Despite the high level of development of medicine, some pathologies remain not fully understood. One of these diseases is Tolosa-Hunt syndrome. Currently, only the symptoms of this pathology are known, while the causes have not yet been fully disclosed. Most likely, this is due to the fact that the disease is very rare and was discovered not so long ago. In addition, Tolosa-Hunt syndrome is often “masked” as other pathologies and is easily confused. The main symptom is damage to the eyes and cranial nerves. It is known that one of the properties of this disease is that it is amenable to hormonal therapy, after which improvement quickly occurs. However, relapse can occur at any time.
Description of Tolosa-Hunt syndrome
The first mention of this disease appeared relatively recently. It was described in 1961 by the English ophthalmologist Hunt. In addition to the main name, the pathology is also called differently, for example, “chameleon”. This is due to the fact that its symptoms resemble many other ailments. Among them: head tumors, infectious encephalitis, orbital myositis and even diseases of the hematopoietic system. In addition, Tolosa-Hunt pathology is called a symptom of the superior orbital fissure, which does not accurately reflect the essence of the problem. The clinical picture of this disease depends on which nerves of the brain are affected. Most often, Tolosa-Hunt syndrome is characterized by pain in the orbital area, the inability to move the gaze, and diplopia. With timely initiation of hormonal therapy, a complete cure or stable remission can be achieved.
Prognosis and prevention
In most cases, with timely treatment, Ramsay Hunt syndrome has a favorable prognosis for recovery. Incomplete elimination of the virus during antiviral treatment causes individual relapses of the disease. The persistent course of prosopalgia is observed mainly in old age. Specific prevention involves vaccinating children against chickenpox. An additional measure that can prevent Hunt syndrome is active antiviral treatment of patients with chickenpox. A healthy lifestyle, which allows you to maintain a high level of immunity, is of no small preventive importance.
Etiology of Tolosa-Hunt syndrome
Due to the fact that the pathology has various manifestations and begins suddenly, it has not yet been possible to establish the exact etiology. This is also due to the low occurrence of the syndrome. For this reason, doctors do not have the opportunity to properly study this disease. There are several assumptions according to which pathology may develop. The following etiological factors are identified in patients with Tolosa-Hunt syndrome:
- Malformation. This term implies abnormal development of the vascular system of the eyes. As a result of the malformation, mixing of arterial and venous blood occurs, which should not be normal. This disorder is more common among the female population.
- Autoimmune aggression. This factor is the trigger for many diseases. However, it is still not possible to answer the question of why immune cells begin to destroy body tissues. In most cases, “aggression” occurs after suffering stress and long-term infectious processes.
- Various neoplasms of the brain and cranial nerves. These can be either benign or cancerous tumors.
Postzoster Ramsay–Hunt syndrome
An urgent problem of modern medicine is postherpetic neuralgia, which is associated with an increase in the number of herpesvirus diseases with the formation of pain syndrome in case of damage to the ganglia. The frequency of herpes zoster after chickenpox with the formation of neuralgia in different countries of the world ranges from 0.4 to 1.6 cases per 1000 patients per year under the age of 20 years.
Herpes viruses are widespread in nature, being the most ancient pathogens of human diseases. This ability to persist over time is associated with their ability to pass into a latent state and integrate into the host genome, transforming into another qualitative form. Herpes viruses have a wide variety of transmission routes and can affect any organs and systems of the human body, causing acute, latent and chronic forms of the disease. In the modern classification, depending on the type of cells involved in the infectious process, the nature of viral replication, and the structure of their genome, these viruses are divided into three subfamilies - α-, β- and ν-herpesviruses [1–3]. Representatives of α-herpesviruses are herpes simplex virus types 1, 2 (HSV type 1, type 2) and varicella-zoster virus (VZV type 3). β-herpes includes HHV type 5 - cytomegalovirus. ν-herpes includes EBV - HHV type 4, HHV types 6, 7 and 8.
The varicella-zoster virus (VHV type 3), causing a well-known childhood infection - chickenpox, can lead to serious damage to the peripheral nervous system - ganglioneuritis and ganglioradiculitis.
It has been proven that even under the conditions of one subclone, virions are characterized by polymorphism and antigenic variability. Therefore, type 3 HHV causes chickenpox in some people, and herpes zoster in others, affecting only the skin in some, mucous membranes in others, and infecting the endoneurial and perineural cells of the olfactory fibers and entering the parenchymal cells of the olfactory bulb, and can penetrate into the central nervous system (CNS). It is believed that this route of transmission is the only way for neurotropic viruses to enter the central nervous system during infections with low levels of viremia. Thus, initially or after chickenpox, the virus penetrates through the skin and mucous membranes, then through the lymphogenous and hematogenous route into the ganglia, intervertebral nodes and dorsal roots of the spinal cord, where it can persist for a long time in a latent state. The virus infects the branches of the olfactory or trigeminal nerves and reaches the olfactory bulb or Gasserian ganglion, which is clinically manifested as acute ganglionitis [4].
With a decrease in immunological reactivity under the influence of various factors, such as an immunodeficiency state, exacerbation of chronic diseases, taking immunosuppressants, intoxication, latent infection may become more active. Activation of the virus is accompanied by the development of ganglionitis (intervertebral ganglia or ganglia of the cranial nerves, as well as dorsal roots). With this disease, regional sensory ganglia are affected with the development of radicular pain, parasthesia, and segmental sensory disturbances, which is observed in almost every patient [5].
By localization, lesions are distinguished: trigeminal (Gasserian ganglion); geniculate; cervical; breast; lumbosacral ganglia [5].
According to ICD-10 they classify:
- herpes zoster with other nervous system complications (B02.2);
- postherpetic ganglionitis of the genu ganglion of the facial nerve (G53.0);
- polyneuropathy (G63.0);
- trigeminal neuralgia (G53.0).
The consequence of damage to the geniculate ganglion by the herpes zoster virus was described in 1907 by the American neurologist JR Hunt, and in 1912 by the French neurologists Dejerine, Souques, Sicard. Manifestations of the disease begin acutely, with general symptoms of intoxication and fever. Some patients may experience damage to the facial nerve and trigeminal neuralgia lasting up to several weeks. JR Hunt (1907) described in detail four clinical forms of this disease, which later became known as Hunt's syndrome. In cases of very common ear zoster, the latter affects not only the external auditory canal, the auricle, the mastoid process, but also the eardrum, which sometimes suffers very seriously. In such cases, the area innervated by pairs V, VII and X is affected, and damage to these nerves is accompanied by damage to the ganglia, corresponding cranial nerves, or anastomoses connecting the terminal branches of all of the above nerves [6, 7].
With ganglionitis of the Gasserian ganglion, excruciating pain and rashes are observed in the area of innervation of I, II, III or all branches of the trigeminal nerve. According to some authors, herpetic ganglionitis of the Gasserian ganglion is more common than ganglionitis of the intervertebral ganglion.
Most patients with this localization of the process experience increased temperature and swelling of the face on the affected side, as well as pain at the exit points of the trigeminal nerve. Neuralgia (from ancient Greek νεuρον - vein, nerve + aλγος - pain) is a lesion of the peripheral nerves, characterized by attacks of pain in the area of innervation of a nerve. Unlike neuritis, neuralgia does not have motor disturbances or loss of sensitivity [7–9].
Post-zoster (postherpetic) neuralgia (PHN) occurs in approximately 10-15% of patients suffering from herpes zoster. The development of post-zoster neuralgia is preceded simultaneously by general insensitivity of the affected dermatome and severe pain in the initial phase of herpes zoster. PHN is described as a constant, excruciating, burning pain of varying intensity, sometimes accompanied by sudden, brief attacks of dysesthesia such as tingling and stabbing pain.
The pain syndrome has a pronounced vegetative coloring in the form of burning, paroxysmal, sharp pain, intensifying at night. Subsequently, the pain recurs and bothers the patient for many months and years, causing loss of ability to work, disrupting sleep, changing his mental and emotional status, forming a permanent syndrome - postherpetic neuralgia. The protracted, severe nature of the disease with a long-term, pronounced algic syndrome contributes to the formation of personality disorders [10].
A clinical example of ganglionitis that developed as a result of a complicated course of chickenpox
Patient Arina K., born June 20, 1992. Case history No. 18230.
Anamnesis of life. The girl was born from the first pregnancy, which proceeded without pathology, term birth, weighing 3650 g, length 53 cm. The early postnatal period proceeded without pathology, breastfeeding for up to 6 months. Development corresponded to age. There is no allergic history. Vaccinations were carried out in accordance with the NCP; no pathological reactions were observed in the post-vaccination period. She suffered from whooping cough at the age of 2.5 years, and enteroviral myalgia at the age of 4 years. The girl lived in the Krasnodar region.
History of the disease. At the age of 7 (1999) she fell ill with chickenpox, which occurred with an abundance of rashes on the skin and mucous membranes, which were mainly localized in the head, neck, face, and ears. Hyperthermic syndrome followed by prolonged low-grade fever (for 40 days) was recorded. On the 21st day from the onset of the disease, the temperature rose again to 40 °C. Several days before, the girl complained of severe “burning” pain in the area of the eye sockets and forehead, where papular-vesicular rashes reappeared. Against this background, she complained of photophobia, lacrimation, sound and noise intolerance, and persistent cephalgia was noted. She was hospitalized.
In the hospital she received antibiotic and glucocorticoid therapy (antiviral therapy was not carried out). The patient's condition improved during treatment and the pain disappeared. However, after 6 months, repeated complaints of “bursting”, “burning” pain in the eyes, ears, and cervical region appeared, which was accompanied by hyperemia and swelling in the periorbital area. With a short course of hormonal therapy, these symptoms were relieved. In the spring of 2000, the same complaints were repeated, she received treatment in a sanatorium without much effect, after which she was periodically hospitalized in the neurological department. Received symptomatic therapy.
In 2002, against the background of increased pain in the same localization, acyclovir therapy was administered with a positive effect. In 2003, there was another attack of more intense and prolonged pain in the eyes, neck, ears, with lacrimation and persistent headache. Ramsay–Hunt syndrome was diagnosed. A short-term effect was obtained from intravenous acyclovir therapy. After 2 weeks, the attack repeated, but of less intensity. During 2003, a monthly course of therapy with Viferon-2 and T-activin was carried out; the girl rarely attended school due to repeated attacks of pain. I was consulted in Moscow at the State Medical Academy named after. I.M. Sechenov, where a psychiatrist diagnosed hypochondriacal syndrome.
In February 2004, she turned to our department for help, where an examination confirmed Ramsay-Hunt syndrome after chickenpox and herpes zoster, which required the exclusion of other background persistent herpesvirus infections and assessment of the immune status.
A neurological examination revealed complaints of dizziness, accompanied by nausea, pain in the occipital-parotid and periorbital areas. Weakness of convergence, significant smoothness of the nasolabial fold on the right, hyperesthesia in the C2-C3 zone on the right were noted; tenderness in the region of the greater occipital nerve on the right; head turns to the sides were limited; the general tone of the mood was reduced, the girl was attuned to her feelings.
X-ray did not reveal any pathology in the cervical spine area.
When examined by an ophthalmologist, a spasm of accommodation and acquired myopia were revealed.
A serological and molecular genetic examination was carried out for the entire spectrum of herpesvirus infections, positive results were obtained for the Epstein-Barr virus, HHV types 1, 6 when examining blood, urine and saliva using enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR) ), which indicated a slow, persistent herpesvirus infection, including varicella-zoster infection.
ELISA for anti-IgG to varicella-zoster virus - 1:16000; anti-IgG - to HSV1–1:24000; anti-IgG to EBV (to VCAg - 1:160; to EAg - 1:80); in saliva: DNA HHV-6 - positive, DNA EBV - positive, DNA CMV - positive; in urine: DNA HHV-6 - positive, DNA EBV - positive, DNA CMV - positive, DNA HSV1 - positive; in blood - negative
The immune status revealed a lack of cellular immunity: a decrease in CD19+, CD20+, CD4+, IRI - to 0.89. Indicators of immunoglobulins A, M and G are within normal limits.
She was consulted and examined by an immunologist at the Research Institute of Immunology of the Russian Academy of Medical Sciences, where a secondary immunodeficiency state was established against the background of a slowly ongoing persistent herpesvirus infection.
General blood tests, urine tests, and biochemical blood tests revealed no pathology.
Thus, taking into account the medical history and the results of an objective examination, the patient was diagnosed with Ramsay–Hunt syndrome (ganglionitis with damage to the nuclei of the facial and trigeminal nerves, neuropathy of the greater occipital nerve), which developed against the background of chronic mixed persistent GVI: HVZ, HSV1, CMV and HHV type 6 with a developed secondary immunodeficiency state. Accompanied by asthenohypochondriacal syndrome against the background of chronic pain syndrome. It should be noted that antiviral therapy was not prescribed in a timely manner, which was not initially used in the acute period of chickenpox, which was severe, and in the recurrent nature of the course, which required clarification of the background pathology that caused the unfavorable outcome of this infection.
Considering the short duration of the effect on previous antiviral and hormonal therapy, at the clinical base of our department - in the Morozov City Children's Clinical Hospital, it was decided to include in complex therapy a course of highly active intravenous immunoglobulin drugs (pentaglobin, Octagam - 22.5 g per course), intranasal myelopid , T-activin 100 mg IM for 1 month; for anti-inflammatory purposes - I received phosphogliv intravenously in an intermittent course - 3 months, Gepon intranasally for 2 weeks, neuropsychotropic drugs: amitriptyline 1/2 table. at night, Finlepsin 1/2 tablet. 2 times - up to 3 months, Cavinton 1 tablet. 3 times a day for 1 month, Phenibut 1 tablet. 3 times during inpatient treatment. With this therapy, the patient's condition improved significantly. Since the girl moved permanently to Moscow, follow-up observation was continued at our department and at the neurological center. During the girl's 5-year follow-up, the intensity and frequency of repeated attacks of pain decreased significantly due to repeated courses of neurotropic and immunotropic drugs, including antiviral therapy with Famvir. This contributed to the inclusion of the patient in a normal mode of education at school and, at the same time, in a music school (which she was deprived of for several years). She continued her studies at a music school.
The current standard and protocol for the treatment and prevention of chickenpox and herpes zoster provides the following recommendations.
Antiviral therapy
In moderate and severe forms of chickenpox or herpes zoster, as well as in immunodeficiency states, including patients receiving immunosuppressive therapy with cytostatics or glucocorticosteroids, suffering from background encephalopathy, regardless of the form of severity, antiviral drugs are used as etiotropic therapy.
Drug of choice for chickenpox:
- Acyclovir orally 0.2 g (children under 2 years); 0.4 g each (children 2–6 years old); 0.8 g (children over 6 years old) 4 times a day, 7 days.
Drug of choice for herpes zoster:
- Valaciclovir orally 1 g 3 times a day, 7 days.
In severe cases, antiviral drugs are prescribed parenterally:
- Acyclovir in 100 ml of 0.9% sodium chloride solution intravenously, 5–10 mg/kg.
Drug of choice for herpes zoster for topical use:
- Valacyclovir (ointment or cream) on the affected areas 5 times a day with an interval of 4 hours, 5–10 days + Glycyrrhizic acid (cream) on the affected areas 5 times a day with an interval of 4 hours, 5–10 days.
Immunotherapy
With the development of encephalitis or menigoencephalitis, as well as in severe atypical forms, standard immunoglobulin preparations are administered to intensify etiotropic therapy: normal human immunoglobulin (IgG + IgA + IgM) IV drip 5 ml/kg 3-5 injections (if necessary after 1 week repeat the course) or normal human immunoglobulin IV drip 5–8 ml/kg 1 time per day, 3–5 injections.
Therapy is carried out with antihistamines along with antipyretics (paracetamol, ibuprofen), and analgesics are prescribed for pain.
Vaccine prevention of chickenpox
Currently, the Varilrix vaccine is used, 0.5 ml is administered subcutaneously or intramuscularly.
One dose of Varilrix is given to children aged 12 months to 13 years, and two doses are given to adolescents aged 13 years and older and adults, with doses separated by 6-10 weeks, providing 95% optimal protection against chickenpox.
Varilrix can be given at the same time as other childhood vaccines, such as measles-rubella-mumps, making it an excellent candidate for universal mass vaccination.
Indicated for single-dose post-exposure prophylaxis up to 96 hours after exposure to the virus (preferably within 72 hours). This reduces the severity of chickenpox and is a reasonable strategy for preventing outbreaks.
Varilrix™ vaccine can be stored in a regular refrigerator at 2–8°C for up to 2 years.
Vaccines from other companies are also registered in Russia: Varivax and Okavax.
The Zostavax vaccine is used in the world, which is used in adults to prevent herpes zoster.
Conclusion
The use of a timely integrated systemic approach in the treatment of the main causes of post-zoster ganglionitis using antiviral, immunotropic, neurotropic, and also drugs that affect pain syndrome can reduce the degree of disability in this category of patients.
Existing myths that chickenpox is a mild childhood infection are dispelled when this infection is layered with a persistent other herpes virus infection, immunodeficiency, organic vascular pathology of the brain, etc., which often predetermine an unfavorable outcome of the disease.
Therefore, the issue of prescribing antiherpetic therapy in such cases is decided in favor of prescribing it even for a mild form of chickenpox.
It remains fundamentally important to underestimate the importance of preventing this infection, where until now there is a common, unsupported opinion that:
- chicken pox is not a dangerous infection;
- with the introduction of vaccinations, the risk of developing shingles increases;
- the vaccine does not give the desired effect;
- introduction of the vaccine is fraught with a high risk of complications, etc.
The authors of this article would really like to draw the attention of pediatricians and general practitioners to the problem of treatment and prevention of chickenpox in children and adults, since, having had it once, even in a mild form, we continue to carry this virus within ourselves throughout our lives with a huge risk of losing a pregnancy , give birth to a disabled person or develop severe neurological pathology.
Literature
- Granitov V.M. Herpesvirus infections. NGMA, 2001. P. 80.
- Dekonenko E.P. Herpes virus and damage to the nervous system // Ros. honey. magazine. 2002. No. 2. P. 46–49.
- Diagnosis of human herpesvirus infections: memorandum of the WHO meeting // Bulletin. WHO. 1991. No. 3. pp. 11–18.
- Redkin Yu. V., Odokienko A. Yu. Modern approaches to pharmacotherapy of recurrent herpetic infection // Experimental and clinical pharmacology. 2005. T. 68, No. 6. P. 67–71.
- Herpes zoster / Ed. A. A. Kubanova. M.: DEX-Press, 2010. 24 p.
- Thakur R., Philip A.G. Treating herpes zoster and postherpetic neuralgia: an evidence-based approach // Journal of Family Practice. 2012. Vol. 61. No. 9. S9–15.
- Hunt JR On herpetic inflammations of the geniculate ganglion: a new syndrome of its complications // [The] Journal of nervous and mental disease, 1907; 34: 73–96.
- Hunt JK The sensory field of the facial nerve: a further contribution to the symptomatology of the geniculate ganglion // Brain. 1915. Vol. 38. P. 418–446.
- Bhupal HK Ramsay Hunt syndrome presenting in primary care. Practitioner 2010. 254 (1727). pp. 33–53.
- Maksimova M. Yu., Sineva N. A., Vodopyanov N. P. Postherpetic neuralgia (neuropathy) caused by herpes zoster // Farmateka. 2013. No. 10. pp. 58–62.
F. S. Kharlamova*, 1, Doctor of Medical Sciences, Professor V. F. Uchaikin*, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences I. M. Drozdova** A. E. Angel**
* GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow ** Morozovskaya State Budgetary Institution of Children's City Clinical Hospital of the Department of Health of the Russian Federation, Moscow
1 Contact information
Buy an issue with this article in pdf
Mechanism of development of the syndrome
Given that the etiology of the disease remains unknown, the pathogenesis also cannot be fully studied. Regardless of the reasons why the pathology develops, only certain structures of the eye and nervous tissue are affected. As you know, the second name of the disease is superior orbital fissure syndrome. This is due to pathogenesis, because the nerves and vessels that pass through it are affected. First of all, changes are observed in the ophthalmic vein and artery. As a result, tissue trophism is disrupted. In addition, the cavernous sinus, which is adjacent to the superior orbital fissure, is damaged. The arteries supplying it become inflamed, and the tissue hypertrophies. As is known, the following cranial nerves pass through the gap: trochlear, abducens, part of the trigeminal and oculomotor. In some cases, all of these pairs are affected. At the same time, the ability to rotate the eyeball suffers. Sometimes the function of one or two pairs of nerves is impaired.
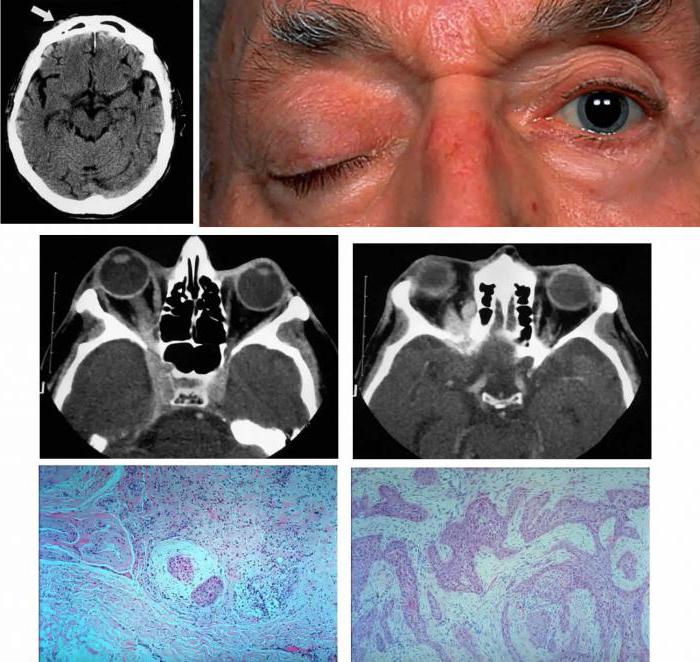
Diagnostics

What is it necessary to differentiate this disease from? There are a huge number of reasons for the development of similar symptoms: tumors of the middle cranial fossa, pterygoid bone, pituitary gland, parasellar tumors, retrobulbar space-occupying processes, cavernous sinus tumors, cavernous sinus thrombosis, carotid artery aneurysms, periostitis, osteomyelitis, leukemic infiltration in the area of the superior orbital fissure.
Do not forget about diseases such as myasthenia gravis, diabetes mellitus, thyroid pathology, temporal arteritis, meningitis, multiple sclerosis, migraine with aura. All of the above conditions can lead to ophthalmoplegia and dysfunction of the cranial nerves. That is why a patient with syndromes of impaired movement of the eyeball and pain in one half of the face requires close attention. The research must be comprehensive and multifaceted. A consultation with an ophthalmologist is necessary to examine the fields and visual acuity and fundus. The neurologist must carefully collect anamnesis and conduct a full clinical examination.
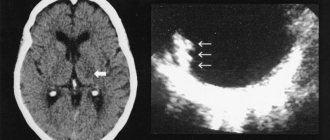
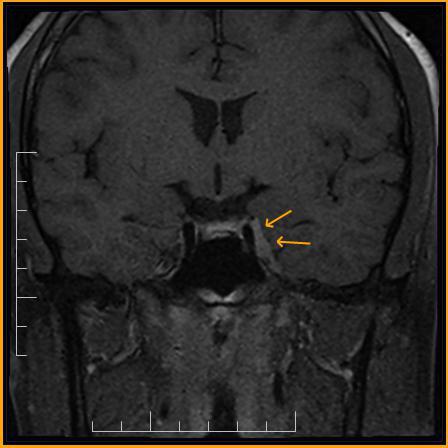
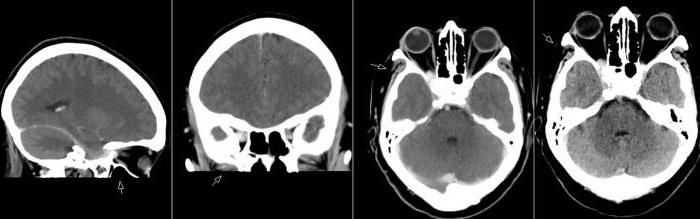
Additional research methods include neuroimaging methods (CT and MRI of the brain and sella turcica), angiography, and echography of the orbits.
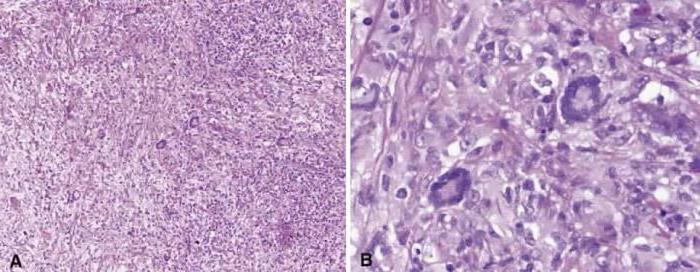
According to modern diagnostic criteria, Tolosa-Hunt syndrome can be diagnosed only in one case: when magnetic resonance imaging (MRI) of the brain reveals granulomatous inflammation of the outer wall of the cavernous sinus. Under ideal conditions, a biopsy should be performed for diagnosis. Recent studies have shown that half of patients with a confirmed diagnosis of Tolosa-Hunt syndrome have changes in the venous bed of the orbital region. If an MRI does not reveal a granuloma, it would be more correct to make a diagnosis of “superior orbital fissure syndrome” and manage the patient under dynamic observation. At the same time, there are clinical diagnostic criteria, which include the following manifestations and conditions:
- “burning” or “tearing” pain of a constant nature behind the orbit or in the orbital-temporo-frontal region;
- impaired mobility of the eyeball that occurred immediately or within 14 days after the onset of pain;
- damage to other nerves that pass through the superior orbital fissure (III, IV, VI cranial nerves, I branch of the trigeminal nerve, autonomic fibers);
- symptoms intensify over several days, even weeks;
- characterized by the presence of spontaneous remissions, often without residual effects;
- the disease may return after several months or years;
- a thorough examination does not find other causes that can cause this condition;
- regression of symptoms within 72 hours after the start of immunosuppressive therapy.
Tolosa-Hunt syndrome: symptoms of the disease
Pathology most often makes itself felt in old age. Both women and men can be affected by this syndrome. The clinical picture of the disease develops suddenly, without any prerequisites. The following symptoms are identified:
- Pain in the orbital region. Unpleasant sensations first appear in the area of the forehead, eyebrows, and head. Later, the intensity of the pain increases and spreads to the eyes.
- Diplopia. This sign appears after the development of pain. It seems to the patient that all the objects he looks at are split into two. It's hard to concentrate your gaze.
- Impaired mobility of the eyeball - ophthalmoplegia. Most often observed on one side. Its degree depends on the intensity and number of nerves affected.
- Edema of the conjunctiva.
- Exophthalmos. It is observed in the absence of treatment and frequent relapses.
- Strabismus. Occurs when the nerves are affected on only one side.
- Low-grade fever and deterioration.
These symptoms usually increase gradually and replace each other. In some cases, they are all observed simultaneously. Signs of the disease may suddenly disappear, just as they appeared. Nevertheless, without treatment, the pathology always makes itself felt again. The frequency of relapses is different for everyone, as is the duration of remission.
Complications
Ramsay Hunt syndrome has a predominantly favorable course. Complications arise when prosopalgia becomes chronic. Chronic pain causes sleep disturbances, emotional and psychological disorders. Patients become irritable, emotionally labile, and their overall mood decreases. In the absence of correct treatment of prosopalgia and psychological support, the development of neurotic manifestations is possible: depression, hypochondria, neurasthenia. Treatment-resistant pain syndrome leads to a persistent decrease in working capacity.
Tolosa-Hunt syndrome: diagnosis of pathology
It is not easy to identify this pathology, since its symptoms are similar to many other diseases. Therefore, Tolosa-Hunt syndrome is considered a diagnosis of exclusion. First of all, the patient is asked about the characteristics of the course of the disease (how it started, how the symptoms developed). After this, laboratory tests and instrumental diagnostics are performed. It is very important to perform an ophthalmological and neurological examination. An MRI is performed to rule out brain tumors. It is also important to conduct an ultrasound and x-ray examination of the eye orbits. The presence of vascular malformation is determined by angiography. In addition, one of the diagnostic criteria is the effectiveness of hormonal therapy. If laboratory and instrumental examinations do not reveal pronounced changes, and the symptoms quickly stop after treatment, then most likely the diagnosis is Tolos-Hunt syndrome. Prednisolone is the most commonly used treatment.
Classification
Ramsay Hunt syndrome occurs in various clinical variants, which also include combined damage to the facial and vestibulocochlear nerves. Understanding the form of the disease and the stage of its clinical course is necessary when choosing treatment tactics. According to the clinical classification, there are four main forms of the syndrome:
- Hunt I - rashes in the area innervated by the geniculate ganglion are not accompanied by neurological symptoms.
- Hunt II - herpetic rashes occur with paresis of the facial nerve.
- Hunt III - facial paresis and blistering rash are combined with hearing impairment.
- Hunt IV - vestibular disorders are added to the manifestations characteristic of Hunt III syndrome.
There are three clinical periods during the course of the disease:
- General infectious - characterized by general symptoms: weakness, lethargy, fever.
- Skin - the period of appearance of a typical herpetic rash.
- Neuropathic - characterized by the predominance of neuralgic pain syndrome.
Differential diagnosis with other diseases
This disease is compared with other pathologies of the eyes and nervous system. First of all, it is necessary to exclude inflammatory processes in the brain and its membranes, as well as tumors. If meningitis or encephalitis is suspected, a spinal tap is performed. In order to exclude benign neoplasms and cancer, the patient undergoes MRI, CT scan of the brain and X-ray of the skull. The disease is differentiated from lymphomas, cavernous sinus cysts and its thrombosis. Also, similar symptoms can be observed in systemic pathologies, such as sarcoidosis, orbital myositis, migraines, etc. To make an accurate diagnosis, the patient must be examined by various specialists: an ophthalmologist, a neurologist, a vascular surgeon, an endocrinologist.

Treatment for Tolosa-Hunt syndrome
Treatment for Tolosa-Hunt syndrome involves prescribing medications that suppress the immune system. For this purpose, hormone-containing medications are used: Prednisolone, Hydrocortisone. These drugs also have an effect in other autoimmune pathologies, but with this disease the symptoms disappear after 3-4 days. Treatment of Tolosa-Hunt syndrome with prednisolone is carried out at a rate of 1-2 mg/kg body weight. If the drug is used in the form of a solution, then 500 to 1000 mg per day is prescribed. In addition, painkillers and vitamins are used.
Causes of Hunt's syndrome
After chickenpox, the pathogen remains in the body in a “dormant” state, so in some cases it can reactivate into shingles. Well, as a result of the complicated course of this infection, the facial nerve becomes inflamed and irritated, as a result of which the patient experiences acute pain. For example, this scenario is typical when the function of the immune system decreases: its ability to fight infections sharply decreases, and the human body becomes vulnerable to the previously harmless chickenpox virus.
Work ability in Tolosa-Hunt syndrome
Usually, with this diagnosis, patients’ ability to work is preserved. It is necessary to be sure that the patient has Tolosa-Hunt syndrome. Disability with this pathology is rare. However, with frequent relapses, group 3 may be prescribed. The patient should be transferred to light work that does not require visual effort. Also, with persistent nerve damage, the patient cannot drive due to impaired movement of the eyeballs and diplopia.