What is the hypothalamic-pituitary system in physiology?
The human body is not a collection of organs and systems.
This is a complex biological system connected by regulatory mechanisms of nervous and endocrine nature. And one of the main structures in the system of regulation of the body’s activity is the hypothalamic-pituitary system. In this article we will look at the anatomy and physiology of this complex system.
Let us give a brief description of the hormones that are secreted by the thalamus and hypothalamus, as well as a brief overview of disorders of the hypothalamic-pituitary system and the diseases to which they lead.
Thalamus - pituitary gland: connected by one chain
The combination of the structural components of the hypothalamus and pituitary gland into a single system ensures the regulation of the basic functions of our body. In this system, there are both direct and feedback connections that regulate the synthesis and secretion of hormones.
The hypothalamus directs the work of the pituitary gland, and feedback is carried out through the hormones of the endocrine glands, which are released under the influence of pituitary hormones. Thus, the peripheral endocrine glands bring their biologically active substances through the bloodstream to the hypothalamus and regulate the secretory activity of the hypothalamic-pituitary system of the brain.
Let us recall that hormones are protein or steroid biological substances that are released into the blood by the internal secretion organs (endocrine) and regulate metabolism, water and mineral balance, growth and development of the body, and also take an active part in the body’s response to stress.
A little anatomy
The physiology of the hypothalamic-pituitary system is directly related to the anatomical structure of the structures that comprise it.
The hypothalamus is a small part of the intermediate section of the brain, which is formed by more than 30 clusters of nerve cells (nodes). It is connected by nerve endings to all parts of the nervous system: the cerebral cortex, hippocampus, amygdala, cerebellum, brain stem and spinal cord.
The hypothalamus regulates the hormonal secretion of the pituitary gland and is the link between the nervous system and the endocrine system. Feelings of hunger, thirst, thermoregulation, sexual desire, sleep and wakefulness - this is not a complete list of the functions of this organ, the anatomical boundaries of which are not clear, and the mass is up to 5 grams.
The pituitary gland is a rounded formation on the lower surface of the brain, weighing up to 0.5 grams. This is the central organ of the endocrine system, its “conductor” - it turns on and off the work of all secretion organs of our body. The pituitary gland consists of two lobes:
- Adenohypophysis (anterior lobe), which is formed by glandular cells of various types that synthesize tropic hormones (directed to a specific target organ).
- Neurohypophysis (posterior lobe), which is formed by the endings of neurosecretory cells of the hypothalamus.
In connection with this anatomical structure, the hypothalamic-pituitary system is divided into 2 divisions - the hypothalamic-adenopituitary and the hypothalamic-neurohypophyseal.
Foremost
If the pituitary gland is the “conductor” of the orchestra, then the hypothalamus is the “composer”. In its nuclei two main hormones are synthesized - vasopressin (diuretic) and oxytocin, which are transported to the neurohypophysis.
In addition, releasing hormones are secreted here, which regulate the formation of hormones in the adenohypophysis. These are peptides that come in 2 types:
- Liberins are releasing hormones that stimulate the secretory cells of the pituitary gland (somatoliberin, corticoliberin, thyrotropin-releasing hormone, gonadotropin).
- Statins are hormone inhibitors that inhibit the functioning of the pituitary gland (somatostatin, prolactinostatin).
Releasing hormones not only regulate the secretory function of the pituitary gland, but also affect the functioning of nerve cells in different parts of the brain. Many of them have already been synthesized and have found their application in therapeutic practice in the correction of pathologies of the hypothalamic-pituitary system.
The hypothalamus also synthesizes morphine-like peptides - enkephalins and endorphins, which reduce stress levels and provide pain relief.
The hypothalamus receives signals from other brain structures using amino-specific systems and thus provides communication between the nervous and endocrine systems of the body.
Its neurosecretory cells influence the cells of the pituitary gland not only by sending a nerve impulse, but also by releasing neurohormones. Signals from the retina, olfactory bulb, taste and pain receptors come here.
The hypothalamus analyzes blood pressure, blood glucose levels, the state of the gastrointestinal tract and other information from internal organs.
Work principles
Regulation of the hypothalamic-pituitary system is carried out according to the principles of direct (positive) and feedback (negative) communication. It is this interaction that ensures self-regulation and normalization of the body’s hormonal balance.
Neurohormones of the hypothalamus act on the cells of the pituitary gland and increase (liberins) or inhibit (statins) its secretory function. This is a direct connection.
When the level of pituitary hormones in the blood increases, they enter the hypothalamus and reduce its secretory function. This is feedback.
This is how the neuro-hormonal regulation of body functions is ensured, the constancy of the internal environment, the coordination of vital processes and adaptability to environmental conditions are ensured.
Hypothalamic-adenopituitary division
This department secretes 6 hormones of the hypothalamic-pituitary system, namely:
- Prolactin or luteotropic hormone - stimulates lactation, growth and metabolic processes, instincts of caring for offspring.
- Thyrotropin – provides regulation of the thyroid gland.
- Adenocorticotropin - regulates the production of glucocorticoid hormones by the adrenal cortex.
- 2 gonadotropic hormones - luteinizing hormone (in men) and follicle-stimulating hormone (in women), which are responsible for sexual behavior and function.
- Somatotropic hormone - stimulates protein synthesis in cells, affects the overall growth of the body.
Hypothalamic-neurohypophyseal division
This department performs 2 functions of the hypothalamic-pituitary system. The posterior part of the pituitary gland secretes the hormones asparotocin, vasotocin, valitocin, glumitocin, isotocin, mesotocin. They play an important role in metabolic processes in the human body.
In addition, in this section, vasopressin and oxytocin received from the hypothalamus are deposited in the blood.
Vasopressin regulates the processes of water excretion by the kidneys, increases the tone of the smooth muscles of internal organs and blood vessels, and is involved in the regulation of aggression and memory.
Oxytocin is a hormone of the hypothalamic-pituitary system, whose role is in stimulating uterine contractions during pregnancy, stimulating sexual desire and trust between partners. This hormone is often called the “happiness hormone.”
Diseases of the hypothalamic-pituitary system
As has already become clear, the pathology of this system is associated with disturbances in the normal activity of one of its departments - the hypothalamus, the anterior and posterior parts of the pituitary gland.
Any change in the hormonal balance in the body leads to serious consequences in the body. Especially when the “composer” or “conductor” makes mistakes.
In addition to hormonal imbalances, pathologies in the hypothalamic-pituitary system can be caused by cancer and injuries that affect these areas. It is impossible to list all the diseases that are in one way or another connected with this regulatory system. We will focus on the most significant pathologies and give a brief description of them.
Dwarfism and gigantism
These growth disorders are associated with disturbances in the production of somatotropic hormone.
Pituitary dwarfism is a disease that is associated with somatotropin deficiency. Manifests itself in retarded growth and development (physical and sexual).
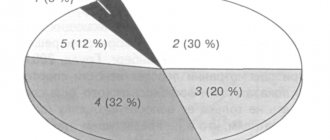
The etiology of the disease is associated with hereditary factors, birth defects, injuries and pituitary tumors. However, in 60% of cases the causes of dwarfism cannot be determined.
Therapy involves the constant use of growth hormones by patients.
Pituitary gigantism is a disease associated with excess or increased activity of growth hormone. It develops more often after 10 years, and predisposing factors are neuroinfections, inflammation in the diencephalon, and trauma. The disease manifests itself in accelerated growth, features of acromegaly (enlargement of the limbs and facial bones). Estrogens and androgens are used for therapy.
Adiposogenital dystrophy
The causes of this pathology can be intrauterine infections, birth injuries, viral infections (scarlet fever, typhus), chronic infections (syphilis and tuberculosis), tumors, thrombosis, and hemorrhages in the brain.
The clinical picture includes underdevelopment of the genital organs, gynecomastia (enlargement of the mammary glands due to fat deposition) and obesity. It is more common in boys 10-13 years old.
Itsenko-Cushing's disease
This pathology develops with damage to the hypothalamus, thalamus and reticular formation of the brain. The etiology is associated with injuries, neuroinfections (meningitis, encephalitis), intoxication and tumors.
The disease develops due to excessive secretion of corticotropin by the adrenal cortex.
With this pathology, patients report weakness, headaches, pain in the limbs, drowsiness and thirst. The pathology is accompanied by obesity and short stature, puffiness of the face, dry skin with characteristic stretch marks (striae).
There are increased red blood cells in the blood, increased blood pressure, tachycardia and dystrophy of the heart muscles.
Treatment is symptomatic.
Source: //FB.ru/article/33377/cu-gipotalamo-gipofizarnaya-sistema—eto-chto-takoe-v-fiziologii
Recovery process
The etiology of all disorders is directly related to the development of neoplasms and dystrophic syndromes. Often we are talking about changes in the structure of a certain part of the neuroendocrine type complex.
Before treating such pathologies, it is necessary to carry out diagnostic procedures to identify the causes of system failure. Thus, hypothalamic-pituitary acute failure can be detected by a number of specific procedures. So the patient must be subjected to a comprehensive examination, and the following procedures take place:
- Magnetic resonance imaging;
- Clinical tests are taken and hormonal tests are performed.
After the diagnostic procedures are completed, a course of hormone replacement and stimulating therapy begins. If tumor-type formations occur, they must be removed by endoscopy. In the vast majority of cases, when the catalysts for the disorders are eliminated, the condition begins to gradually normalize, and the lost functions are restored.
If this is not done, then dysfunction of the unique hypothalamic-pituitary system can cause a person’s disability, and more serious negative consequences for a person may arise.
Pituitary gland massage
Anatomy of the diencephalon, thalamus and hypothalamus
hypothalamus is the human soul, - School of Psychology in Sochi from Yuri Levchenko
Pituitary
!!!Hypothalamus Responsible for...!!! | !!!Gipotalamus Answer za...!!!
Ventricles of the brain | 3D Human Anatomy | Internal organs
Biology in Pictures: Secondary Urine Formation (Issue 20)
#Treatment of the Hypothalamus and Pituitary Gland#|#Lechenie Gipotalamusa i Gipofiza#
Treatment of the hypothalamus. Ayurveda principle. Ruslan Narushevich
Hypothalamic-pituitary system
Pituitary hypothyroidism, pituitary hormone deficiency
Pituitary gland massage
Pituitary
54. Hypothalamic-pituitary system, its functional connections. Pituitary hormones,
their participation in the regulation of the activity of endocrine organs.
Hypothalamic-pituitary system
- a combination of the structures of the pituitary gland and hypothalamus, performing the functions of both the nervous system and the endocrine system. This neuroendocrine complex is an example of how closely the nervous and humoral modes of regulation are connected in the mammalian body.
Structure:
The hypothalamic-pituitary system consists of the pituitary stalk, starting in the ventromedial region of the hypothalamus, and three lobes of the pituitary gland: adenohypophysis (anterior lobe), neurohypophysis (posterior lobe) and intercalary pituitary gland.
The work of all three lobes is controlled by the hypothalamus with the help of special neurosecretory cells. These cells secrete special hormones - releasing hormones.
Releasing factors enter the pituitary gland, or rather the adenohypophysis through the portal vein of the pituitary gland.
There are two types of releasing factors.
- liberating (under their influence, the cells of the adenohypophysis release hormones)
- stopping (under their action the excretion of adenohypophysis hormones stops)
The neurohypophysis and intercalary lobe of the hypothalamus are influenced by special nerve fibers, rather than neurosecretory cells.
Hormones of the hypothalamic-pituitary system:
Under the influence of one or another type of influence, the hypothalamus and pituitary gland secrete various hormones that control the functioning of almost the entire human endocrine system. The exception is the pancreas and the adrenal medulla. They have their own regulatory system.
Hormones of the anterior pituitary gland
Somatotropin
A growth hormone
It has an anabolic effect, therefore, like any anabolic steroid, ST enhances synthesis processes (especially protein synthesis). Therefore, somatotropin is often called “growth hormone”.
When the secretion of somatotropin is impaired, three types of pathologies arise.
- When the concentration of somatotropin decreases, a person develops normally, but his height does not exceed 120 cm - “pituitary dwarfism”. Such people (hormonal dwarfs) are capable of childbearing and their hormonal levels are not greatly disturbed.
- With an increase in the concentration of somatotropin, a person also develops normally, but his height exceeds 195 cm. This pathology is called “gigantism.” During puberty (the period of activation of the reproductive system, starting at approximately 11-13 years. In young men, puberty occurs two years later than in girls, whose hormonal surge, unlike boys, is smooth and its decline is quite rapid.) muscle mass increases greatly, therefore, the number of capillaries increases. The heart is not capable of such rapid growth. Because of this discrepancy, pathologies arise. For example, vegetative-vascular dystonia (VSD), often found in adolescents.
- After 20 years, the production of somatotropin decreases, therefore, the formation of cartilage tissue (as one of the aspects of growth) slows down and decreases. Therefore, the bone tissue slowly “eats” the cartilage tissue, therefore the bones have nowhere to grow except in diameter. If the production of somatotropin does not stop after 20, then the bones begin to grow in diameter. Due to this thickening of the bones, for example, the fingers become thicker, and because of this thickening they almost lose mobility. At the same time, somatotropin also stimulates the production of connective tissue, as a result of which the lips, nose, ears, tongue, etc. enlarge. This pathology is called “acromegaly”.
Thyrotropin
The target of thyrotropin is the thyroid gland. It regulates the growth of the thyroid gland and the production of its main hormone, thyroxine. An example of the action of a releasing factor: Thyroxine is necessary to increase the efficiency of oxygen respiration, thyroxine requires thyrotropin, and thyrotropin requires thyrotropin-releasing hormone, which is the releasing factor of thyrotropin.
Gonadotropins
The name gonadotropins (GT) refers to two different hormones - follicle-stimulating hormone and luteinizing hormone. They regulate the activity of the sex glands - the gonads.
Like other tropic hormones, gonadotropins primarily influence the endocrine cells of the gonads, regulating the production of sex hormones.
In addition, they influence the maturation of gametes, the menstrual cycle and related physiological processes.
Corticotropic hormones
The target of CT is the adrenal cortex. It should be noted that the parathyroid gland regulates mineral metabolism (with the help of parathyroid hormone), like the adrenal cortex, so you can put regulation only on the adrenal cortex, and the parathyroid gland will automatically work in accordance with the adrenal cortex.
Posterior lobe of the pituitary gland (neurohypophysis)
Neuropituitary hormones are antidiuretic hormones
(ADH) or vasopressin and
oxytocin.
The formation of hormones in the posterior lobe of the pituitary gland occurs mainly in the nuclei of the hypothalamus as a result of neurosecretion processes.
ADH is apparently secreted in the supraoptic nucleus, and oxytocin is secreted in the paraventricular nucleus of the hypothalamus. These hormones enter the posterior lobe of the pituitary gland along the axons of nerve cells.
This is facilitated by the presence of a direct nervous connection between the neurohypophysis and the nuclei of the hypothalamus.
The mechanism of action of ADH is that under its influence the reabsorption of water in the collecting ducts of the kidneys increases.
With a decrease in ADH secretion, diabetes insipidus occurs, which is accompanied by the release of large amounts of urine (sometimes tens of liters per day), which is associated with impaired reabsorption of water in the collecting ducts.
In large doses, it causes contraction of smooth muscle vessels (especially arterioles), which leads to an increase in blood pressure.
Oxytocin stimulates the contraction of the smooth muscles of the uterus and, thus, ensures the normal course of labor and affects the secretion of milk.
Intermediate lobe of the pituitary gland
.
Hormone of the intermediate lobe - intermedin
or
melanoma-stimulating hormone
occurs in two forms that differ in the number of amino acid residues. During pregnancy and with adrenal insufficiency (in these cases, changes in skin pigmentation are often observed), the amount of melanostimulating hormone in the pituitary gland increases.
The secretion of intermedin is regulated reflexively under the influence of light on the retina of the eye. It takes part in regulating the movement of cells of the black pigment layer in the eye. In bright light, the cells of the pigment layer release pseudopodia and excess light rays are absorbed by the pigment, which protects the retina from intense irritation.
Source: //studfile.net/preview/6066186/page:35/
Principles of treatment
In case of gonadotropic insufficiency of the pituitary gland, the only method of achieving follicle growth in the ovaries, ovulation, and, consequently, pregnancy is the use of replacement therapy with drugs - gonadotropins. If the hypothalamus is damaged, an alternative method of treating infertility may be the administration of gonadoliberins, which stimulate the gonadotropic function of the pituitary gland.
Infertility treatment consists of two stages: the preparatory stage and ovulation induction.
1. At the preparatory stage, cyclic hormone replacement therapy is carried out with the sequential administration of estrogens and gestagens in order to correct the hormonal status of the woman. The growth and development of female genital organs is also stimulated: an increase in the size of the uterus, growth of the endometrium, the formation of a receptor apparatus in target organs, which increases the effectiveness of subsequent stimulation of ovulation. The duration of preparatory therapy is determined depending on the severity of hypogonadism and averages 3-12 months.
2. Ovulation induction is carried out by gonadotropins and has the goal of ovulation. The adequacy of the prescribed treatment is assessed by ultrasound examination of the ovarian follicles. The adequacy of the dose of the drugs used is assessed by the dynamics of follicle growth (normally 2 mm per day). If the follicles are growing slowly, the dose is increased; if the follicles are growing too quickly, the dose is reduced.
After ovulation is confirmed, the luteal phase of the cycle is supported with drugs from the group of gestagens.
Prevention of infertility due to estrogen deficiency includes replacement therapy. Based on the mechanism of development of the disease, the need for replacement therapy with female sex hormones - estrogens and gestagens, the purpose of which is the formation of female appearance, is generally recognized.
•During puberty – for the formation of a female body type, normal development of the genital organs, mammary glands and secondary sexual characteristics, as well as to achieve normal bone mass. Early diagnosis of HS and timely administration of hormone replacement therapy (from 16-18 years of age) are necessary, and its continuation, if possible, continuously until 20-23 years of age.
•During the reproductive period – before ovulation induction, hormone replacement therapy for 3 months is desirable in preparation for pregnancy. After pregnancy, childbirth and lactation, hormone replacement therapy is required in the form of long courses for at least 12 months in order to prevent osteoporosis.
•In the period after the birth of a child, it is necessary to diagnose systemic changes caused by hormonal disorders and their correction with the help of hormone replacement therapy, herbal medicine and specific drugs for the treatment of osteoporosis. Hormone replacement therapy for hypogonadotropic hypogonadism in women can be continued until the age of natural menopause (45-50 years).
Hypothalamic-pituitary system
The hypothalamic-pituitary system plays an important role in regulating the functions of the endocrine glands. It has the following structure:
1) a system consisting of the hypothalamus and neurohypophysis (posterior pituitary gland) 2) a system formed by the hypophysiotropic zone of the hypothalamus (contained in the median eminence), connected to the adenohypophysis (anterior pituitary gland) via the hematoneural contact zone,
3) the neuroendocrine system, responsible for the formation of neuroregulatory peptides (enkephalins, endorphins, substance P, etc.), which have pituitary activity.
The synthesis of hormones in the hypothalamus, in particular antidiuretic (vasopressin) and oxytocin, occurs in the neurons of the eupraoptic and paraventricular nuclei. These hormones are transported “in the form of granules from the cell bodies by their axons, which form the hypothalamic-pituitary tract infundibulum, to the capillaries of the neurohypophysis, where the hormones are released after the breakdown of the granules.
In addition to large neurosecretory cells that produce vasopressin and oxytocin, the hypothalamus has small nerve cells located in the pituitary zone that produce hormones that stimulate or suppress the release of hormones by the adenohypophysis - called releasing hormones, or releasing factors.
It has recently been proposed to call releasing hormones, which promote the formation of hormones by the adenohypophysis, liberins, and inhibitor hormones - statins. In terms of their chemical composition, releasing hormones are peptides.
Releasing hormones from the pituitary zone of the hypothalamus enter the adenohypophysis through the portal system of pituitary veins, which carry blood to the capillary plexus of the adenohypophysis. In addition to releasing hormones, peptides that have a morphine-like effect are synthesized in the hypothalamus. These are enkephalins and endorphins (endogenous opiates).
They play an important role in the mechanisms of pain and analgesia, regulation of behavior and autonomic integrative processes.
The function of the endocrine glands is influenced by various structures of the central nervous system through the hypothalamus.
Thus, the central regulation of the hypothalamic-pituitary system is carried out by centers that are localized in the preoptic area, limbic system, in neurons of the brain stem (oblongata, middle and pons), up to the cerebral cortex. Signals from many of these centers to the nuclei of the hypothalamus are transmitted through amino-specific brain systems. In turn, the reaction of the centers begins at a certain level of hormones of the peripheral endocrine glands and tropic hormones of the pituitary gland.
The function of most endocrine glands is regulated by hormones from the anterior pituitary gland (adenohypophysis).
The release of these hormones, in turn, is influenced by hormones of neurons in the hypophysiotropic zone of the medial region of the hypothalamus, which have either a stimulating or inhibitory effect on the pituitary gland and are called releasing factors and inhibitory factors, respectively.
Releasing factors are released from the nerve processes in the area of the median eminence and through the hypothalamic-pituitary system enter the adenohypophysis with the blood.
The principle of regulation is that with an increase in the plasma content of hormones of the peripheral endocrine glands, the release of the corresponding releasing factor into the blood vessels of the medial region of the hypothalamus decreases.
Regulation based on the principle of negative feedback, in which the medial hypothalamus, pituitary gland and peripheral endocrine glands participate, operates even in the absence of influences from the central nervous system. Regulation persists after complete separation of the medial region of the hypothalamus from the rest of the central nervous system. The role of the central nervous system is to adapt this regulation to the internal and external needs of the body. For example, under stress, the secretion of cortisol by the adrenal cortex increases as a result of the fact that the activity of neurons in the medial region of the hypothalamus increases, which leads to increased release of releasing factor in the median eminence.
Central regulation of the hypothalamic-pituitary endocrine system is carried out primarily by the centers of the preoptic region, limbic system and midbrain. The influence of these centers switches through the lateral region of the hypothalamus.
It is believed that signals from these centers are transmitted by neurons whose mediators are norepinephrine, dopamine or seratonin. Perhaps these centers also receive information about the content of endocrine hormones in the blood plasma according to the feedback principle.
Neurons that are part of regulatory systems are able to specifically respond to hormones of the endocrine glands and accumulate them.
The close interaction of the nervous and endocrine structures of the hypothalamus can be seen in the example of connections between neurons of the hypophysiotropic zone. A neuron secreting a releasing factor can be influenced by afferent neurons of the limbic system (amygdala and hippocampus), preoptic area and anterior part of the hypothalamus.
The motor processes of this neuron go to a variety of parts of the brain. Such neurons have the property of self-regulation based on the principle of recurrent inhibition. In all motor processes of such neurons, the transmitter appears to be the releasing factor.
Thus, these cells of the hypophysiotropic zone are, on the one hand, final integrating cells, and on the other, endocrine cells that form the hormone.
Didn't find what you were looking for? Use the search:
Source: //studopedia.ru/10_203428_gipotalamo-gipofizarnaya-sistema.html
Treatment of enlarged pituitary gland
If there are no visual impairments and abnormalities in blood tests for hormones, then an enlargement of the pituitary gland requires only observation. Patients are prescribed tomography and repeated blood tests, examination by a neurologist and an ophthalmologist once a year. If an adenoma is detected, then depending on its size and hormonal activity, the doctor chooses treatment tactics:
- removal through the nasal passages (endonasal transsphenoidal adenomectomy) – performed when there is an increased level of hormones with corresponding symptoms, signs of compression of the optic nerves, high intracranial pressure;
- surgery with opening of the skull - a large tumor that cannot be removed by endonasal access, since there is a possibility of damage to neighboring brain structures.
- radiation therapy is prescribed for inactive tumors (does not produce hormones), for elderly patients, or for contraindications to surgery; radiation is also indicated after surgical removal of a large adenoma;
- cryodestruction - inserting a probe through the nasal passage into the pituitary gland and applying cold to it to destroy the tumor;
- medications - somatostatin, which suppresses the formation of growth hormone, Parlodel and Dostinex for high prolactin, Peritol to inhibit cells that produce corticotropin and somatotropin.
After surgery, hormonal deficiency may occur. To correct it, analogs of natural hormones are used - levothyroxine, hydrocortisone, estradiol, testosterone. The same tactics are needed if the cause of the enlargement of the pituitary gland is diseases of the glands of the endocrine system.
Hypothalamic-pituitary system and its functions
Metabolism in the body, the systems that carry it out (endocrine, excretory, respiratory, circulatory), and also ensure growth and reproduction, are regulated by a certain brain structure.
It is called the “hypothalamic-pituitary system” and unites the pituitary gland and hypothalamus, the joint physiology of which is determined by the presence of neurosecretory cells that secrete hormones and special nerve fibers.
The hypothalamus is a small section that borders the optic chiasm in front, the mammillary bodies in the back (subcortical centers of smell). The hypothalamic groove runs above, separating it from the thalamus. From below, the section is represented by a gray tubercle that stretches into a funnel and passes into the pituitary stalk.
The pituitary gland is an oval-shaped organ slightly larger than a pea. It is enclosed in a special sheath of connective tissue, thanks to which it is fixed in the sella turcica - the bony notch of the sphenoid bone.
The hypothalamus, together with the thalamus (subcortical center of sensitivity), epithalamus (endocrine gland) and metathalamus (subcortical center of vision) is part of the diencephalon.
The establishment of communication between these two departments occurs through the pituitary stalk and the circulatory system. The pituitary gland consists of two parts (the third, intermediate, is underdeveloped in humans), each of which performs its own specific functions.
The anterior lobe (adenohypophysis) produces hormones under the influence of certain substances of the hypothalamus: releasing factors (liberins) stimulate this synthesis, statins inhibit it. The posterior lobe (neurohypophysis) does not produce independently, but accumulates hypothalamic hormones.
In this regard, the physiology of the hypothalamus is rarely considered separately from the pituitary gland.
Hypothalamus and adenohypophysis
The entire hypothalamic zone has an abundant blood supply. Groups of cells in the hypothalamus form nuclei, of which in humans there are 32 pairs (hormones are produced in them). Each cell of these nuclei is connected to several capillaries, which are highly permeable to nutrients and other compounds due to the absence of a glial layer.
The physiology of the blood circulation of this structure is such that it allows the anterior lobe of the pituitary gland and the hypothalamus to communicate with each other through the portal system of blood vessels. The arterioles in the area of the gray tubercle disintegrate into a network of capillaries, which, in turn, collect in the portal veins, running along the pituitary stalk to the anterior lobe, and form a secondary capillary network.
Through blood circulation, liberins are sent to the anterior pituitary gland, the functions of which are to help the pituitary gland synthesize hormones, and statins, which stop this process . This is how the hypothalamic-adenopituitary connection is established.
Currently, there are 7 pituitary substances, 7 releasing factors and 3 hypothalamic statins known.
- Gonadotropic (follicle-stimulating and luteinizing) hormones that regulate ovulation and ovarian function in women, spermatogenesis in men, are formed thanks to gonadoliberins (folliberin and luliberin). Their deficiency threatens a person with infertility.
- Somatotropin, whose functions are to ensure human growth and development, is stimulated by somatoliberin. Its deficiency in a child threatens the development of dwarfism. An adult can feel it when he feels severe weakness and decreased performance. The releasing factor can be inhibited by somatostatin.
- Prolactin, which stimulates milk production in a woman’s mammary glands, is produced thanks to prolactoliberin. Its activity increases during pregnancy and the postpartum period, and a deficiency leads to absence or weak lactation. It can be suppressed under the influence of prolactostatin.
- Thyrotropin, which is necessary for the full function of the thyroid gland, is produced thanks to thyrotropin-releasing hormone.
- Adrenocorticotropin, responsible for the functioning of the adrenal cortex, is formed under the influence of corticoliberin. Its deficiency threatens adrenal insufficiency.
- Melanotropin, which is a hormone of the intermediate lobe, which is often referred to as the structure of the adenohypophysis, is responsible for increasing the number of pigment cells. This is regulated by melanoliberin and melanostatin.
The fact that statins are not listed for gonadotropic, adrencocorticotropic, and thyroid-stimulating hormones does not mean that they do not exist: they are currently being searched for and identified.
Hypothalamus and neurohypophysis
The hypothalamic-neurohypophyseal connection is established through the interaction of the axons (processes) of the neurosecretory cells of the large nuclei of the hypothalamus and the posterior lobe of the pituitary gland through the pituitary stalk. The physiology of the neurohypophysis differs from that of the anterior lobe: hypothalamic hormones are not produced in this area, but accumulate and then enter the bloodstream.
Neurons of the supraoptic nuclei produce vasopressin, the main functions of which are the conservation of water in the human body and the constriction of blood vessels.
The action of this hormone determines the physiology of water excretion by the kidneys (it is also called antidiuretic).
The absence or insufficient production of vasopressin leads to the development of a rare serious disease - diabetes insipidus , which is characterized by the patient excreting 15-20 liters of urine daily and increased thirst. Lifelong therapy involves taking a vasopressin analogue.
In addition, it is responsible for increasing blood pressure, tone the smooth muscles of internal organs, and has a hemostatic effect.
There are cases where, thanks to the synthetic drug vasopressin, memory was restored in those suffering from amnesia after injury. Introduced in small doses, it accelerates the development of new skills and improves the reproduction of information.
Neurons of the paraventricular nuclei are responsible for the production of oxytocin, which is key during labor, contracting the uterus, and during breastfeeding, promoting milk transport.
Pituitary gland microadenoma
What is a microadenoma? This is a benign tumor of the gland, less than 10 mm in size. If the size of such a neoplasm is in the range of 10-30 mm, then it is called macroadenoma. Giant formations over 30 mm are extremely rare.
If a pituitary adenoma is discovered, all about the treatment and consequences.
Due to the appearance of compaction, a person experiences hormonal imbalances, and the nervous, endocrine and reproductive systems begin to suffer. Since the clinical manifestation of such processes is pronounced, they were separated into a separate group with a code according to ICD 10.
Depending on hormonal activity, pituitary microadenoma can be:
- Hormonally active.
- Not secreting.
Treatment for shrinkage of the pituitary gland
To replace lost functions, the use of synthetic hormone analogues is indicated:
- growth – Genotropin, Saizen;
- thyroid thyroxine - Eutirox, Bagotirox;
- adrenal cortisol – Hydrocortisone, Cortef;
- gonadotropic (activate the formation of reproductive organs): Pregnyl and Testosterone for young men, to stimulate the formation of sperm - Humegon, Puregon; For girls, estrogens are used - Proginova, Estrofem, and after a year they are prescribed along with progesterone - Trisequence, Cyclo-Proginova.
Hormone replacement therapy is carried out under constant monitoring of blood tests. To correct decreased bone density, calcium supplements and Osteogenon are prescribed. If there is significant weight loss, a diet with sufficient protein, carbohydrates, and vegetable fats is indicated. If necessary, anabolic hormones are prescribed.
Interaction of endocrine glands
Balanced work in the adrenal glands is ensured by the center of influence of the pituitary gland and hypothalamus with the help of adrenocorticotropic hormone (ACTH). Thus, there is an interaction between the adrenal cortex, pituitary gland and hypothalamus. This coordinated work represents an integral system that ensures the resistance of the human body to destruction provoked by stressful situations of external factors. Let us consider each element of the HPA separately and the process of their interaction with each other.