite, muscle pain, aching bones, colds. |
| 18-21 | Excessive sweating, sharp contraction of the muscles of the arms and legs, pain in the right side, bitterness in the mouth, tormenting thirst, increased urination. |
| 21-24 | A noticeable wet cough, heartburn and strong stools occur after eating fatty foods. The skin dries and peels. |
| 24-27 | The pressure steadily decreases, allergic skin reactions appear, high excitability, and an even stronger desire to smoke a cigarette. |
| 27-30 | Intestinal peristalsis is restored, skin color and condition improves, lethargy, drowsiness. |
Herbal antidepressants
There are a large number of herbal drugs, the withdrawal of which does not cause any syndromes, for example:
- extract of motherwort, lemongrass, immortelle - increase performance;
- ginseng root is an excellent immunostimulant;
- honeysuckle and clover flowers exhibit antidepressant properties;
- hawthorn helps the heart function well and normalizes heartbeat;
- pharmaceutical chamomile is a good antispasmodic;
- calendula, mint – helps with overexertion;
- Leuzea exhibits excellent nootropic properties.
Try these herbal remedies. They are harmless and will have a positive effect on the body.
Try to cope with any situation without tragedy. Before self-medicating, consult a psychologist. Perhaps your problem will be solved without taking chemicals. If you are undergoing treatment and are prescribed such medications, do not engage in amateur activities. There is no need to increase or decrease the dosage as you wish. Be sure to consult your doctor.
Source: sindrom.guru
Duration of this state
As you can see, dependence on nicotine after smoking cessation is expressed by very unpleasant symptoms. Their duration and contrast depend on the following indicators: age, gender, health status, smoking experience, genetic factors, how much a person smokes per day. Separately, we note the importance of the degree of motivation of a person to overcome smoking cessation syndrome.
A month after quitting tobacco, a craving for the missing dose of nicotine appears on a psychological level. A person is not fully aware of how much he wants to smoke. Realizing how disgusting the withdrawal sensations are for him, he thinks that it is difficult to cope, to overcome himself. People are inspired to think that smoking is not so bad, but withdrawal symptoms will interfere with a full life.
Meanwhile, 30 days after quitting cigarettes, the symptoms of physical dependence begin to leave the person. But the habit of the psyche still remains strong. I want to smoke for another six months, feeling the aromatic smoke of tobacco. The most difficult period of quitting smoking in terms of psychology is the period from the 2nd to the 3rd months.
People who have given up a bad habit state that cigarette withdrawal syndrome reaches its apogee on the fourth to seventh day after quitting. At this moment, the body realizes that it has been left without nicotine for a long time. Then he begins to rebuild all functions and processes in a healthy way. This is the very starting point that gives rise to a new lifestyle without nicotine.
How long do Zoloft side effects last?
If a side effect occurs after stopping the drug, the symptoms will persist until all the drug is removed from the blood. In the best case, this will happen two weeks after finishing taking the drug. By this time, withdrawal symptoms should be expected to disappear.
Sometimes symptoms persist for more than two or even three months. In the most severe cases, they can appear periodically over a very long time.
The easiest way to prevent withdrawal syndrome is to follow a Zoloft discontinuation regimen.
How to get rid of withdrawal symptoms
There are rules that help with withdrawal symptoms to ease the body's dependence on nicotine. Let us highlight the main methods of combating nicotine withdrawal:
- Nicotine gum, tablets, patches or sprays.
- Exercise, walks in the fresh air.
- Diet: eat more fruits and dairy products.
- Visit the pool, sauna or bathhouse.
- Drink more water.
REFERENCE INFORMATION! In the first days after quitting cigarettes, symptoms will subside when you add vegetables containing nicotine to your meals. These include potatoes, cauliflower, cucumbers, tomatoes, and eggplant.
The liver of a non-smoker produces the minimum amount of nicotine for normal functioning. When you stop smoking cigarettes, it stops supplying the body with the substance due to the fact that it is accustomed to receiving a dose of nicotine in a different way. The listed vegetables activate normal liver function.
After stopping cigarettes, if you have a strong desire to smoke, do the following: count four minutes - during this time the craving will weaken. Take deep breaths 5-10 times, drink water. Lose yourself in other thoughts, chat, or invite someone to go for a walk together.
Official medicine
Narcologists recommend sound and frequent sleep during cigarette withdrawal syndrome. Some experts advise quitting the habit of smoking when you have a cold infection.
There are a number of medications that are recommended by doctors for smoking withdrawal syndrome. We have prepared a list of the most popular remedies used for smoking cessation syndrome:
- Lobelin. Sold in drops and tablets. Take tablets – one per day. Drops should be taken in 4-5 repetitions at a rate of 10-15 per day. We do this for a week. The course may be repeated.
- Bullfight. Herbal preparation with a period of 5-7 weeks. Dosage only under the supervision of a doctor.
- Tabex. For the first 3 days, one daily dose is enough. After 2-3 months for an individual prescription.
- Zyban. Already a week before the ban on nicotine, they begin taking the drug. The course period and dosage are determined from each individual’s personal indicators.
- Champix. Daily course: 1-3 days – 1/2 tablet; 4-7 days – the same norm, now twice; 8-14 days – one full tablet in two doses per day.
Traditional methods
In order to overcome nicotine withdrawal syndrome, grandmother's advice will be very useful. Proven tobacco control tools are:
- Eucalyptus. Eucalyptus oil is used to prepare inhalations that cleanse the smoker’s body of resins, nuclides, tar, and salts. We take eucalyptus and lavender oils by inhalation every other day.
- Ginger. Relieves annoying cough caused by smoking and phlegm. Its roots (500 g) are infused in 1 liter. alcohol for two weeks, stir after a while. Then we strain the tincture, make it again, and let it sit for a day. Drain the liquid, removing the sediment. We drink ginger mixture twice a day after meals.
- Mint. Calms nerves, removes stress and bad emotions. Prepare a mint decoction, drink 50 g eight times a day, 3 tbsp. Pour dried herbs in a proportion of 300 g. Leave for a couple of hours.
- Oats. Oat bran helps fight withdrawal symptoms. We boil them and drink them eight times a day at the same rate as above. Required before eating.
- Lobelia. A unique way to get rid of smoking withdrawal syndrome. Then the nicotine deficiency is replaced by lobelia extract. There is little nicotine in it, you are guaranteed to quit smoking faster and less painfully.
EXPERT ADVICE! Self-treatment is strictly contraindicated. You should only take medications that are prescribed by your doctor. Before use, be sure to take the recommendation of a specialist to avoid side effects.
Recommendations for stopping treatment with antidepressants
Refusal to use such drugs requires a careful and strict approach. If signs of illness occur, it is better to consult a doctor. To combat antidepressant withdrawal syndrome, symptomatic therapy is used, for example, antiemetics, tranquilizers, and intravenous electrolyte solutions. Often, the malaise goes away without the use of specific measures. The duration of the physiological reaction to stopping taking medications depends on the rate of their metabolism and the removal of waste products from the patient’s body.
Non-drug methods of improving well-being are also widely used. Taking a course of massage and physiotherapeutic procedures, such as electrophoresis, is effective.
How to avoid withdrawal syndrome?
This condition is easier to prevent than to treat. Schemes of gradual dosage reduction are used. In this case, the rate of drug withdrawal is determined individually based on the available medical history, the characteristics of the patient’s body and the duration of therapy. Standard recommendations suggest reducing first the amount of the active substance, and then the frequency of taking antidepressants. In the case of long-term use of drug therapy, mild sedatives of plant origin are used in the process of stopping the use of the drug. Psychotherapy, which is the main method of combating obsessive and depressive conditions, also has good reviews. During drug withdrawal, it is recommended to minimize physical activity and exposure to stress factors.